Abstract
Background
Endobronchial valve (EBV) therapy, a validated method for bronchoscopic lung volume reduction (BLVR) in severe emphysema, has been explored for persistent air-leak (PAL) management. However, its effectiveness and safety in the Asian population require further real-world evaluation. In this study, we assessed the outcomes of treatment with EBV within this demographic.
Methods
We conducted a retrospective analysis of medical records from 11 Korean centers. For the emphysema cohort, inclusion criteria were patients diagnosed with emphysema who underwent bronchoscopy intended for BLVR. We assessed these patients for clinical outcomes of chronic obstructive pulmonary disease. All patients with PAL who underwent treatment with EBV were included. We identified the underlying causes of PAL and evaluated clinical outcomes after the procedure.
Results
The severe emphysema cohort comprised 192 patients with an average age of 70.3 years, and 95.8% of them were men. Ultimately, 137 underwent treatment with EBV. Three months after the procedure, the BLVR group demonstrated a significant improvement in forced expiratory volume in 1 s (+160 mL vs. +30 mL; P = 0.009). Radiographic evidence of lung volume reduction 6 months after BLVR was significantly associated with improved survival (adjusted hazard ratio 0.020; 95% confidence interval 0.038–0.650; P = 0.010). Although pneumothorax was more common in the BLVR group (18.9% vs. 3.8%; P = 0.018), death was higher in the no-BLVR group (38.5% vs. 54.5%, P = 0.001), whereas other adverse events were comparable between the groups. Within the subset of 18 patients with PAL, the predominant causes of air-leak included spontaneous secondary pneumothorax (44.0%), parapneumonic effusion/empyema (22.2%), and post-lung resection surgery (16.7%). Following the treatment, the majority (77.8%) successfully had their chest tubes removed. Post-procedural complications were minimal, with two incidences of hemoptysis and one of empyema, all of which were effectively managed.
Conclusions
Treatment with EBV provides substantial clinical benefits in the management of emphysema and PAL in the Asian population, suggesting a favorable outcome for this therapeutic approach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Bronchoscopic lung volume reduction (BLVR) was introduced in 2010 with the publication on the endobronchial valve (EBV) treatment for Emphysema Palliation Trial (VENT) [1]. The EBV is a minimally invasive bronchoscopic device designed for lung volume reduction in patients with severe emphysema. Its primary characteristics include the ability to redirect airflow away from hyperinflated areas of the lung, promoting improved lung function and systemic relief. Although adverse events include pneumothorax, acute exacerbation of chronic obstructive pulmonary disease (COPD), and hemoptysis, the incidences are relatively low at less than 8%. The procedure improved lung function, exercise capacity, and respiratory symptoms [1]. After the VENT trial, the absence of interlobar collateral ventilation (CV) was identified as an important predictor of response to BLVR [2]. Subsequent studies among selected patients without collateral ventilation showed consistent improvements in clinical parameters and acceptable safety profiles [3,4,5].
In 2018, the Zephyr endobronchial valve was approved by the United States Food and Drug Administration [6]. Since then, EBV has become a treatment option for advanced emphysema recommended by GOLD [7] and NICE [8].
In Asian countries, the clinical application of EBV has been relatively scarcely reported. The first reports of EBV in Asia, published in 2015 [9, 10], also showed improvements in lung function, exercise capacity, respiratory symptoms, and quality of life. Meanwhile, these studies also reported a higher complication rate of pneumothorax than that reported in studies conducted involving Western populations [1, 2, 11]. The possible explanations include an older target population, lower body mass index (BMI), and poorer exercise capacity in the Asian target population. Despite lower forced expiratory volume in 1 s (FEV1), hyperinflation, represented by residual volume, was less severe. The findings suggest some discrepancies in patient characteristics among ethnic groups, and thoracic cage morphology may be one of them [12].
Furthermore, there are not enough long-term studies on BLVR including the Asian population. In this study, we collected clinical data of the entire population considered for treatment with EBV in Korea to confirm its long-term efficacy and safety in Korea.
Methods
Study design and study population
This retrospective multicenter cohort study included patients from Korea between July 2012 and July 2021. A total of 13 institutions had experience with EBV during the study period, and 11 of them provided the data. The number of omitted patients was less than 15 based on the market survey.
The inclusion criterion was bronchoscopic assessment for treatment with EBV. The two distinct indications for EBV insertion; i) bronchoscopic lung volume reduction (BLVR) in patients with emphysema and ii) persistent air-leak (PAL) in patients with a chest tube, were considered for the study. Patients were selected at the attending physician’s discretion.
For BLVR candidates, the presence of collateral ventilation (CV) was a primary exclusion criterion due to its negative impact on the treatment outcomes. Most institutes included patients with a minimum Modified Medical Research Council (mMRC) dyspnea scale score of 2; however, one institute included patients with an mMRC score of 1, justifying their inclusion based on their severe airflow limitation. CV status was assessed physiologically with the Chartis® Pulmonary Assessment System (PulmonX Corporation., Redwood City, CA, USA) and radiographically with computed tomography (CT)-fissure analysis. The Chartis system facilitated isolation of a target lobe using a balloon catheter, followed by measurement of airflow and pressure within the lobe. A key criterion for contraindicating BLVR was the detection of significant airflow in the lobe despite balloon occlusion, indicating substantial ventilation. Furthermore, BLVR was contraindicated if the fissure lengths were not clearly defined for 5–10% of their total length. Those who underwent bronchoscopy but did not receive EBV due to CV were classified into the no-BLVR group. All patients with persistent air-leak received treatment with EBV. The valves used in this study were Zephyr one-way EBV (PulmonX Corporation, Redwood City, CA, USA).
For the management of PAL, the treatment approach was uniformly inclusive across all centers. The assessment of collateral ventilation varied among the institutes; three utilized the Chartis system whereas the other three did not.
The present study was approved by the Institutional Review Board (IRB) of each institution. Due to the retrospective nature of the study, the need for informed consent was waived by the IRB of Asan Medical Center. The IRB protocol numbers are documented in the additional file (Additional file 1). The investigation was performed in accordance with the Declaration of Helsinki.
Data collection
The clinical and survival data were retrospectively collected from medical records. Patients were followed from the date of bronchoscopic assessment until death or the last date of follow-up. Collected data included demographics, comorbidities, treatment for the lung disease, pulmonary function test (PFT) results, radiographic findings, chronic obstructive pulmonary disease (COPD) assessment test results, mMRC Dyspnoea Scale score, 6-min walk distance, procedure-related details, clinical outcomes, and adverse events following the procedure. The adverse events included pneumothorax, hemoptysis, empyema, acute exacerbation of COPD, and mortality.
Effects after EBV insertion
Among patients requiring BLVR, all-cause mortality and incidents of acute exacerbation of COPD were evaluated. The events were compared between patients who received EBV and those who did not. Changes in FEV1 and radiographic findings before and after the index date were also compared. Changes in FEV1 were assessed by measuring differences in FEV1 before and after the index date. Lung volume reduction of the target lobe was assessed by the physicians at each participating study site. It was defined by a reduction of more than 50% in lung volume assessed through chest radiographs or chest CT scans obtained 6 months after the procedure. To ensure consistency and objectivity in these assessments, any cases of disagreement or ambiguity were resolved through a consensus decision made by JYH and SWL. Subgroup analyses of mortality and acute exacerbation were performed to determine the effects of response to BLVR. For patients with PAL treated off-label with EBV, we collected information on the air-leak etiology, specifics of the EBV procedure, the timing of chest tube removal, and any subsequent adverse events.
Statistical analysis
Data were analyzed using the Student’s t-test, Mann–Whitney U test, Wilcoxon’s signed-rank test, the χ2 test, Fisher’s exact test, or analysis of variance, as appropriate. Time-to-mortality and time-to-acute exacerbation were evaluated with Kaplan–Meier survival curves. Log-rank test was performed to compare the groups. Additionally, multivariate Cox proportional-hazard regression analyses were implemented. Variables with P < 0.20 in univariate analysis were selected for multivariate analysis.
A value of P < 0.05 was considered statistically significant (two-tailed). All statistical analyses were conducted using R Statistical Software (version 4.0.3; R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline characteristics
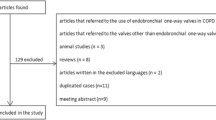
A total of 210 patients were included in the study (Supplementary Fig. 1, Additional file 2). The majority (91.4%) had severe emphysema, and the rest (8.6%) had PAL (Fig. 1). The mean age of the entire population, including 95.7% male patients, was 69.7 years. The median follow-up period was 18.5 months for patients with emphysema and 8.0 months for those with PAL (Table 1).
Among the 192 patients with emphysema, EBV was placed in 137 (71.4%). Distribution of age (72.6 years vs. 69.4 years, P = 0.053), sex (male: 96.4% vs. 95.6%, P > 0.999), and residual volume (209.3% vs. 197.6% predicted, P = 0.247) were comparable between the no-BLVR and BLVR groups; however, BMI was lower in the no-BLVR group (18.7 kg/m2 vs. 20.1 kg/m2, P = 0.013). Additionally, FEV1 after bronchodilation (25.2% predicted vs. 31.4% predicted, P = 0.001) and the diffusing capacity of the lungs for carbon monoxide (5.6 min∙mm Hg vs. 7.1 min∙mm Hg, P = 0.002) were lower in the no-BLVR group than in the BLVR group. Baseline comorbidities, long-term oxygen therapy, use of inhalers, COPD assessment test scores and mMRC dyspnea scale scores were similar (Supplementary Table 1, Additional file 3).
In the 18 (94.4% male) patients with PAL, the mean age was 63.4 years and mean BMI was 21.6 kg/m2 (Table 2). Fifteen patients (83.3%) had been previously diagnosed with chest diseases, and the most common cause of PAL was spontaneous secondary pneumothorax (8/18, 44.4%), followed by parapneumonic effusion/empyema (4/18, 22.2%) and surgical resection of the lung (3/18, 16.7%) (Supplementary Table 3, Additional file 5). Within the cohort, 17 patients retained chest tubes during the procedure. The sole patient without a chest tube at the time of the procedure exhibited an air leak at the pneumonectomy site. Four patients had previously undergone surgical intervention for PAL, which did not result in the resolution of the condition.
Procedure details
EBV insertion was performed on 155 patients. The right upper lobe was the most frequent location for placement. Most procedures (74.2%) were performed under conscious sedation. The emphysema group exhibited increased number of valves placement than the PAL group (3.0 vs. 2.0, P < 0.001). The mean duration of the procedure was 44.3 min, and it was comparable between the patients with emphysema and PAL (45.1 vs. 38.0 min, P = 0.346). The mean hospital stay after the procedure was 6.1 and 30.3 days, respectively (Supplementary Table 2. Additional file 4).
Adverse events
Pneumothorax (14.1%) was the most common adverse event in 192 patients with severe emphysema. It was more frequent in the BLVR group (18.9% vs. 3.8%, P = 0.018). In the BLVR group, 52.0% (13/25) had pneumothorax within 7 days of the procedure (median time: 1 day, interquartile range [IQR]: 1–2 days), whereas 48.0% (12/25) had more delayed pneumothorax (median time: 108 days, IQR: 36.8–245.5 days). EBVs were removed in six patients, and one patient died of tension pneumothorax. The occurrence of hemoptysis (1.9% vs. 9.2%, P = 0.165) and empyema did not differ between the groups (1.9% vs. 0.8%, P > 0.999, Table 3).
In the cohort of patients with PAL, post-procedural complications included hemoptysis in two cases (11%), including one case of non-massive and one of massive hemoptysis. Additionally, one patient (5.6%) developed empyema. No further adverse events were noted (Table 2).
Clinical outcomes of COPD emphysema
For patients with severe emphysema, overall survival rates were comparable between those who underwent BLVR and those who did not (P = 0.181, Supplementary Fig. 2, Additional file 6). However, a subgroup analysis revealed a significant difference in survival between the no-BLVR and BLVR groups categorized based on radiographic evidence of lung volume reduction 6 months after the procedure (P = 0.033, Fig. 2). Kaplan–Meier survival curve analysis indicated similar survival trends between patients in the no-BLVR group and those in the BLVR group without lung volume reduction. Radiographic lung volume reduction at 6 months was an independent prognostic factor for reduced mortality after adjusting for age, sex, BMI, baseline FEV1 (% predicted), and mMRC dyspnea scale scores (adjusted hazard ratio [aHR], 0.020; 95% CI 0.038–0.650; P = 0.010, Table 4). The incidence of COPD acute exacerbation was not significantly different between the BLVR group and no-BLVR group (P = 0.120, Supplementary Fig. 3, Additional file 7).
Three months post-procedure, the FEV1 improvement was more pronounced in the BLVR groups than in the no-BLVR group (+160 mL vs. +30 mL; P = 0.009, Fig. 3). Within the BLVR group, a 20.0% enhancement of FEV1 was noted. On day 300, the FEV1 continued to rise in the BLVR group, whereas it declined in the no-BLVR group (Supplementary Fig. 4, Additional file 8).
Clinical outcomes of persistent air-leak
All the 18 patients underwent CT scans to determine the appropriate sites for EBV insertion. In ten of these patients, indigo carmine blue dye was utilized to further delineate the air-leak sites. Collateral ventilation assessment using the Chartis system was conducted in four patients, which did not reveal any collateral ventilation. Among the 17 patients who had a chest tube at the time of the procedure, 14 (82.4%) had their chest tubes removed after treatment. The median interval from the procedure, as evidenced on chest radiographs, was 3.0 days (IQR: 0–19.5 days). The median time to chest tube removal following the procedure was 16.5 days (IQR: 4.75–33.50). Among the four patients evaluated using the Chartis system, chest tube removal occurred on 2, 4, and 40 days in three patients, respectively, after EBV insertion. The chest tube could not be removed in another patient. Three patients (17.6%) in total were unable to have their chest tubes removed. The causes of the air-leak were spontaneous secondary pneumothorax and bronchobiliary fistula, and it was unknown in one patient.
The valves were removed in two cases. In one case, the valves were removed after the resolution of PAL. In the other case, they were removed after treatment with EBV was considered ineffective. No adverse events related to the procedure were noted in both cases. Additionally, one patient reported expelling the valve during a coughing episode at a follow-up outpatient clinic visit.
Discussion
In this analysis, we reviewed the cases of 210 patients assessed for EBV therapy, of which 155 underwent the procedure. Specifically, BLVR was performed in 137 out of 192 patients with severe emphysema who were evaluated as potential candidates. Notably, an independent predictor of improved overall survival was the radiographic evidence of lung volume reduction, as determined by visual estimation. Furthermore, in 18 patients with PAL, a majority (77.8%) exhibited clinical improvement following treatment with EBV.
Among patients with emphysema, we observed a larger increase in FEV1 and a trend toward better survival in patients who underwent BLVR than in those who did not. The observed 20% improvement in FEV1 after 3 months is consistent with previous studies, which have reported improvements ranging from 17 to 29% [13]. Although we were unable to evaluate long-term changes in FEV1 due to insufficient follow-up PFT data, the trend was sustained up to approximately 1 year. The multicenter randomized controlled LIBERATE trial showed an FEV1 increase of 104 mL after a year of the treatment with EBV [3]. Another recent study including 280 patients reported that the improvements in FEV1 and other clinical outcome measures were maintained at least up to 3 years, albeit with a diminishing effect over time [14].
Improved survival with BLVR has been consistently reported in the literature. In the subgroup analysis in the STELVIO study, Klooster et al. found that predictors of survival, the BODE index score, 6-min-walk distance, and hyperinflation improve after BLVR [15]. In another retrospective cohort study comparing 483 patients in the BLVR group and 988 patients in the no-BLVR group, the median survival was longer in the BLVR group (median 3133 days vs. 2503 days; P < 0.001) [16].
BLVR treatment is usually performed in carefully selected patients with severe emphysema who remain symptomatic despite optimal medical treatment, show evidence of hyperinflation, and demonstrated absence of CV [13, 17]. However, even among the carefully selected patients, treatment response is variable. In our subgroup analysis, we found radiographic reduction in lung volume assessed through visual estimation at 6 months interval to be an independent factor associated with better survival. Nonetheless, survival benefit was not observed without lung volume reduction (Fig. 2). Based on the result, we re-emphasize the importance of evaluating BLVR candidates for their potential to achieve lung volume reduction.
Studies on the off-label use of Zephyr EBV in patients with PAL is limited. However, most of the patients (82.4%) included in this study for PAL were able to have their chest tube removed after placement of EBVs. Similarly, an Italian multicenter retrospective study including 67 patients who had PAL after lung resection, reported a resolution rate of 88.0% after the treatment [18]. Although the treatment success rate was lower in our cohort compared with that is previous studies, this was anticipated since we included all causes of PAL rather than limiting to post-surgical cases. Currently, the FDA has only approved the use of the intrabronchial valve (Spiration. Inc., Redmond, Washington, USA) for managing post-surgical prolonged air-leaks under the Human Device Exemption (HDE) program [19]. Nevertheless, attempts to treat PAL of various causes with bronchoscopies continue, as PAL is detrimental, and its management is still controversial and challenging [20,21,22,23]. Our study adds to the feasibility of managing PAL of different causes with EBV. However, further prospective studies with controlled protocols are warranted, especially for assessing treatment response in the presence of collateral ventilation.
Reports on BLVR from Asian countries, including Korea, Japan, and China, are limited. In Japan, BLVR techniques with autologous blood, thrombin or Spigot have been reported through case series or reports [24, 25], and relatively common methods such as EBV or coil have not been published. In China, experimental devices including flap or occlude have been studied [26, 27], alongside case reports [28, 29] and single-arm studies evaluating the efficacy of endobronchial valve [30, 31], showing improvements in lung function and exercise capacity. In Korea, after the early studies reporting the clinical outcomes of EBV insertion [9, 10], studies on the improvement of ventilation-perfusion mismatch with BLVR and the utility of fissure integrity analyzed through quantitative CT to select EBV insertion sites were published [32, 33]. Essentially, the present evidence of BLVR is mostly based on data from the non-Asian population. In this context, our study showed meaningful insights into BLVR, drawn from data obtained from more than two hundred patients with a median follow-up of 18.5 months, confirming the long-term efficacy and safety of this treatment in the Asian population.
In the general population, lung function differs among racial groups. Caucasians have larger total lung capacity, forced vital capacity, and FEV1, whereas functional residual capacity and residual volume are similar [34, 35]. Although the cause of the disparity is inconclusive, the differences have been attributed to anatomical distinctions. In a study comparing 13 Caucasians, 14 Chinese, and 11 Indian, the width and surface area of the Caucasian were found to be greater [36]. Our study has shown BLVR can be implemented in Asian patients, despite the distinctions.
This study has few limitations. First, this is a retrospective review, limiting the evaluation of confirmative effectiveness. However, the inclusion of data from more than 90% of patients who underwent treatment in one countryprovides valuable insights into how this procedure was conducted and standardized after being introduced to the country. Second, the procedure was performed in 11 institutions, and the protocols were not standardized. For instance, while most institutions performed BLVR under local anesthesia after confirming the absence of CV using the Chartis system, one institution performed BLVR mostly under general anesthesia (35/41, 85.4%) without Chartis evaluation (28/41, 68.3%). Furthermore, the use of the Chartis system for patients with PAL varied as three of the six institutes used it and three did not. These differences can contribute in part to the results that survival benefit was only evident when the target lobar volume was reduced, and EBV insertion alone did not result in sufficient differences. Third, initially, we planned to incorporate the analysis of mMRC dyspnea scale and 6-min-walk distance test to assess functional improvements in patients following BLVR. However, due to the gaps in data, we were unable to evaluate serial changes in those outcomes. Instead, we focused on a comprehensive evaluation of PFT.
Conclusions
We reviewed data from 210 patients considered for treatment with EBV in an Asian country over 10 years, with 155 eventually receiving the valve. Most were patients with severe emphysema. FEV1 improvements were significantly greater in the BLVR group than in the no-BLVR group. Furthermore, a trend for better survival was observed in the BLVR group than in the no-BLVR group. For patients with PAL, treatment with EBV showed satisfactory resolution rate with few adverse events. This study suggests that treatment with EBV is an effective and safe option in the Asian population.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- EBV:
-
Endobronchial valve
- BLVR:
-
Bronchoscopic lung volume reduction
- PAL:
-
Persistent air-leak
- CV:
-
Collateral ventilation
- BMI:
-
Body mass index
- FEV1 :
-
Forced expiratory volume in 1 s
- CT:
-
Computed tomography
- IRB:
-
Institutional review board
- PFT:
-
Pulmonary function test
- COPD:
-
Chronic obstructive pulmonary disease
- mMRC Dyspnea Scale:
-
Modified Medical Research Council Dyspnea Scale
- IQR:
-
Interquartile range
References
Sciurba FC, Ernst A, Herth FJ, Strange C, Criner GJ, Marquette CH, Kovitz KL, Chiacchierini RP, Goldin J, McLennan G. A randomized study of endobronchial valves for advanced emphysema. N Engl J Med. 2010;363(13):1233–44.
Herth FJ, Noppen M, Valipour A, Leroy S, Vergnon JM, Ficker JH, Egan JJ, Gasparini S, Agusti C, Holmes-Higgin D, et al. Efficacy predictors of lung volume reduction with Zephyr valves in a European cohort. Eur Respir J. 2012;39(6):1334–42.
Criner GJ, Sue R, Wright S, Dransfield M, Rivas-Perez H, Wiese T, Sciurba FC, Shah PL, Wahidi MM, de Oliveira HG, et al. A multicenter randomized controlled trial of zephyr endobronchial valve treatment in heterogeneous emphysema (LIBERATE). Am J Respir Crit Care Med. 2018;198(9):1151–64.
Kemp SV, Slebos DJ, Kirk A, Kornaszewska M, Carron K, Ek L, Broman G, Hillerdal G, Mal H, Pison C, et al. A multicenter randomized controlled trial of zephyr endobronchial valve treatment in heterogeneous emphysema (TRANSFORM). Am J Respir Crit Care Med. 2017;196(12):1535–43.
Valipour A, Slebos DJ, Herth F, Darwiche K, Wagner M, Ficker JH, Petermann C, Hubner RH, Stanzel F, Eberhardt R. Endobronchial valve therapy in patients with homogeneous emphysema. Results from the IMPACT study. Am J Respir Crit Care Med. 2016;194(9):1073–82.
Zephyer® Endobronchial VALVE System P180002. https://www.accessdata.fda.gov/cdrh_docs/pdf18/P180002a.pdf. Accessed 11 Oct 2022.
GOLD. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2023.
NICE. Endobronchial valve insertion to reduce lung volume in emphysema. Interventional procedures guidance [IPG600]. 2017.
Park TS, Hong Y, Lee JS, Lee SM, Seo JB, Oh YM, Lee SD, Lee SW. Efficacy of bronchoscopic lung volume reduction by endobronchial valves in patients with heterogeneous emphysema: report on the first Asian cases. J Korean Med Sci. 2014;29(10):1404–10.
Park TS, Hong Y, Lee JS, Oh SY, Lee SM, Kim N, Seo JB, Oh YM, Lee SD, Lee SW. Bronchoscopic lung volume reduction by endobronchial valve in advanced emphysema: the first Asian report. Int J Chron Obstruct Pulmon Dis. 2015;10:1501–11.
Herth FJ, Eberhardt R, Gompelmann D, Ficker JH, Wagner M, Ek L, Schmidt B, Slebos DJ. Radiological and clinical outcomes of using Chartis™ to plan endobronchial valve treatment. Eur Respir J. 2013;41(2):302–8.
Beall CM. A comparison of chest morphology in high altitude Asian and Andean populations. Hum Biol. 1982;54(1):145–63.
Hartman JE, Vanfleteren L, van Rikxoort EM, Klooster K, Slebos DJ. Endobronchial valves for severe emphysema. Eur Respir Rev. 2019;28(152):180121.
Hartman JE, Klooster K, Koster TD, Ten Hacken NHT, van Dijk M, Slebos DJ. Long-term follow-up after bronchoscopic lung volume reduction valve treatment for emphysema. ERJ Open Res. 2022;8(4):00235–2022.
Klooster K, Hartman JE, Ten Hacken NHT, Slebos DJ. Improved predictors of survival after endobronchial valve treatment in patients with severe emphysema. Am J Respir Crit Care Med. 2017;195(9):1272–4.
Hartman JE, Welling JBA, Klooster K, Carpaij OA, Augustijn SWS, Slebos DJ. Survival in COPD patients treated with bronchoscopic lung volume reduction. Respir Med. 2022;196:106825.
Klooster K, Slebos DJ. Endobronchial valves for the treatment of advanced emphysema. Chest. 2021;159(5):1833–42.
Fiorelli A, D’Andrilli A, Cascone R, Occhiati L, Anile M, Diso D, Cassiano F, Poggi C, Ibrahim M, Cusumano G, et al. Unidirectional endobronchial valves for management of persistent air-leaks: results of a multicenter study. J Thorac Dis. 2018;10(11):6158–67.
Dugan KC, Laxmanan B, Murgu S, Hogarth DK. Management of persistent air leaks. Chest. 2017;152(2):417–23.
Lazarus DR, Casal RF. Persistent air leaks: a review with an emphasis on bronchoscopic management. J Thorac Dis. 2017;9(11):4660–70.
Cusumano G, Fiorelli A, Bellofiore S, Lizzio CR, Giarlotta R, Santini M, Terminella A. Endoscopic one-way endobronchial valves in the treatment of persistent air leak with empyema. Shanghai Chest. 2019;3:56–61.
Varela G, Jiménez MF, Novoa N, Aranda JL. Estimating hospital costs attributable to prolonged air leak in pulmonary lobectomy. Eur J Cardiothorac Surg. 2005;27(2):329–33.
Liberman M, Muzikansky A, Wright CD, Wain JC, Donahue DM, Allan JS, Gaissert HA, Morse CR, Mathisen DJ, Lanuti M. Incidence and risk factors of persistent air leak after major pulmonary resection and use of chemical pleurodesis. Ann Thorac Surg. 2010;89(3):891–7; discussion 897-898.
Tsujino K, Sasada S, Kodama M, Ishihara H, Kawase I. Severe bullous emphysema and hypercapnia successfully treated by bronchoscopic lung volume reduction. Respirology. 2009;14(6):907–9.
Mizumori Y, Mochiduki Y, Nakahara Y, Kawamura T, Sasaki S, Morimoto A, Tsukamoto H. Effects of bronchoscopic lung volume reduction using transbronchial infusion of autologous blood and thrombin in patients with severe chronic obstructive pulmonary disease. J Thorac Dis. 2015;7(3):413–21.
Wu Q, Wu JP, Fan Y, Liang CB, Ma JL, Li P, Hua JN, Wang YM, Wang JR, Li WP, et al. Application of bronchoscopic lung volume reduction using one-way flap device in sheep model of heterogeneous emphysema. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 2006;18(8):482–4.
Song L, Zhao F, Ti X, Chen W, Wang G, Wu C, Li Y. Bronchoscopic lung volume reduction for pulmonary emphysema: preliminary experience with endobronchial occluder. Respir Care. 2013;58(8):1351–9.
Yin Y, Hou G, Herth FJ, Wang XB, Wang QY, Kang J. Significant lung volume reduction with endobronchial valves in a patient despite the presence of microcollaterals masked by low-flow Chartis phenotype. Int J Chron Obstruct Pulmon Dis. 2016;11:2913–7.
Hou G, Wang W, Wang QY, Kang J. Bronchoscopic bullectomy with a one-way endobronchial valve to treat a giant bulla in an emphysematic lung: a case report. Clin Respir J. 2016;10(5):657–60.
Yu H, Yang Z, Zhu M, Liang Z, Zhao W, Zhu Q, Chen LA. Endobronchial valve therapy for patients with advanced emphysema. A report from a tertiary care center in China. Saudi Med J. 2022;43(12):1397–401.
Guo F, Huang J, Hu Y, Qiu J, Zhang H, Zhang W, Cheng Y, Liao J, Wang G. Clinical outcomes and quantitative CT analysis after bronchoscopic lung volume reduction using valves for advanced emphysema. J Thorac Dis. 2022;14(6):1922–32.
Lee SW, Lee SM, Shin SY, Park TS, Oh SY, Kim N, Hong Y, Lee JS, Oh YM, Lee SD, et al. Improvement in ventilation-perfusion mismatch after bronchoscopic lung volume reduction: quantitative image analysis. Radiology. 2017;285(1):250–60.
Lee SW, Shin SY, Park TS, Choi YY, Park JC, Park J, Oh SY, Kim N, Lee SH, Lee JS, et al. Clinical utility of quantitative CT analysis for fissure completeness in bronchoscopic lung volume reduction: comparison between CT and Chartis™. Korean J Radiol. 2019;20(7):1216–25.
Saad NJ, Patel J, Minelli C, Burney PGJ. Explaining ethnic disparities in lung function among young adults: a pilot investigation. PLoS One. 2017;12(6):e0178962.
Yang TS, Peat J, Keena V, Donnelly P, Unger W, Woolcock A. A review of the racial differences in the lung function of normal Caucasian, Chinese and Indian subjects. Eur Respir J. 1991;4(7):872–80.
Donnelly PM, Yang TS, Peat JK, Woolcock AJ. What factors explain racial differences in lung volumes? Eur Respir J. 1991;4(7):829–38.
Acknowledgements
None.
Funding
This study was supported through an Investigator Sponsored Research Grant by the Pulmonx Corporation, Redwood City, CA, USA. This was investigator-initiated research, and the sponsor has no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript. This study was also supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (No. 2022M3A9G8017220).
Author information
Authors and Affiliations
Contributions
JYH, BHJ and SWL made substantial contribution to the conception and design of the study and the analysis and interpretation of the data. JYH and SWL drafted the manuscript. JYH, BHJ and SWL substantively revised it. HIY, HK, YJC, CK, SJL, HhK, SWR, YJL, BKK, SKK, KHS contributed to the acquisition of data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by institutional review boards of the 11 participating hospitals. The approval numbers are provided in the Supplementary material. Informed consent was waived due to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Institutional review board protocol numbers. Documentation of the IRB protocol numbers.
Additional file 2: Supplementary Figure 1.
Number of cases from each hospital included in this study.
Additional file 3: Supplementary Table 1.
Baseline characteristics of patients who underwent bronchoscopy for intended bronchoscopic lung volume reduction.
Additional file 4: Supplementary Table 2.
Procedural details of patients who received treatment with EBV.
Additional file 5: Supplementary Table 3.
Comorbidities of patients who underwent treatment with EBV for persistent air-leak.
Additional file 6: Supplementary Figure 2.
Kaplan–Meier survival analysis of the overall survival among patients with severe emphysema following treatment with EBV.
Additional file 7: Supplementary Figure 3.
Kaplan–Meier survival curves for COPD acute exacerbation in patients with severe emphysema who underwent treatment with EBV.
Additional file 8: Supplementary Figure 4.
Changes in FEV1 over 300 days in patients with severe emphysema.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huh, JY., Jeong, BH., Yoon, H.i. et al. Endobronchial valves for emphysema and persistent air-leak: 10-year experience in an Asian country. BMC Pulm Med 24, 162 (2024). https://doi.org/10.1186/s12890-024-02982-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-02982-2