Abstract
Background
The risk factors for osteoporosis and its prognostic value in patients with bronchiectasis is not well characterized. We explored the risk factors for osteoporosis and its prognostic impact in hospitalized non-cystic fibrosis bronchiectasis (NCFB) patients in Southeast China.
Methods
This observational cohort study consecutively enrolled 179 hospitalized patients with NCFB bronchiectasis between 2017 and 2021. The risk factors and the impact of osteoporosis on all-cause mortality were assessed.
Results
21.2% (38/179) of hospitalized NCFB patients were diagnosed with osteoporosis. Patients with osteoporosis had more severe symptoms (assessed by chronic airway assessment test, CAT, median 22 vs. 17, P = 0.017), poorer quality of life (assessed by St. George Respiratory Questionnaires, SQRC, median 42 vs. 27, P = 0.007), more severe disease stage (assessed by bronchiectasis severity index, BSI, median 14 vs. 11, P = 0.02), more comorbidities (assessed by Bronchiectasis Aetiology Comorbidity Index, BACI, median 5 vs. 4, P = 0.021) than patients without. Age, female sex, anemia, post-infection, and history of regular inhaled corticosteroid treatment were independent risk factors for osteoporosis in those patients. 21 patients (11.7%) died over a median follow-up period of 32 months. The all-cause mortality in NCFB patients with osteoporosis [28.94% (11/38)] was significantly higher than those without osteoporosis [7.09% (10/141)] [hazard ratio (HR) 5.34, 95% confidence interval (CI) 2.26–12.67, P < 0.001]. After adjusting for BSI and other confounding factors, osteoporosis was still independently associated with all-cause mortality in hospitalized NCFB patients (HR 4.29, 95% CI 1.75–10.49, P < 0.001).
Conclusions
Osteoporosis had an independent effect on all-cause mortality in hospitalized NCFB patients. Management of comorbidities, including bone health, is a critical aspect of treating NCFB patients.
Similar content being viewed by others
Background
In the Asian population, non-cystic fibrosis bronchiectasis (NCFB) might be one of the most common but heterogeneous chronic respiratory diseases apart from chronic obstructive pulmonary disease (COPD) and asthma. The prevalence of bronchiectasis in Korea was 9.1% in adults [1]. Although the prevalence of bronchiectasis among the population over 40 years in China was estimated at 1.2% [2], the actual prevalence may be higher because only diagnosed patients were included. Patients with bronchiectasis frequently have other comorbid conditions, which contributes to increased healthcare and socioeconomic burden and worsens the quality of life, exacerbation frequency, lung function, and mortality risk [3]. Similar to asthma and COPD, different comorbidities can significantly impact pulmonary and extrapulmonary manifestations of bronchiectasis, disease severity, prognosis, and therapeutic management. However, despite the high prevalence of comorbid conditions in patients with bronchiectasis, their specific impact on clinical outcomes and the natural history of the disease is not well characterized. Besides, the current clinical guidelines barely include recommendations about managing these conditions due to the paucity of scientific evidence.
Osteoporosis, among the major systemic comorbidities of COPD, is related to systemic inflammatory response, impaired lung function, frequent acute exacerbations, and reduced survival of patients with COPD [4]. Common risk factors for osteoporosis and COPD include age, female sex, early menopause, smoking, alcohol consumption, inadequate vitamin D intake, systemic inflammatory response, low body mass index (BMI), and corticosteroid use [5]. Moreover, as an essential mechanism of osteoporosis, vitamin D deficiency strongly correlates with various health outcomes, including all-cause mortality [6, 7]. The effect of vitamin D on the lungs has a robust scientific rationale; its immunomodulatory, anti-inflammatory, and anti-infective properties have been demonstrated in patients with community-acquired infection, acute respiratory failure, and lung transplantation recipients [8].
Bronchiectasis shares many clinical and pathophysiological characteristics with COPD, including an enhanced local and systemic inflammatory milieu. Besides, recurrent infection leading to permanent bronchi dilation is the primary pathophysiological mechanism of bronchiectasis. In a multicenter cohort study in Europe that evaluated the impact of different comorbidities in bronchiectasis, osteoporosis was the fifth most prevalent comorbidity in NCFB patients [9]. Recent retrospective and cross-sectional studies have also shown a higher prevalence of osteoporosis in bronchiectasis patients compared with the general population [10, 11]. However, the risk factors for osteoporosis and the prognostic value of osteoporosis in bronchiectasis patients are not well investigated.
This study aimed to assess the prognostic impact of osteoporosis in hospitalized NCFB patients and identify the clinical risk factors for osteoporosis in these patients.
Methods
An observational cohort study of NCFB patients was conducted at the pulmonary and critical care department of the Longyan First Affiliated Hospital of Fujian Medical University in Southeast China from September 2017 to December 2021. Hospitalized patients with a diagnosis of bronchiectasis based on high-resolution computed tomography (HRCT) and respiratory symptoms were enrolled in the study according to the 2012 Expert consensus on diagnosing and treating adult bronchiectasis in China [12]. Exclusion criteria were: (1) cystic fibrosis bronchiectasis; (2) active tuberculosis or nontuberculous mycobacteria infection; (3) malignant tumor; (4) severe immunosuppression (such as solid-organ or bone marrow transplantation, human immunodeficiency virus infection (HIV), or receiving chemotherapy or other immunosuppressive drugs (≥ 20 mg prednisone per day for > 2 weeks); (5) bronchiectasis secondary to interstitial lung disease; and (6) tracheobronchial foreign body. All patients provided written informed consent (Ethical Review of Clinical Research from Longyan First Hospital affiliated with Fujian Medical University).
Clinical data including demographic data, comorbidity (other pulmonary diseases and non-pulmonary diseases), smoking, BMI, clinical symptoms, history of previous hospitalization and exacerbation, possible etiology, radiographic extension (modified Reiff score was calculated as tubular, 1 point; varicose, 2 points; and cystic, 3 points; the total score (six lobes) ranged from 0 to 18 points), FEV1% to predict value (FEV1% pred) and chronic respiratory infection, were collected. The severity of bronchiectasis was assessed using Bronchiectasis Severity Index (BSI) scores [13]. The Chronic airway assessment test (CAT) [14] and St. George's Respiratory Questionnaires were also completed by patients. The Bronchiectasis Aetiology Comorbidity Index (BACI) was calculated according to the derivation of the BACI and point allocation by McDonnell [9]. Patients were followed-up remotely (telephonically or via an electronic form) to record symptoms, death, and treatment details for 3–6 months until June 2022. Macrolides treatment was defined as continuing the medication for at least 3 months.
Osteoporosis was diagnosed based on any of the following criteria: (1) fragile fracture of the hip or vertebra; (2) bone mineral density (BMD) of axial bone or the distal third of the radius measured by Dual-energy X-ray absorption (DEXA) as T < − 2.5; (3) Bone mineral density measurements consistent with low bone mass (− 2.5 < T < − 1.0), with fragile fractures of the proximal humerus, pelvis, or distal forearm [15, 16] Other comorbidities recorded were COPD, asthma, pulmonary artery hypertension (PAH), sinusitis, cardiovascular diseases (CVD), cerebrovascular diseases, peripheral vascular disease (PVD), hypertension (HT), diabetes, hypoxemia, kidney diseases, liver diseases, connective tissue disease (CTD), and gastroesophageal reflux disease (GERD). We recorded COPD as comorbidity similar to other studies [9]; bronchiectasis associated with COPD was defined as the presence of a history of smoking at least 10 pack-years or Biofuel exposure, with airflow obstruction (FEV1/FVC ratio < 0.7) according to the Global Initiative for Chronic Obstructive Lung Disease recommendations.
Statistical analysis
Statistical analysis was performed using the SAS 9.4 software (SAS Institute, Inc., Cary, NC, USA). Categorical variables were expressed as frequency (%) and compared using the Chi-squared test or Fisher's exact probability method. Continuous variables were expressed by mean ± SD or median (P25, P75). Comparisons among groups were analyzed using the ANOVA or Rank sum tests. Factors with statistically significant differences in the univariate analysis were included in multivariate analysis using Modified Poisson regression analysis to identify risk factors for osteoporosis in hospitalized NCFB patients. Kaplan–Meier curve was constructed to illustrate survival data, and Cox proportional hazard regression model was used for univariate and multivariable mortality analysis to estimate hazard ratios (HRs) and their 95% confidence intervals (CIs). Because the BSI is a comprehensive index including 9 clinical parameters mentioned above (age, BMI, FEV1%pred, history of exacerbation and hospitalization, mMRC score, chronic infection, dilation, imaging) and given the limited sample size of our study, only the BSI score and comorbidities, which were significantly related to survival in univariate analysis, were introduced into the multivariate survival analysis. For all statistical analyses, a p value less than 0.05 was considered statistically significant.
Results
Basic clinical characteristics
A total of 187 hospitalized patients diagnosed with NCFB who qualified the above criteria were initially enrolled in our study. Four patients were lost to follow-up, and 183 patients completed the follow-up study. Four patients were excluded due to incomplete clinical data. Among the 179 patients who were included in the analysis, 95 were male, and 84 were female. The mean age of the patients was 64.19 ± 14.12 years. The three most common comorbidities were COPD (56/179, 31.28%), hypertension (50/179, 27.93%), PAH (44/179, 24.58%), CVD (41/179, 22.91%), followed by osteoporosis (38/179, 21.23%), anemia (36/179, 20.11%), GERD (33/179, 18.44%), sinusitis (30/179, 16.76%), diabetes ( 24/179, 13.41%), liver disease (22/179, 12.29%), asthma (17/179, 9.50%), connective tissue diseases (15/179, 8.38%), kidney disease (11/179, 6.15%), PVD (9/179, 5.03%), and cerebrovascular disease (7/179, 5.03%). Over a median follow-up of 32 (18, 39) months, 21 patients (11.73%) died (19 died because of respiratory-related disease, and 2 patients died because of non-respiratory-related disease). Twenty-nine patients (16.20%) had chronic infection with pathogenic microorganisms, of which 22 were infected with Pseudomonas aeruginosa (PA) (10 were mucoid strains, while 12 were non-mucoid strains), 2 with Escherichia coli, 4 with Aspergillus, and 1 with Klebsiella pneumoniae.
Risk factors for osteoporosis in hospitalized NCFB patients
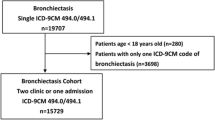
154 patients completed the CAT and SGRQ evaluation. Patients with osteoporosis had significantly higher CAT and SGRQ scores than those without osteoporosis. All the patients completed the BSI and BACI evaluation. The BSI and BACI scores of patients with osteoporosis were also significantly higher than those without osteoporosis (Fig. 1). Patients with osteoporosis were likely to be older, female, suffering from CVD, GERD, and anemia, post-infection, and regular ICS treatment (Table 1). The results of modified Poisson regression analysis showed that age, female sex, anemia, post-infection, and regular ICS treatment were independent risk factors associated with osteoporosis in hospitalized NCFB patients (Table 2).
Differences of CAT, SGRQ, BSI, BACI scores between hospitalized NCFB bronchiectasis patients with and without osteoporosis. Data presented as median (interquartile range). Abbreviations: NCFB, non-cystic fibrosis bronchiectasis; CAT, chronic airway assessment test; SGRQ, St. George Respiratory Questionnaires; BSI, Bronchiectasis Severity Index; BACI, Bronchiectasis Aetiology Comorbidity Index
Impact of osteoporosis and FF on the mortality of hospitalized NCFB patients
Over a median follow-up time of 32 (18, 39) months, 21 (11.73%) patients died. The all-cause mortality rate in NCFB patients with osteoporosis was 28.95% (11/38) compared with 7.09% (10/141) in NCFB patients without osteoporosis. Clinical data in our cohort showed that age, BMI, HE in the previous 2 years, AE in the previous 2 years, FEV1%pred, Reiff score, percentage of chronic infection by PA and pathogenic microorganisms, degree of dyspnea (mMRC > 2 grade), and the BSI score were significantly different between survivors and non-survivors (Table 3). Univariate regression analysis showed that the BSI score, comorbidities of PAH, CVD, HT, anemia, cerebrovascular disease, osteoporosis, and macrolides treatment significantly affected the all-cause mortality in our cohort. Multivariate regression showed that the BSI score, comorbid osteoporosis, PAH, CVD, and cerebrovascular disease were independently associated with all-cause mortality in our cohort (Table 4). The all-cause mortality in NCFB patients with osteoporosis [28.94% (11/38)] was significantly higher than those without osteoporosis [7.09% (10/141)] [hazard ratio (HR) 5.34, 95% confidence interval (CI) 2.26–12.67, P < 0.001]. After adjusting for BSI and other confounding factors, hospitalized NCFB patients with osteoporosis had an HR of 4.29 (95% CI 1.75–10.49) compared with patients without osteoporosis (survivor curve shown in Fig. 2).
Discussion
In our study, NCFB patients with osteoporosis were found to have more severe symptoms (CAT score), worse quality of life (SGRQ score), greater disease severity (BSI score), and more comorbidities (assessed by BACI score) than patients without osteoporosis. Age, female sex, anemia, post-infection, and regular ICS treatment were risk factors for osteoporosis in hospitalized NCFB patients. Osteoporosis was also found to be an independent risk factor for all-cause mortality after adjusting for BSI and other confounding factors, which suggests that clinicians should pay attention to the bone health of NCFB patients. To the best of our knowledge, few studies have investigated the effect of osteoporosis on the prognosis of patients with NCFB, especially in the Asian population.
Osteoporosis is a common finding in NCFB patients worldwide. According to a European study (2015), osteoporosis ranks amongst the top five comorbidities associated with NCFB; in this multicenter European NCFB cohort (986 patients), 15.9% of patients had osteoporosis [9]. In a retrospective study based on electronic medical records in Mayo Clinic, Florida, the prevalence of osteoporosis in NCFB patients reached 30% [15]. In another cross-sectional study conducted in Malaga, Spain, 7% of men and 15% of women with NCFB had osteoporosis [11]. A recent study in China showed a much higher prevalence of osteoporosis in Asian patients with NCFB (70%) [17]. The considerable differences in the reported incidence of osteoporosis in NCFB patients may be attributable to differences in the study population, methods, and data collection methods. Our study found a moderate probability of osteoporosis in hospitalized NCFB patients (21.23%) compared with previous studies; this may be because of a higher proportion of males in our cohort and the fact that not all NCFB patients in our study underwent bone mineral density (BMD) test, which may have underestimated the prevalence in some asymptomatic patients.
The harmful impact of osteoporosis in patients with chronic pulmonary diseases has been widely investigated, especially in COPD and asthma. Vertebral fractures (VF) and bone loss in elderly postmenopausal women were closely related to restrictive lung dysfunction [18]. The decrease in bone density in COPD patients was closely related to the degree of emphysema [19] and the severity of airflow limitation [20]. A meta-analysis showed that osteoporosis and VF significantly increase the mortality risk and decrease pulmonary function among patients with COPD [4]. Among asthmatic patients, osteopenia, osteoporosis, and pathologic fractures were identified as risk factors for emergency department visits [21]. In cystic fibrosis (CF) patients with end-stage lung disease, CF-related bone diseases such as decreased bone mineral density were also commonly detected [22]. There has even been a dicey combination of malignancy (lung cancer) and osteoporosis [23].
The underlying mechanisms of the association between bronchiectasis and osteoporosis are not well characterized. Corticosteroid therapy for comorbidities of COPD or asthma may play a significant role in this respect. In addition, they might share common risk factors, including old age, lower BMI, sex, systematic inflammation, and Vitamin D deficiency. Beyond the classical risk factors mentioned above, especially in tuberculosis-endemic Asian regions, tuberculosis significantly increases the incidence of osteoporosis and osteoporotic fracture in NCFB patients [24]. In our study, too, post-infection (including tuberculosis and other pathogens) were independent risk factors for osteoporosis in hospitalized NCFB patients after adjusting for age, sex, and regular ICS treatment. Systematic inflammation, vitamin D deficiency, and the non-calcemic effect of vitamin D and 1,25(OH)2 D on the organs may mediate the association between osteoporosis and pulmonary diseases [25,26,27,28]. Besides, genetic polymorphisms in vitamin D receptor (VDR) and vitamin D-binding protein (VDBP) may also play a role in the pathogenesis of lung diseases [26, 29].
In our study, anemia was found to be another independent risk factor for osteoporosis in patients with bronchiectasis, similar to several previous studies that described a strong association between bone health and anemia [11, 30]. There are several mechanisms by which clinically detectable anemia could signal bone fragility. The first potential mechanism is impairment of bone cells in providing a supportive microenvironment required to maintain erythropoiesis. Moreover, other scholars have detected that anemia or iron deficiency can increase hematopoietic lineage cells (including osteoclasts) and marrow expansion by decreasing bone volume. Moreover, anemia can affect bone strength by altering the mechanical and loading properties of bone marrow. Another potential mechanism is increased erythropoietin levels, which stimulates bone marrow erythropoiesis and induces bone loss [30]. Although several studies have shown a strong relationship between bone health and anemia in individuals, more work is required to elucidate the relationship between hemoglobin (HGB) levels and bone density, and to evaluate the utility of HGB measurement as a signal for osteoporosis screening.
The causal relationship between osteoporosis and pulmonary diseases and the underlying molecular mechanisms are also not yet fully elucidated. In addition to the common risk factors such as old age, smoking, low BMI, and reduced physical activity, systemic or long-term inhaled glucocorticoid therapy is an established reason for the greater susceptibility of COPD and asthma to develop osteoporosis or fragility fracture (FF) [21]. An increasing number of studies have demonstrated that systemic inflammation is a potential cause of pulmonary disease-associated osteoporosis [19, 31, 32]. Moreover, studies have shown a vital role of vitamin D in mediating the link between osteoporosis and pulmonary diseases [33]; the potential non-calcemic effects of vitamin D have evoked the interest of many researchers. Studies have demonstrated the potential link between vitamin D insufficiency or deficiency and COPD pathogenesis, progression, exacerbations, and comorbidities [25]. In our study, osteoporosis was an independent risk factor for mortality in hospitalized NCFB patients. To the best of our knowledge, this is the first study to directly demonstrate the adverse impact of osteoporosis in NCFB patients of Asian ethnicity. Recently, several studies have investigated the effect of osteoporosis in patients with bronchiectasis. Osteoporosis was the fifth most prevalent comorbidity in the BACI derivation cohort, but it was not associated with a significant risk of 5-year mortality [9]. In a cross-sectional study of 123 patients with bronchiectasis, FEV1, body composition, muscle strength, and bone remodeling markers were associated with a lower BMD [11]. In another retrospective cross-sectional study of NCFB patients, BMD showed a significant negative correlation with the lowest SPO2, the change of SPO2%, and distance-saturation product during the 6-min walk test; the BMD also showed a decrease with the increase of severe exacerbations per year [17].
Limitations
Some limitations of our study should be considered while interpreting the results. First, this was a single-center study and the study population comprised of hospitalized patients, indicating relatively severe disease. Although studies conducted in Europe did not find a significant contribution of osteoporosis to the mortality of NFCB patients [9], different ethnic groups and disease spectrum in different regions may lead to different risk factors. Second, this was an observational study, and the relevant comorbidities were captured from the medical history or examination findings in the electronic medical records. Thus, the possibility of reporting bias cannot be ruled out and some comorbidities may have been missed if patients had no symptoms. Moreover, although we had excluded patients who had malignant tumor or severe immunosuppression (such as oral glucocorticoids treatment), concurrent medication (such as proton pump inhibitors or insulin sensitizing agents) or follow-up intervention may have influenced bone mineral density. Further interventional studies are required to validate the cause-effect relationship between the two diseases. Third, we did not test the level of 1,25(OH)2 D or any other factor that reflects the association between osteoporosis and NCFB. More extensive studies are required to determine the exact impact of osteoporosis in Asian NCFB patients and unravel the associated mechanisms.
Conclusions
Age, female sex, history of infection, anemia, and regular ICS treatment were risk factors associated with osteoporosis in hospitalized NCFB patients from Asia. Our study indicates that comorbid osteoporosis in hospitalized NCFB patients is an independent risk factor for all-cause mortality. Clinicians should pay attention to bone health in patients with chronic pulmonary disease, including bronchiectasis. Further studies are required to investigate the potential mechanism between those two diseases.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
- NCFB:
-
Non-cystic fibrosis bronchiectasis
- FF:
-
Fragility fracture
- BMI:
-
Body mass index
- PA:
-
Pseudomonas aeruginosa
- mMRC:
-
Modified Medical Research Council
- FEV1%pre:
-
Forced expiratory volume in 1 s to predictive value
- BSI:
-
Bronchiectasis Severity Index
- BACI:
-
Bronchiectasis Aetiology Comorbidity Index
- COPD:
-
Chronic obstructive pulmonary disease
- PAH:
-
Pulmonary artery hypertension
- HT:
-
Hypertension
- GERD:
-
Gastroesophageal reflux disease
- CVD:
-
Cardiovascular diseases
- PVD:
-
Peripheral vascular disease
- CTD:
-
Connective tissue disease
- ICS:
-
Inhaled corticosteroid
- CAT:
-
Chronic airway assessment test
- SGRQ:
-
St. George Respiratory Questionnaires
- RR:
-
Relative ratio
- HR:
-
Hazard ratio
- 95% CI:
-
95% Confidence interval
- BMD:
-
Bone mineral density
- DEXA:
-
Dual-energy X-ray absorptiometry
- VF:
-
Vertebral fractures
- VDR:
-
Vitamin D receptor
- VDBP:
-
Vitamin D-binding protein
- HGB:
-
Hemoglobin
- FF:
-
Fragility fracture
References
Kwak HJ, Moon J-Y, Choi YW, Kim TH, Sohn JW, Yoon HJ, et al. High prevalence of bronchiectasis in adults: analysis of CT findings in a health screening program. Tohoku J Exp Med. 2010;222(4):237–42.
Zhou YM, Wang C, Yao WZ, Chen P, Kang J, Huang SG, et al. The prevalence and risk factors of bronchiectasis in residents aged 40 years old and above in seven cities in China. Zhonghua Nei Ke Za Zhi. 2013;52(5):379–82.
Clofent D, Álvarez A, Traversi L, Culebras M, Loor K, Polverino E. Comorbidities and mortality risk factors for patients with bronchiectasis. Expert Rev Respir Med. 2021;15(5):623–34. https://doi.org/10.1080/17476348.2021.1886084.
Kakoullis L, Sampsonas F, Karamouzos V, Kyriakou G, Parperis K, Papachristodoulou E, et al. The impact of osteoporosis and vertebral compression fractures on mortality and association with pulmonary function in COPD: a meta-analysis. Joint Bone Spine. 2021;89(1):105249. https://doi.org/10.1016/j.jbspin.2021.105249.
Inoue D, Watanabe R, Okazaki R. COPD and osteoporosis: links, risks, and treatment challenges. Int J Chron Obstruct Pulmon Dis. 2016;11:637–48. https://doi.org/10.2147/copd.s79638.
Pludowski P, Holick MF, Pilz S, Wagner CL, Hollis BW, Grant WB, et al. Vitamin D effects on musculoskeletal health, immunity, autoimmunity, cardiovascular disease, cancer, fertility, pregnancy, dementia and mortality—a review of recent evidence. Autoimmun Rev. 2013;12(10):976–89. https://doi.org/10.1016/j.autrev.2013.02.004.
Platitsyna NG, Bolotnova TV. Vitamin D deficiency as a risk factor for chronic non-infectious diseases. Adv Gerontol. 2017;30(6):873–9.
Vos R, Ruttens D, Verleden SE, Vandermeulen E, Bellon H, Van Herck A, et al. High-dose vitamin D after lung transplantation: a randomized trial. J Heart Lung Transpl. 2017;36(8):897–905. https://doi.org/10.1016/j.healun.2017.03.008.
McDonnell MJ, Aliberti S, Goeminne PC, Restrepo MI, Finch S, Pesci A, et al. Comorbidities and the risk of mortality in patients with bronchiectasis: an international multicentre cohort study. Lancet Respir Med. 2016;4(12):969–79. https://doi.org/10.1016/s2213-2600(16)30320-4.
Diehl N, Johnson MM. Prevalence of osteopenia and osteoporosis in patients with noncystic fibrosis bronchiectasis. South Med J. 2016;109(12):779–83. https://doi.org/10.14423/smj.0000000000000565.
Contreras-Bolívar V, Olveira G, Porras N, Acosta E, Rubio-Martín E, Tapia-Guerrero MJ, et al. Osteopenia and osteoporosis in patients with bronchiectasis: association with respiratory parameters, body composition, muscle strength and bone remodeling biomarkers. Sci Rep. 2019;9(1):14496. https://doi.org/10.1038/s41598-019-51069-0.
Wang XL, Feng ST, Wang YT, Chen NH, Wang ZZ, Zhang Y. Paeoniflorin: a neuroprotective monoterpenoid glycoside with promising anti-depressive properties. Phytomedicine. 2021;90:153669. https://doi.org/10.1016/j.phymed.2021.153669.
Chalmers JD, Goeminne P, Aliberti S, McDonnell MJ, Lonni S, Davidson J, et al. The bronchiectasis severity index. An international derivation and validation study. Am J Respir Crit Care Med. 2014;189(5):576–85.
Lanza FC, Castro RA, de Camargo AA, Zanatta DJ, Rached S, Athanazio R, et al. COPD Assessment Test (CAT) is a valid and simple tool to measure the impact of bronchiectasis on affected patients. COPD J Chronic Obstr Pulm Dis. 2018;15(5):512–9.
Newsome B. Commentary on “prevalence of osteopenia and osteoporosis in patients with noncystic fibrosis bronchiectasis.” South Med J. 2016;109(12):784.
Chinese Society of Osteoporosis and Bone Mineral Research. Guidelines for the diagnosis and management of primary osteoporosis (2017). Chin J Osteoporos. 2019;25:281–309.
Huang HY, Sheng TF, Lin CW, Wang TW, Lo CY, Chung FT, et al. Oxygen desaturation during the 6-min walk test as a risk for osteoporosis in non-cystic fibrosis bronchiectasis. BMC Pulm Med. 2019;19(1):28. https://doi.org/10.1186/s12890-019-0794-x.
Watanabe R, Shiraki M, Saito M, Okazaki R, Inoue D. Restrictive pulmonary dysfunction is associated with vertebral fractures and bone loss in elderly postmenopausal women. Osteoporos Int. 2018;29(3):625–33. https://doi.org/10.1007/s00198-017-4337-0.
Hu L, Zhang DW, Jiang HY, Ji S, Wei YY, Hu HQ, et al. Correlation between systemic inflammation level and emphysema degree and bone mineral density in chronic obstructive pulmonary disease patients and its mechanism. Zhonghua Jie He He Hu Xi Za Zhi. 2021;44(3):213–7. https://doi.org/10.3760/cma.j.cn112147-20200721-00824.
Watanabe K, Onoue A, Kubota K, Higashi N, Hayashi T, Tsuda T, et al. Association between airflow limitation severity and reduced bone mineral density in Japanese men. Int J Chron Obstruct Pulmon Dis. 2019;14:2355–63. https://doi.org/10.2147/copd.s213746.
Shaheen MS, Silverberg JI. Association of asthma with osteopenia, osteoporosis, osteomalacia, and fractures. Allergy Asthma Proc. 2020;41(2):112–9. https://doi.org/10.2500/aap.2020.41.190035.
Robinson CA, Hofer M, Benden C, Schmid C. Evaluation of bone disease in patients with cystic fibrosis and end-stage lung disease. J Bras Pneumol. 2019;45(1):e20170280. https://doi.org/10.1590/1806-3713/e20170280.
Lakshmana Perumal N, Selvi J, Sahoo JP, Kamalanathan S. Osteoporosis and malignancy: a dicey combination. BMJ Case Rep. 2018. https://doi.org/10.1136/bcr-2017-223881.
Chen YY, Feng JY, Ting WY, Yen YF, Chuang PH, Pan SW, et al. Increased risk of incident osteoporosis and osteoporotic fracture in tuberculosis patients: a population-based study in a tuberculosis-endemic area. Osteoporos Int. 2017;28(5):1711–21. https://doi.org/10.1007/s00198-017-3939-x.
Kokturk N, Baha A, Oh YM, Young JuJ, Jones PW. Vitamin D deficiency: What does it mean for chronic obstructive pulmonary disease (COPD)? A compherensive review for pulmonologists. Clin Respir J. 2018;12(2):382–97. https://doi.org/10.1111/crj.12588.
Pfeffer PE, Hawrylowicz CM. Vitamin D and lung disease. Thorax. 2012;67(11):1018–20. https://doi.org/10.1136/thoraxjnl-2012-202139.
Quint JK, Wedzicha JA. Is vitamin D deficiency important in the natural history of COPD? Thorax. 2010;65(3):192–4. https://doi.org/10.1136/thx.2009.129619.
Liu N, Sun J, Wang X, Zhang T, Zhao M, Li H. Low vitamin D status is associated with coronavirus disease 2019 outcomes: a systematic review and meta-analysis. Int J Infect Dis. 2021;104:58–64. https://doi.org/10.1016/j.ijid.2020.12.077.
Chishimba L, Thickett DR, Stockley RA, Wood AM. The vitamin D axis in the lung: a key role for vitamin D-binding protein. Thorax. 2010;65(5):456–62. https://doi.org/10.1136/thx.2009.128793.
Valderrábano RJ, Wu JY. Bone and blood interactions in human health and disease. Bone. 2019;119:65–70.
Bai P, Sun Y, Jin J, Hou J, Li R, Zhang Q, et al. Disturbance of the OPG/RANK/RANKL pathway and systemic inflammation in COPD patients with emphysema and osteoporosis. Respir Res. 2011;12(1):157. https://doi.org/10.1186/1465-9921-12-157.
Yormaz B, Cebeci H, Yılmaz F, Süerdem M. Bone mineral density in emphysema and chronic bronchitis phenotypes in hospitalized male chronic obstructive pulmonary disease patients. Clin Respir J. 2020;14(1):47–53. https://doi.org/10.1111/crj.13099.
Białek-Gosk K, Rubinsztajn R, Białek S, Paplińska-Goryca M, Krenke R, Chazan R. Serum vitamin D concentration and markers of bone metabolism in perimenopausal and postmenopausal women with asthma and COPD. Adv Exp Med Biol. 2018;1070:27–36. https://doi.org/10.1007/5584_2018_157.
Acknowledgements
We thank Medjaden Inc. for scientific editing of this manuscript.
Funding
This work is supported by the Start-up Funding for Scientific Research in Fujian Medical University (Grant number: 2017XQ1184) and Fujian Provincial Health Technology Project (Grant number: 2018-1-98).
Author information
Authors and Affiliations
Contributions
Literature search: XZ and ZYM; (Data collection: XZ, XHL, KJZ, CCQ, LYX, and XMC; Study design: ZYM and XZ; Analysis of data: XZand ZYM; Manuscript preparation: XZ and XHL; Review of manuscript: ZYM, RZL and DLW. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Review Committee of Longyan First Affiliated Hospital, Fujian Medical University. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all patients included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zou, X., Ma, Z., Liu, X. et al. Risk factors and prognostic value of osteoporosis in hospitalized patients with bronchiectasis. BMC Pulm Med 23, 55 (2023). https://doi.org/10.1186/s12890-023-02346-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02346-2