Abstract
Background
Work-related musculoskeletal disorders (WRMDs) are often caused by inadequate use of the musculoskeletal system during work. Evidence suggests that multimodal intervention through exercises, massage, education, and ergonomic guidelines reduces pain and symptoms in the neck and upper extremities and help to prevent musculoskeletal disorders. The purpose of this study will be to assess the additive effectiveness of a specific and individualized workplace strengthening exercise program to an ergonomic guidance in reducing fatigue, pain and discomfort in the upper extremities and neck perceived by workers.
Methods
This trial was designed according to the Consolidated Standards of Reporting Trials - CONSORT guidelines. Participants will be employees of a tertiary hospital, with any complaints of pain or discomfort in the upper extremities during the past 12 months, without clinical musculoskeletal diagnosis. 166 participants will be randomized into parallels groups as control and workplace exercises. The primary outcomes will be Numerical Pain Scale, isokinetic muscle strength of abduction and isometric handgrip strength. Secondary outcomes on discomfort, fatigue, work capacity and dysfunction will be assessed by QuickDASH, Patient Specific Functional Scale, Neck Disability Index, Need for recovery, Work Ability Index self-report questionnaires and FIT-HANSA performance test. The Ergonomic Work Analysis will be done by Quick Expose Check, RULA, REBA, RARME, ROSA and HARM risk assessment ergonomic tools. We will analyze the difference between baseline and 12 weeks of intervention by T test of independent samples (95% confidence interval, p < 0.05). Clinical significance will be analyzed by the minimum clinically important difference and effect size by Cohen index. The association between the variables will be analyzed by construct validity with the hypothesis of correlations between pain and muscle strength, strength and functionality and strength and fatigue.
Discussion
Although studies have shown promise outcomes for workplace exercises as an available therapeutic resource used to minimize complaints of pain and discomfort related to work, the results of this study aim to bring evidence about the benefit of a specific resistance exercise as an effective modality to facilitate mechanisms of neuromuscular adaptations, with gradual and posterior hypertrophy in the later phases.
Trial registration
(NCT04047056, https://clinicaltrials.gov/ct2/show/NCT04047056?term=NCT04047056&draw=2&rank=1) on Dec 03, 2020.
Similar content being viewed by others
Background
Work-related musculoskeletal disorders (WRMDs) are a group of functional and mechanical disorders, often caused by overuse or inadequate use of the musculoskeletal system during work [1,2,3]. Muscles, tendons, fascia, nerves, joint and bones can be affected, and the result is fatigue, decreased performance at the workplace, temporary disability and absenteeism with economic consequences [4]. WRMDs are the second major cause of sick pay benefits in social security [5] and its prevalence has been increasing [1].
The most affected areas by WRMDs are neck, upper extremity, and low back [6,7,8]. Neck and upper extremity disorders can be divided into specific conditions with clear pathology and diagnosis, such as carpal tunnel syndrome, or non-specific conditions, which are defined by the location of symptoms, with unknown or imprecise physiopathology, such as neck strain syndrome [9].
Risk factors at the workplace related to neck and upper extremity symptoms include physical factors (harmful postures, repetitive tasks and static contractions), organizational factors (excessive work and absence of breaks), and psychosocial factors [6, 9,10,11,12]. Many tools have been developed and validated for the work ergonomics assessment. They aim to facilitate the survey of data regarding the various demands and workplace setting, postures assumed during professional activities, the perception of the worker regarding symptoms and muscle fatigue, and also to identify and classify the risk factors for the development of WRMDs [13,14,15].
In order to reduce WRMDs many companies have been investing more in prevention programs with a multidisciplinary approach for the promotion and maintenance of health, providing safer working conditions [16,17,18], adequate ergonomics [19] and workplace exercises [1, 9, 20]. Workplace exercises consist of specific activities performed during the working time. They usually have a short duration, with both preventive and therapeutic approaches, avoiding overloading or leading the employee to fatigue. It is a physical activity based on exercises to compensate repetitive movements, the absence of movement, or uncomfortable postures assumed during the working period [21].
To achieve more effective results with the implementation of workplace exercises, specific programs must be developed based on the objectives to be achieved. Some factors that are determinants of muscle performance must be taken into consideration, such as strength, power and endurance, together with the physiological adaptations to the exercises, which are influenced by intensity, exercise loads, volume, frequency and duration [22]. The resistance training is an effective method in the prevention and management of various disorders without distinction of sex. It is grounded on short term (6–8 weeks) mechanisms of neuromuscular adaptations, followed by gradual and posterior hypertrophy in the later phases (12–26 weeks) [23], leading to a balance and meeting individual’s needs and goals.
Recent studies aiming to evaluate the effectiveness of a physical exercise program performed in the workplace in reducing symptoms in the upper extremity and neck have shown promising results [1, 2, 4, 24,25,26,27,28,29]. Some randomized clinical trials have observed a reduction in pain and symptoms in the neck and upper extremity after the application of a multimodal intervention protocol composed by specific resistance exercises, muscle stretching, massage, educational and ergonomic guidelines within the work environment [2, 4, 20, 27,28,29].
Considering the aforementioned about previous studies, the aim of this study is to assess the additive effectiveness of a specific and individualized workplace strengthening exercises program to a protocol of ergonomic guidance in reducing fatigue, pain and discomfort in the upper extremity and neck of workers in a university hospital. Our hypothesis is that the group submitted to resisted exercises will demonstrate a decrease in musculoskeletal complaints and a better functional performance, in comparison to the group receiving only ergonomic guidance.
Methods
Trial design
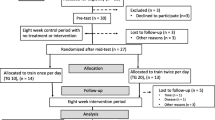
This will be a prospective randomized controlled trial with concealed allocation by using opaque, sealed envelopes consecutively numbered and included each group’s name and deviation from the intention-to-treat analysis [30]. The study was designed according to the Consolidated Standards of Reporting Trials - CONSORT guidelines [31] for randomized clinical trials and following the standard protocol items for randomized interventional trials (SPIRIT) [32]. Participants will be randomized to receive either ergonomic guidance alone or ergonomic guidance and workplace strengthening exercises (Fig. 1).
The study follows all ethical considerations set out in the Declaration of Helsinki and has received the approval from the Local Research Ethical Committee CAAE: 02658018.2.0000.5440. It was prospectively registered at www.ClinicalTrials.gov (NCT04047056).
Participants
The participants of this study will be employees of a tertiary hospital, from any section, with any complaints of pain or discomfort in the upper extremity during the past 12 months. Potential subjects will be recruited by verbal invitation, posters and institutional cell phone messages. Inclusion and exclusion criteria are described in Table 1. All participants will sign a written informed consent form before participating.
Randomization
Employees who agree to participate will be randomized in a 1:1 ratio by a random allocation sequence by concealment envelopes in two parallel groups: control group (CG) and workplace exercise group (WEG).
Blinding
Due to the nature of this study, it is not possible to fully blind the research participant or the clinician investigator providing the intervention. Randomization will be blinded for the outcome data collection and statistician assessors.
Procedures for the experimental proposal of intervention
Control group
Participants in the CG will receive ergonomic guidance. The protocol will be composed by group lectures, digital handouts and specific ergonomic orientations and suggestions of low-cost changes in each participant’s workplace. The content of lectures and digital handouts will comprise information about what are WRMDs and how to prevent them and general posture and ergonomic guidelines, both for daily living and occupational activities.
Workplace exercise group
In addition to the ergonomic guidance, the WEG group will attend exercise sections 3 times/week, for 12 weeks. Exercise sections will take place inside the hospital, according to the workers’ availability during the breaks within working hours and will last 20 min. They will be divided as follows:
-
1.
Five-minute warm-up movements (3 × 15 repetitions each);
-
2.
Ten minutes of specific resistance strengthening exercises (3 × 10 repetitions each);
-
3.
Five minutes of stretching and relaxing movements (3 × 30 seconds each).
Resistance strengthening exercises for cervical region and upper extremity will be performed with individually defined load and progression. The movements will be: flexion, abduction and shoulder elevation in the scapular plane; external shoulder rotation; “push up” on the wall; elbow flexion associated with pronation (concentric) and supination (eccentric) and manual grasping (Additional file 1: Appendix 1). Regarding the intervals between the movements, active recovery will be adopted to neutralize the effects of muscle fatigue. The criteria for interruption will be pain that incapacitates the execution of the movement, pain and /or discomfort or sensory alterations such as tingling and numbness.
Two physiotherapists with the collaboration of an undergraduate student will conduct the intervention. Sections will happen in small groups (Fig. 2), favoring social contact and integration among the employees, with the intention to improve the employee’s mood, as well as their adherence to the protocol.
Outcome measures
Demographic information
Participants will be interviewed and assessed for demographic and descriptive information including age, sex, weight, and height for the body mass index (BMI) calculation, history of smoking or alcoholism, dominance, occupation, work task (repetitive movements, and vibration), time of service, if any previous history of injury and symptoms perceived in the cervical region and upper limbs (intensity of pain, location and duration of the symptoms). Demographic information will be collected at the baseline examination only.
Additionally, the following self-reported questionnaires will be applied:
-
1.
The International Physical Activity Questionnaire (IPAQ) short version, to characterize the sample as very active, active and irregularly active [33].
-
2.
The Global Lateral Preference Inventory (GLPI) [34] to assess laterality and manual preference. The subject can fill out the activities according to his/her preference in the options: always left, majority left, indifferent, majority right, always right and I don’t know. Each of these answers has a different score. At the end, punctuation will be summed to generate the qualitative classification
Primary outcome measures
-
Pain: assessed by the Numerical Pain Scale (NPS) [35].
-
Mean isokinetic peak torque: workers will be submitted to the upper limb strength assessment in the isokinetic dynamometer Biodex System 4 Pro™, following all the calibration and use recommendations referred by the manufacturer in the manual “Biodex multi-joint system - pro setup/operation manual”. Based on Prentice and Voight (2003) [36], all movements will be performed at a speed of 60°/sec. The dynamometer positions will be based on the positioning guidance material, except for the scapular plane elevation that was adapted for this study, based on Kapandji (2000) [37]. The movement to be tested in isokinetic mode will be shoulder elevation in the plane of the scapula. The test will consist of 5 direct repetitions, with the volunteer being instructed to perform his maximum force during all repetitions, with an interval of 3 min between one segment and another [38]. Isokinetic tests will be done bilaterally to collect the parameters of the mean peak torque in Newton (N).
-
Isometric palmar grip strength: will be measured by the JAMAR™ dynamometer, an instrument recommended by the American Society of Hand Therapists (ASHT) because of its reported reliability and validity [39].
Secondary outcome measures
-
Fatigue: muscle performance will be assessed through the The Functional Impairment Test-Hand and Neck/Shoulder/Arm (FIT-HaNSA) [40]. This device assesses fatigue resistance during tasks that simulate gross motor functions of the upper limb, such as reaching and picking up objects at different heights and working sustained above the head [40]. The test consists of three tasks: 1) a shelf is placed at waist level and one 25 cm above it, 3 containers of 1 kg are placed on the lowest shelf; using the committed arm, the volunteer must place the 3 containers, from one shelf to the other, at a speed of 60 beats/minute controlled by a manometer; 2) a shelf is placed at eye level and one 25 cm below it. Volunteers are again instructed to use their affected arm to take the 3 containers from one shelf to another at a speed of 60 beats/minute. 3) A plate containing screws is fixed perpendicularly to the shelf. Volunteers are instructed to use both arms to tighten and loosen screws repeatedly. Each task will be performed only once, for a maximum of 300 s, or when the volunteer uses the criteria for stopping the test, which are: perform compensation with uncorrected trunk movements in up to 5 successive repetitions, interrupt the test due to extreme pain or fatigue or inability to complete 1 repetition of the movement within 2 beats of the metronome for 5 successive repetitions.
-
Map of pain description: Nordic Questionnaire will be applied [41].
-
Patient Specific Functional Scale (PSFS) [42], QuickDASH questionnaire [43], Work Ability Index (WAI) [44, 45], Need for recovery (NFR) [46] and Neck Disability Index [47] self-reported questionnaires will be applied.
Both primary and secondary outcome measures will be collected at baseline and after 12 weeks of intervention for all volunteers. Work ergonomic evaluation will be a complementary analysis, which integrates the scope of secondary outcome measures and also collected at baseline and after 12 weeks for both groups.
Work ergonomic evaluation
For the worker’s biomechanical overload and occupational exposure risk levels classification the following instruments will be used: the Quick Exposure Check (QEC) [48], Rapid Upper Limb Assessment (RULA) [49], Rapid Entire Body Assessment (REBA) [50], Musculoskeletal Risk Assessment Measurement (RARME) [51], the translated version of Hand Arm Risk Assessment Method (HARM) [52] and the Rapid office strain assessment ROSA [53]. They will be applied based on direct and indirect observation by photographic and videos records of the body and the upper limbs in the more critical situations reported by workers. Work ergonomic evaluation will be performed by 2 physiotherapists familiar with the instruments, blinded for the division of interventional groups.
Data analysis
Sample size calculation
The a priori sample size calculation was performed by GraphPad Statemate™, with power of 80%, effect size of 0.5 and alpha level of 0.05, based on the Numeric Pain Rating Scale and the isokinetic scores of the mean peak torque of the abduction movement in the scapular plane [54]. Seventh five participants will be needed per group. A total of 166 participants with pain or discomfort complaints of upper extremity who meet the inclusion / exclusion criteria and consent to participate will be included in the study, considering 10% sample size loss and analysis per intent to treat [30, 55].
Statistical approach
An investigator will receive the encoded data and perform the statistical analysis entered into a database Excel spreadsheet. The Kolmogorov-Smirnov test will be used to verify the normality distribution of the data. Descriptive statistics (frequencies, means, standard deviation, confidence interval) will be used to analyze the sociodemographic characteristics of the participants. The significant statistical difference between the outcome groups will be analyzed by the T test of independent samples to compare the means at the baseline and after 12 weeks of intervention, using as outcome variables the numeric pain scale, the mean isokinetic scores of peak torque and work, the patient self-reported questionnaires, with 95% confidence interval, p < 0.05. Responsiveness values for interventions to changes in clinical significance will be defined to score the minimum clinically important difference [56]. The Cohen Index will be defined to calculate the effect size, considering 0.3 low, 0.5 moderate and 0.8 high effect [57]. The association between the variables will be analyzed through the construct validity by the hypothesis tests, which determine the convergent and discriminant validity [58, 59]. It is expected that there will be moderate inverse correlation between pain and muscle strength production, moderate correlation between strength production and functionality and strong to moderate correlation between strength production and fatigue endurance. The statistical program SPSS Statistics 20.0 will be used for all analyses [57, 60].
The confounding factors that could be accounted for in the statistical plan and potential to bias even with the randomization process are: occupations will be analyzed together for comparations between control and intervention groups, before and after the intervention but not in subgroups by level of activity load; and intention-to-treat analysis will be performed including data for the noncompliance volunteers, in exception for dropout cases due to loss of follow-up [61].
Discussion
The WMSDs impair occupational activities, reducing productivity at work and increasing absenteeism. They also impact activities of daily living, reducing the quality of life in general. Besides, they generate economic consequences [4, 62]. Workplace exercise is an available therapeutic resource that has been widely used to minimize work-related complaints of pain and discomfort [1, 2, 9, 29]. Its benefits for workers’ health and for the company are already well known in some worker populations, but it is not yet well-established which exercise modalities would have the greatest benefit for workers.
Therefore, the purpose of this clinical trial is to evaluate the effects of a specific resistance exercise program associated with muscle stretching for the upper extremity and cervical region during the working day and compare them to just ergonomic guidance in reducing fatigue and complaints perceived by workers at a university hospital. We hypothesize that workers who receive the workplace exercise intervention will experience decreased pain, fatigue, dysfunction and better perceived long-term work capacity.
The results of this study will bring more evidence about the benefit of a specific resistance exercise program for workers with upper extremity complaints. Possible challenges for this study will include difficulties with participants recruitment and loss of participants for follow-up. To address these challenges, we will make the study widely known at the hospital in order to reach about all the professionals of the hospital in the different support areas such as maintenance, hygiene and cleaning and hospital nutrition, as well as employees in the administrative sector and health professionals.
The choice of the intention-to-treat analysis could reflect the reality of clinical practice in that workers often do not follow ergonomic or exercises instructions and sometimes take up a completely different approach from the one recommended. The limitation issue is that if the adherence is poor, then the results of the study may not be generalized well to workers who do comply with the intervention based on exercises in the intervention group and the ergonomic approach for both groups [63].
Availability of data and materials
Not applicable.
Abbreviations
- WRMD:
-
Work-related musculoskeletal disorders
- CONSORT:
-
Consolidated Standards of Reporting Trials
- SPIRIT:
-
Standard Protocol Items for Randomized Interventional Trials
- NPS:
-
Numerical Pain Scale
- QuickDASH:
-
Short version of Disability of Shoulder and hand questionnaire
- PFSF:
-
Patient Specific Functional Scale
- NDI:
-
Neck Disability Index questionnaire
- NFR:
-
Need for recovery
- WAI:
-
Work Ability Index
- FIT-HANSA:
-
The Functional Impairment Test-Hand and Neck/Shoulder/Arm
- QEC:
-
Quick Expose Check
- RULA:
-
Rapid Upper Limb Assessment
- REBA:
-
Rapid Entire Body Assessment
- RARME:
-
Musculoskeletal Risk Assessment Measurement
- ROSA:
-
Rapid Office Strain Assessment
- HARM:
-
Hand Arm Risk Assessment Method
- IPAQ:
-
International Physical Activity Questionnaire
- GLPI:
-
Global Lateral Preference Inventory
- ASHT:
-
American Society of Hand Therapists
- CG:
-
Control group
- WEG:
-
Workplace exercise group
References
Rasotto C, Bergamin M, Simonetti A, et al. Tailored exercise program reduces symptoms of upper limb work-related musculoskeletal disorders in a group of metalworkers: a randomized controlled trial. Man Ther. 2015;20:56–62.
Sundstrup E, Jakobsen M, Brandt M, et al. Workplace strength training prevents deterioration of work ability among workers with chronic pain and work disability: a randomized controlled trial. Scand J Work Environ Health. 2014;40:244–51.
Ferreira VMV, Shimano SGN, Fonseca MCR. Physical therapy for assessing and preventing ergonomic risks in a financial unit workers. Physical Ther Res. 2009;16(3):239–45.
Van Eerd D, Munhall C, Irvin E, et al. Effectiveness of workplace interventions in the prevention of upper extremity musculoskeletal disorders and symptoms: an update of the evidence. Occup Environ Med. 2016;73(1):62–70. https://doi.org/10.1136/Oemed-2015-102992.
Anuário Estatístico da Previdência Social/Ministério da Fazenda, Secretaria de Previdência, Empresa de Tecnologia e Informações da Previdência. 2018. https://www.gov.br/previdencia/pt-br/acesso-a-informacao/dados-abertos/previdencia-social-regime-geral-inss/arquivos/aeps-2018.pdf. Accessed 30 Nov 2020.
Genebra CVS, Maciel NM, Bento TPF, et al. Prevalence and factors associated with neck pain: a population-based study. Braz J Phys Ther. 2017;21(4):274–80.
Silverstein B, Evanoff B. Musculoskeletal disorders. In: Levy BS, Wegman DH, Baron SL, et al., editors. Occupational and environmental health: recognizing and preventing disease and injury. New York: Oxford University Press; 2011. p. 335–65.
Moreira RFC, Sato TO, Foltran FA, et al. Prevalence of musculoskeletal symptoms in hospital nurse technicians and licensed practical nurses: associations with demographic factors. Braz J Phys Ther. 2014;18(4):323–33.
Verhagen AP, Karels C, Bierma-Zeinstra SM, et al. Exercise proves effective in a systematic review of work-related complaints of the arm, neck, or shoulder. J Clin Epidemiol. 2007;60(2):110–7.
Mather L, Ropponen A, Mittendorfer-Rutz E, et al. Health, work and demographic factors associated with a lower risk of work disability and unemployment in employees with lower back, neck and shoulder pain. BMC Musculoskelet Disord. 2019;20(1):1–10.
Balogh I, Arvidsson I, Bjork J, et al. Work-related neck and upper limb disorders–quantitative exposure–response relationships adjusted for personal characteristics and psychosocial conditions. BMC Musculoskelet Disord. 2019;20(1):139.
Costa BR, Vieira ER. Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am J Ind Med. 2010;53:285–323.
Abrahão JI, Sznelwar L, Silvino A, Sarmet M, Pinho D. Introdução à Ergonomia: da teoria a prática. 1st ed. São Paulo: Blucher; 2009.
Iida I, Guimarães LBM. Ergonomia: projeto e produção. 3rd ed. São Paulo: Blucher; 2016.
Couto HA, Couto DC. Ergonomia 4: dos conceitos básicos à 4ª revolução industrial. 1st ed. Belo Horizonte: Ergo; 2020.
Santos AC, Bredemeier M, Rosa KF, et al. Impact on the quality of life of an educational program for the prevention of work-related musculoskeletal disorders: a randomized controlled trial. BMC Public Health. 2011;11:60.
Rodríguez-Blanes GM, Lobato-Cañón JR, Sánchez-Payá J, et al. The influence of information on the prevention of occupational risks and ergonomic requirements in the development of non-traumatic osteomuscular diseases of the shoulder – a pilot study. Int J Occup Med Environ Health. 2019;32(6):825–39. https://doi.org/10.13075/ijomeh.1896.01429.
Hembecker PK, Reis DC, Konrath AC, et al. Investigation of musculoskeletal symptoms in a manufacturing company in Brazil: a cross-sectional study. Braz J Phys Ther. 2017;21(3):175–83.
Oakman J, Neupane S, Proper KI, et al. Workplace interventions to improve work ability: a systematic review and meta-analysis of their effectiveness. Scand J Work Environ Health. 2018;44(2):134–46.
Shariat A, Cleland JA, Danaee M, et al. Effects of stretching exercise training and ergonomic modifications on musculoskeletal discomforts of office workers: a randomized controlled trial. Braz J Phys Ther. 2018;22(2):144–53.
Prieske O, Dalager T, Herz M, et al. Effects of physical exercise training in the workplace on physical fitness: a systematic review and Meta-analysis. Sports Med. 2019;49(12):1903–21. https://doi.org/10.1007/s40279-019-01179-6.
Kisner C, Colby LA. Therapeutic exercise: foundations and techniques. 5th ed. Philadelphia: Davis Plus; 2007.
Bird SP, Tarpenning KM, Marino FE. Designing resistance training programmes to enhance muscular fitness. Sports Med. 2005;35:841–51.
Skamagki G, King A, Duncan M, et al. A systematic review on workplace interventions to manage chronic musculoskeletal conditions. Physiother Res Int. 2018;23(4):e1738. https://doi.org/10.1002/pri.1738.
Hoosain M, de Klerk S, Burger M. Workplace-based rehabilitation of upper limb conditions: a systematic review. J Occup Rehabil. 2019;29(1):175–93. https://doi.org/10.1007/s10926-018-9777-7.
Pedersen MT, Andersen CH, Zebis MK, et al. Implementation of specific strength training among industrial laboratory technicians: long-term effects on back, neck and upper extremity pain. BMC Musculoskel Disord. 2013;14:287.
Zebis MK, Andersen LL, Pedersen MT, et al. Implementation of neck/shoulder exercises for pain relief among industrial workers: a randomized controlled trial. BMC Musculoskelet Disord. 2011;12:205.
Ris I, Sogaard K, Gram B, et al. Does a combination of physical training, specific exercises and pain education improve health-related quality of life in patients with chronic neck pain? A randomized control trial with a 4 – month follow up. Man Ther. 2016;26:132–40.
Andersen LL, Christensen KB, Holtermann A, et al. Effect of physical exercise interventions on musculoskeletal pain in all body regions among office workers: a one year randomized controlled trial. Man Ther. 2010;15:100–4.
Abraha I, Cherubini A, Cozzolino F, De Florio R, Luchetta ML, Rimland JM, Folletti I, Marchesi M, Germani A, Orso M, Eusebi P, Montedori A. Deviation from intention to treat analysis in randomised trials and treatment effect estimates: meta-epidemiological study. BMJ. 2015;350:h2445. https://doi.org/10.1136/bmj.h2445.
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trial. Ann Int Meed. 2010;152:726–33.
Calvert M, Kyte D, Mrcieca-Bebber R, et al. Guidelines for inclusion of patient-reported outcomes in clinical trial protocols. JAMA. 2018;319(5):483–94.
Matsudo S, Araújo T, Marsudo V, et al. Questionário internacional de atividade física (IPAQ): estudo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Fís Saúde. 2001;6(2):05–18.
Marim EA, Lafasse R, Okazaki VHA. Global lateral preference inventory (IPLAG). Braz J Motor Behav. 2011;6(3):14–23.
Hartrick GT, Kovan JP, Shapiro S. The numeric rating scale for clinical pain measurement: a ratio measure? Pain Prat. 2003;3(4):301–16.
Prentice WE, Voight ML. Techniques in Musculoskeletal Rehabilitation. 4th ed. São Paulo: Artmed; 2003.
Kapandji AI. Fisiologia Articular – Membros Superiores. 5th ed. Rio de Janeiro: Guanabara Koogan; 2000.
Edouard P, Codine P, Samozino P, et al. Reliability of shoulder rotators isokinetic strength imbalance measured using the Biodex dynamometer. J Sci Medic Sport. 2013;16(2):162–5. https://doi.org/10.1016/j.jsams.2012.01.007.
Peolsson A, Hedlund R, Oberg B. Intra- and inter-tester reliability and reference values for hand strength. J Rehab Med. 2001;33:36–41.
Silva NC, Pinola LN, Ricci FPFM, et al. Construct validity of the functional impairment test-hand and neck/shoulder and arm (FIT-HANSA) for workers with upper limb complaints of a tertiary hospital. Acta Fisiatr. 2020;27(3):182–9.
Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptom. Appl Ergon. 1987;18:233–7.
Balbi LL, Barbosa RI, Marcolino AM, et al. Validity, reliability and responsiveness of the Brazilian version of the patient specific functional scale (PSFS-Br) in upper limb lesions. Acta fisiatr. 2019;26(2):66–70.
Silva NC, Chaves TC, dos Santos JB, et al. Reliability, validity and responsiveness of Brazilian version of QuickDASH. Musculosk Sci Pract. 2020;48:102163.
Martinez MC, Latorre MRDO, Fischer FM. Validade e confiabilidade da versão brasileira do Índice de capacidade para o Trabalho. Ver Saúde Pública. 2009;43:525–32.
Walsh IAP, Corral S, Franco RN, et al. Capacidade para o trabalho em indivíduos com lesões musculoesqueléticas crônicas. Rev Bras Saúde Púb. 2004;38:149–56.
Moriguchi CS, Alem MER, Coury HJCG. Sobrecarga em trabalhadores da indústria avaliada por meio da escala de necessidade de descanso. Rev Bras Fisioter. 2011;15:154–9.
Cook C, Richardson JK, Braga L, et al. Cross-cultural adaptation and validation of the Brazilian Portuguese version of the neck disability index and neck pain and disability scale. Spine. 2006;31:1621–2.
Comper ML, Costa LOP, Padula RS. Quick exposure check (QEC): a cross cultural adaptation into Brazilian -Portuguese. Work. 2012;41:2056–9.
Valentim DP, Sato TO, Comper MLC, et al. Reliability, construct validity and interpretability of the Brazilian version of the rapid upper limb Assessemnt (RULA) and strain index (SI). Braz J Phys Ther. 2018;22:198–204.
Lamarão AM, Costa LCM, Comper MLC, et al. Translation, cross-cultural adaptation to Brazilian-Portuguese and reliability analysis of the instrument rapid entire body assessment-REBA. Braz J Phys Ther. 2014;18(3):211–7.
Sato T, Coury HG. Validação do Roteiro para Avaliação de Riscos Musculoesqueléticos (RARME) - Aplicação em situações ocupacionais industriais. Rev Bras Fisioter. 2005;9(3):355–63.
Douwes M, Kraker H. Development of a non-expert risk assessment method for hand-arm related tasks (HARM). Int J Industrial ergonomics. 2014;44:316–27.
Sonne M, Villalta DL, Andrews DM. Development and evaluation of an office ergonomic risk checklist: ROSA - rapid office strain assessment. Appl Erg. 2012;43:98–108.
Mayr S, Erdfelder E, Buchner A, et al. A short tutorial of GPower. Tutor Quant Methods Psychol. 2007;3:51–9.
Wang D, Baklai D. Clinical trials: a practical guide to design, analysis and reporting, 498 pages: Remedica; 2006.
Armijo-olivo S, Warren S, Fuentes J, et al. Clinical relevance vs. statistical significance: using neck outcomes in patients with temporomandibular disorders as an example. Man Ther. 2011;16:563–72.
Field A. Discovering statistics using IBM SPSS statistics. 4th ed. London: Sage; 2013.
De Vet HCW, Terwee CB, Mokkink LB, et al. Measurements in medicine. Cambridge: Cambridge University Press; 2011.
Portney LG. Foundations of clinical research: applications to evidence-based practice. 4th ed: FA Davis; 2020.
Dancey CP, Reidy J. Statistics without maths for psychology. 8th ed: Pearson; 2020.
Kamper SJ. Per-protocol, intention-to-treat, and complier average causal effects analyses in randomized controlled trials: linking evidence to practice. J Orthop Sports Phys Ther. 2021;51(6):314–5.
Luger T, Maher CG, Rieger MA, et al. Work-break schedules for preventing musculoskeletal disorders in workers. Cochrane Database Syst Rev. 2019;7(7):CD012886. https://doi.org/10.1002/14651858.
Kamper SJ. Generalizability: linking evidence to practice. J Orthop Sports Phys Ther. 2020;50(1):45–6.
Acknowledgements
We would like to thank the participants for their time taken to take part in the study. We would also like to thank the valuable support of the students: Karina Viana de Sousa on the exercise’s implementation images in the Additional file 1: Appendix 1 and Pedro Campos Ribeiro de Lima, Isabela Sales Bignotto and Elisa Pedigoni Mauro with data collection.
Funding
This work is supported by The São Paulo Research Foundation, FAPESP (Grant 2019/04078–0) and Foundation for Support to Teaching, Research and Assistance, Ribeirao Preto Medical School, University of Sao Paulo (FAEPA), both public foundations which several steps of standard procedures for the peer reviewer’s analysis for a research proposal grant. Both sources of funding are not involved in the design of the study, data collection, management analysis and interpretation of the data, nor in the preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
MCRF and FLRR conceived the study while NCS, FPFMR and VRC designed the study. The study protocol was drafted by ACRL, ERCL, LDSM, KAKS and revised by MEOM and JSS. All authors approved the final manuscript of this study protocol.
Authors’ information
The authors declare no potential conflict of interest regarding the research, authorship or publication of this article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study follows all ethical considerations set out in the Declaration of Helsinki and has received the approval from the Local Research Ethical Committee CAAE: 02658018.2.0000.5440. It was prospectively registered at www.ClinicalTrials.gov (NCT04047056). Written informed consent will be obtained from each participant. The findings of this study will be disseminated widely at national and international conferences, and will be published in peer-reviewed, scientific journals.
Consent for publication
All workers who voluntarily participate in the study will sign a written informed consent. Volunteers are aware of this publication and have clarified the importance of the study and publication of the manuscript. For Fig. 2 written consent for publication has been obtained to allow for the showing of individual faces.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
da Silva, N.C., Ricci, F.P.F.M., de Castro, V.R. et al. Effects of workplace upper extremity resistance exercises on function and symptoms of workers at a tertiary hospital: a randomized controlled trial protocol. BMC Musculoskelet Disord 23, 119 (2022). https://doi.org/10.1186/s12891-022-05059-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05059-5