Abstract
Background
The coexistence of tuberculosis (TB) and type 2 diabetes mellitus (DM) presents unique challenges in treatment optimization and management, given the mutual exacerbation of disease processes.
Objective
This multicenter, open-label, randomized controlled trial aims to evaluate the efficacy and safety of two different treatment durations (6-month versus 9-month regimens) regimen for patients with drug-susceptible pulmonary tuberculosis (DS-PTB) and concurrent type 2 diabetes (DM).
Methods
Patients with DS-PTB and type-2 DM from 22 hospitals in China are enrolled. They are randomized in a 1:1 ratio into either the 6-month regimen arm(2HRZE/4HR) or the 9-month regimen arm(2HRZE/7HR). At the end of the intensive phase (the 8th week), patients in both arms who with sputum positive smear will extent one more month of intensive treatment. The primary outcome is the proportion of unfavorable outcomes at 24 months after randomization. Secondary outcomes include treatment success rate at the end of treatment, proportion of recurrence at 24 months after randomization, time to recurrence after treatment completion, proportion of intensive phrase extension, occurrence of adverse events grade 3 or above during treatment.
Discussion
The study focuses on assessing the optimal treatment duration to maximize treatment success while minimizing recurrence and adverse events. The trial is expected to provide vital insights into the appropriate treatment duration for patients with TB-DM, aiming to reduce recurrence rates and improve overall treatment outcomes in this vulnerable population.
Trail registration
Chictr.org.cn, ChiCTR2100044663. Registered on March 25, 2021.
Similar content being viewed by others
Background
Tuberculosis (TB) and Diabetes Mellitus (DM) are significant global health challenges, with their comorbidity increasingly recognized worldwide. According to the World Health Organization’s Global Tuberculosis Report 2023, in 2022 there were approximately 10.6 million new cases of TB globally, and TB caused an estimated 1.30 million deaths (95% UI: 1.18–1.43 million) [1].Concurrently, global data from 2017 indicated approximately 425 million cases of DM, with projections estimating nearly 629 million cases by 2045 [2]. In a national cross-sectional study conducted in China, the prevalence of DM among individuals aged 18 and above was reported to be 12.8% [3].
The interaction between TB and DM is characterized by a substantial impact on the risk of TB infection and treatment outcomes. Studies have shown that individuals with DM are 2.44 to 8.33 times more likely to contract TB compared to those without DM [4,5,6]. Moreover, the presence of DM significantly affects the outcome of anti-TB treatment. Good glycemic control is conducive to improved TB treatment outcomes, whereas poor glycemic control can lead to prolonged positive sputum cultures, treatment failure, relapse, and increased mortality [7].
Despite the current WHO-recommended 6-month treatment regimen for TB combined with diabetes mellitus (TB-DM) [8], there is ongoing controversy among researchers. Some studies reported that the standard 6-month treatment regimen (2HRZE/4HR) is more prone to relapse compared to 9-month or longer treatment durations [9,10,11]. Additionally, patients treated with the 6-month regimen are more likely to experience adverse reactions to anti-TB drugs and intolerance to treatment [12,13,14,15,16]. Therefore, it is of paramount importance to identify an optimal anti-TB treatment regimen for TB-DM patients.
We conducted a multicenter, open-label, randomized controlled clinical trial to determine whether 6-month treatment regimen (2HRZE/4HR) can provide a favorable efficacy outcome at week 104 after treatment initiation in diabetic participants with drug-susceptible pulmonary TB (DS-PTB), as compared with the 9-month regimen. Safety measures, including adverse events, premature discontinuation of the assigned regimen for a reason other than microbiologic ineligibility, were also assessed and compared. This study protocol (date 2022-03-01, version 1.4) outlines our methodology for achieving this goal.
Methods
Study design and oversight
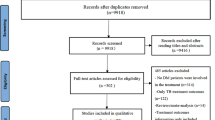
This is a multicenter, open-label, randomized controlled clinical trial with two arms conducted in China. Patients with drug-susceptible pulmonary tuberculosis and type 2 diabetes mellitus are prospectively screened by investigators across 22 participating institutions (Table S1). Eligible patients who meet the inclusion and exclusion criteria are enrolled and randomly assigned to either a 6-month regimen arm (2HRZE/4HR) or a 9-month regimen arm (2HRZE/7HR) in a 1:1 ratio. Both the 6-month regimen arm (Group A) and the 9-month regimen arm (Group B) undergo two phases of treatment: the intensive phase and the consolidation phase. At the end of the intensive phase (week 8), patients with a positive sputum smear extend their intensive treatment by one more month, while those with a negative sputum smear transition to the consolidation phase. During the intensive phase, patients receive four anti-TB agents: isoniazid, rifampin, ethambutol, and pyrazinamide. In the consolidation phase, treatment consists of isoniazid and rifampin. Following the completion of anti-TB treatment, patients are monitored up to 104 weeks from treatment initiation. Glycemic control during TB treatment and glycemic control monitoring during follow-up are managed by diabetes specialists. The primary hypothesis of the study is that the 6-month regimen will be non-inferior to the 9-month regimen in terms of unfavorable outcomes. Figure 1 illustrates the flow chart of the clinical trial.
This study, named “optimized anti-tuberculosis regimens for drug-susceptible pulmonary tuberculosis with diabetes mellitus: A multicenter randomized controlled trial (ORDER-TB)”, was registered with the Chinese Clinical Trials Registry and has received ethical approval from participating hospitals. Written informed consent will be obtained from all participants or their legal guardians by trained medical personnel who may be an investigator, clinician, or designated nurse experienced in explaining the elements of clinical trials.
Site selection
This study is led by the National Center for Clinical Research in Infectious Diseases. The recruiting cooperation units are 22 institutions in seven provinces. All trial sites have adequate staffing, facilities, and laboratory capabilities of performing required mycobacterial tests and glycemic monitoring test. All of them have secure data management systems in place. The cooperative’s quality control will be carried out by a specialist auditing team.
Patient eligibility criteria
Eligible participants are aged ≥ 18 years, with type-2 diabetes and active pulmonary rifampicin-susceptible tuberculosis confirmed by GeneXpert MTB/RIF, subject to exclusion criteria, which include HIV positivity, known drug allergies, and any abnormal lab values among others. Full inclusion and exclusion criteria are outlined in Table 1. Before trial-specific procedures, eligible patients are given comprehensive information, including known benefit of glycemic control, reported adverse events and completed regular treatment and post-treatment follow up. Consent is documented, and screening logs are securely maintained.
Diagnosis criteria and management of type 2 diabetes
Type 2 diabetes is defined before treatment initiation based on the following diagnostic criteria: 1. Fasting Plasma Glucose (FPG) ≥ 7.0 mmol/L (126 mg/dL). Fasting is defined as no caloric intake for at least 8 h.2. 2-hour Plasma Glucose (2hPG) during Oral Glucose Tolerance Test (OGTT) ≥ 11.1 mmol/L (200 mg/dL). The test should be performed using a glucose load containing the equivalent of 75 g anhydrous glucose dissolved in water.3. Glycated Hemoglobin (HbA1c): ≥ 6.5%. 4. a random plasma glucose ≥ 11.1 mmol/L (200 mg/dL) in a patient with classic symptoms of hyperglycemia or hyperglycemic crisis. These guidelines are consistent with those established by the American Diabetes Association (ADA) and other major health organizations [17,18,19].
According to the management of Diabetes Mellitus-Tuberculosis: A Guide to the Essential Practice [20], One or two diabetes specialists are designated in each center for homogeneous management of diabetes. During the anti-TB treatment, blood glucose levels will be measured at least once per month, and HbA1c levels will be monitored every three months. Diabetes specialists will manage and control blood glucose throughout the treatment, including nutritional management, weight management, and the use of hypoglycemic medications. During the follow-up period, blood glucose monitoring will be conducted at least every three months.
Recruitment, randomization and follow-up
Participants with DS-PTB identified by sputum GeneXpert® MTB/RIF assay (Cepheid, Sunnyvale, CA, USA) are screening to ascertain whether they satisfy the other eligibility criteria for enrolment. Participants who meet the inclusion criteria will be randomly assigned to Group A or Group B at a ratio of 1:1 in week 0. The randomization is performed in individual patient in Third People’s hospital of Shenzhen on MedSci RTSM Clout Platform(https://rtsm.medsci.cn/).
Participants of each group will visit the hospital every 2 weeks until 8 weeks after enrollment. Subsequently, visits will be made every 4 weeks until the end of treatment. The drugs and dose of the trial are presented in Table 2. The tests performed at each visit will include the following: physical examination, sputum AFB smear and culture, and blood test. Blood test includes whole blood cell count, live and kidney function and random glucose. Chest CT and Hb1Ac will be performed every 12 weeks. Participants who cannot produce sputum will be encouraged to expectorate sputum. When a participant cannot produce sputum after the first negative culture sputum, they will be considered as having negative sputum culture except of any proof of treatment failure.
After treatment completed, Participants will be followed up every 3 months to 6 months until 24 months after the enrollment date. Physical examination, chest CT, sputum smear and culture, blood test for monitoring glucose control including random glucose and Hb1Ac will be performed. If necessary, electrocardiogram, ophthalmologic examination, brief peripheral neuropathy screen and mental assessment will be carried out. The study timeline is shown in Table 3.
Outcomes definition
The primary outcome is the proportion of unfavorable outcomes at 24 months after randomization. Secondary outcomes include treatment success rate at the end of treatment, proportion of recurrence at 24 months after randomization, time to recurrence after treatment completion, proportion of intensive phrase extension, occurrence of adverse events grade 3 or above during treatment. The treatment success in our study was defined as two consecutive negative results of sputum culture tests at the end of the treatment (the interval is one month) and did not have proof of treatment failure. The severity of each adverse event will be assessed based on Common Terminology Criteria for Adverse Events (CTCAE) version 5.0 [21].
Sample size assumptions
Based on a non-inferiority test designed to compare the rates between two groups, with parameters set as follows: α = 0.05, β = 0.80, Unfavorable outcome in the experimental group and in the control group at 0.2, a group ratio of 1:1, and a cut-off value of 0.1, using Pearson’s chi-square test, indicating low superiority. The calculations determined that a total of 396 participants are required. Accounting for 20% participants loss to follow-up, 495 participants will be enrolled and 248 participants are needed in each of the two groups.
Data collection and quality management
All staff at the collaborating clinical research center or hospital are professionally trained and use a dedicated website for data collection and study management to record information. Staff will only have access to the functions and data required for their position in the study, and all data access on the website will be controlled by a unique login and password. Each sub-center will have a separate login port. And the research centers will summarize the data periodically to ensure the quality of the research progress.
Confidentiality
Collection and operation of participants’ personal information will be limited to only information necessary for the outcome of this study. Paper documents (including personally identifying information and copies of signed consent forms) will be securely maintained in lockable filing cabinets in a closed officed on site. Digital files containing participant data will be saved on a web server, which will be managed and secured by professional engineers. Only authorized staff will have access to the study’s files.
Discussion
The global burden of the dual epidemic of tuberculosis (TB) and diabetes mellitus (DM) remains a significant public health challenge. The median prevalence of TB-DM comorbidity is 16% (IQR 9.0-25.3%) globally [1]. While the prevalence of TB among individuals with diabetes is relatively low, the incidence of both diseases is notably higher in countries within the Asian region [22]. Addressing the management and treatment of patients with TB-DM is crucial.
Currently, the internationally recommended regimen for patients with drug-susceptible TB is a 6-month treatment course [1]. However, there are no specific guidelines tailored for individuals with TB-DM. In 2016, the American Thoracic Society (ATS) recommended that the consolidation period (4 months) could be extended to 7 months, totaling a 9-month course under exceptional circumstances: (1) patients with cavitary TB on the initial chest radiograph and sputum cultures that remain positive after two months of intensive treatment; (2) patients who were not treated with two months of pyrazinamide during the intensive treatment phase [23]. The World Health Organization’s (WHO) updated 2017 guidelines for the treatment of drug-susceptible TB emphasize that patients with TB-DM should be treated with the same anti-TB regimen as those without diabetes [8]. The UNION published the first global guideline on the management of TB-DM in 2019, stating that there is a lack of strong evidence to support a change in the current standard anti-TB regimen for TB-DM [24].
Despite the WHO’s recommendations, previous studies and clinical practice indicate that the standard 6-month anti-TB regimen may not fully address the needs of patients with TB-DM. In China, a longer course of anti-TB treatment for TB-DM, generally 9–12 months with the regimen 2HRZE/10HRE, is advocated [25]. However, there is a lack of high-quality research data to support this extended treatment duration. China’s approach to extending the anti-TB treatment course for TB-DM seems overcautious, often implementing a 1-year treatment regimen based on a review of the literature and multiple surveys. Excessive extension of treatment imposes unnecessary burdens on patients and waste health resources.Given the current trend towards shortening the duration of anti-TB treatment, it is essential to address the optimal treatment course for TB-DM without reversing progress. Therefore, minimizing the treatment duration while ensuring the success rate of anti-TB therapy aligns with the original aim of this study: to investigate the optimal course of treatment for TB-DM through a randomized controlled clinical trial.
2-month sputum smear conversion is a key indicator of treatment response [26]. Pulmonary TB patients with DM are prone to being higher smear grading, lung cavitation and delayed sputum smear and culture conversion [27, 28]. The intensive treatment phase including four potent drugs is critical in TB management as it aims to rapidly reduce the bacterial load, prevent the development of drug resistance, improve patient outcomes and lower relapse rate [29]. In our study, we extended the intensive treatment phase by one month for patients with a positive sputum smear at the end of the initial two months of treatment. Extending the intensive phase for patients who remain sputum-positive ensures that the bacterial load is sufficiently reduced before transitioning to the consolidation phase. This approach is essential because patients who continue to have positive sputum smears at the end of the intensive phase are at a higher risk of treatment failure and relapse [30]. By extending the intensive phase, we aim to ensure a more thorough eradication of the bacteria, thereby improving the likelihood of treatment success and reducing the risk of relapse. Moreover, the extended intensive phase might help prevent the emergence of drug-resistant TB strains.
During the treatment, all participants will receive guidance of blood glucose control regularly from diabetes experts. The effect of the programmatic blood glucose control on the treatment outcome of tuberculosis will be included in the analysis. This study’s findings are expected to provide valuable insights into the optimal duration of intensive treatment for TB-DM patients, helping to inform clinical practice and public health policies. By identifying the most effective treatment regimen, we can improve outcomes for patients with TB-DM, reduce the burden of disease, and enhance the overall efficiency of TB control programs.
In conclusion, the management of TB-DM requires a nuanced approach that considers the unique challenges posed by the coexistence of these two diseases. Extending the intensive treatment phase for patients with persistent sputum positivity might be a critical strategy to enhance treatment outcomes and prevent relapse. This study underscores the importance of optimizing treatment regimens to address the specific needs of TB-DM patients, ultimately contributing to better health outcomes and more efficient use of healthcare resources.
Data availability
The results of this trial will be disseminated only by presentation at academic meetings or publication in academic journals.
References
World Health O. Global tuberculosis report 2023. Geneva: World Health Organization; 2023.
Magliano DJ, Boyko EJ. committee IDFDAtes: IDF Diabetes Atlas. In: Idf diabetes atlas. edn. Brussels: International Diabetes Federation© International Diabetes Federation, 2021.; 2021.
Li Y, Teng D, Shi X, Qin G, Qin Y, Quan H, Shi B, Sun H, Ba J, Chen B, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020;369:m997.
Jabbar A, Hussain SF, Khan AA. Clinical characteristics of pulmonary tuberculosis in adult Pakistani patients with co-existing diabetes mellitus. East Mediterr Health J. 2006;12(5):522–7.
Shetty N, Shemko M, Vaz M, D’Souza G. An epidemiological evaluation of risk factors for tuberculosis in South India: a matched case control study. Int J Tuberc Lung Dis. 2006;10(1):80–6.
Ayelign B, Negash M, Genetu M, Wondmagegn T, Shibabaw T: Immunological impacts of diabetes on the susceptibility of Mycobacterium tuberculosis. J Immunol Res 2019, 2019:6196532.
Pan SC, Ku CC, Kao D, Ezzati M, Fang CT, Lin HH. Effect of diabetes on tuberculosis control in 13 countries with high tuberculosis: a modelling study. Lancet Diabetes Endocrinol. 2015;3(5):323–30.
World Health O. Guidelines for treatment of drug-susceptible tuberculosis and patient care, 2017 update edn. Geneva: World Health Organization; 2017.
Wang JY, Lee MC, Shu CC, Lee CH, Lee LN, Chao KM, Chang FY. Optimal duration of anti-TB treatment in patients with diabetes: nine or six months? Chest. 2015;147(2):520–8.
Khattak M, Rehman AU, Muqaddas T, Hussain R, Rasool MF, Saleem Z, Almalki MS, Alturkistani SA, Firash SZ, Alzahrani OM et al: Tuberculosis (TB) treatment challenges in TB-diabetes comorbid patients: a systematic review and meta-analysis. Ann Med 2024, 56(1):2313683.
Anaam MS, Alrasheedy AA: Recurrence Rate of Pulmonary Tuberculosis in Patients Treated with the Standard 6-Month Regimen: Findings and Implications from a Prospective Observational Multicenter Study. Trop Med Infect Dis 2023, 8(2):110.
Leung CC, Yew WW, Mok TYW, Lau KS, Wong CF, Chau CH, Chan CK, Chang KC, Tam G, Tam CM. Effects of diabetes mellitus on the clinical presentation and treatment response in tuberculosis. Respirology. 2017;22(6):1225–32.
Barss L, Orlikow E, Phang SH, Sabur NF, Arget M, Jarand JM, Field SK, Ainslie M, Fisher DA. Clinical implications of diabetes Mellitus in adults with TB: risk for poor outcomes and mortality. Chest 2016, 150.
Workneh MH, Bjune GA, Yimer SA. Diabetes mellitus is associated with increased mortality during tuberculosis treatment: a prospective cohort study among tuberculosis patients in South-Eastern Amahra Region, Ethiopia. Infect Dis Poverty. 2016;5:22.
Sanghani RN, Udwadia ZF. The association of diabetes and tuberculosis: impact on treatment and post-treatment outcomes. Thorax. 2013;68(3):202–3.
Baker MA, Harries AD, Jeon CY, Hart JE, Kapur A, Lönnroth K, Ottmani SE, Goonesekera SD, Murray MB. The impact of diabetes on tuberculosis treatment outcomes: a systematic review. BMC Med. 2011;9:81.
2. Classification and diagnosis of diabetes: standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S13–27.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, Federici M, Filippatos G, Grobbee DE, Hansen TB, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323.
Jia W, Weng J, Zhu D, Ji L, Lu J, Zhou Z, Zou D, Guo L, Ji Q, Chen L, et al. Standards of medical care for type 2 diabetes in China 2019. Diabetes Metab Res Rev. 2019;35(6):e3158.
Lin YHAD, Kumar AMV, Critchley JA, van Crevel R, Owiti P, Dlodlo RA, Dejgaard A. Management of diabetes mellitus tuberculosis: a guide to the essential practice. Paris, France: International Union Against Tuberculosis and Lung Disease; 2019.
Common Terminology Criteria for Adverse Events (CTCAE). Bethesda MNIoH. 2010. In.
Zheng C, Hu M, Gao F. Diabetes and pulmonary tuberculosis: a global overview with special focus on the situation in Asian countries with high TB-DM burden. Glob Health Action. 2017;10(1):1–11.
Nahid P, Dorman SE, Alipanah N, Barry PM, Brozek JL, Cattamanchi A, Chaisson LH, Chaisson RE, Daley CL, Grzemska M, et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: treatment of drug-susceptible tuberculosis. Clin Infect Dis. 2016;63(7):e147–95.
https://theunion.org/technical-publications/management-of-diabetes-mellitus-tuberculosis-a-guide-to-the-essential-practice (accessed 19 June 2024) MoDM-T-AGttEPTU. In.
Jun -C, Hui -Z, Lin -ZY. Xia -WL, Ting -CM: - mutual impact of diabetes Mellitus and Tuberculosis in China. - Biomedical Environ Sci 2017, – 30(– 5):- 384.
Su WJ, Feng JY, Chiu YC, Huang SF, Lee YC. Role of 2-month sputum smears in predicting culture conversion in pulmonary tuberculosis. Eur Respir J. 2011;37(2):376–83.
Asemahagn MA. Sputum smear conversion and associated factors among smear-positive pulmonary tuberculosis patients in East Gojjam Zone, Northwest Ethiopia: a longitudinal study. BMC Pulm Med. 2021;21(1):118.
Dousa KM, Hamad A, Albirair M, Al Soub H, Elzouki AN, Alwakeel MI, Thiel BA, Johnson JL. Impact of diabetes Mellitus on the presentation and response to treatment of adults with Pulmonary Tuberculosis in Qatar. Open Forum Infect Dis. 2019;6(1):ofy335.
Snider DE Jr., Cohn DL, Davidson PT, Hershfield ES, Smith MH, Sutton FD Jr. Standard therapy for tuberculosis 1985. Chest. 1985;87(2 Suppl):s117–24.
Paradkar MS, Pradhan NN, Balaji S, Gaikwad SN, Chavan A, Dharmashale SN, Sahasrabudhe T, Lokhande R, Deshmukh SA, Barthwal M, et al. Early microbiologic markers of pulmonary tuberculosis treatment outcomes. Ann Am Thorac Soc. 2023;20(12):1760–8.
Acknowledgements
We thank all the physicians and assistants, as well as all enrolled participants who participated in this study.
Funding
This work is supported by the National Natural Science Foundation of China (No. 82070016), the Guangdong Provincial Clinical Research Center for Tuberculosis (No. 2020B1111170014), and the Shenzhen Clinical Research Center for Tuberculosis (No. 20210617141509001). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
P.Z., S.Z., L.F., G.X., and G.D. contributed to the conception and design of the study., P.Z. and L.F. developed the electronic medical record system for data collection. P.Z., Y.X, Y.W., J.T.,and H.Q. managed the participants. H.S., J.L., and Q.H drafted the manuscript. P.Z. and G.D. revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The trial received ethical approval from the Institutional Review Boards of Shenzhen Third People’s Hospital (approval number 2021-014-02) and other participating sites. Participants must provide signed and dated written informed consent prior to undergoing any study-specific procedures.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Trial status
Recruitment began at the first site in June 2021 and is expected to be completed by December 2024.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, P., Shi, H., Xie, Y. et al. Optimized anti-tuberculosis duration for drug-susceptible pulmonary tuberculosis-diabetes mellitus comorbidities: study protocol for a multicenter randomized controlled trial. BMC Pulm Med 24, 469 (2024). https://doi.org/10.1186/s12890-024-03271-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03271-8