Abstract
Background
Consistent reference data used for anatomic posterior cruciate ligament (PCL) reconstruction is not well defined. Quantitative guidelines defining the location of PCL attachment would aid in performing anatomic PCL reconstruction. The purpose was to characterize anatomic parameters of the PCL tibial attachment based on magnetic resonance imaging (MRI) in a large population of adult knees.
Methods
The PCL tibial attachment site was examined in 736 adult knees with an intact PCL using 3.0-T proton density–weighted sagittal MRI. The outcomes measured were the anterior-posterior diameter (APD) of the tibial plateau; angle between the tibial plateau and the posterior tibial ‘shelf’ (the slope where the PCL tibial attachment site was) (PTS); length of the PTS; proximal, central, and distal PCL attachment positions as well as the width of the PCL attachment site; and vertical dimension of the PCL attachment site inferior from the tibial plateau.
Results
The average APD of the tibia plateau was 33.6 ± 3.5 mm, yielding significant differences between males (35.5 ± 3.0 mm) and females (31.6 ± 2.7 mm), P <.05, and there was a significantly decreasing trend with increasing age in males (P <.05). Mean angle between the tibial plateau and the PTS was 122.4° ± 8.1°, and subgroup analysis showed that the young group had a differently smaller angle (120.9° ± 7.5°) than the middle-aged (123.7° ± 8.2°) and the old (123.4° ± 7.7°) in males population, while there were no significant differences between sexes (P >.05). The proximal, central positions and width of the PCL attachment site were 13.4 ± 3.0 mm, 17.8 ± 3.0 mm and 9.6 ± 2.4 mm along the PTS, with significant differences between males and females (P <.05), and accounted for 60.0 % ± 9.1 %, 80.0 % ± 4.6 % and 43.3 % ± 9.7 % of the PTS respectively, with no significant differences between sexes and among age groups (all P >.05).
Conclusions
This study provides reference data of the tibial PCL attachment based on MRI in the sagittal orientation. In analysis of retrospective data from a large population of adult patients, the quantitative values can be used as references to define the inserted angle and depth of the drill guide, and the exact position and size of the tibial PCL tunnel for performing arthroscopic anatomic PCL reconstruction.
Similar content being viewed by others
Background
The posterior cruciate ligament (PCL) is composed of two bundles (the anterolateral bundle and the posteromedial bundle), and is regarded as the central pivot point of the knee and acts as an essential role in joint stability of knee [1]. Biomechanical studies have indicated that the PCL contributes 95 % restraint to posterior translation of tibia [2]. The PCL injury is not as common as anterior cruciate ligament (ACL) injury in high-energy knee trauma. It has been reported that the incidence of PCL injury varies from 1 to 44 % in all knee ligament injuries [2, 3]. And PCL injury presents more frequently in trauma population (as high as 37 %) than that in athletic injury population [4, 5].
The surgical management arthroscopically has been increasingly recommended for PCL tears. Compared with the nonoperative treatment, PCL reconstruction is the preferred treatment for patients with severe or complex PCL injuries [2, 6]. The possible indications for PCL reconstruction include: an acute PCL tear in conjunction with a knee dislocation, or with an anteroposterior laxity ≥12 mm on the PCL stress radiograph, a complete PCL tear with a stress radiographic anteroposterior laxity ≥8 mm and combined with repairable meniscal tear, and a chronic PCL tear with a stress radiographic anteroposterior laxity ≥8 mm with functional limitations [7–13]. Additionally, anatomic PCL reconstruction, which needs to make the tunnels exactly at the attachments of the native PCL, has obtained better clinical outcomes than the nonanatomic reconstruction [14–16]. Currently, two widely used techniques are used to perform anatomic PCL reconstruction: the single-bundle PCL reconstruction and the double-bundle PCL reconstruction. Though several level-2 and −3 studies have quantified potential differences between the two techniques, their conclusions were controversial [8, 17–22].
Regardless of the single-bundle or double-bundle technique, sufficient knowledge of normal PCL anatomy is essential to ensure correct tunnel placement during anatomic PCL reconstruction. Several small sample cadaveric studies have investigated the anatomic characteristics of the anterolateral and posteromedial bundles of the PCL at the femoral attachments [7, 8, 23, 24]. However, few studies have described relevant data of the PCL at the tibial attachment. Therefore, the purpose of this study was to characterize anatomic parameters of the PCL tibial attachment based on MRI in a large population of adult knees. We hypothesized that it would provide some useful reference data to assist orthopaedic surgeons with intraoperative and postoperative assessments of correct tunnel placement during arthroscopic anatomic PCL reconstruction.
Methods
Patient selection
Ethics approval for this study was granted by the institutional review board of our hospital. The inclusion criteria were: (1). patients performed 3.0 Tesla knee MRI; (2). Time between June 2010 and April 2015; (3). patients’ age was not less than 18. We excluded the patients with skeletal dysplasia, a displaced fracture around knee, previous knee surgery, imaging evidence of degenerative joint disease, or knee abnormalities caused by any disease.
Magnetic resonance imaging
All the included patients were performed by 3.0 Tesla MRI according to the standard clinical knee MRI protocols (Siemens AG, Munich). All patients were scanned with coronal, sagittal and axial MR images (matrix: 512 × 512 or 256 × 256, FOV: maximum to 200 mm, slice thickness: 2.5–4 cm) /T1-weighted images (TR/TE = 400–750 msec / 17–30 msec), T2-weighted images (TR/TE = 1800–3500 msec / 60–100 msec) and a turbo spin-echo pulse sequence was used to obtain proton density-weighted images (TR/TE = 1800–3500 msec / 19–40 msec).
Quantitative anatomic measurements
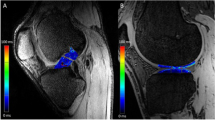
Quantitative anatomic measurements were performed digitally with RadiAnt DICOM Viewer (Medixant, Poznan, Poland) software. Measurements were taken on the T1-weighted sagittal MRI slice that provided the most inclusive view of the PCL tibial attachment. The relevant measurements of the PCL tibial attachment were performed (Fig. 1) referring to an earlier study focus on the measurements of anterior cruciate ligament (ACL) tibial attachment, by Frank et al. [25], including the APD of the tibial plateau, the angle between the tibial plateau and the posterior tibial ‘shelf’ (the slope where the PCL tibial attachment site was) (PTS) [26] (Fig. 2), the length of the PTS. The other data measured were the proximal, central and distal positions of the PCL tibial attachment, the width of the attachment site, and the vertical dimension of the PCL attachment site from the tibial plateau. The APD was measured from the anterior edge to the posterior edge of the tibia plateau. Similarly, the length of the PTS was from the proximal edge to the distal edge of the PTS. The angle was measured between two lines separately along the tibial plateau and the PTS. The proximal, central and distal positions as well as the dimater of the PCL tibial attachment were expressed as a value (mm) along the PTS as well as a percentage of the length of the PTS. As the distal border of the PCL attachment and the distal edge of the PTS was almost the same position on MR images, the same value was defined to the length of the PTS and the distance from the distal position of the attachment to the proximal edge of the PTS. Additionally, the vertical dimension of the PCL attachment site was measured inferior from the center of the PCL attachment perpendicularly to a line along the tibial plateau. Finally, all the measurements were analyzed for the cohort as a whole, as well as the comparison between males and females.
The relevant measurements of the PCL tibial attachment. a MRI showing measurement of the APD of the tibial plateau; b MRI showing measurement of the angle (α) between the tibial plateau and PTS (posterior tibial ‘shelf’); c MRI showing measurement of the distance from the proximal (L1) and central (L2) positions of the tibial PCL attachment to the tibial plateau, the width (L3) of the attachment, and the length of the PTS; d MRI showing measurement of the vertical dimension (L4) of the PCL central attachment site from the tibial plateau
Reliability analysis
To determine the interobserver reliability of the anatomic measurements, a single author (author 1) measured all parameters of the entire data set (n = 736), a second author (author 2) separately performed the measurements of 100 randomly selected cases from the entire data set, blinded to the values from author 1. For the intraobserver reliability, author 1 performed measurements of 40 randomly selected cases from the original data set on a second occasion 4 weeks apart. Throughout the reading session, clinical and demographic information as well as recorded measurements were blinded to the authors.
Statistical analysis
The data were tabulated on Microsoft Excel (v. 2007; Microsoft Corp, Redmond, WA, USA) and all statistical analyses were performed using SPSS software (v. 19; SPSS Inc, Chicago, IL, USA). As the continuous variables showed approximately normal distributions confirmed from review of frequency tables, results were described by mean ± standard deviation. Independent t test was used when anatomic parameters were compared between sex cohorts, while one-way ANOVA among age cohorts, with a significance level of P = .05. Two-way mixed effects model, single-measures intraclass correlation coefficients (ICCs) were calculated to assess inter- and intraobserver reliability.
Results
Totally, patients with 736 knees were included. Of which, 379 were males and 357 were females. The average age at the time of MRI was 39 ± 13.7 years (range, 18–75 years; males, 18–75 years; females, 18–73 years). There were 389 right knees and 347 left knees.
The detailed anatomic parameters of the PCL tibial attachment between males and females are reported in Table 1. The APD of the tibia plateau, absolute values of proximal, central positions and width of the PCL attachment site along the PTS, as well as PTS itself (also the distal position of the PCL tibial attachment), and mean vertical dimension of the PCL attachment site yielded significant differences between males and females, P <.05. The proximal, central positions and width of the PCL attachment when expressed as a percentage of the PTS and mean angle between the tibial plateau and the PTS showed no significant differences between sex cohorts, P >.05.
Measurements of the PCL’s tibial attachment in males, stratified into three age groups: the young (age, 18–30 years), the middle-aged (age, 31–50 years) and the old (age, 51–75 years) (Table 2). Mean APD of the tibal plateau, the angle between the tibial plateau and the PTS, the central position and width of the PCL attachment site along the PTS, as well as PTS itself, and the mean vertical dimension of the PCL attachment site showed significant differences between age groups, P <.05. While the proximal position of the PCL tibial attachment and percentage forms of the proximal, central positions and width of the PCL tibial attachment showed no significant differences among the three age groups, P >.05.
Data comparing anatomic parameters of the tibial PCL attachment among the three age groups in females are shown in Table 3. However, no significant differences were found in the three age groups, all P >.05.
Inter- and intraobserver reliability of tibial anatomic parameters based on ICCs was shown in Table 4. It was assessed to be of high inter- and intraobserver reliability for each measurement with interobserver ICCs ranged from 0.845 to 0.934 and intraobserver ICCs from 0.825 to 0.927.
Discussion
The most important finding of this study was the measurements of the APD and the tibial angle, as well as the determination of normal position of the tibial PCL attachment relative to the sagittal depth of the PTS based on MRI in a large population of adult knees. MRI have proven to be a very accurate technique for diagnosing PCL tears, especially for acute tears [27], with sensitivity values of 100 % and specificity values of 97 to 100 % [28–32]. With thorough MRI information of the PCL attachment, it would provide some reference data to assist orthopaedic surgeons with intraoperative and postoperative assessments of correct tunnel placement during arthroscopic anatomic PCL reconstruction.
On the sagittal plane of the MRI, our study showed that the APD of the tibial plateau was measured at ~34 mm, a little greater in males (~36 mm) than that in females (~32 mm). When stratified into three age groups, the value of the APD showed a significantly decreasing trend with age in males. The author doubts whether it was due to the degeneration changes of the cartilage as each individual goes through the aging process. It needs further research to clarify the issue. One recent study by Osti et al. [33] showed that the anteroposterior diameter of the tibial plateau was 57.43 ± 3.69 mm on radiographs with 20 nonpaired, fresh-frozen human cadaveric knee specimens, while Lorenz et al. [14] measured the anteroposterior diameter of the tibial plateau in true lateral radiography to be 61 mm based on 16 human cadaver specimens. The two studies both performed the largest anteroposterior diameter of the tibial plateau from the anterior edge of the tibia to the posterior tibial cortex. In another study by Frank et al. [25], the anteroposterior diameter of the tibia was 50 ± 4 mm, measured from the anterior edge of the tibia at the articular margin, proximal to the tibial tubercle, to the tibial origin of PCL. Differences with values of these studies were resulted from the fact that we used a different APD measurement technique in the present study. We measured the APD of the tibial plateau from the anterior edge to the posterior edge of the tibia plateau (as shown in Fig. 1). With this value, we can decide the insertion depth of the drill guide along the tibial pateau to reach the tibial PCL attachment, so it would be helpful to find the attachment of the PCL during arthroscopic PCL reconstruction.
The angle between the tibial plateau and the PTS was ~122°, with no significant differences between males and females. However, the young group had a differently smaller angle than the middle-aged and the old group. The explanation might be the appearance of slight knee hyperplasia in the middle-aged and old group. The measurements of the APD and the angle described above might be useful for defining the angle and depth of the drill guide during arthroscopic PCL reconstruction.
On the surface of the posterior tibial ‘shelf’, we performed measurements of the distance from the proximal, central as well as distal positions (also the length of the PTS) of the tibial PCL insertion to the tibial plateau and the width of the PCL attachment. The PCL attachment was measured to be 9.6 ± 2.4 mm on the MR images in our study, which is consistent with the findings from Osti et al. [33] by cadaveric knee specimens. They found that the superoinferior value of the PCL attachment was 9.58 ± 1.60 mm. Additionally, we found that there were statistically significant differences in all sites examined between males and females when the results were expressed in absolute values. However, no significant differences were found between the two groups when using the percentage of total depth of the PTS. It is likely due to differences of tibia size between males and females. The smaller size of tibia in females resulted in statistical differences when compared with males in absolute numbers. When the measurements were expressed as a percentage of tibial size, the outcomes were then standardized and the differences no longer presented. The results were similar with those from Frank et al. [25], who found statistically significant differences in tibial ACL attachment positions between males and females when the measurements were expressed in absolute values, and noted no differences when expressed as percentage of tibial APD. Therefore, a percentage measurement which allows for standardization of the positions, regardless of patient sex or size, might be more clinically significant and practical.
When stratified into three age groups in males, the values of the central, distal positions (also the length of the PTS) and width of the tibial PCL insertion along the PTS were greater in the young group than the middle-aged and the old. However, the value of the proximal position of the tibial PCL attachment showed no significant differences among age groups. Additionally, based on the 736 MR images, the values of the proximal, central positions and the width of the tibial PCL attachment accounted for 60.0 ± 9.1, 80.0 ± 4.6 and 43.3 ± 9.7 % of the PTS, respectively, regardless of sex or age. It means that the center of tibial PCL attachment locates ~ 80 % along the PTS distal from the posterior edge of the tibial plateau and covers ~43 % of the PTS. Therefore, for tibial tunnel placement when performing anatomic PCL reconstruction, we should strive for an accurate position centered at the midpoint of the normal tibial PCL attachment (~80 %), and pay more attention not to extending outside of this range (~43 %).
However, absolute values of the PCL attachment on the PTS might be more practical during arthroscopic PCL reconstruction. Based on our results in this study, when position the PCL attachment on the PTS, the drill guide should insert to a depth of ~18.9 mm in males, while ~16.7 mm in females. And the diameter of the tibial PCL tunnel should not be more than 10.1 and 9.1 mm respectively in males and females. These might be the most useful information for intraoperative and postoperative assessments of correct tunnel placement during arthroscopic anatomic PCL reconstruction. However, whether these data are clinically accurate and will lead to good clinical outcomes, more studies are still needed to validate the efficacy of our work.
Additionally, we performed the measurement of the width of PCL attachment in the sagittal orientation. Combining with the mediolateral value of the PCL attachment from Osti et al. [33], maybe we could determine the approximate position and size of tibial tunnel for PCL reconstruction. However, as the size and shape of the PCL attachment site are different from patient to patient [24, 34–36], and different shapes of the PCL attachment site may require different types of reconstruction to ensure proper attachment restoration, we should define the accurate outline of the PCL attachment site and perform the measurements in multiple orientations in future research. This can help to choose proper type and size of the graft and perform more individual and accurate PCL reconstruction [37].
The vertical dimension from the PCL attachment center to the tibial plateau was 15.0 ± 3.3 mm in this study. We did not search the similar measuring method and results about this parameter. However, several relevant studies about this parameter can still provide useful information for PCL reconstruction. Lorenz et al. [14] performed the perpendicular distance of the geometric insertion point to the tangent of the medial tibial plateau on lateral X-ray images, and the value was 8 mm on average, almost twice the size compared with the result in the present study. The differences might be due to the inclusion of tibial intercondylar eminence and the appearance of cartilage and soft tissue on MR images. In a quantitative analysis of the anterolateral and posteromedial bundles’ insertion areas, Johannsen et al. [23] measured the vertical dimension from the tibial PCL attachment center to a line intersecting the champagne glass drop-off ridge [38] perpendicular to the tibial axis line, and the value was 5.5 ± 1.7 mm. However, they did not report the vertical distance from the PCL center site to the tibial plateau. As a supplement to the results by Johannsen et al. [23], the present study provided more reference data for PCL reconstruction.
Limitations and future directions
We acknowledge that this study has some limitations. First, since it was a retrospective study, the weight and height of the patient could not be acquired, which prevented us from comparing males and females in equal size. Second, all our measurements were performed on the sagittal slice of the MRI, which cannot fully represent anatomy of the PCL tibial attachment as 3-dimensional reconstruction. However, routine preoperative 2-dimensional MRI is commonly performed to identify knee injury as 3-dimensional MRI of the knee is not feasible at most centers. Therefore, we performed the measurements of the reference parameters on 2-dimensional MRI. Third, the present study merely used MRI to determine the position of the tibial PCL attachment without relevant anatomic data. Therefore, there might be some small deviations between the estimated position of the tibial PCL attachment and the actual insertion. However, the degree of deviation would be limited for the current sensitivity and specificity of MRI, and the reliability analysis we conducted in the present study made the results more reliable. In addition, the patients included were from a single ethnicity-Chinese Han nationality, therefore, there might be some limitations when the reference data were used for other ethnicities. In future research, we should include patients from multiple ethnicities and record the weight and height of the patients, so that we could collect more comprehensive information for research when needed.
Conclusion
This study provides reference data of the tibial PCL attachment based on MRI in the sagittal orientation. In analysis of retrospective data from a large population of adult patients, the quantitative values can be used as references to define the inserted angle and depth of the drill guide, and the exact position and size of the tibial PCL tunnel for performing arthroscopic anatomic PCL reconstruction.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- APD:
-
Anterior-posterior diameter
- ICCs:
-
Intraclass correlation coefficients
- MRI:
-
Magnetic resonance imaging
- PCL:
-
Posterior cruciate ligament
- PTS:
-
Posterior tibial ‘shelf’
References
Fanelli GC, Beck JD, Edson CJ. Current concepts review: the posterior cruciate ligament. J Knee Surg. 2010;23(2):61–72.
Orakzai SH, Egan CM, Eustace S, Kenny P, O’Flanagan SJ, Keogh P. Correlation of intra-articular osseous measurements with posterior cruciate ligament length on MRI scans. Br J Radiol. 2010;83(985):23–7.
Shelbourne KD, Davis TJ, Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries. A prospective study. Am J Sports Med. 1999;27(3):276–83.
Wind Jr WM, Bergfeld JA, Parker RD. Evaluation and treatment of posterior cruciate ligament injuries: revisited. Am J Sports Med. 2004;32(7):1765–75.
Harner CD, Hoher J. Evaluation and treatment of posterior cruciate ligament injuries. Am J Sports Med. 1998;26(3):471–82.
Årøen A, Sivertsen EA, Owesen C, Engebretsen L, Granan LP. An isolated rupture of the posterior cruciate ligament results in reduced preoperative knee function in comparison with an anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2013;21(5):1017–22.
Anderson CJ, Ziegler CG, Wijdicks CA, Engebretsen L, LaPrade RF. Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament. J Bone Joint Surg Am. 2012;94(21):1936–45.
LaPrade CM, Civitarese DM, Rasmussen MT, LaPrade RF. Emerging updates on the posterior cruciate ligament: a review of the current literature. Am J Sports Med. 2015;43(12):3077–92.
Mariani PP, Margheritini F, Christel P, Bellelli A. Evaluation of posterior cruciate ligament healing: a study using magnetic resonance imaging and stress radiography. Arthroscopy. 2005;21(11):1354–61.
Montgomery SR, Johnson JS, McAllister DR, Petrigliano FA. Surgical management of PCL injuries: indications, techniques, and outcomes. Curr Rev Musculoskelet Med. 2013;6(2):115–23.
Race A, Amis AA. PCL reconstruction. In vitro biomechanical comparison of ‘isometric’ versus single and double-bundled ‘anatomic’ grafts. J Bone Joint Surg (Br). 1998;80(1):173–9.
Schulz MS, Steenlage ES, Russe K, Strobel MJ. Distribution of posterior tibial displacement in knees with posterior cruciate ligament tears. J Bone Joint Surg Am. 2007;89(2):332–8.
Sekiya JK, Whiddon DR, Zehms CT, Miller MD. A clinically relevant assessment of posterior cruciate ligament and posterolateral corner injuries. Evaluation of isolated and combined deficiency. J Bone Joint Surg Am. 2008;90(8):1621–7.
Lorenz S, Elser F, Brucker PU, Obst T, Imhoff AB. Radiological evaluation of the anterolateral and posteromedial bundle insertion sites of the posterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2009;17(6):683–90.
Kim YM, Lee CA, Matava MJ. Clinical results of arthroscopic single-bundle transtibial posterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2011;39(2):425–34.
McGuire DA, Hendricks SD. Comparison of anatomic versus nonanatomic placement of femoral tunnels in Achilles double-bundle posterior cruciate ligament reconstruction. Arthroscopy. 2010;26(5):658–66.
Kim SJ, Jung M, Moon HK, Kim SG, Chun YM. Anterolateral transtibial posterior cruciate ligament reconstruction combined with anatomical reconstruction of posterolateral corner insufficiency: comparison of single-bundle versus double-bundle posterior cruciate ligament reconstruction over a 2- to 6-year follow-up. Am J Sports Med. 2011;39(3):481–9.
Kim SJ, Kim TE, Jo SB, Kung YP. Comparison of the clinical results of three posterior cruciate ligament reconstruction techniques. J Bone Joint Surg Am. 2009;91(11):2543–9.
Li Y, Li J, Wang J, Gao S, Zhang Y. Comparison of single-bundle and double-bundle isolated posterior cruciate ligament reconstruction with allograft: a prospective, randomized study. Arthroscopy. 2014;30(6):695–700.
Shon OJ, Lee DC, Park CH, Kim WH, Jung KA. A comparison of arthroscopically assisted single and double bundle tibial inlay reconstruction for isolated posterior cruciate ligament injury. Clin Orthop Surg. 2010;2(2):76–84.
Wang CJ, Weng LH, Hsu CC, Chan YS. Arthroscopic single- versus double-bundle posterior cruciate ligament reconstructions using hamstring autograft. Injury. 2004;35(12):1293–9.
Yoon KH, Bae DK, Song SJ, Cho HJ, Lee JH. A prospective randomized study comparing arthroscopic single-bundle and double-bundle posterior cruciate ligament reconstructions preserving remnant fibers. Am J Sports Med. 2011;39(3):474–80.
Johannsen AM, Anderson CJ, Wijdicks CA, Engebretsen L, LaPrade RF. Radiographic landmarks for tunnel positioning in posterior cruciate ligament reconstructions. Am J Sports Med. 2013;41(1):35–42.
Lopes Jr OV, Ferretti M, Shen W, Ekdahl M, Smolinski P, Fu FH. Topography of the femoral attachment of the posterior cruciate ligament. J Bone Joint Surg Am. 2008;90(2):249–55.
Frank RM, Seroyer ST, Lewis PB, Bach Jr BR, Verma NN. MRI analysis of tibial position of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1607–11.
Amis A, Gupte C, Bull A, Edwards A. Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):257–63.
Servant CT, Ramos JP, Thomas NP. The accuracy of magnetic resonance imaging in diagnosing chronic posterior cruciate ligament injury. Knee. 2004;11(4):265–70.
Fischer S, Fox J, Del Pizzo W, Friedman M, Snyder S, Ferkel R. Accuracy of diagnoses from magnetic resonance imaging of the knee. A multi-center analysis of one thousand and fourteen patients. J Bone Joint Surg Am. 1991;73(1):2–10.
Gross ML, Grover JS, Bassett LW, Seeger LL, Finerman GA. Magnetic resonance imaging of the posterior cruciate ligament Clinical use to improve diagnostic accuracy. Am J Sports Med. 1992;20(6):732–7.
Heron CW, Calvert PT. Three-dimensional gradient-echo MR imaging of the knee: comparison with arthroscopy in 100 patients. Radiology. 1992;183(3):839–44.
Laoruengthana A, Jarusriwanna A. Sensitivity and specificity of magnetic resonance imaging for knee injury and clinical application for the Naresuan University Hospital. J Med Assoc Thai. 2012;95(10):S151–7.
Polly D, Callaghan J, Sikes R, McCabe J, McMahon K, Savory C. The accuracy of selective magnetic resonance imaging compared with the findings of arthroscopy of the knee. J Bone Joint Surg Am. 1988;70(2):192–8.
Osti M, Tschann P, Künzel KH, Benedetto KP. Anatomic characteristics and radiographic references of the anterolateral and posteromedial bundles of the posterior cruciate ligament. Am J Sports Med. 2012;40(7):1558–63.
Tajima G, Nozaki M, Iriuchishima T, Ingham SJ, Shen W, Smolinski P, Fu FH. Morphology of the tibial insertion of the posterior cruciate ligament. J Bone Joint Surg Am. 2009;91(4):859–66.
Forsythe B, Harner C, Martins CA, Shen W, Lopes Jr OV, Fu FH. Topography of the femoral attachment of the posterior cruciate ligament. Surgical technique. J Bone Joint Surg Am. 2009;91(Suppl 2 Pt 1):89–100.
Mejia EA, Noyes FR, Grood ES. Posterior cruciate ligament femoral insertion site characteristics. Importance for reconstructive procedures. Am J Sports Med. 2002;30(5):643–51.
Guenther D, Irarrazaval S, Nishizawa Y, Vernacchia C, Thorhauer E, Musahl V, Irrgang JJ, Fu FH. Variation in the shape of the tibial insertion site of the anterior cruciate ligament: classification is required. Knee Surg Sports Traumatol Arthrosc. 2015. doi:10.1007/s00167-015-3891-2.
Spiridonov SI, Slinkard NJ, LaPrade RF. Isolated and combined grade-III posterior cruciate ligament tears treated with double-bundle reconstruction with use of endoscopically placed femoral tunnels and grafts: operative technique and clinical outcomes. J Bone Joint Surg Am. 2011;93(19):1773–80.
Acknowledgments
Not applicable.
Funding
None
Availability of data and materials
The data and materials in current paper may be made available upon request through sending e-mail to first author.
Authors’ contributions
YJT, LWG, MW and YYX designed the study; YJT, LWG, TEX, BZ and ND collected the data; YJT, LWG, MW, TEX, LGZ, JJ, XYS and LHX analyzed and interpreted the data; YJT, LWG, TEX, BZ and ND wrote the initial draft; YJT, LWG, MW and YYX ensured the accuracy of the data. YJT, LWG, MW, TEX, LGZ, JJ, XYS, LHX, BZ, ND and YYX participated in revising the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Approvals for this study and report were obtained from the Medical Ethics Committee of the Second Hospital of Lanzhou University, Lanzhou, Gansu Province, China. The informed consent was waived by the Medical Ethics Committee as it was a retrospective study utilizing the data and images with the patients’ identification information all removed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Teng, Y., Guo, L., Wu, M. et al. MRI analysis of tibial PCL attachment in a large population of adult patients: reference data for anatomic PCL reconstruction. BMC Musculoskelet Disord 17, 384 (2016). https://doi.org/10.1186/s12891-016-1232-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-016-1232-3