Abstract
Purpose
In 2015, the World Health Organization renamed mucinous bronchioloalveolar adenocarcinoma as pulmonary invasive mucinous adenocarcinoma (IMA). Due to its low incidence and unclear prognosis with surgical treatment, previous studies have presented opposing survival outcomes. We aimed to investigate the differences in surgical prognosis and prognosis-related risk factors by comparing IMA with non-mucinous invasive adenocarcinoma (NMA).
Methods
A total of 20,914 patients diagnosed with IMA or NMA from 2000 to 2014 were screened from the Surveillance, Epidemiology, and End Results database. The screened patients were subjected to propensity score matching (PSM) in a 1:4 ratio to explore the survival differences between patients with IMA and NMA and the factors influencing prognosis.
Results
For all patients, IMA was prevalent in the lower lobes of the lungs (p < 0.0001), well-differentiated histologically (p < 0.0001), less likely to have lymph node metastases (94.4% vs. 72.0%, p < 0.0001) and at an earlier pathological stage (p = 0.0001). After PSM, the IMA cohort consisted of 303 patients, and the NMA cohort consisted of 1212 patients. Kaplan‒Meier survival analysis showed no difference in overall survival (OS) between patients in the IMA cohort and those in the NMA cohort (p = 0.7). Cox proportional hazards analysis showed that differences in tumor pathological type did not influence OS between the two cohorts (p = 0.65). Age (HR: 1.98, 95% CI 1.7–2.31, p < 0.0001), gender (HR: 0.64, 95% CI 0.55–0.75, p < 0.0001), and radiation treatment (HR: 2.49, 95% CI 1.84–3.37, p < 0.0001) were independent predictors of patient OS.
Conclusion
There was no significant difference in OS between patients with IMA and those with NMA after surgical treatment. Age, sex, and radiation treatment can independently predict OS.
Similar content being viewed by others
Introduction
According to Global Cancer Statistics 2021 [1], there were approximately 19.3 million new tumor cases and approximately 10 million deaths worldwide, with approximately 2.2 million new cases and 1.7 million deaths from lung cancer, which remains the deadliest cancer to date. The most common type of lung cancer today is lung adenocarcinoma, which accounts for approximately 50% of all lung cancers [2]. A specific subtype of lung adenocarcinoma, once known as mucinous bronchioloalveolar adenocarcinoma [3], accounts for approximately 5% of all adenocarcinomas of the lung [4]. Because there are many subtypes of bronchoalveolar carcinoma, the prognosis of each subtype varies greatly. In 2011, the International Association for the Study of Lung Cancer (IASLC), the American Thoracic Society (ATS), and the European Respiratory Society (ERS) jointly proposed renaming mucinous bronchioloalveolar adenocarcinoma as invasive mucinous adenocarcinoma (IMA) [5]. In 2015, the WHO officially updated the classification of lung tumors and renamed mucinous bronchioloalveolar adenocarcinoma as IMA.
IMA possesses unique pathological and molecular biological features. The tumor cells are composed of goblet cells and columnar cells rich in mucin. Compared to other types of lung adenocarcinoma, the cellular heterogeneity of IMA is less pronounced, making it more challenging to diagnose clinically [4, 6]. On imaging, IMA may appear as either a nodule or a mass or as a pneumonia-like feature [7]. The diagnosis of IMA can therefore be easily missed in clinical practice based on imaging data alone. At the genetic level, previous studies have demonstrated that IMA is susceptible to mutations in the KRAS gene [8], accounting for approximately 35–75% of all mutation types [9, 10]. The prognosis of patients with IMA with mutations is poor; the prognosis of IMA is highly variable, and previous studies have shown contrasting survival outcomes. Some studies have shown a significantly better overall survival (OS) than non-mucinous invasive adenocarcinoma (NMA) [11,12,13]. Other reports have shown conflicting results [14,15,16]. The relationship between the clinicopathological features and prognosis of IMA is poorly understood, as this type of adenocarcinoma is rare, and there are few retrospective studies of large numbers of cases. The accurate diagnosis of IMA is crucial to patient treatment and prognosis. Therefore, this study collected data from patients with pathologically confirmed IMA and NMA from 2000 to 2014 through the Surveillance, Epidemiology and End Results (SEER) database to compare whether there is a difference in OS between patients with IMA and NMA. This provides support for the clinical treatment of patients with IMA.
Methods
Patient selection
This study was a retrospective study in which we used SEER*Stat 8.4.0 software and selected data collected from 17 centers from 2000 to 2019 (SEER Research Plus Data, 17 Registries, Nov 2021 Sub[2000–2019]), resulting in 20,914 patients meeting our inclusion criteria. The inclusion criteria were as follows: (1) patients with a year of diagnosis of 2000–2014 were selected; (2) complete follow-up was available; (3) virtual survival status and exact survival time were available; (4) the site of diagnosis was “Lung and Bronchus”(5) “only one primary cancer” status was met; and (6) the pathological type at diagnosis was selected by “Site and Morphology, ICD-O-3 Hist/Behav, malignant”. The pathological types of NMA were as follows: adenocarcinoma (8140/3), bronchioloalveolar carcinoma nonmucinous (8252/3), papillary adenocarcinoma (8260/3), bronchioloalveolar NOS (8250/3), adenocarcinoma with mixed subtypes (8255/3), and acinar cell carcinoma (8550/3). The pathological type of IMA was bronchioloalveolar carcinoma mucinous (8253/3). In contrast, 8481/3 mucinous-producing adenocarcinoma is a mucinous-producing adenocarcinoma; this type is not IMA, so we excluded this pathological type.
The data were then screened, first selecting patients with a single primary tumor surgically removed and confirmed by pathology. Patients diagnosed by autopsy and puncture biopsy were excluded, and patients with an overall survival of less than one month were excluded. Patients with unknown age, race, marital status, radiotherapy information, or unknown survival status were also excluded. Patients with unknown lymph node dissection and distant metastatic status were excluded. Finally, we selected data from patients who did not develop metastases.
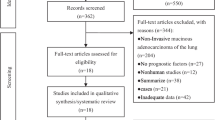
Once the data had been selected, we extracted the patient details from the database, including basic demographic, TNM stage, differentiation grade, lesion location and size, survival time, survival status, radiotherapy, and chemotherapy information. Figure 1 summarizes the process of cleaning the data. A final dataset was created to describe the clinical characteristics of patients with IMA and NMA. This included 20,611 patients with NMA and 303 patients with IMA. To exclude the effect of confounding factors on survival outcomes, the screened patients were subjected to propensity score matching (PSM) with a ratio of 1:4.
Statistical analysis
The primary endpoint of this study was the OS of patients in both cohorts, counted in months. Patients who survived at the last follow-up date in the SEER database (including those who died after the follow-up date) were recorded as surviving.
Characteristics were summarized using standardized statistical parameters, with continuous variables described as the mean ± standard deviation or median + upper and lower quartiles and categorical variables described as frequencies and percentages based on the results of the Kolmogorov‒Smirnov test. Analysis of the distribution of nonnormal continuous variables was performed using the Mann‒Whitney U test. Categorical variables were compared using the chi-square test or Fisher's exact test.
As the patients selected from the database all had TNM staging according to the 6th edition of the AJCC TNM staging system, we converted all patients' staging to the 8th edition TNM staging by comparing the 6th and 8th editions of the AJCC. The dataset was matched with 1:4 PSM using the MatchIt package of R software. The matched IMA cohort contained 303 patients, and the NMA cohort contained 1212 patients. The balance between the two groups was checked by standardized mean differences after matching.
The Kaplan‒Meier method was applied to obtain survival and OS data for patients with IMA and NMA. PH assumptions were made for all variables included in the model and all covariates pass the PH assumption. Cox PH analysis was used to evaluate the influencing factors affecting survival, and variables with p values < 0.05 in the univariate analysis were included in the multivariable analysis. They were evaluated again using the Cox PH analysis model with the propensity-matched data. All p values less than 0.05 were considered statistically significant. Hazard ratios (HRs) and 95% confidence intervals (CIs) were used to indicate the relative risk of each factor.
Results
General characteristics of IMAs and NMAs
A total of 20,914 eligible patients were included in this study. The baseline characteristics of patients with IMA and NMA are shown in Dataset 1 (Table 1). There were no differences in age at diagnosis (p = 0.299), race (p = 0.320), gender (p = 0.156), marital status (p = 0.029), right and left lung distribution (p = 0.134) or type of surgery (p = 0.138). However, the distribution of upper, middle, and lower lobes (p < 0.0001), tumor histological grade (p < 0.0001), T stage (p < 0.0001), N stage (p < 0.0001), pathological stage (p = 0.0001), tumor size (p < 0.0001), radiotherapy (p < 0.0001), and chemotherapy (p < 0.0001) showed differences between the two groups. The majority of tumor differentiation in IMA was grade I, while NMA showed a different distribution of differentiation. The TNM staging of patients in the SEER database was staged according to the 6th edition of the AJCC staging system. After conversion to the 8th edition staging system, the two groups showed differences in T stage, N stage, and TNM stage (p < 0.0001). Ninety-four percent of patients in the IMA group were lymph node metastasis free. The two groups also showed significant differences in the receipt of adjuvant radiotherapy and chemotherapy (p < 0.0001). There was no significant difference between the IMA group and the NMA group in terms of the choice of surgical procedure.
Comparative postoperative survival of patients with IMA and NMA: analysis of the propensity-matched dataset
The screened patients were grouped in PSM according to a ratio of 1:4. This resulted in 303 patients with IMA and 1212 patients with NMA. The baseline characteristics of the two groups are shown in Dataset 2 (Table 2). There were no differences between the matched patients in variables such as age, race, gender, and tumor differentiation grade. This allowed for the exclusion of confounding factors on the survival of patients in both cohorts. In the prematching cohort, the median survival time was longer in the IMA group than in the NMA group (124 ± 34 months (95% Cl 96.23–151.77) for patients with IMA and 83 ± 30 months (95% Cl 80.82–85.18) for patients with NMA p = 0.001) (Fig. 2). However, patients with IMA and NMA in the matched cohort did not show a difference in survival. The median survival times were 124 ± 34 months (95% CI 96.23–151.77) for patients with IMA and 119 ± 44 months for patients with NMA (95% CI 105.47–132.54; p = 0.7) (Fig. 3). To further validate the impact of IMA and NMA on patient OS, univariate and multivariate Cox analyses were performed on the prematched and postmatched data (Tables 3 and 4). Variables that were significant in the univariate analysis were then subjected to multivariable analysis. In the unmatched data, Cox multivariable analysis showed that age, radiotherapy, chemotherapy, histological grade, location, marital status, mode of surgery, race, gender, tumor volume, T stage, N stage, and pathological stage could predict the OS of patients, while in the postmatched data, Cox multivariable analysis showed that age, gender, and receipt of radiotherapy independently predicted the OS of patients.
Discussion
IMA has unique clinical and pathological features [17,18,19,20,21]. The main difference between IMA, which account for only 5% of all adenocarcinomas, and other lung adenocarcinomas is that the tumor cells consist of goblet cells and columnar cells [4]. IMA was known as mucinous bronchioloalveolar adenocarcinoma until 2011. Although there have been many studies on IMA due to its clinical rarity, the survival of patients with IMA remains controversial, which makes the clinical treatment of IMA difficult. This calls for data analysis from cohorts containing large number of samples, which in turn will further clarify the survival and prognosis of patients with IMA.
Although IMA gene mutations in patients with information from the SEER database is not known, but according to the previously reported [22, 23], KRAS is the most common mutation type, and KRAS mutation may be a poor predictor of survival [24]. This may be because tumors with KRAS mutations may grow faster than tumors without KRAS mutations [25].In addition to KRAS mutation, NRG1 fusion is another common mutation in IMA. It has been reported that 7–27% of IMA have detected NRG1 fusion [23, 26]. EGFR mutations were also found in a small number of IMA patients. Research suggests that EGFR mutation in IMA is an indicator of poor prognosis [27]. Studies indicate abnormal expression of MUC6 in IMA which is associated with survival differences that may reflect MUC6 induced changes in cell adhesion properties [28].
By comparing patients' baseline data, we found that IMA was more likely to occur in the lower lobe, with approximately 59% of patients having tumors in the lower lobe at diagnosis. At the same time, NMA was more likely to occur in the upper lobe, which is in line with the finding of previous studies [11]. The histological grading of IMA was better, in line with the finding of previous studies [13]. Approximately 59% of IMA cases were grade 1 at diagnosis. In contrast, approximately 45% of NMAs were grade II, and 30% were grade III at diagnosis. Contrary to the data of previous studies [29], in our data, there was no difference between the sexes of patients with IMA and NMA. This may be due to the differences between the Eastern and Western populations. In contrast, the T stage, N stage, and pathological stage of the tumor and treatment with radiotherapy showed differences between the IMA group and the NMA group, which is consistent with the results of previous studies [13].
Previous studies have included small sample sizes due to the rarity of IMA. Many studies have reached contradictory conclusions. Some studies found that the OS of patients with IMA is worse than that of patients with NMA [30]. Some studies suggest that the OS of patients with IMA is comparable to that of patients with NMA [31]. Some studies found that the OS of patients with IMA is better than that of patients with NMA [5, 29]. Our data were obtained from the SEER database. A total of 20,914 patients with IMA and NMA were enrolled. PSM was used to minimize the impact of confounding factors on survival outcomes. Survival analysis of patients after PSM showed that the mean survival time of patients with IMA was 124 ± 34 months, with a 3 year survival rate of 73.8% (95% Cl 0.69–0.79). The 5 year survival rate was 66.8% (95% Cl 0.62–0.72). The mean survival in months for patients with NMA was 119 ± 44 months. The 3 year survival rate was 78% (95% CL 0.76–0.80), and the 5 year survival rate was 67.2% (95% CL 0.65–0.70). OS was the same for patients with IMA and NMA (p = 0.7). This is consistent with the findings of several previous studies.
After PSM, Cox multivariable analysis of the data showed that patients' OS was not affected by the histological type of the tumor. These results are consistent with those of previous studies [32].Some studies showed that [13] pneumonectomy and sublobar resection can predict OS in patients, which contradicts our findings. This may be due to data discrepancies, and a larger sample size is needed to determine this further. Some studies found that lesion location is also an independent risk predictor of patient OS [29], which is different from our results. This may be due to differences in the data between Eastern and Western populations. Further subgroup analysis of the Eastern and Western populations is needed.
Regarding lymph nodes, patients with IMA and those with NMA showed significant differences, with approximately 94% of patients in the IMA group and approximately 72% of patients in the NMA group being at stage N0. Some previous studies have also shown that patients with IMA have a lower rate of lymph node metastasis [31, 33]. This may show that IMA and NMA are two different types of lung cancer. The results of studies on mutations and immune profiles of both could further confirm this hypothesis [10, 14, 34].
There are limitations to this study. First, due to the small amount of data on stage IV patients, it was not possible to conduct a precise analysis when performing statistical analysis. Therefore, when screening the data, the stage IV data were removed. Only patients with M0 were retained. This made it impossible to compare the survival of stage IV patients. Second, the SEER database only has the OS data of patients and no data on disease recurrence. Therefore, only the OS of patients could be analyzed, not the disease-free survival of patients. A significant indicator for the assessment of patients' condition is missing. Third, the inclusion criteria were based on the patients’ ICD-0-3 code. Although the diagnosis was confirmed by pathology, a small proportion of the pathology was NOS, and this part of the pathology may affect the outcome.
Our article also has some shortcomings, minimally invasive adenocarcinoma (MIA) was diagnosed as invasive adenocarcinoma in version sixth edition TNM stage and not listed separately in the sixth edition TNM stage, but MIA is listed separately in the eighth edition TNM stage, MIA cancer cells also infiltrate, but are listed separately in the eighth edition TNM stage. We examined other SEER database articles [12, 13, 32] which did not specify how to exclude MIA and assume that MIA is also invasive adenocarcinoma.
We matched patients with IMA to patients with NMA by PSM. The impact of confounding factors on the survival of patients in both groups was eliminated as much as possible. However, due to the rarity of IMA, although patients diagnosed from 2000 to 2014 were selected, only 303 patients with IMA met the criteria. We also attempted to screen the data for patients diagnosed in 2015–2019, but unfortunately, due to the revision of the SEER database and the lack of various patient information, it was impossible to filter the required patient information from 2015 to 2019. This also greatly limited the number of cases enrolled. Finally, as this study was retrospective, and compared to prospective studies with the highest level of evidence, there were inevitable confounding factors despite PSM. Despite these limitations, the present study has merit. We selected data from 17 centers in the SEER database to avoid bias due to single-center data. Second, the data collected had information on patients' radiotherapy and chemotherapy, allowing us to assess the sensitivity of patients with IMA and NMA to radiotherapy and chemotherapy.
Conclusion
In conclusion, there was no significant difference in OS between the pathological subtypes of IMA and NMA in patients with a pathological staging of M0. Age, gender, and radiation therapy receipt independently predicted patient OS. Our findings can be combined with those of previous studies to jointly analyze survival in patients with IMA.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the SEER database. The address of the SEER database is: https://seer.cancer.gov/. The data that support the findings of this study are openly available in [SEER database].
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Li T, Kung HJ, Mack PC, Gandara DR. Genotyping and genomic profiling of non-small-cell lung cancer: implications for current and future therapies. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31(8):1039–49.
Tang ER, Schreiner AM, Pua BB. Advances in lung adenocarcinoma classification: a summary of the new international multidisciplinary classification system (IASLC/ATS/ERS). J Thorac Dis. 2014;6(Suppl 5):S489–501.
Shim HS, Kenudson M, Zheng Z, Liebers M, Cha YJ, Hoang Ho Q, Onozato M, Le LP, Heist RS, Iafrate AJ. Unique genetic and survival characteristics of invasive mucinous adenocarcinoma of the lung. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2015;10(8):1156–62.
Warth A, Muley T, Meister M, Stenzinger A, Thomas M, Schirmacher P, Schnabel PA, Budczies J, Hoffmann H, Weichert W. The novel histologic International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification system of lung adenocarcinoma is a stage-independent predictor of survival. J Clin Oncol Off J Am Soc Clin Oncol. 2012;30(13):1438–46.
Liu Y, Zhang HL, Mei JZ, Guo YW, Li RJ, Wei SD, Tian F, Yang L, Wang H. Primary mucinous adenocarcinoma of the lung: a case report and review of the literature. Oncol Lett. 2017;14(3):3701–4.
Marx A, Chan JK, Coindre JM, Detterbeck F, Girard N, Harris NL, Jaffe ES, Kurrer MO, Marom EM, Moreira AL, et al. The 2015 world health organization classification of tumors of the thymus: continuity and changes. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2015;10(10):1383–95.
Watanabe H, Saito H, Yokose T, Sakuma Y, Murakami S, Kondo T, Oshita F, Ito H, Nakayama H, Yamada K, et al. Relation between thin-section computed tomography and clinical findings of mucinous adenocarcinoma. Ann Thorac Surg. 2015;99(3):975–81.
Hata A, Katakami N, Fujita S, Kaji R, Imai Y, Takahashi Y, Nishimura T, Tomii K, Ishihara K. Frequency of EGFR and KRAS mutations in Japanese patients with lung adenocarcinoma with features of the mucinous subtype of bronchioloalveolar carcinoma. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2010;5(8):1197–200.
Ichinokawa H, Ishii G, Nagai K, Kawase A, Yoshida J, Nishimura M, Hishida T, Ogasawara N, Tsuchihara K, Ochiai A. Distinct clinicopathologic characteristics of lung mucinous adenocarcinoma with KRAS mutation. Hum Pathol. 2013;44(12):2636–42.
Cha YJ, Kim HR, Lee HJ, Cho BC, Shim HS. Clinical course of stage IV invasive mucinous adenocarcinoma of the lung. Lung Cancer (Amsterdam, Netherlands). 2016;102:82–8.
Chen Z, Li M, Ma K, Shang G, Liang J, Yin J, Luo J, Zhan C, Shi Y, Wang Q. Analysis of the clinicopathological characteristics, genetic phenotypes, and prognostic of pure mucinous adenocarcinoma. Cancer Med. 2020;9(2):517–29.
Moon SW, Choi SY, Moon MH. Effect of invasive mucinous adenocarcinoma on lung cancer-specific survival after surgical resection: a population-based study. J Thorac Dis. 2018;10(6):3595–608.
Casali C, Rossi G, Marchioni A, Sartori G, Maselli F, Longo L, Tallarico E, Morandi U. A single institution-based retrospective study of surgically treated bronchioloalveolar adenocarcinoma of the lung: clinicopathologic analysis, molecular features, and possible pitfalls in routine practice. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2010;5(6):830–6.
Yanagawa N, Shiono S, Abiko M, Ogata SY, Sato T, Tamura G. New IASLC/ATS/ERS classification and invasive tumor size are predictive of disease recurrence in stage I lung adenocarcinoma. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2013;8(5):612–8.
Yoshizawa A, Motoi N, Riely GJ, Sima CS, Gerald WL, Kris MG, Park BJ, Rusch VW, Travis WD. Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic subgroups and implications for further revision of staging based on analysis 514 stage of cases. Modern Pathol Off J U S Can Acad Pathol Inc. 2011;24(5):653–64.
Wislez M, Antoine M, Baudrin L, Poulot V, Neuville A, Pradere M, Longchampt E, Isaac-Sibille S, Lebitasy MP, Cadranel J. Non-mucinous and mucinous subtypes of adenocarcinoma with bronchioloalveolar carcinoma features differ by biomarker expression and in the response to gefitinib. Lung Cancer (Amsterdam, Netherlands). 2010;68(2):185–91.
Awaya H, Takeshima Y, Yamasaki M, Inai K. Expression of MUC1, MUC2, MUC5AC, and MUC6 in atypical adenomatous hyperplasia, bronchioloalveolar carcinoma, adenocarcinoma with mixed subtypes, and mucinous bronchioloalveolar carcinoma of the lung. Am J Clin Pathol. 2004;121(5):644–53.
Blons H, Côté JF, Le Corre D, Riquet M, Fabre-Guilevin E, Laurent-Puig P, Danel C. Epidermal growth factor receptor mutation in lung cancer are linked to bronchioloalveolar differentiation. Am J Surg Pathol. 2006;30(10):1309–15.
Sato K, Ueda Y, Shikata H, Katsuda S. Bronchioloalveolar carcinoma of mixed mucinous and nonmucinous type: immunohistochemical studies and mutation analysis of the p53 gene. Pathol Res Pract. 2006;202(10):751–6.
Lee KS, Kim Y, Han J, Ko EJ, Park CK, Primack SL. Bronchioloalveolar carcinoma: clinical, histopathologic, and radiologic findings. Radiograph Rev Publ Radiol Soc N Am Inc. 1997;17(6):1345–57.
Hwang DH, Sholl LM, Rojas-Rudilla V, Hall DL, Shivdasani P, Garcia EP, MacConaill LE, Vivero M, Hornick JL, Kuo FC, et al. KRAS and NKX2-1 mutations in invasive mucinous adenocarcinoma of the lung. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2016;11(4):496–503.
Nakaoku T, Tsuta K, Ichikawa H, Shiraishi K, Sakamoto H, Enari M, Furuta K, Shimada Y, Ogiwara H, Watanabe S, et al. Druggable oncogene fusions in invasive mucinous lung adenocarcinoma. Clin Cancer Res Off J Am Assoc Cancer Res. 2014;20(12):3087–93.
Luo J, Wang R, Han B, Zhang J, Zhao H, Fang W, Luo Q, Yang J, Yang Y, Zhu L, et al. Analysis of the clinicopathologic characteristics and prognostic of stage I invasive mucinous adenocarcinoma. J Cancer Res Clin Oncol. 2016;142(8):1837–45.
Kakegawa S, Shimizu K, Sugano M, Miyamae Y, Kaira K, Araki T, Nakano T, Kamiyoshihara M, Kawashima O, Takeyoshi I. Clinicopathological features of lung adenocarcinoma with KRAS mutations. Cancer. 2011;117(18):4257–66.
Fernandez-Cuesta L, Plenker D, Osada H, Sun R, Menon R, Leenders F, Ortiz-Cuaran S, Peifer M, Bos M, Daßler J, et al. CD74-NRG1 fusions in lung adenocarcinoma. Cancer Discov. 2014;4(4):415–22.
Deng C, Zhang Y, Ma Z, Fu F, Deng L, Li Y, Chen H. Prognostic value of epidermal growth factor receptor gene mutation in resected lung adenocarcinoma. J Thorac Cardiovasc Surg. 2021;162(3):664-674.e667.
Leir SH, Harris A. MUC6 mucin expression inhibits tumor cell invasion. Exp Cell Res. 2011;317(17):2408–19.
Xu X, Shen W, Wang D, Li N, Huang Z, Sheng J, Rucker AJ, Mao W, Xu H, Cheng G. Clinical features and prognosis of resectable pulmonary primary invasive mucinous adenocarcinoma. Transl Lung Cancer Res. 2022;11(3):420–31.
Dacic S. Pros: the present classification of mucinous adenocarcinomas of the lung. Transl Lung Cancer Res. 2017;6(2):230–3.
Lee HY, Cha MJ, Lee KS, Lee HY, Kwon OJ, Choi JY, Kim HK, Choi YS, Kim J, Shim YM. Prognosis in resected invasive mucinous adenocarcinomas of the lung: related factors and comparison with resected nonmucinous adenocarcinomas. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2016;11(7):1064–73.
Wang Y, Liu J, Huang C, Zeng Y, Liu Y, Du J. Development and validation of a nomogram for predicting survival of pulmonary invasive mucinous adenocarcinoma based on surveillance, epidemiology, and end results (SEER) database. BMC Cancer. 2021;21(1):148.
Russell PA, Wainer Z, Wright GM, Daniels M, Conron M, Williams RA. Does lung adenocarcinoma subtype predict patient survival?: A clinicopathologic study based on the new International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary lung adenocarcinoma classification. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2011;6(9):1496–504.
Copin MC, Buisine MP, Leteurtre E, Marquette CH, Porte H, Aubert JP, Gosselin B, Porchet N. Mucinous bronchioloalveolar carcinomas display a specific pattern of mucin gene expression among primary lung adenocarcinomas. Hum Pathol. 2001;32(3):274–81.
Acknowledgements
We would like to thank pathologist Jiankun He for her guidance on this paper. We would like to thank Dr. Xin Huang for his help, review and guidance in this paper.
Funding
The authors declare that the paper manuscript is not financially supported by the institution.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. DYC collected and analyzed the data in the study. DYC and SNX discussed the results and contributed to the final manuscript. QYL drafted the manuscript. QYL conceived the presented idea and completed critical revision of the article. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The data were obtained from the SEER database, and the local research ethics committee confirmed that ethical approval was not required. No personal identifying information was used in the study. Hence, we did not require Institutional Review Board approval or patient informed consent.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cui, D., Xie, S. & Liu, Q. Postoperative survival of pulmonary invasive mucinous adenocarcinoma versus non-mucinous invasive adenocarcinoma. BMC Pulm Med 23, 9 (2023). https://doi.org/10.1186/s12890-023-02305-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02305-x