Abstract
Background
Exposure to wood dust can cause respiratory symptoms, like cough, phlegm, breathlessness, and chest pain, reduce lung function.
Objective
The objective of the study was to assess the prevalence of respiratory symptoms and associated factors among woodwork workers in Bahir-Dar city, Ethiopia.
Methods
A comparative cross-sectional study was employed among 229 exposed and 228 unexposed groups. Participants for the study were selected using simple random sampling technique. The chronic respiratory symptoms were assessed using a questionnaire adopted from the American Thoracic Society. The data was entered using Epi-Data version 4.6 and export to SPSS version 22 for analysis. Poisson regression, Multivariate linear regression and multivariable logistic regression analysis were used to identify factors associated with woodworkers, general population and in pooled analysis.
Result
The prevalence of having at least one chronic respiratory symptom was higher among exposed group (59.4%) than unexposed group (18.0%) with PR = 3.03(95%CI: 2.45, 4.45). In woodworker; Not taking health and safety training(5.15,95%(CI:1.93–13.76),primary educational(3.85,95%,CI:(1.1,13.47), not using Mask(6.38, 95%CI:(2.69–15.76) & number of families(3.05,95%,CI:1.04–9.028), In general population; Number of family members(2.75, 95%CI:1.1–7.19)& lower monthly income (3.3, 95%CI: (1.49–7.4), and In pooled analysis; wood dust exposure status 14.36 95%, CI:(7.6–27.00),primary education(2.93,95%CI:1.24–6.92), number of families(3.46,95%CI:1.8–6.64), lower monthly income(2.13,95%CI:1.19–3.81), & smoking (6.65, 95%CI:1.19–36.9) were associated with respiratory symptom.
Conclusion
Prevalence of respiratory symptoms was higher among exposed group than unexposed group. Reduced wood dust exposure status, Provision of occupational safety and health training, use of respiratory protective devices is recommended to reduce respiratory symptoms among woodwork workers.
Similar content being viewed by others
Background
Wood dust and its components are known to cause respiratory symptoms and have sensitizing and irritating properties to mucous membranes [1]. Work-related respiratory illnesses are the major global public health problems, accounting for up to 30% of all work-related diseases and up to 50% among workers in high dust-generating industries or work activities [2]. Inhaling wood dust and its various components cause respiratory disorders and irritates the mucous membrane of the airways, which are exhibited by a variety of signs and symptoms in exposed workers [3]. Workers in the woodwork industry are at high risk of being exposed to wood dust, and the development of various respiratory symptoms [4].
The European Union and Occupational Safety and Health Administration(OSHA) regulations stipulate a marginal value for wood dust exposure level [5], and such regulation is single 8-hour time weighted average(TWA) of 5 mg/m3 and a short term exposure limit(STEL) of 10 mg/m3 for all hard wood and soft wood dusts [6]. Occupational exposure to wood dust has been linked to a variety of respiratory disorders, including asthma, allergic rhinitis, chronic bronchitis, and lung function impairment [4, 7].
Two million woodworkers around the world are exposed to wood dust every day, and increase prevalence of respiratory tract diseases [8]. Wood dust is produced during the process of the wood furniture making which involves sanding, sawing and drilling either manually or with machines [9],and globally the prevalence of respiratory disease in such occupation is reported in the range of 5.6–18%, and in Africa is between 3 and 7% [10]. Some studies showed a high prevalence of respiratory symptoms like cough, phlegm, chest tightness, wheezing, and breathlessness among exposed group relative to unexposed groups [11,12,13]. Similar studies also reported a high prevalence of respiratory symptoms among wood dust exposed group [7, 14,15,16].
Respiratory symptoms are associated with different factors such as socio-demographic variables like gender [17,18,19], Socio-economic status, level of education, types of occupation [20,21,22], family size [23], family history of respiratory illness [19, 24, 25], behavioral factors like smoking [19, 26, 27], working condition factors like duration of exposure [28], and working department [17], utilization of personal protective equipment such as dust mask [22], and effective housekeeping and exhaust ventilation [14, 29], health and safety training [21]. But there is limited evidence on the prevalence of respiratory symptoms and associated factors among woodwork workers in Ethiopia, especially in the Bahir Dar City. Therefore, this study aimed to assess the prevalence of work-related respiratory symptoms and associated factors among woodworkers in Bahir-Dar city, Ethiopia.
Methods and materials
Study design and period
A comparative cross-sectional study was conducted in Bahir Dar city among woodwork workers from March to April 2021.
Study area
The study was conducted in Bihar Dar city, which is the capital city of Amhara regional State, and it is found 565 km from Addis Ababa, the capital city of Ethiopia. Based on the Central Statistical Agency of Ethiopia’s (CSA) 2007 Census, the Bahir Dar Special Zone had a total population of 221,991, of which 108,456 were male and 113,535 were female; 180,174 or 81.16% are urban residents, the rest living in rural kebeles around Bahir Dar [30]. In the city, there are 280 woodwork industries with a total of 1600 workers (in average there were 6–10 workers in one woodwork industry. The common types of wood that used for furniture making were Wanza (local language) tid(timber), and medium density fiber board(mdf).
The woodwork production process begins with logwood, from which various raw materials are stoked, and it is distributed to the sawmill, which splits the wood to the required size. After splitting the material to the required size, the moisture content is lost through drying to produce a good product. The wood will then be cut and split using a cutter saw or a circular saw depending on the size product required. Then, sanding is performed to obtain components that have been refined with the same size and smoothness prior to the assembling process, which involves joining different components together to produce finished goods. The final process in the woodworking industry is finishing, which is layering wood surface with the purpose of making it beautiful, and products move to packaging area to add some accessories like key, handle, real, soon (Fig. 1).
Source and study population
This study includes all woodwork workers (exposed group) who had worked 1 year and above in the woodwork industries, and the general population (unexposed group) who live nearby with those factories around 2.5-km from the woodwork industries and had never worked in the woodwork industry [31].
Inclusion criteria
In this study, participants with 1 year and above work experience were included in the study.
Exclusion criteria
Both woodwork workers (exposed) and the general population (unexposed groups) with a history of pulmonary disease, abdominal tumor, heart failure, or recent surgery or thorax procedures were excluded from this study. Unexposed groups were exclude that had wood dust exposure history.
Sample size determination
The sample size was done for both prevalence and associated factors. For the prevalence, sample size was done using the double population proportion formula, by considering the proportion of respiratory symptoms for the exposed(44.2%), and unexposed(14.3%) groups in the manufacturing industry [3], 95%CI, and 80% power respectively.
n 1 = n 2 = (Zα/2 + Zβ)2 × [p(1 − p1) + (p2(1 − p2)]
The sample size was 32 exposed and 32 non-exposed groups and after adding a 10% non-response rate, the total sample size was 70 for both populations [3]. The sample size for associated factors was done using Open Epi info software version 7,by considering 95% confidence interval, and 80% power, ratio exposed to unexposed group is 1:1, and factors from the previous study; smoking and proportion among exposed (7.3%) and unexposed group (3.8%) [2] and the sample size was 348 for both groups. The other factor was occupational safety and health training with the proportion of exposed (8%) and unexposed(3.8%) with 10% non –response rate, the total sample size was 472 (236 for exposed and 236 unexposed groups [2]. Therefore, the sample size for factors is higher than a sample size of the prevalence and the final sample size for this study was 472.
Sampling procedure
In Bahir Dar City, there are nine sub-cities, and from the nine sub-cities, by using lottery method three sub cities such as Dagimawie Minilk, Fasilo, and Tewodrose sub-cities, with a total of 107 woodwork factories were selected. Samples in the exposed and unexposed groups were proportional allocated and simple random sampling technique was used to select study participants. The study population from the general community was recruited from the selected sub-cities found around 2.5 k meters from woodwork factories (assuming less wood dust exposure).
Data collection procedure
The questionnaire was adapted and modified from a validated standardized questionnaire from the American thoracic society(ATS) to assess respiratory symptoms in adult populations [32]. The questionnaire had the following components: Socio-demographic characteristics, respiratory symptoms, family history of respiratory diseases, behavioral factors including housing condition with types of energy used for cooking, and working conditions factors. The data was collected through face-to-face interviews. Observational checklist also was used to see safe work practices like respiratory protective device utilization and workplace ventilation.
Data quality assurance
The quality of data was assured through careful design, languge translation, and retranslation of the questionnaire. Two-days training were given for data collectors and supervisors. A pre-test was carried out before the actual data collection in Geshi- Abay sub city to check the competency of the data collectors, and the reliability and validity of the data collection tools and necessary corrections were taken accordingly. Data were collected by five public health professionals.
Study variable
Dependent variables
Chronic respiratory symptoms.
Independent variables
There are different factors that affect respiratory symptom including socio-demographic variables (age, sex, education, marital status, income level), previous and family history of respiratory disease, behavioral factors (smoking habit, PPE, types of energy source at home), work-related factors including working condition factors such as wood dust exposure status, and OSH training, work experience, work place ventilation, periodic medical check-up & pre-medication.
Operational definition
Chronic respiratory symptoms
Workers with one or more symptoms of cough, phlegm, wheezing, chest tightness, and breathlessness last at least 3 months in 1 year [3].
Past chronic respiratory disease
One or more respiratory diseases like chronic bronchitis, emphysema, tuberculosis (TB), heart disease, chronic sinus, asthma, and lung cancer that could be developed before the current working position and identified by physicians [19].
Cough
In this study, Cough is defined as it occurs 4 to 6 times a day for most days of the week (≥ 4 days) for at least 3 months a year [21].
Phlegm
Participants were considered to have chronic Phlegm if they answered yes/ to at least one of the following four questions; Phlegm first thing in the morning, Phlegm during the day or night, phlegm as much as four to six times a day in a week or phlegm for most days as much as three consecutive months during the year [14].
Breathlessness
Participants were considered to have chronic breathlessness if he/she was troubled by shortness of breath when hurrying on level ground or walking up a slight hill, or getting shortness of breath when walking at /her own pace on level ground [33].
Chest pain
Chest discomfort that has held of phlegm workers’ jobs in the past 1 year or above [17].
Wheeze
Whistling breathing during the respiratory cycle perceived by the respondents at least 3 months in a year [3].
Current smokers
Workers who smoked at the time of the study or someone who smokes cigarettes every day or every few days) [34].
Ever smoker
A person who smoked at least 100 cigarettes in his entire life [19].
Wood dust
Wood dust is an accumulation of any wood particulate that is generated during the processing or handling of wood. When this dust becomes airborne it may be inhaled by workers [35, 36].
Data management and analysis procedure
The data were cleaned and checked using frequency table and entered into the Epi-Data version 4.6,EpiData Association, Denmark, Europe [37] and exported to SPSS version 22 for further analysis. Descriptive statistics, Poisson regression models with robust variance were employed to estimate the prevalence ratios (PR) and corresponding 95% confidence intervals (CI) [38]. Logistic regression analysis was used to identify whether exposure variables are significantly associated with outcome variables or not. Thus, variables in the bi-variable analysis with p ≤ 0.2 were included in the multivariable analysis by adjusting confounding variables. We considered variables as significant independent factors based on Adjusted Odds Ratio (AOR) with 95% CI and P-value of < 0.05. The P-value of < 0.05 was considered as statistically significant.
Results
Socio-demographic characteristics of the study participants
A total of 457(229 exposed and 228 unexposed groups) respondents with a response rate of 96.8% participated. The mean ± (SD) age of the participant among exposed and unexposed groups was 33 ± 6 and 35 ± 7 years respectively. The majority of the study participants were males. Less than half (43.2%) of the exposed group have secondary level education, and more than a quarter (31.1%) of the unexposed group attend secondary educational level (Table 1).
Behavioral characteristics of study participants
In this study, nearly two third(65.5%) of exposed groups and the majority(83.8%) of the unexposed groups used electricity as the source of energy at home, and 8.3% of exposed groups and 1.3% of unexposed groups ever cigarette smokers (Table 2).
Work-related characteristics of study participants
More than half (58.5%) of woodwork workers had 5 and below years of work experience. The average (±SD) work experience of woodworkers in woodwork industry was 5.62 ± 3.37 years. The majority (84.7%) of workers had worked 6–8 hours per day. One-fourth 58(25.3%) of participants had taken occupational health and safety training. Almost 40 % (39.7%) of participant had utilized personal protective equipment and the rest were not used personal protective equipment.
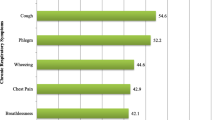
Prevalence of chronic respiratory symptoms
After Adjusting, sex, age, educational status, monthly income, work experience, working hours per day, dust exposure in previous employments, biofuel energy use, use of PPE, and OSH training, and the prevalence of at least one chronic respiratory symptom was higher among exposed group (59.4%) than unexposed group (18.0%)(PR = 3.03(95%CI: 2.45, 4.45). The prevalence ratio of cough (PR = 2.37(1.56, 3.6), phlegm (PR = 2.39(1.46, 3.89), wheezing (PR = 7.3(3.17, 16.8), Shortness of breath (PR = 4.5(3.01, 6.86), and Chest pin (PR = 4.97(2.45, 4.45). The prevalence of all the respiratory symptoms was high significantly for the exposed group than non-exposed groups (p-value < 0.05) (Table 3).
Factors association with respiratory symptoms among woodwork workers (model I)
Factors such as sex, income, age, marital status, and educational level, and family size, use of PPE, cigarette smoking, work experience, occupational health, and safety training were found candidate (p-value ≤0.2) for multivariable logistic regression model. But, variables such as use of respiratory protective equipment (RPE), educational status, family size, and, occupational health and safety training were found associated with respiratory symptoms among woodwork workers in multivariable logistic regression model.
The respiratory health symptoms was 5.15 times higher among woodwork workers who did not take occupational safety and health training when compared to workers who did take occupational safety and health training (AOR = 5.15, 95%CI: 1.93–13.76).The respiratory health symptoms among woodworkers who did not use respiratory protective equipment was 1.79 times higher than workers who used respiratory protective equipment (AOR = 6.38, 95%(CI: 2.69–15.76). The respiratory health symptom among participants with lower education was 3.85 times higher when compared to those participants with diploma and above education (AOR = 3.85(95%CI: 1.10–13.47). The respiratory symptoms among woodworkers who had more than 3 family members was 3.06 times higher than workers who had less than or equal to 3 family members (AOR = 3.06, 95%CI: 1.04–9.02) Table 4).
Factors association with respiratory symptoms among unexposed group (model II)
Risk factors like sex, family size, educational status, and monthly income, were candidate (p value≤0.2) for multivariable logistic regression. But, variables such as monthly income and family size were associated with respiratory symptoms among the general population. The respiratory health symptom was 2.75 times higher among participants who had more than three family members when compared to participants who had less than three family members (AOR = 2.75, 95%, CI: (1.1–7.19).The respiratory health symptom was 3.3 times higher in participants who had lower monthly income when compared to participants who had higher monthly income (AOR = 3.3, 95%CI: (1.49–7.4) (Table 5).
Factors association with exposed group and unexposed group (model III)
In a pooled model, sex, age, wood dust exposure status, family size, marital status, educational level, income, smoking status were candidate (p value≤0.2) for multivariable logistic regression analysis. But, variables such as wood dust exposure status, family size, income, and educational level and Ever smoker were significantly associated with the respiratory symptoms in poled analysis.
The respiratory health symptom among exposed group was 14.36 times higher among exposed group when compared to unexposed groups (AOR = 14.36 95%CI: (7.6–27.0).The respiratory health symptom was 3.46 times higher among participants who had more than three family members when compared to participants who had less than three family members (AOR = 3.46, 95%, CI: (1.8–6.64). The respiratory health symptom among participants who had family size more than three was 3.46 times that of participants with less than three family sizes(AOR = 3.46, 95%CI:(1.8–6.64)). The respiratory health symptom among participants with lower education was 2.93 times higher when compared to those participants with diploma and above education (AOR = 2.93(95%CI: 1.24–6.92). The respiratory health symptom among ever smokers was 6.65 times higher when compared to non-smokers (AOR = 6.65, 95%CI: (1.19–36.9) (Table 6).
Discussion
In this study, the overall prevalence of respiratory symptom was higher among the exposed group (59.4%) than unexposed groups (18.0%).This finding is similar to other studies conducted in Europe, Macedonia, [11], Iran [12], Thailand [14], Nigeria [16], and Ethiopia [2, 7]. All of these studies reported that the prevalence of respiratory symptom was higher among the exposed group than in the unexposed groups. This might be due to exposure to dust from woodwork being higher among exposed group than in unexposed groups. Hence, occupational exposure to wood dust has been linked with respiratory symptoms among woodworkers, and the presence of higher prevalence of respiratory symptoms compared with the unexposed groups. On the other hand, this study found higher prevalence of chest pain (13.5% vs 10.8%), phlegm (15.2% vs5.4%), wheezing (8%), and breathlessness (10.5%vs 8.1%) than a study conducted in Europe among woodwork workers [21]. The possible reasons might be due to difference in the implementation of effective dust control measures like natural and artificial exhaust ventilation and utilization of personal protective equipment (PPE) such as dust mask. But the findings of this study was lower than a study conducted in India [39]. The difference might be due to work experience (duration of exposure), utilization of personal protective equipment, and difference in the wood dust exposure level of woodwork workers between the two countries.
In this study associated factor like worker’s exposure status (exposed and unexposed), family size, income, OSH training, use of PPE, and smoking status were significantly associated with respiratory symptoms. In this study the respiratory symptom was more likely among exposed group when compared to unexposed group, and this finding is in agreement with studies conducted in Iran among woodwork workers [40], and Indian sawmill workers [39], and the respiratory symptoms were significantly more prevalent among exposed groups than unexposed group [40].
In this study, the respiratory symptoms were higher among study participants having more than three family members when compared to participants who had less than or equal to 3 family members. This finding is in line with a study conducted in New Zealand [23], and the possible justification might be due to different characteristics of family members, insufficient ventilation, increasing exposure to the infectious agent during social life, overcrowding and difference in lifestyles. Moreover, other factors related to respiratory symptoms was cigarette smoking and were higher among ever smokers when compared to non-smokers and this finding is consistent with studies conducted in Spain [41], South Carolina, US [26], and Iran [42].
In this study, the other significant variable was occupational safety and health-related training, and the probability of having respiratory symptoms was higher among study participants who did not take occupational health and safety training when compared to workers who did take occupational health and safety training. This finding is consistent with other studies conducted in Egypt, and Ethiopia [2, 21, 43]. The possible justification is that training about occupational safety and health improves workers’ attitudes towards respiratory health issues and provides skills and knowledge to implement prevention strategies for occupational hazards (wood dust) in their workplaces.
In this study the respiratory symptoms was more likely among woodworker who did not use respiratory protective equipment (RPE) when compared to workers who used respiratory protective equipment(RPE). This finding is similar to studies carried out in Thailand and Ethiopia [14, 22]. On the other hand, this finding contradicts the finding from the Dejen cement factory, in Ethiopia [21]. This difference could be due to the differences in the amount and kind of dust produced and the quality of respiratory protective equipment provided.
This study also found that the respiratory symptoms of woodworkers were linked with a lower educational level, and this finding was supported by a study performed in Ethiopia, [21] which described that respiratory symptoms were associated with a lower educational level. This might be because higher education provides individuals with skills and knowledge about how to safeguard their health from work-related exposure to health hazards [21].
Moreover, in this study participants with better household income were fewer to have respiratory symptoms when compared to workers with low house hold income. The possible justification might be due to participants with better household income have better living standards and better quality of life, and reduced respiratory symptoms.
Limitation of study
One of the limitations of this study is the healthy workers effect; workers who developed the symptoms may have quit the job. The use of the questionnaire method was also another limitation of this study because it may cause participants to recall bias and interviewer bias.
Conclusion
The prevalence of respiratory symptom was higher among exposed group when compared to the unexposed group. In pooled analysis, wood dust exposure status, having more than three family number, and cigarette smoking in the past were associated factors for respiratory symptom. Good work practice to reduce wood dust generation at the source is needed, OSH training, modifying behavioral factors and use of respiratory protective devices are recommended to reduce wood dust exposure and respiratory symptoms among woodwork workers.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Määttä J, Lehto M, Leino M, Tillander S, Haapakoski R, Majuri M-L, et al. Mechanisms of particle-induced pulmonary inflammation in a mouse model: exposure to wood dust. Toxicol Sci. 2006;93(1):96–104.
Awoke TY, Takele AK, Mekonnen WT, Abaya SW, Zele YT, Alemseged EA, et al. Assessment of dust exposure and chronic respiratory symptoms among workers in medium scale woodwork factories in Ethiopia; a cross sectional study. BMC Public Health. 2021;21(1):1–12.
Fentie D, Mulat E, Reta W. Assessment of respiratory symptoms among woodworkers in Jimma town, Southwest Ethiopia, a comparative cross-sectional study. Biomed J Scient Tech Res. 2019;18(2):13425–30.
Jacobsen G, Schaumburg I, Sigsgaard T, Schlunssen V. Non-malignant respiratory diseases and occupational exposure to wood dust. Part II. Dry wood industry. Ann Agricul Environ Med. 2010;17(1):29–44.
Mračková E, Krišťák Ľ, Kučerka M, Gaff M, Gajtanska M. Creation of wood dust during wood processing: size analysis, dust separation, and occupational health. BioResources. 2016;11(1):209–22.
Tang J, Wang J, Pei Y, Dereje SB, Chen Q, Yan N, et al. How adverse and benevolent childhood experiences influence depression and suicidal ideation in Chinese undergraduates: a latent class analysis. Environ Health Prev Med. 2023;28:17.
Demissie WR. Effect of occupational wood dust on pulmonary function among woodworkers in Jimma town, Southwest Ethiopia, a comparative cross sectional study. EC Pulmonol Respirat Med. 2019;8:587–93.
Bentum L, Brobbey LK, Adjei RO, Osei-Tutu P. Awareness of occupational hazards, and attitudes and practices towards the use of personal protective equipment among informal woodworkers: the case of the Sokoban Wood Village in Ghana. Int J Occup Saf Ergon. 2022;28(3):1690–8.
Yusof M, Hod R, Aizuddin A, Samsuddin N. Health effects of Hevea Brasiliensis wood dust exposure among furniture factory workers. Online J Health Allied Sci. 2019;18(3):10.
Chamba P, Nunes E. Work-related asthma among workers in the wood-processing industry: a review: allergies in the workplace. Curr Aller Clin Immunol. 2016;29(2):110–7.
Bislimovska D, Petrovska S, Minov J. Respiratory symptoms and lung function in never-smoking male workers exposed to hardwood dust. Open access Macedonian j med sci. 2015;3(3):500.
Neghab M, Jabari Z, Shouroki FK. Functional disorders of the lung and symptoms of respiratory disease associated with occupational inhalation exposure to wood dust in Iran. Epidemiol health. 2018:40.
Alonso-Sardón M, Chamorro A-J, Hernández-García I, Iglesias-de-Sena H, Martín-Rodero H, Herrera C, et al. Association between occupational exposure to wood dust and cancer: a systematic review and meta-analysis. PLoS One. 2015;10(7):e0133024.
Soongkhang I, Laohasiriwong W. Respiratory tract problems among wood furniture manufacturing factory workers in the northeast of Thailand. Kathmandu University Med J. 2015;13(2):125–9.
Thepaksorn P, Fadrilan-Camacho VFF, Siriwong W. Respiratory symptoms and ventilatory function defects among Para rubber wood sawmill workers in the south of Thailand. Human Ecolog Risk Assess: An Int J. 2017;23(4):788–97.
Tobin E, Ediagbonya T, Okojie O, Asogun D. Occupational exposure to wood dust and respiratory health status of sawmill workers in south-South Nigeria. J Pollut Effect Control. 2016:1–6.
Wang X, Eisen E, Zhang H, Sun B, Dai H, Pan L, et al. Respiratory symptoms and cotton dust exposure; results of a 15 year follow up observation. Occup Environ Med. 2003;60(12):935–41.
Chaiear N, Ngoencharee J, Saejiw N. Respiratory symptoms and pulmonary function among Workers in a Rubber Wood Sawmill Factory in Thailand. Am J Public Health. 2018;6(2):65–71.
Asfaw S, Enquselassie F, Tefera Y, Gizaw M, Wakuma S, Woldemariam M. Determinants of chronic respiratory symptoms among pharmaceutical factory workers. J Trop Med. 2018. https://doi.org/10.1155/2018/3815689.
Kanervisto M, Vasankari T, Laitinen T, Heliövaara M, Jousilahti P, Saarelainen S. Low socioeconomic status is associated with chronic obstructive airway diseases. Respir Med. 2011;105(8):1140–6.
Gizaw Z, Yifred B, Tadesse T. Chronic respiratory symptoms and associated factors among cement factory workers in Dejen town, Amhara regional state, Ethiopia, 2015. Multidiscip respirat med. 2016;11(1):1–9.
Kifle M, Gebremariam B, Alemu K, Woldeyohannes SM. Prevalence and factors associated with respiratory symptoms among Bahir Dar textile industry workers, Amhara region. Ethiopia Environ Health Insights. 2020;14:1178630220965933.
Wickens KL, Crane J, Kemp TJ, Lewis SJ, D'Souza WJ, Sawyer GM, et al. Family size, infections, and asthma prevalence in New Zealand children. Epidemiol. 1999;699-705.
García-Sancho C, Buendía-Roldán I, Fernández-Plata MR, Navarro C, Pérez-Padilla R, Vargas MH, et al. Familial pulmonary fibrosis is the strongest risk factor for idiopathic pulmonary fibrosis. Respir Med. 2011;105(12):1902–7.
Lindström M, Jönsson E, Kotaniemi J, Lundbäck B. Smoking, respiratory symptoms, and diseases: a comparative study between northern Sweden and northern Finland: report from the FinEsS study. Chest. 2001;119(3):852–61.
Liu Y, Pleasants RA, Croft JB, Wheaton AG, Heidari K, Malarcher AM, et al. Smoking duration, respiratory symptoms, and COPD in adults aged≥ 45 years with a smoking history. Int J Chronic Obstruct Pulmon Disease. 2015;10:1409.
Ugheoke A, Ebomoyi M, Iyawe V. Influence of smoking on respiratory symptoms and lung function indices in sawmill workers in Benin City, Nigeria. Nigerian J Physiol Sci. 2006;21(1-2).
Aguwa E, Okeke TA, Asuza M. The prevalence of occupational asthma and rhinitis among woodworkers in South-Eastern Nigeria. Tanzania J Health Res. 2007;9(1):52–5.
Fong YL, Mahfar M. Relationship between occupational stress and turnover intention among employees in a furniture manufacturing company in Selangor. Jurnal Teknologi. 2013;64(1).
Guadu T, Shite A, Chanie M, Bogale B, Fentahun T. Assessment of knowledge, attitude and practices about rabies and associated factors: in the case of Bahir Dar town. Global Veterin. 2014;13(3):348–54.
Wami SD, Chercos DH, Dessie A, Gizaw Z, Getachew A, Hambisa T, et al. Cotton dust exposure and self-reported respiratory symptoms among textile factory workers in Northwest Ethiopia: a comparative cross-sectional study. J Occupation Med Toxicol. 2018;13(1):1–7.
Eisner MD, Anthonisen N, Coultas D, Kuenzli N, Perez-Padilla R, Postma D, et al. An official American Thoracic Society public policy statement: novel risk factors and the global burden of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;182(5):693–718.
Abaya SW, Bråtveit M, Deressa W, Kumie A, Moen BE. Reduced lung function among workers in primary coffee processing factories in Ethiopia: a cross sectional study. Int J Environ Res Public Health. 2018;15(11):2415.
Ryan H, Trosclair A, Gfroerer J. Adult current smoking: differences in definitions and prevalence estimates—NHIS and NSDUH, 2008. J Environ Public Health. 2012. https://doi.org/10.1155/2012/918368.
Proto AR, Zimbalatti G, Negri M. The measurement and distribution of wood dust. J Agricult Eng. 2010;41(1):25–31.
Alemseged EA, Takele AK, Zele Y, Abaya SW, Kiros KG, Mehari M, et al. Assessment of chronic respiratory health symptoms and associated factors among flour mill factory Workers in Addis Ababa, Ethiopia, 2019: a cross-sectional study. J Asthma Allerg. 2020;13:483.
Christiansen TB, Lauritsen JM, editors. EpiData - Comprehensive Data Management and Basic Statistical Analysis System. Odense: EpiData Association; 2010. http://www.epidata.dk.
Barros AJD, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empiri cal comparison of models that directly estimate the pre valence ratio. BMC Med Res Methodol. 2003;3:21. https://doi.org/10.1186/1471-2288-3-21.
Asri AA, Anua SM, Safuan S, Shakri SF, Hussein NS, Ishak NS, Zin RA. Inhalable Dust Exposure and Lung Function Among Rice Mill, Sawmill and Furniture Factory Workers. Malays J Med Health Sci. 2020;16.
Neghab M, Jabari Z, Kargar SF. Functional disorders of the lung and symptoms of respiratory disease associated with occupational inhalation exposure to wood dust in Iran. Epidemiol Health. 2018;40:e2018031.
Isabel U, Alberto C, María QJ, Nerea M, Xavier B, Jordi S, et al. Smoking habit, respiratory symptoms and lung function in young adults. Eur J Pub Health. 2005;15(2):160–5.
Younesian M, Homayoun VJ, Asghari F, Forouzanfar M, Hosseinpour AR, Farhoud D. Smoking-Related Respiratory Symptoms In Tehran. In: A Cross-Sectional Study; 2008.
Shafik SA, El-Mohsen A. Occupational health: health promotion program to improve health workers in Tourah cement factory. J Am Sci. 2012;8(3):486–96.
Acknowledgments
We authors would like to acknowledge data collectors, supervisors, and study participants.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
G.A. conceived the research idea and contributed to the data collection, data analysis, and interpretations of the results. Z.G. and MG contributed to data analysis and result interpretation. E.A. contributed to the manuscript write-up. All authors have commented, edited, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was conducted respecting the Helsinki Declaration of research ethics for studies with human participants and the ethical soundness of the research was approved by the Ethical Review Committee at the Institute of Public Health, College of Medicine and Health Science, the University of Gondar with official letter Ref No/IPH/1472/2013 and date 15//07/2021. Written informed consent was obtained from each study participant and confidentiality was also kept using an unknown identification code.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abateneh, G., Gizaw, Z., Gebrehiwot, M. et al. Prevalence of chronic respiratory symptoms and associated factors among woodwork workers in Bahir Dar City, Ethiopia; a comparative cross-sectional study. BMC Pulm Med 24, 3 (2024). https://doi.org/10.1186/s12890-023-02812-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02812-x