Abstract
Background
Cystic fibrosis (CF) and chronic obstructive pulmonary disease (COPD) are often associated with airway fluid acidification. Mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene leads to impaired bicarbonate secretion contributing to CF airway pathology. Chronic cigarette smoke (CS) -the major cause of COPD- is reported to induce acquired CFTR dysfunction underlying airway acidification and inflammation. We hypothesize that bicarbonate-containing aerosols could be beneficial for patients with CFTR dysfunctions. Thus, we investigated the safety of hypertonic sodium bicarbonate (NaHCO3) inhalation in CS-exposed guinea pigs.
Methods
Animals were divided into groups inhaling hypertonic NaCl (8.4%) or hypertonic NaHCO3 (8.4%) aerosol for 8 weeks. Subgroups from each treatment groups were further exposed to CS. Respiratory functions were measured at 0 and after 2, 4, 6 and 8 weeks. After 8 weeks blood tests and pulmonary histopathological assessment were performed.
Results
Neither smoking nor NaHCO3-inhalation affected body weight, arterial and urine pH, or histopathology significantly. NaHCO3-inhalation did not worsen respiratory parameters. Moreover, it normalized the CS-induced transient alterations in frequency, peak inspiratory flow, inspiratory and expiratory times.
Conclusion
Long-term NaHCO3-inhalation is safe in chronic CS-exposed guinea pigs. Our data suggest that bicarbonate-containing aerosols might be carefully applied to CF patients.
Similar content being viewed by others
Background
Cystic fibrosis (CF) is a fatal hereditary condition caused by mutations in the cystic fibrosis conductance regulator (CFTR) gene. Although it is a multiorgan disorder, morbidity and mortality are attributed to progressive airway complications, exhibited as chronic obstructive lung disease. Over the last decades, chronic respiratory diseases (CRDs) such as chronic obstructive pulmonary disease (COPD), asthma and bronchiectasis have become leading causes of morbidity and mortality worldwide. Despite the different pathogeneses, COPD and CF share common phenotypic features, such as airflow limitation, mucus obstructions and progressive deterioration of pulmonary function [1]. Impaired mucus clearance leads to repeated lung infections and may contribute to the chronicity of COPD, thus physiological airway functions are closely correlated to epithelial ion and water transport [2]. Airway acidification has been shown in both CF and COPD [3, 4], which could be due to defective bicarbonate (HCO3−) transport through the CFTR anion channel [5]. In fact, CFTR−/− pigs exhibit reduced airway pH and impaired bacterial killing, which are increased after aerosolizing NaHCO3 into the trachea [6]. While CF is relatively rare, other CRDs affect hundreds of millions of people worldwide. Importantly, growing body of evidence suggests that acquired CFTR dysfunction underlies chronic rhinosinusitis, COPD, non-atopic asthma, non-CF bronchiectasis and tobacco smoke-induced pulmonary diseases [7, 8]. It has been reported that cigarette smoke exposure, the major cause of COPD, leads to downregulation of CFTR mRNA, protein and function [9,10,11] and CFTR activity is reduced in smokers both with and without COPD associated with chronic bronchitis and the severity of dyspnea [12]. Such an acquired CFTR-dysfunction can also reduce the mucociliary clearance and may contribute to COPD pathogenesis [3, 13]. Furthermore, uncompensated proton secretion tends to further acidify the airways which could be an important pathogenic factor in CRDs [14]. Ivacaftor, and GLPG2196 CFTR potentiators have already been shown to reverse cigarette smoke extract-induced CFTR-dysfunctionin vitro and COPD ferrets as well, respectively [15, 16]. Therefore, drugs developed to enhance CFTR activity might also be beneficial in COPD patients [17].
Bicarbonate acts not only as a buffer, but it has many other important roles in the airways. Impaired bicarbonate secretion is likely to be responsible for aggregated mucus in CF mice [18] and pigs [19]. Re-administration of bicarbonate reduces mucus viscosity and corrects mucociliary transport [18]. These effects are especially important because viscous mucus and impaired mucociliary transport provide an appropriate environment for pathogen growth, evoking immune response and inflammation. We have recently found that NaHCO3 inhibits both the growth and biofilm formation of bacteria relevant in CF [20, 21]. Moreover, in order to mimic sodium bicarbonate inhalation treatment, apical administration of 75 mM HCO3−-containing media to CF bronchial epithelial cells was also well-tolerated, suggesting that these cells can endure changes in tonicity, pH and HCO3− [22]. Furthermore, HCO3− alters bacterial susceptibility to antibiotics [23] and oral NaHCO3 activates splenic anti-inflammatory pathways [24].
Hypertonic saline nebulization has long been used as a mucolytic treatment for CF [25]. Animal studies also demonstrated the potential of hypertonic saline in alleviating mucus obstruction in a spontaneous lung disease model using βENaC transgenic mice exhibiting airway surface dehydration characteristic to CF and COPD [13]. However, the above-mentioned data suggest that inhalation of HCO3−-containing aerosols might be an even more effective therapeutic approach in CF and/or CRDs. It is no accident that usage of inhalation solution of mineral salt containing high amount of HCO3− (5.6 g/l) is recommended for patients with rhinosinusitis, acute or chronic bronchitis, COPD, bronchial asthma and CF [26]. However, to our best knowledge, no in vivo animal data are available on the effects of long-term hypertonic NaHCO3 inhalation.
In light of the listed beneficial effects of HCO3− as well as the cigarette smoke-induced acquired CFTR-deficiency we intended to investigate the impact of hypertonic NaHCO3 inhalation on general physiologic and respiratory parameters in a mild cigarette smoke-exposure model to mimic the molecular alterations characteristic to both CF and COPD. We have chosen this animal model because guinea pig lungs translate more to human airway pathophysiology [27]. On the other hand, CF mice do not exhibit lung disease presumably because of lacking ATP12A protein in the apical membrane of airway epithelial cells [3].
Materials and methods
Animals
Experiments were performed on 8-week-old male guinea pigs weighing 600 ± 150 g at the beginning of the study. Animals were bred and kept in the Laboratory Animal House of the Department of Pharmacology and Pharmacotherapy, University of Pécs, Hungary at 24–25 °C, provided with standard chow, vegetables and fruits and water ad libitum, maintained under 12 h light–dark cycle. All procedures were performed in accordance with the 40/2013 (II.14.) Government Regulation on Animal Protection and Consideration Decree of Scientific Procedures of Animal Experiments and Directive 2010/63/EU of the European Parliament. They were approved by the Animal Welfare Committee of the University of Pécs and the National Scientific Ethics Committee on Animal Research of Hungary (licence No.: BA02/2000–4/2019 issued on 29 Jan 2019 by the Government Office of Baranya County).
Experimental design
Guinea pigs were divided into 4 groups (4 animals/group); 2 groups treated with hypertonic NaCl (8.4% corresponding to 1.44 M) and the other 2 groups with hypertonic NaHCO3 (8.4% corresponding to 1 M) aerosol for 30 min, twice daily, 5 days/week, for 8 weeks. Hypertonic NaCl and NaHCO3 solutions were prepared freshly each week and were aerosolized by a nebulizer (1–5 μM particle size; Boneco 7145 W ultrasonic nebulizer, BonAir BG Ltd., Budapest, Hungary) into 55 × 35 × 40 cm boxes where guinea pigs were placed during inhalational treatment. The treatment groups were subdivided into groups inhaling only NaCl or NaHCO3, and groups exposed to cigarette smoke besides the respective aerosol treatments. Cigarette smoke exposure (CSE) was performed after aerosol treatment in a whole-body smoke exposure chamber (Teague Enterprise, USA) for 30 min followed by a ventilation period of 30 min twice daily, 10 times/week for 8 weeks with the use of 2 research cigarettes at a time (3R4F Kentucky Research Cigarette; University of Kentucky, USA) [28]. Body weight was measured daily, respiratory functions were assessed at the beginning and at the end of week 2, 4, 6 and 8. At the end of the experimental protocol animals were anaesthetized by pentobarbital sodium (1% Euthanimal 400 mg/ml, Alfasan, the Netherlands; 0.5 ml/100 g) and arterial as well as venous blood was collected for laboratory tests. Lungs were excised and fixed in 6% formaldehyde solution for histopathological assessment.
Investigation of respiratory functions
Airway function was measured by unrestrained whole-body plethysmography (WBP) (PLY3213 Buxco Europe Ltd., Winchester, UK) at the beginning and at the end of week 2, 4, 6 and 8 in conscious, spontaneously breathing guinea pigs. Breathing frequency, tidal volume, minute ventilation, inspiratory and expiratory times, peak inspiratory and expiratory flows, as well as baseline enhanced pause (Penh) correlating with airway resistance were measured for 15 min following a 15-min-long acclimation period.
Histopathological evaluation
Lung samples were fixed in 6% paraformaldehyde solution and embedded in paraffin. Hematoxylin–eosin staining was performed on 5 μm sections for the assessment of lung pathophysiology. Three different localizations (apex, hilus, base) were excised from the lungs of each animal. Slides were examined using a bright field microscope (Olympus CH30). Ten non-cartilaginous airways, ten vessels and ten septa (examined by high power field) were selected from each lung site of every group (equally chosen from each animal). Acute inflammatory cell infiltration (eosinophil and neutrophil granulocytes) was counted in the airways, vessels and septa to evaluate the extent of airway inflammation [29]. Airway intraluminal perimeter was measured with Case Viewer software (3DHISTECH Ltd, Hungary) after scanning each slide with 20 × objective (Pannoramic 250 FLASH III scanner, 3DHistech Ltd., Hungary). Airway intraluminal perimeter was used to normalize airway dimensions.
Laboratory parameters
Urine pH was assessed every week of the experimental protocol. Animals were placed in a metabolic cage for the period of urine collection. pH was assessed from freshly collected urine by a FiveEasyPlus™ pH meter (Mettler Toledo, Hungary). At the end of the experimental protocol arterial blood was collected for blood gas and acid base analysis by Astrup's equilibration technique in the Department of Laboratory Medicine, University of Pécs, Hungary. Other laboratory parameters were measured from heparinized venous blood by an AU5800 clinical chemistry analyzer (Beckman Coulter Hungary, Budapest, Hungary) in the Deparment of Laboratory Medicine, Semmelweis University, Budapest, Hungary.
Statistical analysis
Statistical analysis was performed by GraphPad Prism v6 software (GraphPad, San Diego, CA, USA). Respiratory parameters and body weight were analyzed by repeated measures two-way ANOVA followed by Tukey's multiple comparisons test. Histopathological and laboratory parameters were assessed by Kruskal–Wallis followed by Dunn's multiple comparisons test.
Results
Long-term NaHCO3 inhalation improves some CSE-induced transient respiratory alterations
Frequency, inspiratory and expiratory times, as well as peak inspiratory flow showed mild and transient significant alterations in response to CSE throughout the 8-week-long experimental protocol. In the 8.4% NaCl + CSE-treated group frequency and peak inspiratory flow significantly decreased, while inspiratory time increased compared to the non-smoking respective controls at the end of week 4 (Fig. 1a,c,e,g). These alterations were counteracted by 8.4% NaHCO3 treatment in CS-exposed animals. The protective effect of NaHCO3 is also supported by the facts that i) in contrast to the NaCl-treated animals, no significant differences developed in any parameters of the NaHCO3 + CSE-treated guinea pigs in comparison with the respective controls, and ii) the inspiratory and expiratory times were significantly shorter in the NaHCO3 + CSE group compared to the NaCl + CSE animals at weeks 2 and 6 (Fig. 1e, f). There were no changes in tidal volume, Penh and peak expiratory flow in any groups (Fig. 1b,d,h). At the end of the treatments no differences were revealed in the parameters of different experimental groups. The parameters were similar to intact conditions (Additional file 1: Fig. 1), thus long-term hypertonic NaHCO3 aerosol inhalation did not induce any respiratory functional deteriorations in either group.
Respiratory function parameters, such as (a) frequency, (b) tidal volume, (c) minute ventilation, (d) enhanced pause, (e) inspiratory time, (f) expiratory time, (g) peak inspiratory flow, (h) peak expiratory flow measured by unrestrained whole body plethysmography. n = 4/group, data represent means ± SEM, repeated measures two-way ANOVA followed by Tukey's multiple comparisons test *p < 0.05, **p < 0.005 vs. NaCl + CSE-treated group; #p < 0.05 ##p < 0.05 vs. NaCl-treatment
Histopathological changes
Chronic hypertonic NaHCO3 inhalation did not induce significant eosinophil (Fig. 2a–c) or neutrophil granulocyte infiltration (Fig. 2d–f) measured in the non-cartilaginous airways, vessels and septa of lung (Fig. 2g–i). There was no decreased airway intraluminal perimeter (Fig. 3f) either in the non-smoking (Fig. 3a, b) or CS-exposed (Fig. 3c,d) groups quantified by the Case Viewer software (3DHISTECH Ltd, Hungary) (Fig. 3e). There were some lymphoid follicles sporadically observed in the lung sections of NaCl-, NaCl + CSE-, as well as NaHCO3-treated guinea pigs. For representative histopathological pictures see Additional file 1: Fig. 2.
Histopathological assessment of inflammatory cells in the lung. Eosinophil (a-c) and neutrophil (d-f) granulocyte numbers measured in the airways (a,d,g), septa (b,e,h) and vessels (c,f,i). n = 10 measurements group, graph represents individual data and median; Kruskal–Wallis, followed by Dunn's multiple comparisons test
Assessment of airway intraluminal perimeter. Representative histopathological pictures of bronchioles of (a) NaCl, (b) NaHCO3, (c) NaCl + CSE, and (d) NaHCO3 + CSE-treated guinea pigs. Neither treatment induced significant changes in airway intraluminal perimeter (f). n = 10 measurements/group, graph represents individual data and median; Kruskal–Wallis followed by Dunn's multiple comparisons test. Panel (e) represents the method for measurement
Laboratory parameters
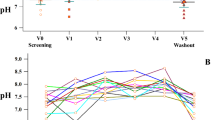
Parameters of electrolyte balance, such as sodium and chloride; creatinine referring to kidney and albumin, total protein, bilirubin, alkaline phosphatase (ALP) as well as alanine transaminase (ALT) levels indicating liver functions were within the normal range (Fig. 4 and Table 1). Hyperkalemia observed in all groups might be due to hemolysis upon blood collection. Chronic inhalation of hypertonic NaHCO3 did not induce metabolic alkalosis, the alkaline urine pH characteristic of herbivores was within the physiologic range. The arterial blood gas analysis performed before tissue harvesting revealed acute respiratory acidosis with elevated PaCO2 and acidotic arterial pH that could be most likely due to pentobarbital anaesthesia-induced respiratory depression.
Laboratory parameters and body weight change at the end of the treatment protocol. Urine pH (a), sodium (Na +) (b), creatinine (c) and albumin levels (d) of guinea pigs 8 weeks after hypertonic bicarbonate aerosol and chronic cigarette smoke exposure compared to sodium chloride treatment. Graph represents individual data and median; Kruskal–Wallis followed by Dunn's multiple comparisons test. Panel (e) demonstrates weight change throughout the 8-week-long protocol. Data represent means ± SEM, two-way ANOVA followed by Tukey's multiple comparisons test
The body weight gain of the animals was affected neither by hypertonic NaHCO3 aerosol treatment nor by CSE (Fig. 4e).
Discussion
Although sodium bicarbonate has been considered as a mucolytic agent for decades, there is no consensus about its usefulness in mucus clearance disorders [26]. Patients with CF and other CRDs instill natural inhalation solutions (i.e. spring waters of mineral salts), often without doctor’s recommendation. Although the composition of these solutions is different, high HCO3− concentrations (up to approx. 178 mM corresponding to 1.5%) is their common feature. Furthermore, a number of recent evidence suggests that HCO3− has not only mucolytic activity. It reduces inflammatory responses [24], inhibits bacterial growth and biofilm formation [20], enhances bacterial killing capacity of the innate immune system [6] and strengthens the efficacy of aminoglycosides [23] as well. Since all these effects would be desirable in CRDs, instillation of HCO3− on the airways could be of versatile remedy. Thus, there is an urgent need to define both beneficial and possible harmful effects of chronic administration of bicarbonate-containing aerosols in vivo. Data presented here provide evidence that 8-week-long inhalation of either hypertonic sodium bicarbonate (8.4%) or sodium chloride (8.4%) does not elicit harmful effects even in cigarette smoke-exposed guinea pig airways, and therefore both may be considered to be equally safe. Furthermore, some cigarette smoke-induced mild respiratory functional changes are improved compared to hypertonic sodium chloride (8.4%) treatment.
There are different animal models of CRDs such as CF mice, ferrets and pigs [30], as well as cigarette smoke-exposed mice, rats and guinea pigs of COPD [28, 29, 31]. However, CF ferret and pig models are not only expensive but also difficult to breed, whereas CF mice do not develop CF lung disease [32]. Therefore, we chose the cigarette smoke-exposed guinea pig model considering that these animals are easy to breed and their lung anatomy and physiology share common features with humans [31]. Our data could have important implications in CF as well, since recent studies suggest substantial overlap between COPD and CF due to CFTR dysfunction [1, 2, 11, 12, 17, 33]. Hypertonic NaCl has long been used in the treatment of CF and is known to improve lung function and to have marked benefits regarding exacerbations [25, 34,35,36]. The primary goal of this study was to investigate the safety of hypertonic sodium bicarbonate inhalation in vivo. Cigarette smoke-exposure COPD models suffer a disadvantage because only mild airway disease develops in the first few months [29]. Indeed, our study has limitations, since 8 week-long protocol has not promoted significant airway inflammation. In fact, we cannot exclude the possibility that the lack of any signs of airway inflammation might have been masked by the beneficial effects of the hypertonic NaCl or NaHCO3, which prevented CS-induced alterations. However, extended and more intense exposure is required to induce substantial inflammation and consequent airway remodelling in this experimental paradigm [29]. Another caveat regarding inhalation therapy is that bicarbonate may deposit in upper airways potentially reducing either its efficacy or possible side effects. Nonetheless, mathematical models would be needed to describe the deposition of inhaled particles based on their size and the anatomical distribution of the bronchial tree [37].
Since hypertonic sodium chloride (3–7%) instillation is a well-established medication for CF patients [25], we have tested the most concentrated sodium bicarbonate solution (8.4%) available for injection [38]. Nebulized sodium bicarbonate solution (4.2%) has been shown to have beneficial short-term effects in patients with reactive airway dysfunction syndrome [39]. Bronchoalveolar lavage with NaHCO3 is safe and inhibits bacterial and fungal growth in patient with lower respiratory tract infection[40]. Recently, we have demonstrated that hypertonic (300 mmol/L) NaHCO3 reduces the gel strength of CF sputum samples [41]. Furthermore, nebulized NaHCO3 (both 4.2% and 8.4%) was found safe and well tolerated in the management of CF patients [42].
Our data show that neither blood nor urine pH increased in HCO3−-treated animals indicating that long-term inhalation of 8.4% NaHCO3 has not induced systemic alkalosis. Furthermore, weight-gain was not different in any groups suggesting that both hypertonic NaCl and NaHCO3 have been well-tolerated. However, it should be emphasized that administration of aerosols containing high concentrations of NaHCO3 might induce unpredictable changes in tonicity, pH and volume of ASL in vivo.
Mucus hypersecretion has been implicated in both CF and COPD pathology [43]. Furthermore, it has been demonstrated that cigarette smoke induced MUC5AC mucus overproduction which further highlights its potential involvement in airway pathogenesis [44, 45]. Interestingly, as opposed to COPD, studies assessing CF airway secretions reported rather controversial results of MUC5AC and MUC5B mucins [46, 47]. However, it is beyond doubt that mucus hypersecretion is a key feature in the airway pathology. Guaifenesin has been shown to inhibit MUC5AC significantly, as opposed to other mucolytics as N-acetylcysteine and ambroxol (48). Therefore, a plausible additional beneficial effect of hypertonic NaCl and NaHCO3 inhalation might be the potential inhibition of mucus production, which should also be addressed in further studies.
Conclusion
We have demonstrated that 8-week-long inhalation of hypertonic NaHCO3 is as safe as NaCl in cigarette smoke-induced airway irritation guinea pig model. HCO3− should therefore be considered a potentially valuable therapeutic agent in chronic inflammatory airway diseases.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CF:
-
Cystic fibrosis
- CFTR:
-
Cystic fibrosis transmembrane conductance regulator
- COPD:
-
Chronic obsructive pulmonary disease
- CRD:
-
Chronic respiratory disease
- CS:
-
Cigarette smoke
- CSE:
-
Cigarette smoke exposure
- NaCl:
-
Sodium chloride
- NaHCO3 :
-
Sodium bicarbonate
References
Rab A, Rowe SM, Vamsee Raju S, Bebok Z, Matalon S, Collawn JF. Cigarette smoke and CFTR: implications in the pathogenesis of COPD. Am J Physiol Lung Cell Mol Physiol. 2013;305:530–41.
Livraghi A, Randell SH. Cystic fibrosis and other respiratory diseases of impaired mucus clearance. Toxicol Pathol. 2007;35(1):116–29.
Shah VS, Meyerholz DK, Tang XX, Reznikov L, Alaiwa MA, Ernst SE, et al. Airway acidification initiates host defense abnormalities in cystic fibrosis mice. Science. 2016;351(6272):503–7.
Kostikas K, Papatheodorou G, Ganas K, Psathakis K, Panagou P, Loukides S. pH in expired breath condensate of patients with inflammatory airway diseases. Am J Respir Crit Care Med. 2002;165(10):1364–70.
Riordan JR, Rommens JM, Kerem BS, Alon N, Rozmahel R, Grzelczak Z, et al. Identification of the cystic fibrosis gene: Cloning and characterization of complementary DNA. Science. 1989;245(4922):1066–73.
Pezzulo AA, Tang XX, Hoegger MJ, Abou Alaiwa MH, Ramachandran S, Moninger TO, et al. Reduced airway surface pH impairs bacterial killing in the porcine cystic fibrosis lung. Nature. 2012;487(7405):109–13.
Kreindler JL, Jackson AD, Kemp PA, Bridges RJ, Danahay H. Inhibition of chloride secretion in human bronchial epithelial cells by cigarette smoke extract. Am J Physiol Lung Cell Mol Physiol. 2005;288:894–902.
Banks C, Freeman L, Cho DY, Woodworth BA. Acquired cystic fibrosis transmembrane conductance regulator dysfunction. World J Otorhinolaryngol Head Neck Surg. 2018;4(3):193–9.
Hassan F, Nuovo GJ, Crawford M, Boyaka PN, Kirkby S, Nana-Sinkam SP, et al. MiR-101 and miR-144 regulate the expression of the CFTR chloride channel in the lung. PLoS ONE. 2012;7(11):e50837.
Savitski AN, Mesaros C, Blair IA, Cohen NA, Kreindler JL. Secondhand smoke inhibits both Cl-and K+conductances in normal human bronchial epithelial cells. Respirat Res. 2009;27;10(120).
Cantin AM, Hanrahan JW, Bilodeau G, Ellis L, Dupuis A, Liao J, et al. Cystic fibrosis transmembrane conductance regulator function is suppressed in cigarette smokers. Am J Respir Crit Care Med. 2006;173(10):1139–44.
Dransfield MT, Wilhelm AM, Flanagan B, Courville C, Tidwell SL, Raju SV, et al. Acquired cystic fibrosis transmembrane conductance regulator dysfunction in the lower airways in COPD. Chest. 2013;144(2):498–506.
Mall MA. Unplugging mucus in cystic fibrosis and chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2016;1(13):S177–85.
Lennox AT, Coburn SL, Leech JA, Heidrich EM, Kleyman TR, Wenzel SE, et al. ATP12A promotes mucus dysfunction during Type 2 airway inflammation. Sci Rep. 2018;8(1):1–13.
Raju SV, Lin VY, Liu L, McNicholas CM, Karki S, Sloane PA, et al. The cystic fibrosis transmembrane conductance regulator potentiator ivacaftor augments mucociliary clearance abrogating cystic fibrosis transmembrane conductance regulator inhibition by cigarette smoke. Am J Respir Cell Mol Biol. 2017;56(1):99–108.
Kaza N, Lin VY, Stanford D, Hussain SS, Libby EF, Kim H, et al. Evaluation of a novel CFTR potentiator in COPD ferrets with acquired CFTR dysfunction. Eur Respir J. 2021;2101581.
Fernandez Fernandez E, de Santi C, de Rose V, Greene CM. CFTR dysfunction in cystic fibrosis and chronic obstructive pulmonary disease. Vol. 12, Expert Review of Respiratory Medicine. Taylor and Francis Ltd.; 2018. p. 483–92.
Gustafsson JK, Ermund A, Ambort D, Johansson MEV, Nilsson HE, Thorell K, et al. Bicarbonate and functional CFTR channel are required for proper mucin secretion and link cystic fibrosis with its mucus phenotype. J Exp Med. 2012;209(7):1263–72.
Birket SE, Chu KK, Liu L, Houser GH, Diephuis BJ, Wilsterman EJ, et al. A functional anatomic defect of the cystic fibrosis airway. Am J Respir Crit Care Med. 2014;190(4):421–32.
Dobay O, Laub K, Stercz B, Kéri A, Balázs B, Tóthpál A, et al. Bicarbonate inhibits bacterial growth and biofilm formation of prevalent cystic fibrosis pathogens. Front Microbiol. 2018;9(SEP):1–12.
Jaikumpun P, Ruksakiet K, Stercz B, Pállinger É, Steward M, Lohinai Z, et al. Antibacterial effects of bicarbonate in media modified to mimic cystic fibrosis sputum. Int J Mol Sci. 2020;21(22):1–15.
Gróf I, Bocsik A, Harazin A, Santa-Maria AR, Vizsnyiczai G, Barna L, et al. The effect of sodium bicarbonate, a beneficial adjuvant molecule in cystic fibrosis, on bronchial epithelial cells expressing a wild-type or mutant CFTR channel. Int J Mol Sci. 2020;21:4024.
Farha MA, French S, Stokes JM, Brown ED. Bicarbonate alters bacterial susceptibility to antibiotics by targeting the proton motive force. ACS Infect Dis. 2018;4(3):382–90.
Ray SC, Baban B, Tucker MA, Seaton AJ, Chang KC, Mannon EC, et al. Oral NaHCO3 activates a splenic anti-inflammatory pathway; evidence cholinergic signals are transmitted via mesothelial cells. J Immunol. 2018;200(10):3568–86.
Reeves EP, McCarthy C, McElvaney OJ, Vijayan MSN, White MM, Dunlea DM, et al. Inhaled hypertonic saline for cystic fibrosis: Reviewing the potential evidence for modulation of neutrophil signalling and function. World J Crit Care Med. 2015;4(3):179–91.
Michel O, Essers S, Heppt WJ, Johannssen V, Reuter W, Hommel G. The value of Ems Mineral Salts in the treatment of rhinosinusitis in children: Prospective study on the efficacy of mineral salts versus xylometazoline in the topical nasal treatment of children. Int J Pediatr Otorhinolaryngol. 2005;69(10):1359–65.
Ressmeyer AR, Larsson AK, Vollmer E, Dahlèn SE, Uhlig S, Martin C. Characterisation of guinea pig precision-cut lung slices: Comparison with human tissues. Eur Respir J. 2006;28(3):603–11.
Kemény Á, Csekő K, Szitter I, Varga ZV, Bencsik P, Kiss K, et al. Integrative characterization of chronic cigarette smoke-induced cardiopulmonary comorbidities in a mouse model. Environ Pollut. 2017;229:746–59.
Domínguez-Fandos D, Peinado VI, Puig-Pey R, Ferrer E, Musri MM, Ramírez J, et al. Pulmonary inflammatory reaction and structural changes induced by cigarette smoke exposure in the guinea pig. COPD J Chronic Obstruct Pulmonary Dis. 2012;9(5):473–84.
Lavelle GM, White MM, Browne N, McElvaney NG, Reeves EP. Animal models of cystic fibrosis pathology: phenotypic parallels and divergences. Biomed Res Int. 2016;2016:5258727.
Ghorani V, Boskabady MH, Khazdair MR, Kianmeher M. Experimental animal models for COPD: a methodological review. Tob Induc Dis. 2017;15(25):1–13.
Fisher JT, Zhang Y, Engelhardt JF. Comparative biology of cystic fibrosis animal models. Methods Mol Biol. 2011;742:311–34.
Shi J, Li H, Yuan C, Luo M, Wei J, Liu X. Cigarette smoke-induced acquired dysfunction of cystic fibrosis transmembrane conductance regulator in the pathogenesis of chronic obstructive pulmonary disease. Oxid Med Cell Longev. 2018;2018:6567578.
Wark P, McDonald VM, Jones AP. Nebulised hypertonic saline for cystic fibrosis. Cochrane Database Syst Rev. 2005; 20(3):CD001506.
Elkin MR, Robinson M, Rose BR, Harbour C, Moriarty CP, Guy BM, et al. A controlled trial of long-term inhaled hypertonic saline in patients with cystic fibrosis. N Engl J Med. 2006;354(3):229–40.
Enderby B, Doull I. Hypertonic saline inhalation in cystic fibrosis - Salt in the wound, or sweet success? Arch Dis Child. 2007;92(3):195–6.
Fernández Tena A, Casan Clarà P. Deposition of inhaled particles in the lungs. Vol. 48, Archivos de Bronconeumologia. 2012. p. 240–6.
Adeva-Andany MM, Fernández-Fernández C, Mouriño-Bayolo D, Castro-Quintela E, Domínguez-Montero A. Sodium bicarbonate therapy in patients with metabolic acidosis. Sci World J. 2014;2014:627673.
Aslan S, Kandiş H, Akgun M, Çakir Z, Inandi T, Görgüner M. The effect of nebulized NaHCO3 treatment on “RADS” due to chlorine gas inhalation. Inhalation Toxicol. 2006;18(11):895–900.
el Badrawy MK, Elela MA, Yousef AM, Abou El-Khier NT, Abdelgawad TT, Abdalla DA, et al. Effect of sodium bicarbonate 84% on respiratory tract pathogens. Chest Lung Res. 2018;1(1):3–7.
Budai-Szűcs M, Berkó S, Kovács A, Jaikumpun P, Ambrus R, Halász A, et al. Rheological effects of hypertonic saline and sodium bicarbonate solutions on cystic fibrosis sputum in vitro. BMC Pulmonary Med. 2021;21(225).
Gomez CCS, Parazzi PLF, Clinckspoor KJ, Mauch RM, Pessine FBT, Levy CE, et al. Safety, tolerability, and effects of sodium bicarbonate inhalation in cystic fibrosis. Clin Drug Invest. 2020;40(2):105–17. https://doi.org/10.1007/s40261-019-00861-x.
Radicioni G, Ceppe A, Ford AA, Alexis NE, Barr RG, Bleecker ER, et al. Airway mucin MUC5AC and MUC5B concentrations and the initiation and progression of chronic obstructive pulmonary disease: an analysis of the SPIROMICS cohort. Lancet Respir Med. 2021;9(11):1241–54.
Di YP, Zhao J, Harper R. Cigarette smoke induces MUC5AC protein expression through the activation of Sp1. J Biol Chem. 2012;287(33):27948–58.
Shao MXG, Nakanaga T, Nadel JA. Cigarette smoke induces MUC5AC mucin overproduction via tumor necrosis factor-converting enzyme in human airway epithelial (NCI-H292) cells. Am J Physiol Lung Cell Mol Physiol. 2004;287:420–7.
Henke MO, Renner A, Huber RM, Seeds MC, Rubin BK. MUC5AC and MUC5B mucins are decreased in cystic fibrosis airway secretions. Am J Respir Cell Mol Biol. 2004;31(1):86–91.
Niv Y, Ho SB, Rokkas T. Mucin secretion in cystic fibrosis: A systematic review. Vol. 39, Digestive Diseases. S. Karger AG; 2021. p. 375–81.
Seagrave JC, Albrecht HH, Hill DB, Rogers DF, Solomon G. Effects of guaifenesin, N-acetylcysteine, and ambroxol on MUC5AC and mucociliary transport in primary differentiated human tracheal-bronchial cells. Respiratory Res. 2012;13(98).
Acknowledgements
The Astrup equilibration technique was performed in the Department of Laboratory Medicine, University of Pécs, Medical School, Pécs, Hungary.
Funding
Open access funding provided by Semmelweis University. This work was supported by 20765–3/2018/FEKUTSRTAT, Higher Education Institutional Excellence Program of the Ministry of Human Capacities in Hungary; EFOP-3.6.2–16-2017–00006 LIVE LONGER, Human Resource Development Operational Program; EFOP-3.6.2–16-2017–00008, The role of neuro-inflammation in neurodegeneration: from molecules to clinics and GINOP-2.3.2–15-2016–00048 STAY ALIVE, Economic Development and Innovation Operational Program. The funding had no role in the design, execution, interpretation, or writing of the study.
Author information
Authors and Affiliations
Contributions
Á.Z. and Z.H. made substantial contributions to the conception; K.C. and L.D. performed the plethysmography measurements; D.H. performed the histopathological analysis, K.C., D.H., L.D., P.J., A.K., and B.K. performed data interpretation and analysis, Á.Z., Z.H. and K.C. were the major contributors in writing of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures were performed in accordance with the 40/2013 (II.14.) Government Regulation on Animal Protection and Consideration Decree of Scientific Procedures of Animal Experiments and Directive 2010/63/EU of the European Parliament. They were approved by the Animal Welfare Committee of the University of Pécs and the National Scientific Ethics Committee on Animal Research of Hungary (licence No.: BA02/2000–4/2019 issued on 29 Jan 2019 by the Government Office of Baranya County). The study was carried out in compliance with the ARRIVE guidelines.
Consent for publication
Not applicable.
Competing interests
Author Z. H. was employed by the company PharmInVivo Ltd. The company had no role in the design, execution, interpretation, or writing of the study. The remaining authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Figure 1. Respiratory function parameters after 8-week-long treatment with hypertonic NaCl or hypertonic NaHCO3 aerosol compared to intact guinea pigs. Long-term NaCl and NaHCO3 inhalational treatment does not alter respiratory parameters. Figure 2. Representative histopathological pictures of HE-stained lung sections of guinea pigs after 8-week long treatment with hypertonic NaCl, NaHCO3, NaCl+CSE and NaHCO3+CSE.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Csekő, K., Hargitai, D., Draskóczi, L. et al. Safety of chronic hypertonic bicarbonate inhalation in a cigarette smoke-induced airway irritation guinea pig model. BMC Pulm Med 22, 131 (2022). https://doi.org/10.1186/s12890-022-01919-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-022-01919-x