Abstract
Background
Postoperative pulmonary complication (PPC) is a leading cause of mortality and poor outcomes in postoperative patients. No studies have enrolled intensive care unit (ICU) patients after noncardiac thoracic surgery, and effective prediction models for PPC have not been developed. This study aimed to explore the incidence and risk factors and construct prediction models for PPC in these patients.
Methods
This study retrospectively recruited patients admitted to the ICU after noncardiac thoracic surgery at West China Hospital, Sichuan University, from July 2019 to December 2022. The patients were randomly divided into a development cohort and a validation cohort at a 70% versus 30% ratio. The preoperative, intraoperative and postoperative variables during the ICU stay were compared. Univariate and multivariate logistic regression analyses were applied to identify candidate predictors, establish prediction models, and compare the accuracy of the models with that of reported risk models.
Results
A total of 475 ICU patients were enrolled after noncardiac thoracic surgery (median age, 58; 72% male). At least one PPC occurred in 171 patients (36.0%), and the most common PPC was pneumonia (153/475, 32.21%). PPC significantly increased the duration of mechanical ventilation (p < 0.001), length of ICU stay (p < 0.001), length of hospital stay (LOS) (p < 0.001), and rate of reintubation (p = 0.047) in ICU patients. Seven risk factors were identified, and then the prediction nomograms for PPC were constructed. At ICU admission, the area under the curve (AUC) was 0.766, with a sensitivity of 0.71 and specificity of 0.60; after extubation, the AUC was 0.841, with a sensitivity of 0.75 and specificity of 0.83. The models showed robust discrimination in both the development cohort and the validation cohort, and they were well calibrated and more accurate than reported risk models.
Conclusions
ICU patients who underwent noncardiac thoracic surgery were at high risk of developing PPCs. Prediction nomograms were constructed and they were more accurate than reported risk models, with excellent sensitivity and specificity. Moreover, these findings could help assess individual PPC risk and enhance postoperative management of patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Postoperative pulmonary complications (PPC) including respiratory tract infection, pleural effusion, respiratory failure, and acute respiratory distress syndrome (ARDS), are commonly observed in postoperative patients [1,2,3]. The impact of PPC varies, leading to postoperative morbidity, intensive care unit (ICU) admission, in-hospital mortality, and prolonged length of hospital stay(LOS) [2, 4, 5]. However, previous investigators have primarily concentrated on specific subgroups of postoperative patients, such as those undergoing lobectomy, hepatectomy, abdominal surgery, or cardiac surgery [6,7,8,9,10,11,12,13]. Studies that specifically investigate the occurrence of PPCs in patients undergoing general thoracic surgeries are rare. Additionally, while previous studies have acknowledged ICU admission as a postoperative complication, reports of the incidence of PPCs in ICU patients are rare [4, 14]. The PPC studies enrolled ICU patients who underwent hepatectomy, on-pump cardiac surgery, or noncardiothoracic surgery [8, 11, 14]. However, ICU patients who underwent noncardiac thoracic surgery have not been included.
The prediction of PPCs could enhance the provision of personalized care for patients and contribute to the efficient allocation of limited resources. Prior research has identified various risk factors for PPC, including sex, age, body mass index (BMI), smoking status, chronic obstructive pulmonary disease (COPD), forced expiratory volume in one second (FEV1), and intraoperative variables [1, 6, 7, 15,16,17,18]. The prevalence and screening of lung cancer and esophageal tumors have significantly increased, leading to an increase in the number of thoracic surgeries performed globally [19,20,21]. With the increasing prevalence of video-assisted thoracic surgery(VATS) and robot-assisted thoracic surgery(RATS) [22, 23], different risk factors are emerging and prediction models for PPCs need to be updated. Several studies have proposed prediction models for PPC [1, 12, 15, 16]. Only the association between the American Society of Anesthesiologists (ASA) grade and the Assess Respiratory Risk in Surgical Patients in Catalonia (ARISCAT score) and the occurrence of PPC was confirmed [1, 24, 25]. Several risk models of postoperative morbidity in patients undergoing thoracic surgery from American or European Thoracic Surgeons database have been reported [26,27,28], but they have been used for specific types of patients and have not been validated in ICU patients. There is a lack of prediction models for PPC in ICU patients who underwent noncardiac thoracic surgery. Therefore, this study aimed to examine the occurrence of PPC events in postoperative ICU patients who underwent noncardiac thoracic surgery, explore the risk factors and establish new prediction models for PPCs.
Methods
Ethics and study design
The ethical committee of West China Hospital, Sichuan University approved this retrospective study (20,221,074). Informed consent was waived due to the retrospective and noninterventional design. All the authors followed the Declaration of Helsinki.
This study was conducted in the Department of Critical Care Medicine, West China Hospital, Sichuan University. This study aimed to investigate the incidence of PPC events in ICU patients after noncardiac thoracic surgery; identify risk factors for postoperative pulmonary complications, develop prediction models for PPC; assess and compare the predictive value of established models for PPC with reported risk models. Besides, we aimed to construct staged prediction models based on the timeline of patients after admitted to the ICU, one at ICU admission and one after extubation. At ICU admission, the risk for PPCs was assessed, to identify high-risk patients and improve management. After extubation, those patients reevaluated at high risk of PPCs could be intervened earlier.
All patients admitted to the ICU from July 2019 to December 2021 at West China Hospital, Sichuan University were enrolled. Patients who meet one of the following criteria were considered to transfer to the ICU: (1) Older than 75 years old; (2) With difficulty in extubation after surgery; (3) Required vasoactive agents to stabilize hemodynamics; (4) At high risk of postoperative complications considered by surgeon or anaesthesiologist. Patients were included if they were: (1) at least 18 years old; (2) admitted to the ICU after surgery (including emergency surgery, limited surgery, or elective surgery); (3) underwent surgery including lung, mediastinum, esophagus or thoracic wall; (4) intubated at ICU admission. Patients were excluded from enrollment if they were: (1) scheduled for pregnancy-related surgery; (2) or not immediately admitted to the ICU after surgery; (3) or secondarily admitted to ICU; (4) or whose length of ICU stay was less than 24 h. Perioperative and postoperative care, including anaesthesia and analgesia protocols, fluid management, transfusion, nutritional support or ventilation strategy was performed at the discretion of the physician in charge. Extubation was performed after discussion among the surgeon, physician and respiratory therapist in charge. Spontaneous breathing trials were performed following the protocol of the American Association for Respiratory Care.
The sample size of this study was calculated following formulas reported [29]. A pilot study was performed before developing prediction models for PPC, and the incidence of PPC was 30%. The calculated sample size of the developing cohort was at least 332(7 predictors [1]), and the total was 474(7:3 ratio).
Data collection and outcomes
Perioperative clinical data were collected following the predesigned collection forms (Supplemental 1). Preoperative data included patient demographics, medical history, pulmonary function test results including postoperative predictive FEV1 (FEV1-ppo, L) 30, baseline laboratory test results, ASA class, the ARISCAT score, the Eurolung1(2016) and Eurolung1(2019) scores [26, 27]. Intraoperative information included the surgical method, duration of surgery, prophylactic antibiotics, and liquid volume(mL). During the postoperative phase (in the ICU), the Acute Physiology and Chronic Health Evaluation II (APACHE II) score, vital signs, laboratory test results, imaging results, and ventilation strategies at ICU admission and after extubation were recorded during the seven postoperative days (pod).
The primary outcome was PPC events occurring from the first postoperative day (pod 0) until the seventh postoperative day (pod 7) or hospital discharge. The PPC was defined as a composite of the following: pneumonia, respiratory failure, pleural effusion (moderate to severe), acute respiratory distress syndrome (ARDS), pulmonary embolism, pneumothorax(moderate to severe), or bronchospasm [1, 3]. The presence and type of PPC were independently evaluated by two clinical physicians. The time of occurrence and the number of PPCs were also documented. Secondary outcomes included the length of ICU stay (d), length of hospital stay (LOS, d), duration of mechanical ventilation (duration of MV, h), events of re-intubation, ICU re-admission, in-hospital mortality, and automatic discharge, and other clinical outcomes.
Statistical analysis
All the patients were divided into two groups by PPC events. Patients were categorized into several subgroups according to the specific type, cumulative number and time of occurrence of PPCs. Additionally, patients underwent different surgical procedures were divided into several groups. To develop prediction models, all the patients enrolled were randomly divided into a development cohort(n = 332) and a validation cohort (n = 143). The baseline characteristics of the two cohorts were also compared (Fig. 1A). Kolmogorov–Smirnov–Lilliefors test was used to test the normality of all the variables. Normally distributed continuous variables are represented by the mean and standard deviation (SD), and continuous variables with a skewed distribution are represented by the median and interquartile range (IQR). Categorical variables are represented by counts and percentages. Differences in baseline characteristics and outcomes are calculated by chi-square test, Fisher test or Kruskal-Wallis test for categorical variables, and t test or Wilcoxon rank sum test for continuous variables. A p-value less than 0.05 was considered statistically significant.
(A) Flow chart of the analysis. All patients underwent noncardiac thoracic surgery and fulfilled the inclusion criteria were enrolled, and patients were excluded if they fulfilled the exclusion criteria. Patients were subsequently divided into a development cohort and a validation cohort (7:3); (B) Cumulative number and percentage of patients with numerous PPCs; (C) Incidence of postoperative pulmonary complication events; (D) Timeline of occurrence of PPCs during the ICU stay
Abbreviations: ARDS: acute respiratory distress syndrome; ICU: intensive care unit; pod: postoperative day; PPC: postoperative pulmonary complication
The association between each variable and PPC was examined by univariate logistic regression; a p-value less than 0.1 was considered a candidate predictor for PPC. The results are expressed as odds ratios (ORs) and 95% confidence intervals (CIs). Multivariate logistic regression analysis (stepwise, backwards elimination) [31] was subsequently used to determine the independent risk factors, and the results are expressed as OR values and 95% CIs; a p-value less than 0.05 was considered statistically significant. Then, nomograms for predicting the probability of PPC were established and receiver operating characteristic (ROC) curves were drawn with STATA V.16.0 software. We constructed staged prediction models based on the timeline of patients after admitted to the ICU, one at ICU admission and one after extubation, to compare the area under the curve (AUC), sensitivity, and specificity. The calibration plot was calculated by 500 repetitions of bootstrap resampling to assess the predictive accuracy of the PPCs. In addition, the AUC, sensitivity and specificity of the reported prediction models for PPCs (ASA class and the ARISCAT score), risk scores for morbidities after thoracic surgery (Eurolung1) and risk models obtained from the American Society of Thoracic Surgeons General Thoracic Surgery Database (of lung cancer and esophageal cancer) were evaluated and compared to those of above-established models.
All the data analyses were performed with SPSS V.25.0 software and STATA V.16.0 software.
Results
Baseline characteristics and incidence of PPC events
In the present study, 475 patients admitted to the ICU after noncardiac thoracic surgery were recruited. The median (interquartile range, IQR) age was 58(49–68), and 72% (342/475) were male. At least one PPC occurred in 171 patients (36.0%), with 276 PPC events. Patients with PPCs had more cases of hypertension, a higher ASA class and lower albumin level (p < 0.05; Table 1). There were more cases of emergency surgery, more cases of surgery in the mediastinum or thoracic wall, and more cases of open chest surgery in patients with PPCs (p < 0.05; Table 1). Regarding the data during the ICU stay, most of data differed between patients with and without PPCs (Table 2 and Supplemental Table 1). After extubation, the patients who developed PPCs were in a worse condition and needed higher FiO2, and had lower PaO2 and pH according to arterial blood gas (ABG) analysis (Table 2). There were no significant differences in baseline characteristics between the development cohort and the validation cohort except for the median age (Supplemental Table 2).
In patients who developed PPCs, 77 patients (15.58%) developed multiple PPCs: 53 patients (11.16%) had two PPCs, and 21(4.42%) had three PPCs (Fig. 1, B), with no patients developing four or more PPCs. The most common PPC was pneumonia (153/475, 32.21%), followed by respiratory failure (58/475, 12.21%), pleural effusion (47/475, 9.89%), ARDS (6/476, 1.26%), pulmonary embolism (5/475, 1.05%), pneumothorax (4/475, 0.84%), and bronchospasm (3/475, 0.63%) (Fig. 1, C). Most of the PPCs occurred during the first three pods (138/171, 80.70%), especially the first two pods (104/171, 60.82%) (Fig. 1, D).
Patient outcomes
As shown in Table 3, patients who developed at least one PPC had a longer duration of mechanical ventilation (h, median [IQR], 13.8[8.18–38.33] vs. 8.9[3.36-14.00], p < 0.001), length of ICU stay (d, median [IQR], 3[2–6] vs. 2[2–2], p < 0.001) and LOS (d, median [IQR], 14[10–22] vs. 11[7–14], p < 0.001). In addition, patients with at least one PPC were more likely to undergo reintubation (20/171[11.70%] vs. 4/304[1.32%], p = 0.047). Differences in specific PPCs, the cumulative number of PPCs and time of the occurrence of PPCs were also compared (Supplemental Tables 3 and Table 4). Moreover, there were no significant differences in the primary or secondary outcomes between the development cohort and the validation cohort (Supplemental Table 2).
Development and validation of nomograms
Univariate logistic regression analysis was applied to evaluate the association of each variable with the PPC, shown in Supplemental Table 5. A p-value less than 0.1 was considered a candidate predictor. Multivariate logistic regression (stepwise backward elimination, p < 0.05) was subsequently used to exclude confounding factors. Hence, an ASA class higher than 3, preoperative albumin level, surgery site, surgery type and albumin level at ICU admission, PaO2 at ICU admission, and duration of mechanical ventilation were found to be significantly and independently associated with PPC (Table 4). Two models were subsequently constructed; one at ICU admission, and one after extubation. The ROC curves and nomograms are shown in Fig. 2.
(A) ROC curve for PPCs, at ICU admission and after extubation in the development cohort; (B) ROC curve for PPCs, at ICU admission and after extubation in the validation cohort; (C) Nomogram for PPCs, at ICU admission; (D) Nomogram for PPCs, after extubation. To estimate the risk of PPCs, mark patient values at each axis, draw a straight line perpendicular to the point axis, and sum the points for all variables. Next, mark the sum on the total point axis and draw a straight line perpendicular to the risk axis. PaO2, mmHg; albumin, g/L; duration of MV, h
Abbreviations: ASA: American Society of Anesthesiologists; ICU: intensive care unit; MV: mechanical ventilation; PaO2: pulmonary arterial oxygen tension; PPC: postoperative pulmonary complication
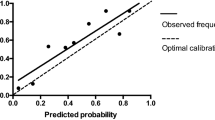
In the development cohort, at ICU admission, an ASA class higher than 3, preoperative albumin level, surgery site and surgery type, PaO2, and albumin levels formed the first model, whose AUC was 0.766 (95% CI, 0.687 to 0.849), with a sensitivity of 0.71 and specificity of 0.60(Goodness of fit test showed x2 = 247.81, p = 0.37). After extubation, the duration of MV was added to the second model, whose AUC was 0.841(95% CI,0.773 to 0.909), with a sensitivity of 0.75 and specificity of 0.83(Goodness of fit test showed x2 = 131.55, p = 0.26) (Fig. 2A). To assess the predictive accuracy, the calibration plot was calculated by 500 repetitions of bootstrap resampling. Both models showed excellent predictive value. At ICU admission, the Brier score (%) was 4.6, and the C-statistic was 0.654; after extubation, the Brier score (%) was 13.1 and the C-statistic was 0.728(Fig. 3A, B). The two models were further tested in the validation cohort. The AUC at ICU admission was 0.703(95% CI, 0.503 to 0.903) and after extubation was 0.833(95% CI, 0.680 to 0.985) (Fig. 2B). Both models performed well in the development cohort and the validation cohort, thus they could be used at different times to evaluate the risk of PPC and enhance the postoperative care of patients.
(A) Calibration plot of the nomogram for predicting PPC, at ICU admission; (B) Calibration plot of the nomogram for predicting PPC, after extubation. The X-axis is the predicted probability of PPC; the Y-axis is the observed probability of PPC. (C) ROC curve of reported risk models for PPCs. The reported risk models included the ASA class, the ARISCAT score, the Eurolung1 score (2016), and the Eurolung1 score(2019), obtained from the STS GTSD (of lung cancer and esophageal cancer)
Abbreviations: ARISCAT: The Assess Respiratory Risk in Surgical Patients in Catalonia; ASA: American Society of Anaesthesiologists; Eurolung1: European risk models for morbidity to predict outcome following anatomic lung resections; ICU: intensive care unit; PPC: postoperative pulmonary complication; STS GTSD: The Society for Thoracic Surgeons General Thoracic Surgery Database
Since reported risk scores for PPCs are not widely used in clinical practice, we aimed to develop simple and effective models for PPCs. Then the ROC curves of our models with those of the ASA class, the ARISCAT score, the Eurolung1 score(2016), Eurolung1 score(2019), and risk models from the STS GTSD (of lung cancer and esophageal cancer) were drawn. The ROC curves and AUC of the reported risk models were shown in Fig. 3C. The sensitivity and specificity of our established models and reported risk scores are shown in Supplemental Table 6. These findings indicated that our established models were more effective than the reported risk models and had excellent sensitivity and specificity.
Discussion
As expected, ICU patients after noncardiac thoracic surgery were prone to develop PPCs, with a percentage of 36.0%, which is higher than that reported previously [1, 4, 15]. Our findings are consistent with a multicenter prospective observational study, in which the percentage of PPC was 33.4% [4]. However, it enrolled high risk patients. Current studies have shown that ICU admission is a poor outcome of PPC [4], so ICU patients are at high risk of PPCs. According to Tables 1 and 2, ASA class higher than 3 and the APACHE II score significantly differed between the PPC group and no PPC group. These findings demonstrated that patients with PPCs had worse organ function at admission, leading to more frequent PPC events and worse outcomes.
In line with prior studies, the current study confirmed that patients developed at least one PPC had a longer duration of mechanical ventilation, longer length of ICU stay, longer LOS, and a greater rate of reintubation [2, 4, 5, 13, 17]. There was no difference in in-hospital mortality between the two groups, due to the few events documented and the significant difference in automatic discharge. In addition, unlike in prior studies, the rise in the number of PPCs was associated with worse outcomes [1, 5]. This study showed that the number of PPCs had no impact on the duration of mechanical ventilation, or the length of ICU stay or LOS. In this study, most of the PPCs occurred during the first three pods, but the time of occurrence of PPCs did not influence clinical outcomes (Supplemental Table 3).
The current study showed that the most common PPC occurring in ICU patients after noncardiac thoracic surgery was pneumonia, which included respiratory infection and inspiration pneumonia. After major surgery, hypoxemia is common [32]. Therefore, most patients admitted to the ICU after surgery are always intubated and under mechanical ventilation. Ventilation-induced lung injury has been increasingly common in the ICU over the years, and leads to poor outcomes [33]. Thus, postoperative ICU patients are more likely to develop pneumonia.
There were plenty of studies highlighting the effects of intraoperative factors on PPC and clinical outcomes. In this study, patients who underwent emergency surgery, surgery in the mediastinum, esophagus, or thoracic wall, open chest surgery, or surgery lasting more than three hours had a greater incidence of PPCs, which is consistent with original articles [2, 15, 17]. VATS or RATS has been confirmed to have better short-term and long-term outcomes than thoracotomy [22, 23, 34]. Similar results were found in this study.
Moreover, several different risk factors for PPCs were identified in this study. During the preoperative phase, an ASA class higher than 3 and a lower preoperative albumin level were independently associated with PPCs, consistent with previous studies [3, 15, 24, 35]. Interestingly, there were no differences in age, BMI, SpO2, history of pulmonary infection or COPD, smoking status, the Brinkman index, or abnormal lung function [3, 36]. However, the intraoperative factors were the same as those reported, for the surgery site and surgery type. Patients who underwent emergency surgery or surgery in the mediastinum or thoracic wall were more likely to develop PPCs [15, 28]. It is innovative in this study, we found that PaO2, albumin level, and the duration of MV during the ICU stay were independently associated with the occurrence of PPCs, which was different from what was observed in original PPC articles recruiting postoperative ICU patients [4, 11]. At ICU admission, patients with lower PaO2 and albumin levels were prone to develop PPCs [17, 37]. The risk of PPCs augmented with the increase in the duration of mechanical ventilation [38]. Our findings illustrated the effect of PaO2 and duration of mechanical ventilation on the occurrence of PPCs, which was rarely reported previously. Therefore, we developed prediction nomograms for PPCs. To comprehensively evaluate the risk of PPCs in ICU patients, two prediction models were constructed based on the timeline after patients were admitted to the ICU. At ICU admission, the AUC was 0.766 (95% CI, 0.687 to 0.845). This could help identify high-risk patients in developing PPCs at ICU admission and improve postoperative management. After extubation, the AUC was 0.841 (95% CI,0.773 to 0.909). It is possible that those patients at high risk of PPCs at ICU admission were at a lower risk level after extubation. As the duration of mechanical ventilation was independently associated with PPCs, the model including the duration of MV was more precise. Concerning those patients reevaluated at high risk of PPCs after extubation, appropriate ventilation strategies could be administrated in time. Both models were well calibrated, showing good Brier score and C-statistic values. These models performed well in the validation cohort. Among these, the predictive value of our models with reported risk scores for PPC and morbidities after thoracic surgery were compared. With similar postoperative morbidities [1, 26,27,28, 39], these models might be effective in this study. Interestingly, the highest AUC of the reported risk models was obtained from the STS GTSD (for lung cancer), which was 0.675(0.613 to 0.737), followed by that obtained from the STS GTSD (for esophageal cancer), the ARISCAT score, the ASA class, the Eurolung1(2019) and the Eurolung1(2016). This indicated that our established models had the highest AUC, and could be considered the most effective prediction models (Supplemental Table 6). Considering the sensitivity, our established models performed better than most of the reported models, other than the ARISCAR score with the highest sensitivity (0.78). Regarding the specificity, the risk model after extubation had the highest specificity, following the risk model obtained from the STS GTSD (for lung cancer)(0.70). In conclusion, it indicated that our prediction models are more effective than previously reported risk models and have higher sensitivity and specificity. This might due to different enrolled populations and different risk factors identified. In this study, there were few lung sections and few available FEV1-ppo values (Table 1), leading to incomplete aggregated scores of Eurolung1. Several predictors were identified based on the American Society of Thoracic Surgeons General Thoracic Surgery Database. In addition to age, sex and type of surgery, the other predictors also included FEV1-ppo, steroid use and specific surgical procedures, which are different from our results. In addition, the reported risk models include only preoperative and intraoperative variables [1, 26, 27, 39, 40], and we also included ICU parameters during the postoperative phase.
This study has several strengths. First, to the best of our knowledge, this is the first study of PPC to enroll ICU patients after non-cardiac thoracic surgery. Previous PPC studies considered ICU admission as a complication, and those studies enrolled ICU patients focused on hepatectomy, on-pump cardiac surgery or noncardiothoracic surgery, rarely on non-cardiac thoracic surgery. Second, few PPC studies have enrolled patients who underwent noncardiac thoracic surgery. The tumour screening and cases of surgery at an early stage have been increasing these years, and the cases of VATS/RATS are increasingly common. Novel risk factors for PPCs emerged. Third, this study identified several novel risk factors for PPCs in ICU patients and established new prediction models for PPCs. A lower PaO2 level at ICU admission and a longer duration of mechanical ventilation were newly found to be independently associated with PPCs. Moreover, compared with reported risk models, the established models showed robust discrimination.
This study has several limitations. First, as a retrospective study, it was less effective than a prospective study. Second, the risk factors and prediction models in this study were applicable only to postoperative ICU patients after noncardiac thoracic surgery, and not to all postoperative patients. Due to the exclusion of patients whose length of ICU stay less than 24 h, the representativeness and validity of this study is limited. This could lead to selection bias, and severe cases of PPCs could be potentially underestimated. In addition, the intraoperative data were not completely documented, leading to defects in risk factors. Third, although the prediction models established in this study had high sensitivity and specificity, due to the modest sample size, the accuracy of the risk models needs to be further tested in larger population-based prospective studies and different enrolled populations. Despite these limitations, since there is no prediction model for PPC widely used, we hope that our models could help clinical physicians identify high-risk patients in developing PPCs and ameliorate the outcomes of postoperative ICU patients.
Conclusion
In the present study, we found that ICU patients after noncardiac thoracic surgery were at high risk of developing PPCs. PPC significantly increased the duration of mechanical ventilation, length of ICU stay, LOS, and rate of reintubation. The ASA class, preoperative albumin level, surgery site, surgery type, PaO2 and albumin level at ICU admission, and duration of MV were found to be independent risk factors of PPCs. Then we constructed effective prediction nomograms with excellent sensitivity and specificity. These risk models were more accurate than reported risk models and could help assess the individual risk of PPC and improve the postoperative management of critical patients after noncardiac thoracic surgery.
Data availability
The datasets used and analysed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- ARISCAT:
-
The Assess Respiratory Risk in Surgical Patients in Catalonia
- ASA:
-
American Society of Anesthesiologists
- AUC:
-
Area under curve
- BMI:
-
Body mass index
- CRRT:
-
Continuous renal replacement therapy
- Eurolung1:
-
European risk models for morbidity to predict outcome following anatomic lung resections
- FEV1-ppo:
-
Postoperative forced expiratory volume in one second
- ICU:
-
Intensive care unit
- LOS:
-
Length of hospital stay
- MV:
-
Mechanical ventilation
- PaCO2:
-
Arterial carbon dioxide tension
- PaO2:
-
Pulmonary arterial oxygen tension
- PEEP:
-
Post end-expiratory pressure
- POD:
-
Postoperative days
- PPC:
-
Postoperative pulmonary complication
- RATS:
-
Robot-assisted thoracic surgery
- ROC:
-
Receiver Operating Characteristic curve
- STS GTSD:
-
The Society for Thoracic Surgeons General Thoracic Surgery Database
- VATS:
-
Video-assisted thoracic surgery
References
Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113(6):1338–50. https://doi.org/10.1097/ALN.0b013e3181fc6e0a
Epidemiology. Practice of ventilation and outcome for patients at increased risk of postoperative pulmonary complications: LAS VEGAS - an observational study in 29 countries. Eur J Anaesthesiol. 2017;34(8):492–507. https://doi.org/10.1097/EJA.0000000000000646
Miskovic A, Lumb AB. Postoperative pulmonary complications. Br J Anaesth. 2017;118(3):317–34. https://doi.org/10.1093/bja/aex002
Fernandez-Bustamante A, Frendl G, Sprung J, et al. Postoperative pulmonary complications, early mortality, and hospital stay following noncardiothoracic surgery: a multicenter study by the perioperative research network investigators. JAMA Surg. 2017;152(2):157. https://doi.org/10.1001/jamasurg.2016.4065
Mazo V, Sabaté S, Canet J, et al. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology. 2014;121(2):219–31. https://doi.org/10.1097/ALN.0000000000000334
Mao X, Zhang W, Ni YQ, Niu Y, Jiang LY. A prediction model for postoperative pulmonary complication in pulmonary function-impaired patients following lung resection. JMDH. 2021;14:3187–3194. https://doi.org/10.2147/JMDH.S327285
Li XF, Jin L, Yang JM, Luo QS, Liu HM, Yu H. Effect of ventilation mode on postoperative pulmonary complications following lung resection surgery: a randomised controlled trial. Anaesthesia. 2022;77(11):1219–27. https://doi.org/10.1111/anae.15848
the PROVECS Study Group, Lagier D, Fischer F, et al. Effect of open-lung vs conventional perioperative ventilation strategies on postoperative pulmonary complications after on-pump cardiac surgery: the PROVECS randomized clinical trial. Intensive Care Med. 2019;45(10):1401–12. https://doi.org/10.1007/s00134-019-05741-8
Neto AS, Hemmes SN, Barbas CS, et al. Incidence of mortality and morbidity related to postoperative lung injury in patients who have undergone abdominal or thoracic surgery: a systematic review and meta-analysis. Lancet Respiratory Med. 2014;2(12):1007–15. https://doi.org/10.1016/S2213-2600(14)70228-0
Brooks-Brunn JA. Predictors of postoperative pulmonary complications following abdominal surgery. Chest. 1997;111(3):564–71. https://doi.org/10.1378/chest.111.3.564
Wang B, Liang H, Zhao H, Shen J, An Y, Feng Y. Risk factors and predictive model for pulmonary complications in patients transferred to ICU after hepatectomy. BMC Surg. 2023;23(1):150. https://doi.org/10.1186/s12893-023-02019-1
Hanada M, Yamauchi K, Miyazaki S, et al. Short-physical performance battery (SPPB) score is associated with postoperative pulmonary complications in elderly patients undergoing lung resection surgery: a prospective multicenter cohort study. Chron Respir Dis. 2020;17:147997312096184. https://doi.org/10.1177/1479973120961846
Piccioni F, Spagnesi L, Pelosi P, et al. Postoperative pulmonary complications and mortality after major abdominal surgery. An observational multicenter prospective study. Minerva Anestesiol. 2023;89(11):964–76. https://doi.org/10.23736/S0375-9393.23.17382-2
Shang K, Xia Z, Ye X, Li Z, Gong C. Positive end-expiratory pressure and risk of postoperative pulmonary complications in patients living at high altitudes and undergoing surgery at low altitudes: a single-centre, retrospective observational study in China. BMJ Open. 2022;12(6):e057698. https://doi.org/10.1136/bmjopen-2021-057698
Neto AS, da Costa LGV, Hemmes SNT, et al. The LAS VEGAS risk score for prediction of postoperative pulmonary complications: an observational study. Eur J Anaesthesiol. 2018;35(9):691–701. https://doi.org/10.1097/EJA.0000000000000845
Amar D, Munoz D, Shi W, Zhang H, Thaler HT. A clinical prediction rule for pulmonary complications after thoracic surgery for primary lung cancer. Anesth Analgesia. 2010;110(5):1343–8. https://doi.org/10.1213/ANE.0b013e3181bf5c99
Oh EJ, Kim J, Kim BG, et al. Intraoperative factors modifying the risk of postoperative pulmonary complications after living donor liver transplantation. Transplantation. 2023;107(8):1748–55. https://doi.org/10.1097/TP.0000000000004544
Li X, Liu H, Wang J, et al. Individualized positive end-expiratory pressure on postoperative atelectasis in patients with obesity: a randomized controlled clinical trial. Anesthesiology. 2023;139(3):262–73. https://doi.org/10.1097/ALN.0000000000004603
Xia C, Dong X, Li H, et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J (Engl). 2022;135(5):584–90. https://doi.org/10.1097/CM9.0000000000002108
Lim E, Batchelor T, Shackcloth M, et al. Study protocol for VIdeo assisted thoracoscopic lobectomy versus conventional open LobEcTomy for lung cancer, a UK multicentre randomised controlled trial with an internal pilot (the VIOLET study). BMJ Open. 2019;9(10):e029507. https://doi.org/10.1136/bmjopen-2019-029507
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660
Ma J, Li X, Zhao S, Wang J, Zhang W, Sun G. Robot-assisted thoracic surgery versus video-assisted thoracic surgery for lung lobectomy or segmentectomy in patients with non-small cell lung cancer: a meta-analysis. BMC Cancer. 2021;21(1):498. https://doi.org/10.1186/s12885-021-08241-5
Xie D, Deng J, Gonzalez-Rivas D, et al. Comparison of video-assisted thoracoscopic surgery with thoracotomy in bronchial sleeve lobectomy for centrally located non-small cell lung cancer. J Thorac Cardiovasc Surg. 2021;161(2):403–e4132. https://doi.org/10.1016/j.jtcvs.2020.01.105
Ülger G, Sazak H, Baldemir R, et al. The effectiveness of ARISCAT risk index, other scoring systems, and parameters in predicting pulmonary complications after thoracic surgery. Medicine. 2022;101(30):e29723. https://doi.org/10.1097/MD.0000000000029723
Kokotovic D, Degett TH, Ekeloef S, Burcharth J. The ARISCAT score is a promising model to predict postoperative pulmonary complications after major emergency abdominal surgery: an external validation in a Danish cohort. Eur J Trauma Emerg Surg. 2022;48(5):3863–7. https://doi.org/10.1007/s00068-021-01826-6
Brunelli A, Salati M, Rocco G, et al. European risk models for morbidity (EuroLung1) and mortality (EuroLung2) to predict outcome following anatomic lung resections: an analysis from the European Society of thoracic surgeons database† ‡. Eur J Cardiothorac Surg Published Online Oct. 2016;15:ezw319. https://doi.org/10.1093/ejcts/ezw319
Brunelli A, Cicconi S, Decaluwe H, Szanto Z, Falcoz PE. Parsimonious eurolung risk models to predict cardiopulmonary morbidity and mortality following anatomic lung resections: an updated analysis from the European Society of thoracic surgeons database. Eur J Cardiothorac Surg. Published online October 11, 2019:ezz272. https://doi.org/10.1093/ejcts/ezz272
Shapiro M, Swanson SJ, Wright CD, et al. Predictors of major morbidity and mortality after pneumonectomy utilizing the society for thoracic surgeons general thoracic surgery database. Ann Thorac Surg. 2010;90(3):927–35. https://doi.org/10.1016/j.athoracsur.2010.05.041
Riley RD, Ensor J, Snell KIE, et al. Calculating the sample size required for developing a clinical prediction model. BMJ Published Online March. 2020;18:m441. https://doi.org/10.1136/bmj.m441
Steéphan F, Boucheseiche S, Hollande J, et al. Pulmonary complications following lung resection. Chest. 2000;118(5):1263–70. https://doi.org/10.1378/chest.118.5.1263
Heinze G, Dunkler D. Five myths about variable selection. Transpl Int. 2017;30(1):6–10. https://doi.org/10.1111/tri.12895
Canet J, Gallart L. Postoperative respiratory failure: pathogenesis, prediction, and prevention. Curr Opin Crit Care. 2014;20(1):56–62. https://doi.org/10.1097/MCC.0000000000000045
Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2013;369(22):2126–36. https://doi.org/10.1056/NEJMra1208707
Oda R, Okuda K, Osaga S, et al. Long-term outcomes of video-assisted thoracoscopic surgery lobectomy vs. thoracotomy lobectomy for stage IA non-small cell lung cancer. Surg Today. 2019;49(5):369–77. https://doi.org/10.1007/s00595-018-1746-4
Chen Y, Wu G, Wang R, Chen J. Preoperative albumin level serves as a predictor for postoperative pulmonary complications following elective laparoscopic gastrectomy. Curr Pharm Des. 2018;24(27):3250–5. https://doi.org/10.2174/1381612824666180713104307
Uchihara T, Yoshida N, Baba Y, et al. Risk factors for pulmonary morbidities after minimally invasive esophagectomy for esophageal cancer. Surg Endosc. 2018;32(6):2852–8. https://doi.org/10.1007/s00464-017-5993-z
Douville NJ, Jewell ES, Duggal N, et al. Association of intraoperative ventilator management with postoperative oxygenation, pulmonary complications, and mortality. Anesth Analgesia. 2020;130(1):165–75. https://doi.org/10.1213/ANE.0000000000004191
Papazian L, Klompas M, Luyt CE. Ventilator-associated pneumonia in adults: a narrative review. Intensive Care Med. 2020;46(5):888–906. https://doi.org/10.1007/s00134-020-05980-0
Wright CD, Kucharczuk JC, O’Brien SM, Grab JD, Allen MS, Society of Thoracic Surgeons General Thoracic Surgery Database. Predictors of major morbidity and mortality after esophagectomy for esophageal cancer: a society of thoracic surgeons general thoracic surgery database risk adjustment model. J Thorac Cardiovasc Surg. 2009;137(3):587–95. https://doi.org/10.1016/j.jtcvs.2008.11.042. discussion 596.
Kozower BD, Sheng S, O’Brien SM, et al. STS database risk models: predictors of mortality and major morbidity for lung cancer resection. Ann Thorac Surg. 2010;90(3):875–83. https://doi.org/10.1016/j.athoracsur.2010.03.115
Acknowledgements
Not applicable.
Funding
This study was funded by the National Key R&D Program of China (2022YFC2504500) and the 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYGD23012).
Author information
Authors and Affiliations
Contributions
XJH and MLD designed and drafted the manuscript. XJH, MLD, HYX, YKZ and FP conducted data analysis and interpretation, prepared tables and figures. BW and YK revised the manuscript and approved the final version. All the authors have approved the final and submitted version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
The Ethics Committee of West China Hospital, Sichuan University approved this retrospective study (20,221,074). Informed consent was waived due to the non-interventional design.
Consent to participate
Informed consent was waived by the Ethics Committee of West China Hospital, Sichuan University (20,221,074), due to the retrospective and non-interventional design.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
He, X., Dong, M., Xiong, H. et al. Prediction models for postoperative pulmonary complications in intensive care unit patients after noncardiac thoracic surgery. BMC Pulm Med 24, 420 (2024). https://doi.org/10.1186/s12890-024-03153-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03153-z