Abstract
Background
In people with anterior cruciate ligament (ACL) injury, high self-efficacy facilitates recovery, indicated by improved muscle function, reduced knee symptoms and increased physical activity. Impact of treatment on future self-efficacy is however not well investigated. The aims of the study were to 1) investigate knee-related self-efficacy 6 years after acute ACL injury in patients treated with exercise therapy alone or in combination with either early or the option of delayed ACL reconstruction (ACLR), and 2) to investigate associations between single-leg physical performance at various time points after ACL injury and knee self-efficacy at 6 years after injury.
Methods
Participants (n = 121) originated from the KANON-study (ISRCTN84752559), a treatment RCT including active adults with acute ACL injury treated with structured exercise therapy combined with early or the option of delayed ACLR. In this ancillary study, participants with knee self-efficacy data at 6 years (n = 89) were analyzed as treated; exercise therapy alone (n = 20), exercise therapy plus early ACLR (n = 46), and exercise therapy plus delayed ACLR (n = 23). The participants performed physical performance tests (hop, strength and balance) at the end the of exercise therapy (mean 10 (SD 6) months), and at 5 years, and rated their knee self-efficacy using Knee Self-Efficacy Scale (K-SES) questionnaire (0 to 10, worst to best) at 6 years.
Results
Median K-SES score for the total group (n = 89) was 7.8 (IQR 5.9–9.0). There were no differences between treatment groups in K-SES scores at 6 years nor in physical performance at any time point (p ≥ 0.097). Worse knee flexion strength LSI (rsp = 0.341, p = 0.042) at the end of the exercise therapy, and worse LSI for single-leg hop test (rsp = 0.310, p = 0.005) at the end of the exercise therapy and at 5 years, correlated moderately with worse knee-related self-efficacy at 6 years. Low associations were observed between the remaining physical performance tests and K-SES scores (rsp ≤ 0.265, p ≥ 0.045).
Conclusion
Knee-related self-efficacy at 6 years after ACL injury did not differ between those treated with ACLR, performed early or as a delayed procedure, or exercise therapy alone. Good physical performance at the end of the exercise therapy, and at 5 years, appears to have a positive, yet small, impact on future knee-related self-efficacy.
Similar content being viewed by others
Background
In recent years, there has been increased focus on psychosocial factors and their association to recovery and return to sport (RTS) after anterior cruciate ligament (ACL) injury [1, 2]. The expectations of good recovery of knee function and RTS are high among individuals with ACL injury [3, 4]. However, despite treatment, with or without surgical reconstruction, impairments in patient-reported outcome measures (PROMs) [5, 6] and in physical performance often persist [7]. Only 81% return to any sport and 55% return to competitive level sports following an ACL injury or anterior cruciate ligament reconstruction (ACLR) [8].
The way in which a person reacts to an sport injury, i.e., the psychosocial response, includes cognitive, affective and behavioral aspects [9]. Negative psychological responses following an ACL injury or ACLR include pain and anxiety response, depression, and loss of athletic identity [10,11,12]. Positive psychological responses, on the other hand, include high motivation, high confidence and low fear of reinjury [1, 2] in addition to high self-efficacy [13]. These positive psychological responses interact both with each other and with the outcomes of the treatment [9]. In those with ACL injury, studies show that positive psychological responses, including high self-efficacy (cognitive response), facilitate recovery, in terms of improved muscle function, reduced knee symptoms and increased physical activity and that these are associated with higher return to pre-injury level of sports [1, 2]. However, we are not aware of any studies with the reverse design that evaluate whether modifiable treatment factors influence future self-efficacy.
Self-efficacy has been defined as the perception of one’s capability to perform a specific task, irrespective of whether one actually does or can perform it [14]. The level of self-efficacy can influence one’s initiative for action, level of effort and resilience to setbacks [14]. Previous experience of failure and success, including one’s own and through observation of others, can conversely effect one’s self-efficacy. [14] Commonly used measures evaluating knee-related self-efficacy after ACL injury, are the ACL-Return to Sports after Injury scale (ACL-RSI) [15], the Modified Self-Efficacy for Rehabilitation Outcome Scale (SER) [16], knee confidence with the single item Q3 from the Knee injury and Osteoarthritis Outcome Score subscale quality of life (KOOS item Q3) [17], and the Knee Self-Efficacy Scale (K-SES).
Low knee-related self-efficacy, in terms of low K-SES scores, has been reported in the early stages of treatment after ACL injury or reconstruction but is suggested to improve during the course of rehabilitation [18, 19]. One reason for this improvement in knee-related self-efficacy could be associated with decreased knee-related symptoms and the improvements in physical performance that are achieved during rehabilitation, however, to our knowledge this has not been studied. Another potential contributing factor for achieving high self-efficacy may be the treatment strategy, i.e., exercise therapy plus ACLR or exercise therapy alone. Thomeé et al. [20] investigated the role of knee-related self-efficacy in ACL-injured patients, undergoing exercise therapy with or without ACLR, and concluded that self-efficacy increased during the first year after injury and ACLR. The influence of self-reported knee function, age, gender and physical activity on the patients’ perceived knee self-efficacy was investigated [20]. However, the possible impact of different treatment strategies on future knee-related self-efficacy following ACL injury has not been reported.
Therefore, the aims of this study were to 1) report knee-related self-efficacy 6 years after acute ACL injury in patients treated with exercise therapy alone or in combination with either early or the option of delayed ACLR, and to 2) investigate associations between objectively measured single-leg physical performance at various time points after ACL injury and self-reported knee self-efficacy at 6 years after injury.
Methods
Participants
The participants in the present study originate from the Knee Anterior Cruciate Ligament, Nonsurgical versus Surgical Treatment (KANON) study (ISRCTN84752559) [5], a randomized controlled trial including 121 physically active adults with an acute ACL injury to a previously un-injured knee. The KANON-trial compared two treatments strategies: structured exercise therapy combined with an early ACLR (n = 62) or exercise therapy with the option of a delayed ACLR performed if needed (n = 59) [5]. The exercise therapy program was consistent with consensus in the literature [21]. At 2 and 5 years, there were no differences between the groups as randomized or as treated in knee-related outcomes, health status, return to preinjury activity level [5], or knee osteoarthritis (OA) frequency [6].
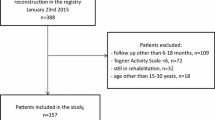
In this ancillary study all participants with available results on the K-SES (n = 89, Table 1) were included and analyzed according to treatment actually received: exercise therapy alone (ACL-D, n = 20), exercise therapy plus early reconstruction (ACL-R n = 46), and exercise therapy plus delayed reconstruction (ACL-X n = 23). Of the included participants, 62 performed the physical performance tests at the end of the exercise therapy period (mean 10 (SD 6) months after injury) [22] and 85 participants performed the physical performance test at 5 years after ACL injury; knee related self-efficacy was self-reported by mail at 6 years (Fig. 1). There were no differences in the physical performance tests between the groups as treated (ACL-D, ACL-R, ACL-X). The KANON study was approved by the Research Ethics Committee at Lund University, Sweden (LU 535–01) and all participants gave their written informed consent.
Flow chart of participants and follow-ups with physical performance tests and the Knee Self-Efficacy Scale (K-SES). †Long-distance relocation or transferal to a physical therapist (PT) not involved in the study. ††Pregnancy (n = 1), disc herniation (n = 1), advised against performing test by PT (n = 3), missing test protocols (n = 3). Participants with K-SES data and physical performance test data were included in the analyses
Physical performance
Physical performance was assessed at two time points; at the end of the exercise therapy and at 5 years follow-up. Seven single-leg physical performance tests, as described in Ericsson et al. [22] were assessed at the end of the exercise therapy when all goals of the exercise protocol were considered to be met [22]. The tests included the single-leg hop for distance, vertical hop, square hop, single-leg rise, single-leg balance test, knee extension strength, and knee flexion strength (Table 2). At mean 5 (SD 0.5) years after injury, performance was only assessed by the single-leg hop test for distance. The change in single-leg hop performance between the end of the exercise therapy and at 5 years was also calculated.
The Limb Symmetry Index (LSI) was used for all analyses of physical performance. The LSI was calculated by dividing the result for the injured leg by that of the uninjured leg and multiplying by 100 [23].
Thirty-four participants (9 women, 25 men) did not complete the physical performance tests at the end of the exercise therapy (Fig. 1), and, were excluded from the correlation analyses. These participants did not differ from those who completed the physical performance tests with respect to age (p = 0.41), gender (p = 0.99), BMI (p = 0.24), activity level (p = 0.96), treatment randomized (p = 0.30), or number of supervised exercise therapy sessions (p = 0.32). Depending on data normality and type, the χ2 test or the Mann-Whitney test were used for the between-group comparisons, as appropriate.
Knee-related self-efficacy
Perceived knee-related self-efficacy was self-reported at mean 6 (SD 1) years after injury using the K-SES. K-SES consists of four sections; A – daily activities, B – sports and leisure activities, C – knee function tasks and D – future knee function. The full K-SES includes 22 items and the individual rates the certainty about the capability of performing an activity on an 11-point Likert scale, ranging from 0 (not at all certain) to 10 (very certain). Item scores are summarized and divided by the number of items for each section (A-D), yielding a total K-SES score ranging from 0 to 10 [24]. Two subscores, K-SES Present and Future, are also calculated each with a range of 0 to 10 [24]. In sections A through C, the participants report their perception about their present capability of performing knee-related tasks, yielding the subscore K-SES Present. In section D, they report their perception about their future knee function capability, such as return to preinjury level sport and fear of reinjury (plus decreasing knee function if undergoing ACLR), yielding the subscore K-SES Future. [24] The K-SES has been assessed for the following measurement properties; internal consistency, test-retest reliability, face validity, content validity and construct validity [20, 24]. The K-SES is reliable and valid for measuring perceived self-efficacy in patients with an ACL injury [24].
Statistical analysis
Data were analyzed on a post-hoc as-treated basis. The one-way ANOVA test was used for the comparison of age at baseline between the treatment groups, and, the Kruskal-Wallis test was used for between-group comparisons of the BMI, the performance tests and the K-SES scores in the three treatment groups. Spearman’s, and partial Spearman’s, rank-order correlation analyses were used to assess associations between physical performance and K-SES, controlling for age, gender and treatment. Correlation coefficients thresholds suggested by Cohen [25] were used as follows; ≥ 0.10 to 0.29 denote low association, ≥ 0.30 to 0.49 moderate association and coefficients ≥0.50 large association. P-values less than or equal to 0.05 were considered statistically significant. Statistical analyses where performed using IBM SPSS for Windows, version 23.0 (IBM corp., Armonk, NY, USA).
Results
The median K-SES scores at 6 years for all participants (n = 89) were K-SES 7.8 (IQR 5.9–9.0), K-SES present 8.7 (IQR 6.8–9.6) and K-SES future 4.8 (IQR 2.5–7.5). There were no differences between the three treatment groups in K-SES scores 6 years after injury (p ≥ 0.501, Fig. 2).
Distribution of Knee Self-Efficacy (K-SES) scores in the different treatment groups (total n = 89) at 6 years after injury. The bar in the box represents the median, the box represents the interquartile range (IQR) and the whiskers extend to the minimum or the maximum values within 1.5 IQR from the lower and the higher edges of the box. Circles represent cases with values between 1.5 and 3 IQR from the lower edge of the box
There were no differences between treatment groups in single-leg physical performance at any time point (p ≥ 0.097, Table 2). Therefore, the correlation analyses were performed with data from all patients combined. Worse LSI for knee flexion strength (rsp = 0.341, p = 0.042) at the end of the exercise therapy, as well as worse LSI on the single-leg hop test at 5 years (rsp = 0.310, p = 0.005), correlated moderately with worse knee-related self-efficacy at 6 years after injury (Table 3). Low associations were observed between the remaining physical performance tests at the end of the exercise therapy and K-SES, ranging from rsp = 0.148 (p = 0.264) for the LSI for the single-leg hop test to rsp = 0.265 (p = 0.045) for the LSI in the square hop test.
Discussion
Knee-related self-efficacy at 6 years after acute ACL injury was not associated with treatment strategy, in terms of exercise therapy alone or combined with early or optional delayed ACLR. Worse LSI in knee flexion strength at the end of the exercise therapy and worse LSI in the single-leg hop test for distance, at 5 years, were moderately associated with worse knee-related self-efficacy at 6 years.
The K-SES scores (median 7.4–8.2) for our cohort were comparable, or better, than K-SES scores previously reported from other Swedish cohorts: mean 6.8 and 7.6 at 12 months after ACL injury and ACLR, respectively [20]; mean 7.3 at 12 months after ACL injury or ACLR [26]; and median 6.7 at 1–12 month after ACL injury and 3–12 months after ACLR [24].
In a previous study, similar levels of K-SES scores (mean 6.9–8.3), have been shown to be associated with greater likelihood of satisfaction with knee function, at mean 3 years after ACLR [27]. In the present study, the K-SES Present scores (perception about one’s present capability of performing knee-related tasks) can be considered to be high, whereas the K-SES Future scores (perception about one’s return to preinjury level sports and fear of reinjury plus decreasing knee function if undergoing ACLR) were remarkably low, for all three treatment groups. In contrast, previous studies report that the K-SES Future scores correspond to or are higher than the K-SES Present scores [18, 20, 24, 26]. One explanation for this could be that previous studies investigated knee-related self-efficacy within one month after ACL injury or before ACLR and up to 1 year after injury or ACLR [18, 20, 24, 26], whereas in the present study we assessed knee-related self-efficacy at 6 years after ACL injury or ACLR. The K-SES Future score refers to perceptions about return to preinjury level sports, fear of reinjury and decreasing knee function. Previous reports have shown, that less than 50% return to sports, at preinjury or competitive level, at 2–7 years after ACLR [28]. In the KANON-trial, only about 20% of the participants were active at their preinjury activity level or higher at 5 years after structured rehabilitation with or without the addition of ACLR [6]. Thus, it may be assumed that no more than 20% of participants in the present cohort were active at their preinjury activity level at 6 years. This may be reflected by the low K-SES Future scores presented in the present study. Fear of reinjury, despite the perception of good knee function, has been shown to be the most common hindrance for return to sports [29, 30]. This may explain the discrepancy between the high K-SES Present (perception of good knee function capability) and the low K-SES Future (uncertainty about return to preinjury level sports and reinjury) scores. In addition, the expectations and motivation of return to preinjury level sports and the perception of acceptable knee function may change over time. High, and potentially unrealistic, expectations of return to sports and knee function have been reported by patients prior to surgery for an ACL or a meniscus injury [3, 4, 31]. As in the current study, lower, and perhaps more realistic, expectations may be expressed several years later. Therefore, other potentially relevant explanations for the low K-SES Future scores may be natural changes, including increasing age or changes in social commitments. A longitudinal study is required to further investigate these potential explanations for change in future knee self-efficacy in individuals after ACL injury.
The lack of differences in K-SES scores between groups as treated (ACL-D, ACL-R and ACL-X) is in line with previous observations for various outcomes of the KANON-trial, in terms of self-reported outcomes [5] and osteoarthritis (OA) [5, 6] at 2 or 5 years, and muscle function [7] evaluated at 3 years after ACL injury. All participants followed the same exercise therapy protocol regardless of treatment strategy. The as treated group, receiving exercise therapy alone, progressed faster and needed fewer exercise sessions than the two groups who had early or delayed ACLR in addition to exercise therapy. The exercise program was goal-based and progression to a more strenuous level was allowed when the goals for range of motion, muscle function, and functional performance, respectively, were met [5]. As a result, the exercise program was based on functional goals rather than a pre-determined number of sessions. This approach was chosen to ensure that all treatment groups would achieve a similar and good level of physical function. Thus, the extensive exercise therapy program, rather than the early or the optional delayed ACLR, may be the common factor explaining our findings of similar K-SES scores across all treatment groups.
To our knowledge, our study is the first to investigate the influence of physical performance on knee-related self-efficacy after ACL injury. In contrast, previous studies have the reverse design, focusing on the influence of psychological responses on physical function and performance [32]. Higher knee-related self-efficacy, in terms of higher K-SES score, before ACLR has been reported to be associated with good physical performance (LSI ≥ 90 in single-leg hop and muscle power tests) and improved self-reported knee function (KOOS) at 1-year follow-up after ACLR [33]. Our results indicate that greater (better) LSI for knee flexion strength at the end of exercise therapy after ACL injury, correlated with better knee-related self-efficacy (higher K-SES scores) at 6 years. Although these associations were only moderate, our findings are supported by results from previous longitudinal studies, indicating that symmetry between legs in single-leg physical performance after exercise therapy, or within one year after ACL injury or ACLR, is one contributing factor for good future self-reported outcomes, such as, self-reported knee function and high return to pre-injury sports [34,35,36].
We observed that worse LSI in single-leg physical performance at 5 years correlated moderately with worse knee-related self-efficacy at 6 years. Longitudinal results have previously shown that worse single-leg physical performance after ACL injury or ACLR was associated with worse knee confidence, a construct similar to knee-related self-efficacy. Lower (worse) LSI for single-leg hop performance at 3 years after ACL injury has been shown to be associated with worse knee confidence (KOOS item Q3) at 5 years [37]. These moderate associations between single-leg physical performance and knee confidence found in a previous study [37] and in our present longitudinal study, suggest that good single-leg physical performance is one factor contributing to better psychological outcome after ACL injury or ACLR. Further studies are required to evaluate the relative contribution of physical performance, as well as other factors, that may play a role for the psychological response after injury.
The level of knee-related self-efficacy is important after ACL injury and surgery as it can influence one’s initiative for action, level of effort and resilience to setbacks. Surgical treatment in addition to exercise therapy after ACL injury does not appear to influence later knee-related self-efficacy. The findings of the current study show that after ACL injury, patients may benefit from training that targets symmetry between legs, specifically, in knee flexion muscle strength and in single-leg hop performance.
The main strength of the current study is that data originates from the KANON-trial, a high quality RCT. Another strength is that there were no differences between participants and non-participants in baseline characteristics. There are some limitations to the present ancillary study. The completion rates for the physical performance tests at the end of the exercise therapy were between 33% and 70% and only 74% of the participants of the KANON-trial completed the K-SES questionnaire at 6 years after injury. These low completion rates may be explained by equipment problems at the test sites, or participants declining to perform test at the end of the exercise therapy, and that the K-SES was sent out by mail instead of being filled out at a clinical visit at 6 years. However, the majority of the participants included in this study completed the physical performance test at 5 years (96%). Additional limitations are that several testers assessed the physical performance tests at the end of the exercise therapy [22]. However, all assessors were experienced and similar written instructions were used at all centers and for all tests. The use of LSI for the analyses of the physical performance tests may be considered a limitation. Despite the LSI being a common measure, it may misrepresent the performance of the injured leg [38]. Bilateral deficiencies in hop tests have been reported in individuals after ACLR [39]. Since the LSI represents the level of limb symmetry, a high (good) LSI may be the result of either a good, or poor, performance of both legs. Lastly, K-SES was only assessed at 6 years after injury, not allowing adjustment for baseline scores or analyses of change in K-SES scores.
Conclusions
Knee-related self-efficacy at 6 years after an acute ACL injury did not differ between patients treated with ACL reconstruction, performed early or as a delayed procedure, or those treated with exercise therapy alone. At 6 years after injury, the self-efficacy for present knee function capability (K-SES subscore present) was higher than the self-efficacy for return to preinjury level sport and not being reinjured (K-SES subscore Future). Worse single-leg physical performance at the end of the exercise therapy period, and at 5 years, was weakly to moderately associated with worse knee self-efficacy at 6 years. Targeted training to improve the symmetry between legs in knee flexion muscle strength and in the single-leg hop for distance may have a positive, yet small, long-term impact on knee-related self-efficacy after ACL injury.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ACL-D:
-
exercise therapy alone
- ACLR:
-
Anterior cruciate ligament reconstruction
- ACL-R:
-
exercise therapy plus early reconstruction
- ACL-RSI:
-
the ACL-Return to Sports after Injury scale
- ACL-X:
-
exercise therapy plus delayed reconstruction
- BMI:
-
Body mass index
- IQR:
-
Inter-quartile range
- KANON:
-
the Knee Anterior Cruciate Ligament, Nonsurgical versus Surgical Treatment
- KOOS item Q3:
-
the single item Q3 from the Knee injury and Osteoarthritis Outcome Score subscale quality of life
- KOOS:
-
the Knee injury and Osteoarthritis Outcome Score
- K-SES:
-
the Knee Self-Efficacy Scale
- LSI:
-
Limb symmetry index
- MRI:
-
Magnetic resonance imaging
- OA:
-
Osteoarthritis
- PROMs:
-
in patient-reported outcome measures
- PT:
-
Physical therapist
- rs :
-
Spearman’s rank-order correlations
- rsp :
-
Spearman’s rank-order partial correlations
- RTS:
-
Return to sports
- SD:
-
Standard deviation
- SER:
-
the Modified Self-Efficacy for Rehabilitation Outcome Scale
References
Ardern CL, Taylor NF, Feller JA, Webster KE. A systematic review of the psychological factors associated with returning to sport following injury. Br J Sports Med. 2013;47(17):1120–6.
te Wierike SCM, van der Sluis A, van den Akker-Scheek I, Elferink-Gemser MT, Visscher C. Psychosocial factors influencing the recovery of athletes with anterior cruciate ligament injury: a systematic review. Scand J Med Sci Sports. 2013;23(5):527–40.
Feucht MJ, Cotic M, Saier T, Minzlaff P, Plath JE, Imhoff AB, Hinterwimmer S. Patient expectations of primary and revision anterior cruciate ligament reconstruction. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA. 2016;24(1):201–7.
Sonesson S, Kvist J, Ardern C, Osterberg A, Silbernagel KG. Psychological factors are important to return to pre-injury sport activity after anterior cruciate ligament reconstruction: expect and motivate to satisfy. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA. 2017;25(5):1375–84.
Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363(4):331–42.
Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. BMJ (Clinical research ed). 2013;346:f232.
Ageberg E, Thomee R, Neeter C, Silbernagel KG, Roos EM. Muscle strength and functional performance in patients with anterior cruciate ligament injury treated with training and surgical reconstruction or training only: a two to five-year followup. Arthritis Rheum. 2008;59(12):1773–9.
Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–52.
Wiese-bjornstal DM, Smith AM, Shaffer SM, Morrey MA. An integrated model of response to sport injury: psychological and sociological dynamics. Journal of Applied Sport Psychology. 1998;10(1):46–69.
Tripp DA, Stanish WD, Coady C, Reardon G. The subjective pain experience of athletes following anterior cruciate ligament surgery. Psychol Sport Exerc. 2004;5(3):339–54.
Podlog L, Dimmock J, Miller J. A review of return to sport concerns following injury rehabilitation: practitioner strategies for enhancing recovery outcomes. Physical therapy in sport: official journal of the Association of Chartered Physiotherapists in Sports Med. 2011;12(1):36–42.
Garcia GH, Wu HH, Park MJ, Tjoumakaris FP, Tucker BS, JDt K, Sennett BJ. Depression symptomatology and anterior cruciate ligament injury: incidence and effect on functional outcome--a prospective cohort study. Am J Sports Med. 2016;44(3):572–9.
Hamrin Senorski E, Samuelsson K, Thomee C, Beischer S, Karlsson J, Thomee R. Return to knee-strenuous sport after anterior cruciate ligament reconstruction: a report from a rehabilitation outcome registry of patient characteristics. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA. 2017;25(5):1364–74.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215.
Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Physical therapy in sport: official journal of the Association of Chartered Physiotherapists in Sports Med. 2008;9(1):9–15.
Chmielewski TL, Zeppieri G, Jr., Lentz TA, Tillman SM, Moser MW, Indelicato PA, George SZ: Longitudinal changes in psychosocial factors and their association with knee pain and function after anterior cruciate ligament reconstruction. Phys Ther 2011, 91(9):1355–1366.
Ageberg E, Roos EM. The association between knee confidence and muscle power, hop performance, and postural orientation in people with anterior cruciate ligament injury. The Journal of orthopaedic and sports physical therapy. 2016:1–16.
Thomee P, Wahrborg P, Borjesson M, Thomee R, Eriksson BI, Karlsson J. A randomized, controlled study of a rehabilitation model to improve knee-function self-efficacy with ACL injury. J Sport Rehabil. 2010;19(2):200–13.
Chmielewski TL, George SZ, Tillman SM, Moser MW, Lentz TA, Indelicato PA, Trumble TN, Shuster JJ, Cicuttini FM, Leeuwenburgh C. Low- versus high-intensity plyometric exercise during rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(3):609–17.
Thomee P, Wahrborg P, Borjesson M, Thomee R, Eriksson BI, Karlsson J. Self-efficacy, symptoms and physical activity in patients with an anterior cruciate ligament injury: a prospective study. Scand J Med Sci Sports. 2007;17(3):238–45.
Arna Risberg M, Lewek M, Snyder-Mackler L. A systematic review of evidence for anterior cruciate ligament rehabilitation: how much and what type? Physical Therapy in Sport. 2004;5(3):125–45.
Ericsson YB, Roos EM, Frobell RB. Lower extremity performance following ACL rehabilitation in the KANON-trial: impact of reconstruction and predictive value at 2 and 5 years. Br J Sports Med. 2013;47(15):980–5.
Engelen-van Melick N, van Cingel RE, Tijssen MP, Nijhuis-van der Sanden MW. Assessment of functional performance after anterior cruciate ligament reconstruction: a systematic review of measurement procedures. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA. 2013;21(4):869–79.
Thomee P, Wahrborg P, Borjesson M, Thomee R, Eriksson BI, Karlsson J. A new instrument for measuring self-efficacy in patients with an anterior cruciate ligament injury. Scand J Med Sci Sports. 2006;16(3):181–7.
Cohen J. Statistical power analysis for the behavioral sciences, 2nd ed. edn. New Jersey: Lawrence Erlbaum Associates, Inc; 1988.
Thomee P, Wahrborg P, Borjesson M, Thomee R, Eriksson BI, Karlsson J. Determinants of self-efficacy in the rehabilitation of patients with anterior cruciate ligament injury. Journal of rehabilitation medicine: official journal of the UEMS European Board of Physical and Rehabilitation Medicine. 2007;39(6):486–92.
Ardern CL, Osterberg A, Sonesson S, Gauffin H, Webster KE, Kvist J: Satisfaction With Knee Function After Primary Anterior Cruciate Ligament Reconstruction Is Associated With Self-Efficacy, Quality of Life, and Returning to the Preinjury Physical Activity. Arthroscopy : the journal of arthroscopic & related surgery: official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 2016, 32(8):1631–1638.e1633.
Ardern CL, Taylor NF, Feller JA, Webster KE. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40(1):41–8.
Ardern CL. Anterior cruciate ligament reconstruction-not exactly a one-way ticket back to the preinjury level: a review of contextual factors affecting return to sport after surgery. Sports health. 2015;7(3):224–30.
Langford JL, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2009;43(5):377–81.
Pihl K, Roos EM, Nissen N, JoRgensen U, Schjerning J, Thorlund JB. Over-optimistic patient expectations of recovery and leisure activities after arthroscopic meniscus surgery. Acta Orthop. 2016;87(6):615–21.
Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA. 2015;23(3):752–62.
Thomee P, Wahrborg P, Borjesson M, Thomee R, Eriksson BI, Karlsson J. Self-efficacy of knee function as a pre-operative predictor of outcome 1 year after anterior cruciate ligament reconstruction. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA. 2008;16(2):118–27.
Grindem H, Logerstedt D, Eitzen I, Moksnes H, Axe MJ, Snyder-Mackler L, Engebretsen L, Risberg MA. Single-legged hop tests as predictors of self-reported knee function in nonoperatively treated individuals with anterior cruciate ligament injury. Am J Sports Med. 2011;39(11):2347–54.
Logerstedt D, Grindem H, Lynch A, Eitzen I, Engebretsen L, Risberg MA, Axe MJ, Snyder-Mackler L. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. Am J Sports Med. 2012;40(10):2348–56.
Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med. 2015;43(4):848–56.
Flosadottir V, Roos EM, Ageberg E. Muscle function is associated with future patient-reported outcomes in young adults with ACL injury. BMJ Open Sport Exerc Med. 2016;2(1):e000154.
Wellsandt E, Failla MJ, Snyder-Mackler L. Limb symmetry indexes can overestimate knee function after anterior cruciate ligament injury. The Journal of orthopaedic and sports physical therapy. 2017;47(5):334–8.
Gokeler A, Welling W, Benjaminse A, Lemmink K, Seil R, Zaffagnini S. A critical analysis of limb symmetry indices of hop tests in athletes after anterior cruciate ligament reconstruction: a case control study. Orthopaedics & traumatology, surgery & research: OTSR. 2017;103(6):947–51.
Acknowledgements
Not applicable.
Funding
This research was funded by the Swedish Research Council (2009–1447), the Crafoord Foundation, the Swedish Rheumatism Association, the Swedish National Centre for Research in Sports and the Faculty of Medicine of Lund University. The original KANON study, from which the patients were included, was additionally supported by the Faculty of Medicine of Lund University, Region Skåne, Sweden, Pfizer Global Research, the Swedish Research Council, the Swedish National Centre for Research in Sports, the Swedish Rheumatism Association, Thelma Zoegas Fund, and the Stig & Ragna Gorthon Research Fund.
Availability of data and materials
The data that support the findings of this study is available from the KANON steering committee but restrictions apply to the availability of these data, which was used with permission for the current study. The data is not publicly available. Data is however available upon reasonable request and with permission of the KANON steering committee.
Author information
Authors and Affiliations
Contributions
VF, EA and RF contributed to the study design. RF and EMR were in charge of data collection. VF was responsible for the analysis and interpretation of the data, and wrote the first draft of the manuscript. EA contributed in analysis and interpretation of data, contributed in writing the manuscript and provided feedback on drafts of this manuscript. RF and EMR contributed in interpretation of data and critically revised the manuscript for important intellectual content. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research Ethics Committee at Lund University (LU 535–01). All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Flosadottir, V., Frobell, R., Roos, E.M. et al. Impact of treatment strategy and physical performance on future knee-related self-efficacy in individuals with ACL injury. BMC Musculoskelet Disord 19, 50 (2018). https://doi.org/10.1186/s12891-018-1973-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-018-1973-2