Abstract
Background
Obesity in children and adolescents is associated with increased morbidity and mortality due to multisystemic impairment, including deleterious changes in lung function, which are poorly understood.
Objectives
To perform a systematic review to assess lung function in children and adolescents affected by obesity and to verify the presence of pulmonary changes due to obesity in individuals without previous or current respiratory diseases.
Methods
A systematic search was performed in the MEDLINE-PubMed (Medical Literature Analysis and Retrieval System Online), Embase (Excerpta Medica Database) and VHL (Virtual Health Library/Brazil) databases using the terms “Lung Function” and “Pediatric Obesity” and their corresponding synonyms in each database. A period of 10 years was considered, starting in February/2008. After the application of the filters, 33 articles were selected. Using the PICOS strategy, the following information was achieved: (Patient) children and adolescents; (Intervention/exposure) obesity; (Control) healthy children and adolescents; (Outcome) pulmonary function alterations; (Studies) randomized controlled trial, longitudinal studies (prospective and retrospective studies), cross-over studies and cross-sectional studies.
Results
Articles from 18 countries were included. Spirometry was the most widely used tool to assess lung function. There was high variability in lung function values, with a trend towards reduced lung function markers (FEV1/FVC, FRC, ERV and RV) in obese children and adolescents.
Conclusion
Lung function, measured by several tools, shows numerous markers with contradictory alterations. Differences concerning the reported results of lung function do not allow us to reach a consensus on lung function changes in children and adolescents with obesity, highlighting the need for more publications on this topic with a standardized methodology.
Similar content being viewed by others
Authors summary
What is known?
(i) Obesity in children and adolescents is a risk factor to higher morbidity and mortality due to multisystemic impairment;
(ii) Obesity as a deleterious factor in lung function is poorly understood.
What is new?
(i) Spirometry was the most widely used tool to assess lung function in obesity and showed a high variability in its values, with a trend towards reduced lung function markers in children and adolescents with obesity;
(ii) Differences regarding the reported results of lung function do not allow us to reach a consensus on lung function changes in children and adolescents with obesity, highlighting the need for more publications on this topic with a standardized methodology.
Background
Obesity is a dysfunction that interferes with systems of the body and whose prevalence increases in epidemic proportion [1]. The comprehensive impact of obesity prompts researchers to reflect on its deleterious effects, which progressively worsen the quality of life of increasingly younger individuals, leading children and adolescents to suffer from impairments that had been previously observed in adults only [2, 3].
The respiratory system is one of the systems affected by obesity. Among adults, the most frequent findings in the comparison of lung function of healthy individuals versus individuals affected by obesity are the reduction in functional residual capacity (FRC) and expiratory reserve volume (ERV). One of the main reasons for these changes is the impairment of the respiratory mechanics. Excessive adipose tissue, mainly in the thorax and abdomen, causes an increase in the intra-abdominal pressure on the diaphragm and in the pressure of the fat tissue on the rib cage, hindering thoracic expansion and, consequently, lung compliance. This change leads to a reduction in lung volumes and capacities and is characteristic of a restrictive lung disease [4, 5].
Respiratory mechanics are not the only way of compromising lung function in obesity. There is also an inflammatory component that causes obstructive pulmonary disorders. Adipose tissue macrophages produce proinflammatory substances and adipocytes secrete hormones (adipokines), which reach the systemic circulation, and are able to act directly on the respiratory system or alter the immune response. The entire pathophysiological process favors the induction of bronchial hyperreactivity and may compromise pulmonary air flow [6,7,8].
The prevalence of obesity has increased worldwide, and although it is a relevant public health problem that affects all age groups, the role and methods to evaluate its impact on lung function in children and adolescents is still unclear, and full understanding of the topic is still far from being attained.
As the obesity and lung function are complex phenotypes and their interaction has not been well understood, we included Fig. 1 that summarizes the mechanisms of lung function impairment due to obesity. Despite the relevance of the topic, it is still not well-established when lung function damages related to obesity start. Studies with children and adolescents diverge in their conclusions. Body changes during childhood and adolescence, variations in age range as well as in ethnic/environmental/genetic specificities make understanding of the cause-effect relationship between obesity and lung function more difficult.
Obesity and its association with lung function have been more often studied to ascertain the diagnosis of patients with asthma. Obesity and asthma have shown increasing prevalence in the last decades, and at the same time, they share common aspects, including the inflammatory process [8,9,10].
Obesity and asthma have been described as concomitant risk factors, with characteristics of a cause-effect relationship. The assessment of lung function in individuals with obesity and without asthma has yielded mixed results. Comprehensive studies are needed to understand whether mechanical and inflammatory changes are present in childhood obesity and during the growth process. Further studies should verify whether the disorders manifest differently during childhood and adolescence due to body changes throughout these periods, especially in individuals without a known lung disease, which is the focus of this systematic review [8,9,10].
This systematic review aimed to assess lung function in children and adolescents with obesity and to verify the presence of pulmonary restrictive or obstructive damages due to obesity in individuals without previous or current respiratory diseases, including asthma.
Methods
A systematic search was conducted in MEDLINE-PubMed (Medical Literature Analysis and Retrieval System Online, Public Medline), Embase (Excerpta Medica Database) and VHL (Virtual Health Library – Brazil) databases. Platform-specific tools were used, considering the descriptors (PubMed – MeSH Terms, VHL – DeCS and Embase – Emtree Terms) and equivalent terms, as well as excluding the descriptor “asthma” in order to achieve the objective of the study. The terms used in each database are described in Table 1.
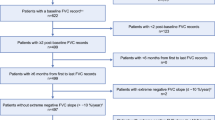
The articles were selected in three stages, as detailed in Fig. 2. The titles were first read and the articles that were not relevant to the review were excluded (358, 1,010 and 68 articles found in PubMed, Embase and VHL, respectively, were excluded). After the first database search filter was used, the articles were selected based on the abstracts (40, 35 and six articles found in PubMed, Embase and VHL, respectively, were excluded). In the third stage, the articles were read in full and then, carefully screened according to their relevance to the topic (10, 23 and seven articles found in PubMed, Embase and VHL, respectively, were excluded). Also, using the PICOS strategy, the following information was achieved: Patient – children and adolescents; Intervention (Exposure) – obesity; Control – healthy children and adolescents; Outcome – pulmonary function variability; Studies – randomized controlled trial, longitudinal studies (prospective and retrospective studies), cross-over studies and cross-sectional studies.
Eligibility criteria
In our study we included the following types of studies: randomized controlled trial, longitudinal studies (prospective and retrospective studies), cross-over studies and cross-sectional studies. Also, there was no restriction regarding the length of follow-up, and we considered only studies published between 2008 and 2018. We considered studies published in English, Spanish or Portuguese, and that were available in full text.
Information sources
All the studies were collected from the following databases: MEDLINE-PubMed, Embase and VHL databases. All the data was extracted directly from the studies and there was no contact with the study authors.
Search in the databases using descriptors
The following strategies were used to perform all searches in the study:
MEDLINE-PubMed.
(((((“Lung function”[Title/Abstract]) OR ((Respiratory Function Tests [MeSH Terms]) OR “Respiratory Function Tests”[Title/Abstract])) OR ((Spirometry [MeSH Terms]) OR Spirometry[Title/Abstract]))) AND (((((Obesity[MeSH Terms]) OR Obesity[Title/Abstract])) OR ((Pediatric Obesity[MeSH Terms]) OR “Pediatric Obesity”[Title/Abstract])) OR ((((((Childhood Obesity[MeSH Terms]) OR “Childhood Obesity”[Title/Abstract]) OR Adolescent Overweight[MeSH Terms]) OR “Adolescent Overweight”[Title/Abstract]) OR Adolescent Obesity[MeSH Terms]) OR “Adolescent Obesity”[Title/Abstract]))) NOT ((Asthma[MeSH Terms]) OR Asthma[Title/Abstract])
VHL
((tw:(Pediatric Obesity)) OR (tw:(Obesity, Pediatric)) OR (tw:(Childhood Obesity)) OR (tw:(Obesity, Childhood)) OR (tw:(Childhood Onset Obesity)) OR (tw:(Obesity, Childhood Onset)) OR (tw:(Child Obesity)) OR (tw:(Obesity, Child)) OR (tw:(Childhood Overweight)) OR (tw:(Childhood Overweights)) OR (tw:(Overweight, Childhood)) OR (tw:(Obesity in Childhood)) OR (tw:(Infant Obesity)) OR (tw:(Obesity, Infant)) OR (tw:(Infant Overweight)) OR (tw:(Overweight, Infant)) OR (tw:(Infantile Obesity)) OR (tw:(Obesity, Infantile)) OR (tw:(Adolescent Obesity)) OR (tw:(Obesity, Adolescent)) OR (tw:(Obesity in Adolescence)) OR (tw:(Adolescent Overweight)) OR (tw:(Overweight, Adolescent))) AND ((tw:(Lung function)) OR (tw:(Function Tests, Pulmonary)) OR (tw:(Function Test, Pulmonary)) OR (tw:(Pulmonary Function Test)) OR (tw:(Test, Pulmonary Function)) OR (tw:(Tests, Pulmonary Function)) OR (tw:(Function Test, Lung)) OR (tw:(Function Test, Respiratory)) OR (tw:(Function Tests, Lung)) OR (tw:(Function Tests, Respiratory)) OR (tw:(Lung Function Test)) OR (tw:(Respiratory Function Test)) OR (tw:(Test, Lung Function)) OR (tw:(Test, Respiratory Function)) OR (tw:(Tests, Lung Function)) OR (tw:(Tests, Respiratory Function)) OR (tw:(Lung Function Tests)) OR (tw:(Pulmonary Function Tests))) AND NOT (asthma)
Study selection
In brief, the study selection was carried out as represented in Fig. 2. Also, two authors (MFS and FALM or MFS and VLWW) decided about the eligibility before including the study in the review. In the presence of ambiguous conclusion, a third author (RTM or JDR) was contacted to perform a full consideration. Afterwards, a fourth author revised all the studies and the dataset to reach a final decision (RTM or JDR).
Data collection process
The data collection was carried out by two authors (MFS and FALM or MFS and VLWW), in this way, the data collection was performed twice for each study. Also, after the data extraction, the study was described as Table 2 and both authors included a summary using both datasets generated in the individual data collection. In the presence of ambiguous information, a third author (RTM or JDR) was contacted to perform a full consideration.
Results
As described in the methods, in brief, the articles were selected in three stages. A total of 48 articles were selected. After the exclusion of duplicates, 33 articles were included in the systematic review.
Table 2 shows a detailed informative and descriptive summary of the articles in this review: authorship, year of publication, place of study (country), study objective, presence or absence of respiratory disease, type of study, type of evaluation of lung function and type of posture and markers used in the analysis, main results and conclusions.
A wide age range (5 to 18 years) could be observed in the studies, with a higher prevalence between 11 and 13 years, which was an inclusion criterion in 69.7% (23/33) of the articles [11, 13,14,15, 17,18,19,20,21,22, 24,25,26,27, 29, 30, 32, 33, 35, 36, 38,39,40].
It is important to highlight the exclusion of studies that included participants with respiratory diseases, since the focus was to evaluate the pulmonary changes resulting exclusively (or with the least possible influence of other factors) from obesity. Therefore, including children with previous respiratory diseases could evolve into sampling (selection of individuals), confounding (proven impact on outcomes) or information bias (previous knowledge of an existing problem). In this context, 66.7% (22/33) [12,13,14,15, 17,18,19,20,21, 25, 26, 29, 32,33,34,35,36,37, 39,40,41,42] of the studies excluded individuals with respiratory diseases, 27.3% (9/33) [16, 22,23,24, 27, 28, 30, 31, 38] did not mention respiratory diseases as a factor of exclusion or non-inclusion, and 6% (2/33) [11, 43] excluded only individuals with a history of smoking. Among the studies that excluded previous respiratory diseases, several exclusion criteria could be observed: some authors excluded only individuals with exacerbation of asthma or cough; others excluded any respiratory conditions that might impair the evaluation; and others used standardized instruments such as the ISAAC questionnaire (The International Study of Asthma and Allergies in Childhood). This demonstrates the variability of methods adopted by the authors of the different studies, low standardization of exclusion/inclusion criteria, and difficulties/limitations to evaluate, diagnose and exclude patients with possible respiratory diseases in some specific cases among the evaluated children and adolescents [44].
Additionally, in the studies analyzed, the inclusion of healthy controls (HC), without obesity, was described as a criterion to compare lung function. In this context, 78.8% (26/33) [11, 13, 14, 16,17,18,19,20, 24,25,26,27,28,29,30,31,32,33,34,35,36,37,38, 41,42,43] of the studies compared individuals affected by obesity with HC.
The articles included were produced in 18 countries, with a predominance of European (8) [21,22,23, 31, 34, 35, 40], South American (8) [17, 18, 26, 32, 33, 37, 39, 41] and Asian (7) [11, 13, 15, 27, 30, 31, 42] countries. Also, 4 studies from North America were included [19, 24, 38, 43], as well as one from Central America [29], one from Oceania [20] and four from intercontinental countries ( three Euroasians [14, 25, 36] and one from Asia and Oceania [12]).
In the evaluation of lifestyle habits, 15.2% (5/33) [20, 24, 30, 41, 42] of the studies assessed the participation of individuals in physical activities. Also, 9.1% (3/33) [16, 20, 42] of the studies assessed screen time of the participants and one [24] study mentioned the use of a lifestyle habits questionnaire but did not detail the assessed variables.
There was no uniform definition of obesity among studies: 27.3% (9/33) [11, 14, 15, 20, 35,36,37, 40, 42] used references by Cole et al. [45,46,47]; 21.2% (7/33) [12, 17, 19, 26, 29, 38, 43] used the criteria established by the Center for Disease Control and Prevention (CDC); 15.1% (5/33) [13, 18, 33, 39, 41] used the definition of the World Health Organization (WHO); 12.1% (4/33) [16, 24, 32, 34] did not mention any references for the definition of obesity; and 27.3% (9/33) [14, 21,22,23, 25, 27, 28, 31, 36] used references according to their countries of origin. Two [14, 36] of the studies mentioned above, used references by Cole et al. [45,46,47] in addition to references according to their countries of origin.
Inflammatory markers were assessed and correlated with lung function in just 6% (2/33) [11, 21] of the studies, which is a quite low percentage, considering the systemic and complex nature of obesity, which requires an interdisciplinary approach. Among the studies that assessed inflammatory process, one study evaluated fraction of exhaled nitric oxide (FeNO) [11] and another serum levels of C-reactive protein (CRP), adiponectin, leptin, interleukin 6 (IL-6), tumor necrosis factor (TNF-α), monocyte chemoattractant protein-1 (MCP-1), visfatin and retinol binding protein 4 [21].
Spirometry was the most commonly used tool to assess lung function, i.e., in 93.9% (31/33) [11,12,13,14,15,16,17,18,19,20,21,22,23,24, 26, 27, 29,30,31,32,33,34,35,36,37,38,39,40,41,42,43] of the studies. Next, body plethysmography and measurement of the respiratory muscle strength (RMS) were the most used tools in 12.1% (4/33) [15, 19, 40, 43] and 9.1% (3/33) [18, 37, 41] of the studies, respectively. Optoelectronic plethysmography (OEP) [23, 37], impulse oscillometry (IOS) [28, 33] and peak expiratory flow measured by peak flow meter (PFE) were included in the analyses of 6.1% (2/33) [25, 32] of the studies. Other tools were used in only one study each: nitrogen [20] and helium [39] washout, FeNO [11], volumetric capnography (VolC) [26] and methacholine challenge testing [29].
Among the spirometry variables, forced expiratory volume in the first second (FEV1) of the forced vital capacity (FVC) was the most prevalent marker in the studies, included in 90.9% (30/33) [11, 12, 14,15,16,17,18,19,20,21,22,23,24, 26, 27, 29,30,31,32,33,34,35,36,37,38,39,40,41,42,43] of the analyses, followed by FVC and the FEV1/FVC ratio, used in 87.9% (29/33) [11,12,13,14,15,16,17,18,19,20,21,22,23,24, 26, 27, 29,30,31,32,33,34,35,36,37,38,39, 42, 43] and 72.7% (24/33) [11, 12, 14,15,16,17,18, 21,22,23,24, 26, 27, 31,32,33,34,35,36,37,38,39, 42, 43] of the studies, respectively. Forced expiratory flow between 25 and 75% of FVC (FEF25–75%) was also a widely assessed marker, being analyzed in 57.6% (19/33) [11, 14, 15, 17,18,19,20,21, 29,30,31,32,33,34,35,36, 39, 42, 43] of the studies. In addition, PEF and PFE were included in 33.3% (11/33) [11, 14, 17, 22, 23, 25, 29, 32, 36, 42] of the studies.
Among the variables analyzed using other tools besides spirometry, total lung capacity (TLC) and FRC could be observed in 21.2% (7/33) [15, 19, 20, 23, 39, 40, 43] and 18.2% (6/33) [15, 19, 20, 23, 40, 43] of the studies, respectively.
The comparison of the studies with a control group that showed comparative values or significant associations is described in Table 3. In this context, a great number of studies for each variable could be observed due to the selection of the various markers evaluated. No clear pattern emerged, as regards FEV1 and FVC, with about half of the studies reporting no association between obesity and lung function parameters [11, 14, 16,17,18,19,20, 26, 27, 29,30,31,32,33,34,35,36,37,38, 41,42,43]. A clearer pattern emerged as regards FEV1/FVC and FEF25–75%, as most studies found either a negative association or no association between obesity and lung function [11, 14, 16,17,18,19,20, 26, 27, 29,30,31,32,33,34,35,36,37,38, 41,42,43], with only one study reporting a positive association (Table 3) [13].
Discussion
Effects of growth and development on lung function
Childhood and adolescence are characterized by major changes in the structure and functions of the human body systems. The physiological processes that influence lung function in 6-year-old children are different from those influencing 15-year-old adolescents, even if we disregard other multiple factors, such as gender, ethnicity, environment and genetics. Changes in lung function of adults with obesity are related to increased intra-abdominal pressure due to the deposition of fat in this region, which compromises the efficiency of diaphragmatic mobility, as well as the deposition of fat on the rib cage, which reduces its compliance. However, such aspects are insufficient to understand the influence of obesity on lung function of children and adolescents [48, 49].
Figure 3 lists some factors that influence lung function in children and adolescents and that should be considered in the discussion about the variability of the findings in this systematic review. The first factor is the increase in lung volume and surface for gas exchange until approximately eight years of age. In this context, 45.5% (14/33) [11, 13, 16, 17, 22, 24,25,26,27,28, 33, 34, 38, 41] of the studies in this review included individuals under 8 years old – a period characterized by airway growth and development. Among these studies, 13 [11, 13, 16, 17, 22, 24,25,26,27, 33, 34, 38, 41] included, at the same time, individuals over eight years of age – a period, in which the respiratory tract is anatomically formed.
According to the literature, until the end of the preschool age, the respiratory tract growth follows a dysanaptic pattern, i.e., the growth of the airways is slower than the growth of the lung parenchyma. After this period, the growth is isometric, showing greater homogeneity. This pattern of growth up to early childhood may lead to increased airway resistance and higher risk of obstructive processes in these individuals, especially in males, who have proportionally smaller airways than females during this maturation period. Thus, the findings regarding lung function in children and adolescents should be analyzed considering the lung growth phase and the child’s development [49, 50].
The second and third factors described in Fig. 3 are interrelated and associated with changes arising from growth. The onset of puberty marks the beginning of a process of maturation, characterized by body and psychological changes. The changes vary according to gender, and in women, the pubertal development begins approximately two years earlier than in men. Moreover, hormonal changes may directly influence lung function: at first, by growth spurts, followed by increase in trunk height and ribcage diameter, which influence the increase in lung capacity and volumes. Another example is the increase in the production of male testosterone during puberty, which triggers a muscle growth peak, which includes the respiratory muscles and favors the increase of FVC and respiratory flows [51, 52].
Among individuals affected by obesity, the changes mentioned in the previous paragraph tend to occur at an earlier stage. Although the mechanisms are not yet well-established, studies have shown a relationship between insulin resistance and increased serum levels of leptin. Thus, comparing individuals of the same age group, at different stages of pubertal development and different genders, may be a bias in the analysis of lung function. Of the studies included in the systematic review, 21.2% (7/33) [14, 16, 21, 23, 32, 38, 43] analyzed pubertal development [53, 54].
The last item described in Fig. 3 is fundamental to understand lung function in children and adolescents and is associated with physical activities and sedentary lifestyle habits. In this context, we should emphasize that the comprehensive knowledge of the studied sample is of utmost importance. Today, the majority of the population is sedentary, and sedentary behaviors are not exclusively associated to the group of individuals affected by obesity. So, if the sample is composed of individuals with obesity under treatment/follow-up and HC with sedentary lifestyle habits, there may be a bias in relation to cardiorespiratory conditioning, which may affect lung function. Therefore, in the analysis of lung function in children and adolescents with obesity, information about physical activities and screen time is fundamental [55, 56].
Interestingly, despite the importance of this data, only 15.1% (5/33) [20, 24, 30, 41, 42] of the studies in this systematic review assessed participation in physical activities, 9.1% (3/33) [16, 20, 42] included the assessment of screen time, and 1 [24] study mentioned lifestyle habits without detailing the assessment items used.
Measurement tools to define obesity
Body mass index (BMI) was the most commonly used tool to determine obesity in children and adolescents. However, the criteria to define obesity varied among the studies. The option of using country-specific standards of normality or those published by the CDC or WHO, determined the lack of homogenization of the samples. Also, the cut-off points for the definition of obesity within the selected references were different. Therefore, the use of comparable criteria between the studies would allow a more precise definition regarding the presence of obesity in children and adolescents. Comprehensive references, including data collection at a global level, are best indicated as they analyze normality patterns, taking ethnic differences into account.
The amounts of body fat and lean mass make the assessment of lung function in individuals with obesity more reliable. This can be explained because BMI, which is the most commonly used indicative of obesity, shows some limitations. BMI measures excess weight rather than excess fat and the variability due to gender, age, ethnicity and lifestyle habits may act as modifiers. Thus, well-trained individuals with high lean mass indexes are classified with obesity [57, 58].
In this systematic review, only 12.1% (4/33) [15, 18, 23, 38] of the studies used instruments that allowed the quantification of body fat. The first study used bioimpedance (BIA) [23], which estimates fat mass, fat-free mass and total body water. The second study [18] used BIA and the skinfold measurement test, which estimates the amounts of fat in each segment. However, the literature reports that this method has its limitations for the assessment of individuals with obesity [59]. The third study [38] only analyzed the skinfolds, and the fourth [15] used BIA and dual energy X-ray absorptiometry (DXA), which is a more accurate tool, as DXA assesses the amount and distribution of fat and lean body mass. The analysis of the distribution of body fat is an important tool to detect alterations caused by impaired respiratory mechanics, which is greater with the increase in fat in the thorax and abdomen.
Obesity epidemic reflected on the diversity of the studied populations
The inclusion of studies with individuals from almost all continents, except for Africa, is relevant for the analysis of the findings. They reflect a global epidemic of obesity among children and adolescents. According to the WHO, the prevalence of overweight and obesity among children aged 5 to 19 years increased from 4% in 1975 to 18% in 2016. Currently, more than 124 million children and adolescents are affected by excess of weight. Weight gain trends include both developed and underdeveloped countries, and currently, overweight and obesity are more prevalent and more often associated with causes of death than underweight, except in some parts of Africa (especially sub-Saharan Africa) and Asia [60, 61].
Trends related to lung function in children and adolescents with obesity
The variability of the results showed an inability to establish lung function changes in children and adolescents with obesity. However, some trends have been detected and are discussed as follows.
Among the variables analyzed, the comparison of FEV1/FVC between individuals with obesity and HC was observed in 54.5% (18/33) [11, 12, 14, 16,17,18, 26, 27, 31,32,33,34,35,36,37,38, 42, 43] of the studies and of those, 55.6% (10/18) [11, 12, 16, 17, 26, 31, 34, 35, 38, 42] found lower value or negative association of the variable with obesity. The described changes may be an indication of the obstructive disorder in individuals affected by obesity during childhood and adolescence. The obstruction is related to pro-inflammatory activity of the adipose tissue, which could trigger bronchial hyperreactivity. Prior to our study, a review described similar findings regarding FEV1/FVC [62].
The analysis of inflammatory markers to identify systemic impacts caused by obesity was reported in only 6% (2/33) [11, 21] of the studies. One study [21] did not make any references to comparisons with the HC group. But, in another study [11], a positive association of FeNO with BMI was determined, suggesting that inflammation was more often detected in individuals affected by obesity and that these inflammatory changes should be considered in the clinical evaluation.
Despite the changes in FEV1/FVC, in the 22 [11, 14, 16,17,18,19,20, 26, 27, 29,30,31,32,33,34,35,36,37,38, 41,42,43] studies that analyzed FEV1 in children and adolescents with obesity and HC, there were discrepancies in the findings to confirm the presence of obstructive ventilatory disorder: (i) 56.5% (13/23) [17, 19, 20, 26, 29, 31,32,33,34, 36, 37, 41, 43] found no differences or associations between the groups; (ii) 26.1% (6/23) [14, 16, 18, 27, 38, 42] found lower value or a negative association between FEV1 and obesity; (iii) 17.4% (4/23) [11, 24, 30, 35] found higher value or a positive association in individuals with obesity. Thus, FEV1 was not associated with lung function impairment in overweight individuals.
FEF25–75% should also be considered, as it is a marker of obstructive ventilatory disorder. Some studies indicate that this tool is more sensitive than FEV1, and it can detect early ventilatory changes, especially in the small airways [63, 64]. However, as with most variables, there was also variability in the results. In total, 48.5% (16/33) [11, 14, 17, 19, 20, 26, 29,30,31,32,33,34,35,36, 42, 43] of the studies analyzed FEF25–75% of individuals with obesity and HC and of those: (i) 43.8% (7/16) [19, 20, 30,31,32,33, 43] found no differences and associations between indicators of obesity and FEF25–75%; (ii) 46.7% (8/16) [14, 17, 26, 29, 34,35,36, 42] found lower value or a negative association of FEF25–75% with obesity; (iii) one (6.6%) [13] found a positive association between FEF25–75% and obesity in children and adolescents.
In short, FEV1/FVC was the spirometry marker with the greatest sensitivity to identify a possible obstructive process due to obesity in children and adolescents. However, the variability of this marker – and, even more of other indications of obstruction – was high, regardless of the study. Thus, the development of cohort studies on indicatives of growth stages and body development is of utmost importance, since these factors are different between individuals affected by obesity and HC and also influence lung function. Pubertal development or age cohorts considering the time of dysanaptic growth and isometric growth would considerably reduce confounding factors and allow better understanding of lung function changes due to obesity in children and adolescents.
In the evaluation of FVC, which indicates restrictive respiratory disorder, 66.7% (23/33) [11, 13, 14, 16,17,18,19,20, 24, 26, 27, 29,30,31,32,33,34,35,36,37,38, 42, 43] of the studies included comparison with HC and 43.5% (10/23) [14, 17, 20, 31,32,33, 36, 37, 42, 43] of them did not find any differences between individuals with or without obesity. Only 21.7% (5/23) [16, 18, 27, 34, 38] found a negative association or lower values of FVC in children and adolescents with obesity. In a systematic review conducted in 2012, the authors concluded that the literature references demonstrated an association between reduced FVC and FEV1 with obesity in children and adolescents, in disagreement with our findings [65].
Besides the spirometry variables, some other measures contributed to the analysis of lung function in children and adolescents with obesity. TLC, FRC and residual volume (RV) were markers used in only 9.1% (3/33) [19, 20, 43] of the studies comparing individuals with obesity and HC. All these studies reported that individuals affected by obesity showed lower value or a negative association of FRC and RV with obesity. However, there were no differences in relation to TLC. If TLC – which is the sum of the inspiratory capacity (IC), and FRC (FRC = RV + ERV) – does not present a difference between individuals with obesity and HC, and if FRC and RV are reduced, it can be assumed that IC should be higher in individuals affected by obesity. Only 2 [18, 43] studies analyzed this variable and found a higher value or a positive association of IC with obesity.
These results are in agreement with a systematic review published in 2016, which evaluated the effects of obesity on lung volume and capacity in children and adolescents, and found a reduction in some markers in obesity, especially the reduction in FRC, ERV and RV [66].
Issues on respiratory physiology and biomechanics requiring further investigation
The values for respiratory mechanics of individuals with obesity are incoherent. Some hypothesis and questions can be raised, namely:
-
(i).
Are individuals with obesity actually “stronger” and are, therefore, able to inspire more air?
-
(ii).
However, if there is an increase in RMS, considering the 9 [11, 14, 17, 25, 29, 32, 33, 36, 42] studies that analyzed peak expiratory flow measured by spirometry (individuals with obesity x HC), why did only 2 [11, 29] studies find a positive association with obesity? Why did 4 [17, 25, 32, 36] studies find lower value or a negative association between obesity and peak expiratory flow measured by spirometry? And, why did 3 [14, 33, 42] studies find no differences between groups?
-
(iii).
Are lung function changes in individuals with obesity due to the differences between males and females, since in females, there is a pattern of gynoid obesity, with higher fat concentration on the hip and legs; whereas in males, an android pattern occurs, with more volume of fat in the chest and abdomen?
-
(iv).
It is well-known that individuals affected by obesity tend to initiate pubertal development earlier than healthy individuals. So, is there greater muscle development among individuals with obesity, which tends to be balanced at the end of puberty? Can impairment of lung function in individuals with obesity be clearly observed after puberty?
Confounding biases to clarify the mechanisms that interfere with lung functions in children and adolescents affected by obesity
Obesity is a multisystemic dysfunction, and therefore it is difficult to control the variables in order to understand the damage caused to lung function. For this reason, we found high variability in the results. Given the studies included in this systematic review, we are not able to establish which ventilatory changes are due to obesity in children and adolescents, even excluding data whose focus was the influence of asthma on obesity, which is a bias in this analysis. There are mechanisms that correlate both dysfunctions and the causal relationship between them may hinder perception of what is actually a consequence of obesity and/or asthma [8,9,10].
The findings of this review, although inconclusive, may give us a direction for future research. The strategies include: greater sampling control; reduction of confounding variables; conducting interdisciplinary and longitudinal studies with individuals with obesity versus HC; detailed analysis of environmental and social aspects; validation of findings among different populations; larger sample size; inclusion of measurements of lean mass and fat mass in order to unify and establish better criteria to define obesity; and future studies aiming to associate different genetic aspects, with predisposition to variability for weight gain, as well as for the individual nuance of lung function.
Thus, the inclusion and analysis of lung function in children and adolescents have become fundamental. Pubertal staging should be considered in order to avoid the influence of early maturation of individuals affected by obesity on the overestimation of lung capacity. It is important to analyze fat distribution, considering the concentration of abdominal and thoracic fat as factors that directly influence lung function. For this analysis, the use of instruments, such as DXA, may help determine the influence of the distribution and amount of body fat on lung function.
Assessing RMS with manuvacuometry or the distribution of lean mass with DXA, or even amount of lean mass using BIA, also favours the understanding of the physical conditions that influence lung function in children and adolescents. In order to analyze physical conditions, it is also important to include the evaluation of programmed and non-programmed physical activities as well as the screen time.
It is essential to exclude previous respiratory conditions that may influence lung function and control variables that are indicatives of inflammation, including CRP, erythrocyte sedimentation rate, FeNO or serum levels of leptin, adiponectin, IL-6 and TNF-α, which will allow precise determination of the influence of overweight in lung function of children and adolescents with obesity.
Meta-analysis
Meta-analysis is the gold standard in order to interpret a specific topic such as the importance of lung function in cases of obesity in the pediatric population. However, as described in our data there is no standardization in the studies about lung function in children and adolescents with obesity. To perform a meta-analysis, a minimum of standardization should be applied in the data acquisition. However, looking for the data included in Table 2, the studies were performed using different methodologies and/or lung function tools and/or lung functions measures (markers). Moreover, the age range was not equal, and the objectives were different among the studies. In brief, articles [11, 13,14,15,16,17, 19, 20, 22, 25, 26, 28,29,30, 32,33,34,35,36,37,38, 40,41,42] were described as cross-sectional studies on children-adolescents without respiratory diseases, where spirometry markers (such as FVC, FEV1 and FEV1/FVC) were assessed, and the relation between lung function and body mass, expressed as either BMI or norm weight/overweight/obesity, was estimated. Those studies did not allow us to perform a meta-analysis because there is a disparity of study objectives, population type (age range, sex distribution), origin of the population, presence of other lung function measurement, obesity as an independent variable and the exercise analysis. The information about the disparities among the studies is shown in Table 2 and Table 4.
Conclusion
The different results observed for lung function in children and adolescents with obesity show that there is no consensus on the impairment in such individuals in the literature. Considering the influence of growth and development on the function of all systems, it is fundamental to control the variables to reduce sampling, information and confounding biases, as well as to enable the analysis of the deleterious effects of obesity. In this context, new studies should require greater control of variables that influence growth and development to better understand the influence of obesity on lung function of children and adolescents.
However, studies on individuals with obesity describe a trend towards lower FEV1/FVC, FRC, ERV and RV, suggesting that both mechanical and inflammatory impairments influence lung function throughout childhood and adolescence.
Studies on pubertal development would be significant for a standard comparison including hormonal and structural changes in this period and the onset and duration of maturation. The quantification and distribution of body fat and the analysis of lifestyle habits would promote coherence and standardization on this subject, favoring the clinical approach to individuals.
The prevalence of obesity has increased worldwide, and although it is a relevant public health problem that affects all age groups, the role and methods to evaluate its impact on lung function in children and adolescents have not been established yet, and full understanding of the topic is still far from being attained.
Availability of data and materials
This is a systematic review and we can give all the information about the articles used to develop the study if requested by a reader. MSF, FALM or JDR should be contacted to request the data.
Abbreviations
- -:
-
Studies that showed comparative markers with lower value in obesity or with negative association with variables that are indicative of obesity
- +:
-
Studies that showed comparative markers with greater value in obesity or positive associations with variables that are indicative of obesity
- 6MWT:
-
Six-minute walk test
- alv:
-
Alveolar
- ATS:
-
American Thoracic Society
- AX:
-
Reactance area
- BD:
-
Bronchodilator
- BIA:
-
Bioimpedance
- BMI:
-
Body mass index (Weight/Height2)
- BP:
-
Blood pressure
- CDC:
-
Center for Disease Control and Prevention
- CI:
-
Capnography index [(Slp2/Slp3)× 100]
- CRP:
-
C-reactive protein
- DBP:
-
Diastolic blood pressure
- DLCO :
-
Diffusing capacity of the lungs for carbon monoxide
- DSV:
-
Dead space volume
- DSV/TV:
-
Relation between dead space volume and tidal volume
- DXA:
-
Dual energy X-ray absorptiometry
- EIB:
-
Exercise-induced bronchospasm
- Embase:
-
Excerpta Medica Database
- ERS:
-
European Respiratory Society
- ERV:
-
Expiratory reserve volume
- EtCO2 :
-
End-tidal carbon dioxide
- FEF25–75% :
-
Forced expiratory flow between 25 and 75% of forced vital capacity
- FEF25% :
-
Forced expiratory flow at 25% of forced vital capacity
- FEF50% :
-
Forced expiratory flow at 50% of forced vital capacity
- FEF75% :
-
Forced expiratory flow at 75% of forced vital capacity
- FeNO:
-
Fraction of exhaled nitric oxide
- FEV0.75 :
-
Forced expiratory volume at 0.75 s
- FEV1 :
-
Forced expiratory flow in the first second of forced vital capacity
- FEV1/FVC:
-
Relation between forced expiratory volume in the first second and forced vital capacity
- FRC:
-
Functional residual capacity
- Fres:
-
Resonant frequency
- FuncVC:
-
Functional vital capacity
- FVC:
-
Forced vital capacity
- FVC/weight:
-
Forced vital capacity index by weight
- GINA:
-
Global Initiative for Asthma
- HC:
-
Healthy controls
- HDL:
-
High density lipoprotein
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- HR:
-
Heart rate
- Hz:
-
Hertz
- IC:
-
Inspiratory capacity
- IL-6:
-
Interleukin 6
- IOS:
-
Impulse oscillometry
- ISAAC:
-
The International Study of Asthma and Allergies in Childhood
- LAR:
-
Leptin to adiponectin ratio
- LLN:
-
Lower limit of normal
- MCP-1:
-
Monocyte chemotactic protein-1
- MEDLINE:
-
PubMed, Medical Literature Analysis and Retrieval System Online - Public Medline
- MEP:
-
Maximum expiratory pressure
- MIP:
-
Maximal inspiratory pressure
- MV:
-
Minute volume
- MVD:
-
Mixed ventilatory disorder
- MVV:
-
Maximum voluntary ventilation
- OEP:
-
Optoelectronic plethysmography
- OVD:
-
Obstructive ventilatory disorder
- pBMI:
-
BMI percentile
- PEF:
-
Peak expiratory flow measured by spirometry
- PFE:
-
Peak expiratory flow measured by Peak Flow Meter
- R20:
-
Central airway resistance
- R5:
-
Total resistance
- RMS:
-
Respiratory muscle strength
- RR:
-
Respiratory rate
- RV:
-
Residual volume
- RV/TLC:
-
Ratio of residual volume and total lung capacity
- RVD:
-
Restrictive ventilatory disorder
- SAH:
-
Systemic arterial hypertension
- SBP:
-
Systolic blood pressure
- Slp2 :
-
Slope of phase 2
- Slp2/TV:
-
Relation between slope of phase 2 and tidal volume
- Slp3 :
-
Slope of phase 3
- Slp3/TV:
-
Relation between slope of phase 3 and tidal volume
- SpO2 :
-
Peripheral oxygen saturation
- Tanner:
-
Pubertal developmental stage according to Tanner’s criteria
- Te:
-
Expiratory time
- Ti:
-
Inspiratory time
- TLC:
-
Total lung capacity
- TNF-α:
-
Tumor necrosis factor
- tot:
-
Total
- TV:
-
Tidal volume
- VC:
-
Vital capacity
- VCO2 :
-
Volume of exhaled carbon dioxide
- VHL:
-
Virtual Health Library (Brazil)
- VolC:
-
Volumetric capnography
- VTAB:
-
Tidal volume of the abdomen
- VTRCa:
-
Tidal volume of the abdominal rib cage
- VTRCa%:
-
Percentage of contribution of the tidal volume in the abdominal rib cage to the total tidal volume
- VTAB%:
-
Percentage of abdominal tidal volume contribution to tidal volume
- VTRCp:
-
Tidal volume of the pulmonary rib cage
- VTRCp%:
-
Percentage of contribution of the tidal volume in the rib cage to total tidal volume
- WC:
-
Waist circumference
- WHO:
-
World Health Organization
- WHR:
-
Waist hip ratio
- X5:
-
Reactance at 5 Hz
- Z5:
-
Respiratory impedance
- θ:
-
Phase transition between two compartments
References
GBD 2015 Obesity Collaborators, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27.
Bhadoria A, Sahoo K, Sahoo B, Choudhury A, Sufi N, Kumar R. Childhood obesity: causes and consequences. J Fam Med Prim Care. 2015;4(2):87–192.
Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360(9331):473–82.
Littleton SW. Impact of obesity on respiratory function. Respirology. 2012;17(1):43–9.
Melo LC, Silva MA, Calles AC. Obesity and lung function: a systematic review. Einstein (São Paulo). 2014;12(1):120–5.
Salome CM, King GG, Berend N. Physiology of obesity and effects on lung function. J Appl Physiol (1985). 2010;108(1):206–11.
Mancuso P. Obesity and lung inflammation. J Appl Physiol (1985). 2010;108(3):722–8.
Dixon AE, Holguin F, Sood A, Salome CM, Pratley RE, Beuther DA, et al. Anerican thoracic society ad hoc subcommittee on obesity and lung disease. An official American Thoracic Society workshop report: obesity and asthma. Proc Am Thorac Soc. 2010;7(5):325–35.
Farah CS, Salome CM. Asthma and obesity: a known association but unknown mechanism. Respirology. 2012;17(3):412–21.
Camilo DF, Ribeiro JD, Toro AD, Baracat EC, Barros Filho AA. Obesity and asthma: association or coincidence? J Pediatr. 2010;86(1):6–14.
Yao TC, Tsai HJ, Chang SW, Chung RH, Hsu JY, Tsai MH, et al. Obesity disproportionately impacts lung volumes, airflow and exhaled nitric oxide in children. PLoS One. 2017;12(4):e0174691.
Supriyatno B, Sapriani I, Hadinegoro SRS. Pulmonary dysfunction in obese early adolescents. Med J Indones. 2010;19(3):179–84.
Peng R, Li S, Zhang H, Zeng H, Jiang B, Liu Y, et al. Weight status is associated with blood pressure, vital capacity, dental decay, and visual acuity among school-age children in Chengdu, China. Ann Nutr Metab. 2016;69(3–4):237–45.
Özgen İT, Çakır E, Torun E, Güleş A, Hepokur MN, Cesur Y. Relationship between functional exercise capacity and lung functions in obese chidren. J Clin Res Pediatr Endocrinol. 2015;7(3):217–21.
Kongkiattikul L, Sritippayawan S, Chomtho S, Deerojanawong J, Prapphal N. Relationship between obesity indices and pulmonary function parameters in obese thai children and adolescents. Indian J Pediatr. 2015;82(12):1112–6.
Bekkers MB, Wijga AH, De Jongste JC, Kerkhof M, Postma D, Gehring U, et al. Waist circumference, BMI, and lung function in 8-year-old children: the PIAMA birth cohort study. Pediatr Pulmonol. 2013;48(7):674–82.
Ferreira MS, Mendes RT, Marson FAL, Zambon MP, Paschoal IA, Toro AA, et al. The relationship between physical functional capacity and lung function in obese children and adolescents. BMC Pulm Med. 2014;14:199.
Faria AG, Ribeiro MA, Marson FAL, Schivinski CI, Severino SD, Ribeiro JD, et al. Effect of exercise test on pulmonary function of obese adolescents. J Pediatr. 2014;90(3):242–9.
Davidson WJ, Mackenzie-Rife KA, Witmans MB, Montgomery MD, Ball GD, Egbogah S, et al. Obesity negatively impacts lung function in children and adolescents. Pediatr Pulmonol. 2014;49(10):1003–10.
Gibson N, Johnston K, Bear N, Stick S, Logie K, Hall GL. Expiratory flow limitation and breathing strategies in overweight adolescents during submaximal exercise. Int J Obes (Lond). 2014;38(1):22–6.
Del Río-Camacho G, Domínguez-Garrido MN, Pita J, Aragón I, Collado R, Soriano-Guillén L. Masa ventricular izquierda, espirometría basal forzada y perfil de adipocitocinas en niños obesos con y sin síndrome metabólico. An Pediatr. 2013;78(1):27–34.
Berntsen S, Edvardsen E, Carlsen KH, Kolsgaard ML, Carlsen KC. Effects of posture on lung function in obese children. Clin Respir J. 2011;5(4):252–7.
LoMauro A, Cesareo A, Agosti F, Tringali G, Salvadego D, Grassi B, et al. Effects of a multidisciplinary body weight reduction program on static and dynamic thoraco-abdominal volumes in obese adolescents. Appl Physiol Nutr Metab. 2016;41(6):649–58.
Chen Y, Rennie D, Cormier Y, Dosman JA. Waist circumference associated with pulmonary function in children. Pediatr Pulmonol. 2009;44(3):216–21.
Gundogdu Z, Eryilmaz N. Correlation between peak flow and body mass index in obese and non-obese children in Kocaeli, Turkey. Prim Care Respir J. 2011;20(4):403–6.
Ferreira MS, Mendes RT, Marson FAL, Zambon MP, Antonio MARGM, Paschoal IA, et al. Spirometry and volumetric capnography in lung function assessment of obese and normal-weight individuals without asthma. J Pediatr. 2017;93(4):398–405.
Alghadir AH, Aly FA. Effect of obesity on pulmonary functions among Saudi children. Biomed Res India. 2012;23(4):605–8.
Kalhoff H, Breidenbach R, Smith HJ, Marek W. Impulse oscillometry in preschool children and association with body mass index. Respirology. 2011;16(1):174–9.
Del Rio-Navarro BE, Blandon-Vijil V, Escalante-Domínguez AJ, Berber A, Castro-Rodriguez JA. Effect of obesity on bronchial hyperreactivity among Latino children. Pediatr Pulmonol. 2013;48(12):1201–5.
He Q, Wong TW, Du L, Jiang ZQ, Qiu H, Gao Y, et al. Respiratory health in overweight and obese Chinese children. Pediatr Pulmonol. 2009;44(10):997–1002.
Jeon YH, Yang HJ, Pyun BY. Lung function in Korean adolescent girls: in association with obesity and the menstrual cycle. J Korean Med Sci. 2009;24(1):20–5.
Silva LO, Silva PL, Nogueira AMOC, Silva MB, Luz GCP, Narciso FV, et al. Evaluation of exercise-induced bronchospasm assessed by peak flow meter in obese adolescent. Rev Bras Med do Esporte. 2011;17(6):393–6.
Assumpção MS, Ribeiro JD, Wamosy RMG, Figueiredo FCXS, Parazzi PLF, Schivinski CIS. Impulse oscillometry and obesity in children. J Pediatr. 2018;94(4):419–24.
Spathopoulos D, Paraskakis E, Trypsianis G, Tsalkidis A, Arvanitidou V, Emporiadou M, et al. The effect of obesity on pulmonary lung function of school aged children in Greece. Pediatr Pulmonol. 2009;44(3):273–80.
Cibella F, Bruno A, Cuttitta G, Bucchieri S, Melis MR, De Cantis S, et al. An elevated body mass index increases lung volume but reduces airflow in Italian schoolchildren. PLoS One. 2015;10(5):e0127154.
Torun E, Cakir E, Özgüç F, Özgen IT. The effect of obesity degree on childhood pulmonary function tests. Balkan Med J. 2014;31(3):235–8.
Silva L, de Barcelar J, Rattes CS, Sayão LB, Reinaux CA, Campos SL, et al. The influence of supine posture on chest wall volume changes is higher in obese than in normal weight children. Appl Physiol Nutr Metab. 2015;40(2):178–83.
Khan S, Little J, Chen Y. Relationship between adiposity and pulmonary function in school-aged Canadian children. Pediatr Allergy Immunol Pulmonol. 2014;27(3):126–32.
Assunção SN, Daltro CH, Boa Sorte NC, Ribeiro Junior HC, Bastos ML, Queiroz CF, et al. Lung function in the absence of respiratory symptoms in overweight children and adolescents. J Bras Pneumol. 2014;40(2):134–41.
van de Griendt EJ, van der Baan-Slootweg OH, van Essen-Zandvliet EE, Van der Palen J, Tamminga-Smeulders CL, Benninga MA, et al. Gain in lung function after weight reduction in severely obese children. Arch Dis Child. 2012;97(12):1039–42.
Rosa GJ, Schivinski CIS. Assessment of respiratory muscle strength in children according to the classification of body mass index. Rev Paul Pediatr. 2014;32(2):250–5.
Paralikar SJ, Kathrotia RG, Pathak NR, Jani MB. Assessment of pulmonary functions in obese adolescent boys. Lung India. 2012;29(3):236–40.
Rastogi D, Bhalani K, Hall CB, Isasi CR. Association of pulmonary function with adiposity and metabolic abnormalities in urban minority adolescents. Ann Am Thorac Soc. 2014;11(5):744–52.
Solé D, Camelo-Nunes IC, Wandalsen GF, Mallozi MC. Asthma in children and adolescents in Brazil: contribution of the international study of asthma and allergies in childhood (ISAAC). Rev Paul Pediatr. 2014;32(1):114–25.
Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7(4):284–94.
Cole TJ, Flegal KM, Nicholls D, Jackson AA. Body mass index cut offs to define thinness in children and adolescents: international survey. Br Med J. 2007;335(7612):194–7.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Estabilishing a standard definition for child overweight and obesity worldwide : international survey. BMJ. 2000;320:1240.
Stanojevic S, Wade A, Stocks J, Hankinson J, Coates AL, Pan H, et al. Reference ranges for spirometry across all ages: a new approach. Am J Respir Crit Care Med. 2008;177(3):253–60.
Lebowitz MD, Sherrill DL. The assessment and interpretation of spirometry during the transition from childhood to adulthood. Pediatr Pulmonol. 1995;19(2):143–9.
Becklake MR, Kauffmann F. Gender differences in airway behaviour over the human life span. Thorax. 1999;54(12):1119–38.
Nève V, Girard F, Flahault A, Boulé M. Lung and thorax development during adolescence: relationship with pubertal status. Eur Respir J. 2002;20(5):1292–8.
Rogol AD, Clark PA, Roemmich JN. Growth and pubertal development in children and adolescents : effects of diet and physical activity. Am J Clin Nutr. 2000;72(2):521S–8S.
De Leonibus C, Marcovecchio ML, Chiarelli F. Update on statural growth and pubertal development in obese children. Pediatr Rep. 2012;4(4):e35.
Solorzano CMB, Mccartney CR. Obesity and the pubertal transition in girls and boys. Reproduction. 2010;140(3):399–410.
Laurson KR, Eisenmann JC, Welk GJ, Wickel EE, Gentile DA, Walsh DA. Combined influence of physical activity and screen time recommendations on childhood overweight. J Pediatr. 2008;153(2):209–14.
LeBlanc AG, Katzmarzyk PT, Barreira TV, Broyles ST, Chaput JP, Church TS, et al. Correlates of total sedentary time and screen time in 9-11 year-old children around the world: the international study of childhood obesity, lifestyle and the environment. PLoS One. 2015;10(6):e0129622.
Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutr Today. 2015;50(3):117–28.
Department of Health and Human Services, Centers for Disease Control and Prevention. Body mass index: considerations for practitioners. Atlanta: Centers for Disease Control and Prevention. Available from: www.cdc.gov/obesity/downloads/bmiforpactitioners.pdf. Accessed 2018.
Watts K, Naylor LH, Davis EA, Jones TW, Beeson B, Bettnay F, et al. Do skinfolds accurately assess changes in body fat in obese children and adolescents? Med Sci Sports Exerc. 2006;38(3):439–44.
NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–42.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384(9945):766–81.
Robinson PD. Obesity and its impact on the respiratory system. Paediatr Respir Rev. 2014;15(3):219–26.
Rao DR, Gaffin JM, Baxi SN, Sheehan WJ, Hoffman EB, Phipatanakul W. The utility of forced expiratory flow between 25 and 75% of vital capacity in predicting childhood asthma morbidity and severity. J Asthma. 2012;49(6):586–92.
Simon MR, Chinchilli VM, Phillips BR, Sorkness CA, Lemanske RF Jr, Szefler SJ, et al. Childhood asthma research and education network of the National Heart, lung and blood institute. Forced expiratory flow between 25 and 75% of vital capacity and FEV1/forced vital capacity ratio in relation to clinical and physiological parameters in asthmatic children with normal FEV1 values. J Allergy Clin Immunol. 2010;126(3):527–34.
Tenório LHS, Santos AC, de Oliveira AS, de Lima AMJ, Brasileiro-Santos MS. Obesidade e testes de função pulmonar em crianças e adolescentes: Uma revisão sistemática. Rev Paul Pediatr. 2012;30(3):423–0.
Winck AD, Heinzmann-Filho JP, Soares RB, da Silva JS, Woszezenki CT, Zanatta LB. Effects of obesity on lung volume and capacity in children and adolescents: a systematic review. Rev Paul Pediatr. 2016;34(4):510–7.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MSF, FALM, JDR and RTM conception and design of the work, data collection, data analysis and interpretation, drafting the article and critical revision of the article. VLWW data analysis and interpretation and drafting the article. The authors approved the final draft prior to submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no competing of interest to declare;
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Institution where the study was conducted: School of Medical Sciences, Unicamp, Campinas, São Paulo, Brazil.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ferreira, M.S., Marson, F.A.L., Wolf, V.L.W. et al. Lung function in obese children and adolescents without respiratory disease: a systematic review. BMC Pulm Med 20, 281 (2020). https://doi.org/10.1186/s12890-020-01306-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-020-01306-4