Abstract
Background
We aimed to explore the association of socioeconomic status (SES) and life’s essential 8 (LE8) with cardiovascular disease (CVD) and all-cause mortality in north China.
Methods
A total of 91,365 adults from the Kailuan study were included in this study. Comprehensive individual SES, mainly including monthly household income, education, Occupation position, and community environment, was confirmed by latent class analysis. Furthermore, the mediation and combination effects of SES and LE8 on CVD and all-cause mortality were further assessed. The Cox regression model was conducted to estimate HRs and 95% CI.
Results
During about 13 years of follow-up, 7,646 cardiovascular events and 11,749 deaths were recorded. Relative to the high SES, there were decreased risks of CVD [HR (95% CI): 1.57(1.43–1.72)] and high all-cause death [HR (95% CI): 1.43(1.31–1.53)] in the low SES. The associations between SES and CVD [Mediation % (95% CI): 22.3 (16.4–30.4)] and mortality [Mediation % (95% CI): 10.1 (7.1–14.0)] were partially mediated by LE8 when comparing medium SES to high SES. Meanwhile, relative to high LE8, the elevated risk of death [HR (95% CI): 1.72(1.56–1.89)], and incident CVD [HR (95% CI): 3.34(2.91–3.83)] were detected in low LE8. Compared to participants who had the high SES and LE8, participants who had both the low SES and LE8 further increased the risk of CVD [HR (95% CI): 7.76(5.21–11.55)] and all-cause mortality [HR (95% CI): 2.80(2.19–3.58)].
Conclusion
Low SES was related to a higher risk of CVD and mortality in low- and middle-income countries, which was partially mediated by LE8.
Similar content being viewed by others
Background
Cardiovascular diseases (CVDs) rank first among the global causes of non-communicable disease deaths and are an important factor leading to adult disability [1, 2]. Over the past three decades, the incidence of CVDs in China has steadily increased, reaching 330 million cases by 2020 [3]. Concurrently, deaths due to CVDs rose from 3.09 million in 2005 to 4.58 million in 2020 [3]. Moreover, the impact of low SES on CVDs and all-cause mortality may be more pronounced in low- and middle-income countries (LMICs) compared to high-income countries (HICs) [4]. In developed countries, individuals with low SES experience a 1.26-fold higher risk of mortality compared to those with high SES [5], while in China, this risk increases to1.8-fold [6]. Although some studies conducted in developed countries have found an association between SES and cardiovascular health [7], few studies have focused on developing countries.
The American Heart Association (AHA) has proposed an updated and enhanced conception of “Life’s Essential 8 (LE8)” in 2022, in which sleep is considered an additional essential component for improving cardiovascular health [8]. Previous research has demonstrated that healthy lifestyle habits may partially ameliorate the relationship between SES and mortality from CVD [9, 10]. However, the extent to which LE8 can improve CVD and mortality outcomes across different SES levels remains unclear, and the combined effects of LE8 and SES on health outcomes are yet to be determined. Since 2004, the cost of managing cardiovascular diseases in China has risen annually by 18.6%, presenting major challenges to limited medical resources [3]. There is an urgent need to identify the populations with the highest rates of sudden CVD and all-cause mortality, especially in LMICs with limited medical resources.
Socioeconomic inequalities regarding mortality and CVD have been widely noted in developed countries, and low SES is positively associated with adverse health outcomes [11, 12]. Studies conducted in developed countries showed that 35.6% of premature deaths were attributable to differences in SES [13]. Specifically, the risk of death for individuals with low SES was found to be 1.26 times higher than for those with high SES [12]. Recently, a study based on the database of NHANES and UKB identified that low SES was associated with an extraordinary 26% and 15% risk of death and CVD [9]. Furthermore, the developed Asian countries, Korea, and Japan also indicated that the risk of death was 1.05 (95%CI:1.02–1.07) and 1.09 ((95%CI:1.07–1.12) for moderate and lower SES compared to higher SES [14]. However, research on the relationship between SES and CVD in low- and middle-income countries is limited, and there is currently no consistent conclusion [15,16,17,18]. Currently, a small amount of research in China assessed the relationship between SES and hypertension, blood lipid abnormalities, and mortality [19,20,21,22], with only one survey reporting a 40-80% increase in mortality for low SES [10]. When we conducted this survey, China belonged to the lower middle-income countries.
China is one of the largest developing countries experiencing rapid economic growth, urbanization, and population aging, all of which have contributed to a raised risk of CVDs [23]. Therefore, identifying and describing the SES in CVDs and mortality in China can provide valuable insights for decision-making in LMICs. Therefore, we analyzed the adult population in China to examine the disparities in CVDs and all-cause mortality based on SES, and to assess the effects of LE8 and SES on the disparities.
Methods
Study population
The Kailuan study is a prospectively community-based cohort study, the study design and procedure have been described in detail elsewhere [24, 25]. This study was allowed to the guidelines of the Declaration of Helsinki [26] and was approved by the ethics committee of the Kailuan General Hospital (No.2006-05). The informed consent was provided by each participant. A total of 155,418 active and retired employees aged 18 years or older of the Kailuan Group, Tangshan, China, were invited to participate in 2006. Finally, 101,510 adults (81,110 men and 20,400 women) agreed to participate and completed the first survey. The consent rate of this study was 65.31%. Four unified modules, including standardized questionnaire assessment, clinical examinations, and laboratory tests, were performed at baseline and biennial follow-ups by medical faculty (e.g., nurses and physicians) from 11 hospitals in the Kailuan community.
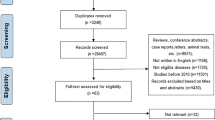
At present, we aimed to detect the potential effects of LE8 Metric and SES on CVD and all-cause death. A total of 3,923 participants with missing data on monthly household income, education, occupation, and community environment were excluded. Considering incomplete LE8 data, 2,600 participants were excluded. An additional 3,622 participants were excluded due to diagnoses of malignant tumors, strokes, or myocardial infarctions, as identified through standardized questionnaires, medical insurance records, and hospital records. A total of 91,365 participants with missing data < 5% for all included covariates were included in the final analysis after inclusion and exclusion (Fig. 1). Baseline characteristics between inclusion and exclusion seemed not different in the current study (Table S1).
Flow chart for the analysis of the association between SES, LE8 with cardiovascular disease and all-cause mortality. A total of 101,510 active and retired workers participated in the 2006–2007 health examination. Excluding those with incomplete income, education, occupation, community environment, and LE8 metrics. history of cardiovascular disease and cancer, 91,365 participants were included in the statistical analysis. The participants were followed until December 31, 2020. A total of 11,749 all-cause death, 7,646 cardiovascular events, 6,223 strokes, and 1,629 myocardial infarctions occurred
Assessment of SES
The quantification of the SES of a participant was based on monthly household income, education, Occupation position, and community environment using a standardized questionnaire according to the previous study [9, 27]. SES was created using a LCA according to four categorized socioeconomic factors (monthly household income: <¥800, ¥800–1000, and ≥¥1000; education: <9 years, 6–9 years, and ≥ 9 years; Occupation position: low, medium, and high; and community environment: low, medium, and high) [9, 10, 27]. The classification of occupational status was considered the work position and working environment. Participants who were managers and working on the ground were defined as having high occupational status. Participants who were managers but working down a mine were defined as having middle occupational status. Participants who were merely miners were considered as having low occupational status. The classification of community environment status was based on the surrounding environment and housing area. Housing areas larger than 100 m [2] and located away from factories and commercial areas were considered high. On the other hand, areas that are < 50 m [2] and situated near factories and commercial areas were classified as low. Any other housing areas fall into the medium range. Finally, four categories were respectively identified including high, medium, and low according to item response probability (Table S2 and Table S3) [28].
Assessment of LE8
The components of LE8 [8] consisted of the four health behaviors (daily diet, PA, tobacco exposure, and sleep duration) and four health factors (body mass index (BMI), non- high-density lipoprotein cholesterol (HDL-C), fasting blood glucose (FBG), and BP) for Chinese adults (Table S4) [29, 30]. Although detailed dietary information was not collected at baseline, salt intake effectively replaced the DASH-style diet among Chinese [31]. To comprehensively estimate the diet quality, tea drinking, and fatty food consumption were also incorporated [32,33,34,35]. The range of each metric was 0 to 100, and the overall LE8 score was calculated as the unweighted average of all 8 component metric scores for each participant. Using the cutting points suggested by FE8, it was defined as high LE8 (scores of ≥ 80), moderate LE8 (scores of 50–79), and low LE8 (scores of < 50).
Trained medical staff conducted the face-to-face interview to collect basic information, lifestyle (smoking, physical activity, sleeping duration, and diet habits), and health status (comorbidity and medication history) via a standardized questionnaire. BMI was measured as weight (kilograms) divided by height (meters squared). After 5 min of rest in the sitting position, blood pressure was recorded with an appropriate cuff blood pressure as previously described [24]. Venous blood samples were collected from the antecubital vein after an overnight fast (8–12 h). All blood samples were stored at -80℃ and analyzed in a blinded manner at the Central Laboratory of Kailuan General Hospital. In addition, an auto-analyzer (Hitachi 747; Hitachi, Tokyo, Japan) was used to analyze the blood samples at the central laboratory of Kailuan Hospital. FBG levels were measured using the hexokinase/glucose-6-phosphate dehydrogenase method (BioSino Bio-technology and Science Inc., Beijing, China), with the coefficient of variation using blind quality control specimens < 2.0% [36]. Fasting HDL-C concentrations were measured with the direct test method (Mind Bioengineering Co. Ltd, Shanghai, China) and with upper limits of detection of 12.90 and 3.88 mmol/L and total cholesterol (TC) with the endpoint test method. The intra- and inter-assay variable coefficients for each measurement were < 10% [37]. Non-HDL-C was calculated using TC subtract HDL-C.
Assessment of CVD and all-cause mortality
The main outcomes included incident CVDs, including stroke and myocardial infarction, and all-cause mortality. The outcomes in the prospective cohort were updated via medical insurance information and searching for hospital records until December 31, 2020. The diagnosis of CVD was performed as previously described [31, 38]. Myocardial infarction was diagnosed based on clinical symptoms, dynamic changes in cardiac enzymes and/or biomarker concentrations, and electrocardiogram results. Stroke was diagnosed based on clinical signs and symptoms, neuroimaging (via computed tomography or magnetic resonance imaging), and additional diagnostic reports. All participants were linked to the Municipal Social Insurance Institution and the Hospital Discharge Register for the incidence of CVDs according to the International Classification of Diseases, 10th (ICD–10) [39]. As suspected CVD events and the subtypes were determined by three experienced physicians who checked the medical records, the details of the diagnosis had been described elsewhere [40, 41]. Two major types of strokes, including cerebral infarction and cerebral hemorrhage (excluding epidural, subdural, or subarachnoid hemorrhage), were estimated in the current study. Mortality was collected from provincial vital statistics offices [36]. All participants were followed up every two years to collect data on CVDs and mortality. The follow-up for deaths was not terminated by CVDs. The endpoint of the follow-up was either the occurrence of the death or the last physical examination, whichever occurred first.
Covariates
The covariates were selected from previous studies [9, 10]. The face-to-face interview was performed by medical faculty to collect potential factors, including demographic factors (age, gender, marriage), daily behaviors (drinking, sedentary behavior, and snoring), comorbidity (hypertension, diabetes, atrial fibrillation, congestive heart failure, and fatty liver disease), and family history of related diseases (hypertension, diabetes, stroke, and myocardial infarction). Diabetes was diagnosed according to the American Diabetes Association guidelines, including a self-reported history of diabetes, FPG ≥ 7.0 mmol/L, or intake of anti-diabetes drug [42]. Hypertension was defined as the history of hypertension, the usage of the anti-hypertension drug, SBP ≥ 140 mmHg or DBP ≥ 90 mmHg [43].
Statistical analysis
Continuous variables with normal distribution were described as means ± standard deviation (SD) and compared using One-way ANOVA. Non-normally distributed continuous variables were presented as median and interquartile range and compared using the Mann-Whitney test. The categorized variables were described using frequencies (percentages) and compared using the χ [2] test.
Cox proportional hazard models which met the criteria of proportional hazard assumption were conducted to assess HR and 95% CI in our study. The proportional hazards assumption, assessed using log(-log[survival]) curves and the Schoenfeld residuals test (P > 0.05), was not violated. Model 1 was conducted after adjustment for demographic factors (age, gender, and marriage), lifestyle (drinking, sedentary, and snoring), chronic diseases (hypertension, diabetes, atrial fibrillation, congestive heart failure, and fatty liver disease), and family history of related diseases (hypertension, diabetes, stroke, and myocardial infarction). To further exclude the potential effect of LE8, we further adjusted LE8 in Model 2.
Moreover, mediation analysis was conducted to further explore the potential association of SES, LE8, CVDs, and mortality. We calculated the mediation proportion of LE8 in the association between SES and each outcome in Model 2. There were 5,000 repeated samples derived from a biased-corrected bootstrap used to obtain 95% CI for direct and indirect effects. Interaction analysis was performed to measure the interaction effect of SES and LE8 on outcomes by comparing nested models with and without the cross-product terms. In addition, the relative excess risk due to interaction (RERI) was also conducted to measure the additive interaction effect [44]. Furthermore, SES and LE8 were separately categorized as low, middle, and high, and created a 9-category variable to represent the combined effect [9, 10].
Sensitivity analyses were conducted. First, the associations between individual socioeconomic factors (monthly household income, education, occupational position, and community environment), CVDs, and mortality were examined. Second, we reanalyzed the data after excluding patients who had baseline or newly developed AF or CHF. Third, we re-run the results after further excluding the participants who had CVDs and death within the three years of follow-up to exclude potential reverse causation. Fourth, we additionally adjusted for the use of anti-hypertensive, anti-diabetic, and lipid-lowering medications during the follow-up period. Furthermore, stratified analyses were performed on age (< 60, ≥ 60) and gender to test potential variations among different subgroups. All analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC) and R (http://www.R-project.org; version 4.1.1). A two-sided P < 0.05 was considered significant.
Results
General clinical information
A total of 91,365 participants with a mean age of 51.0 years were included in this study. There were 79.5% males, consisting of high (15.6%), medium (49.4%), and low (35.0%) SES. Individuals with low SES tended to be older, male, and lower income, education, occupation position, and LE8 score. Moreover, the burden of chronic diseases was heavier in individuals with low SES than in the high SES population. The prevalence of drinking, snoring, and family history of hypertension, diabetes, and CVDs were higher in those with high SES than low SES (Table 1). Individuals excluded from the current analysis were more likely to be older, male, had more comorbidities and had low SES (Table S1). During follow-up, 11,749 deaths (median follow-up of 13.3 years) and 7,646 CVD cases (median follow-up of 12.9 years) were recorded. In addition, 6,223 stroke cases (median follow-up of 13.0 years) and 1,629 MI cases (median follow-up of 13.2 years) were also documented.
The risks of CVDs and mortality between high SES and low SES
Compared to high SES, the risk of death was higher in participants with medium SES [HR (95% CI):1.36 (1.27–1.46)] and low SES [HR (95% CI):1.40(1.29–1.50)]. For incident CVDs, the risks also increased in medium SES [HR (95% CI):1.36 (1.26–1.50)] and low SES [HR (95% CI):1.50 (1.37–1.65)]. Similarly, the risks of stroke [HR (95% CI):1.54 (1.39–1.71)] and MI [HR (95% CI):1.48 (1.21–1.80)] were increased in the low SES compared to the high SES (Table 2). When comparing low SES with high SES, each socioeconomic factor was associated with increased risks for death or CVD (Table S5-S8).
The association of LE8 with CVDs and mortality
Low LE8 score was associated with higher risks of mortality [HR (95% CI): 1.72(1.56–1.89)] and incident CVD [HR (95% CI): 3.34(2.91–3.83)] (Table S9). Furthermore, behavior health score and factor health score were associated with mortality and CVD, and the risks comparing low with high score were [HR (95% CI):1.22 (1.16–1.33)] and [HR (95% CI):1.43 (1.26–1.63)], and [HR (95% CI):1.79 (1.68–1.91)] and [HR (95% CI):2.92 (2.70–3.15)], respectively (Table S9). When low and medium SES were compared with high SES, the proportion mediated by the LE8 score were 7.1% (95% CI: 4.0-12.1%) and 10.1% (95% CI: 7.1–14.0%) for mortality, and 18.0% (95% CI: 12.7–26.2%) and 22.3% (95% CI: 16.4–30.4%) for CVDs. The highest mediation proportion of LE8 was detected in incident MI with 36.5% (95% CI: 21.2–64.4%, Table 2).
The association of LE8 with SES in CVDs and mortality
There was a multiplicative interaction between LE8 and SES on CVD, stroke, and cerebral infarction. However, there was no additive interaction in any of the outcomes (Fig. 2). It was noteworthy that the impacts of low LE8 on mortality, CVD, stroke, cerebral infarction, and myocardial infarction were all increased in higher SES. The hazard ratios for those with low LE8 for all-cause mortality were 2.11 (95% CI:1.53–2.90) among individuals with high SES and 1.75 (95% CI:1.46–2.11) among those with low SES. Similar patterns were found for incident CVD, stroke, and MI (Fig. 2). The results using individual socioeconomic factors were largely consistent with the primary analysis (Figures S1-S4). The combined effect of LE8 score and SES on all-cause mortality and CVD was further increased. Compared with individuals with high SES and LE8, the individuals with low SES and LE8 had the highest hazard ratio for all-cause mortality [HR (95% CI):2.80 (2.19–3.58)], CVD [HR (95% CI):7.76(5.21–11.55)], stroke [HR (95% CI):7.95(5.13–12.33)], and MI [HR (95% CI):6.98(2.74–17.77)] (Table 3), as well as when using individual socioeconomic factors in the analysis (Tables S10-S13).
Associations of LE8 score with All-cause mortality and CVDs (including stroke, CI, CH, and MI) by SES. HRs were adjusted for age, sex, drinking, sedentary, snoring, atrial fibrillation, congestive heart failure, fatty liver disease, and family history of diseases at baseline. Multiplicative interaction was evaluated using HRs for the product term between the LE8 score (Low versus High) and SES (low versus high), and the CI did not include 1 was statistically significant. Additive interaction was evaluated using RERI between the LE8 score (Low versus High) and SES (low versus high), and the CI did not include 0 was statistically significant
Sensitivity and subgroup analyses
The results derived from sensitivity and subgroup analyses were largely consistent with the primary results (Figures S5-S11 and Tables S14-S27). In contrast to men, low LE8 levels in women are associated with higher risks of death or CVD in low SES populations, rather than in high SES populations. Furthermore, the combined impacts of LE8 and SES on mortality and CVDs were more pronounced in individuals under the age of 60 years old than those over 60 years old. These trends were observed in different genders, with a stronger combined impact in males than in females.
Discussion
This is a rare large-scale cohort study from the largest LMIC revealing socioeconomic disparities in mortality and CVD, which were partially mediated by LE8. Low LE8 was associated with the risk of mortality and CVD across different SES levels. However, the risk was found to be highest in individuals with high SES. The combination of low SES and LE8 shows the highest risk of mortality and CVDs. Our study found that a low socioeconomic status increases the risk of cardiovascular disease by 50% and all-cause mortality by 40%. We further discovered that a similar phenomenon exists for stroke and myocardial infarction. It was suggested that low socioeconomic status is closely related to high incidence CVD and mortality, with higher risks in China than in developed countries.
Different socioeconomic statuses result in disparities in accessing health resources and maintaining healthy lifestyles [45]. However, the debate remains regarding whether health behaviors can reduce socioeconomic inequalities in adverse health events. The reasons for this heterogeneity in results may be numerous. Most previous studies have used single factors such as income level, education, employment status, and environmental factors to reflect individual SES, no comprehensive measurement of individual SES was performed [46,47,48,49]. In addition, previous studies have commonly employed a method whereby healthy behaviors are ranked from 0 to 1 for low, 2–3 for medium, and more than 3 for high, to define the level of cardiovascular health (CVH). While it is true that different health lifestyle factors may be correlated, each one reflects a different aspect of CVH and cannot simply be replaced by others. Furthermore, the socio-demographic characteristics of each study population vary due to differences in countries, ethnicities, cultural customs, and economic development levels [9, 10].
Given the reasons above, our study employed latent class analysis (LCA) to develop an overall measurement of SES [9, 10]. Additionally, we substituted the assessment of lifestyle with the LE8 score to evaluate cardiovascular health, as it encompasses both health factors and behaviors. A prospective cohort study conducted in developed countries found that, when comparing low SES to high SES, 12.3% of all-cause mortality was mediated by the lifestyle score (including smoking, alcohol consumption, physical activity, and diet) in the US NHANES, while 4.0% of all-cause mortality and 3.7% of incident CVD were mediated by the lifestyle score in the UK Biobank [9]. Similarly, a study conducted in China demonstrated that, when comparing low and medium SES to high SES, the proportion mediated by the overall lifestyle score (including smoking, physical activity, diet, and BMI) was 6.3% and 11.5% for all-cause mortality [10]. This study found that, in northern Chinese adults, when comparing low SES to high SES, 10.1% of the association between SES and mortality and 22.3% of the association with CVD were mediated by the individual LE8 score. Compared to previous studies, the LE8 score demonstrates a more pronounced mediating effect in the relationship between SES and CVD, largely attributed to variations in participant characteristics and the LE8 score’s more comprehensive evaluation of cardiovascular health. Obviously, both in developed and developing countries, health factors and health behaviors can only reduce health-related socioeconomic inequalities to a certain extent. Therefore, we still need to explore other measures to address health inequalities caused by SES disparities.
Unhealthy lifestyle habits are associated with a higher risk of mortality and cardiovascular events across different SES levels [9, 10]. However, the degree of this risk may vary depending on the level of development of the country. Studies in developed countries showed that a healthy lifestyle has a stronger protective effect on health outcomes among those in lower SES categories [9, 50]. On the other hand, research in China indicates that the protective effect of a healthy lifestyle is strongest among those in higher SES categories [10]. Our study has also found that individuals with low LE8 scores have a higher risk of mortality and cardiovascular events, and that high LE8 scores have a stronger protective effect for those in higher SES categories. We speculate that the reason for this difference may be related to the overall socioeconomic status of the country, the transition of social structure, and lifestyle changes. Over the past few decades, the Chinese economy has experienced significant growth and development. As a result, it has been observed that people with higher socioeconomic statuses tend to adopt Western cultural practices and lifestyles more frequently [51]. A meta-analysis including 39 LMICs demonstrated that higher SES groups tended to be less physical activity and consume more fat, salt, and processed foods than those of lower SES [52]. Therefore, individuals with higher socioeconomic in China may share similar characteristics with those with lower-middle socioeconomic in developed countries. Consequently, the protective effect of high LE8 scores in different SES categories may be influenced by the level of economic development in the country. In lower-middle-income countries, individuals in higher SES categories may benefit more from maintaining high cardiovascular health scores.
Our study found that there was no interaction between LE8 and SES about mortality, but there was an interaction for CVD, which is consistent with previous research results [9, 10, 53]. Furthermore, we found that compared to individuals with high SES and LE8 scores, those with low SES and LE8 scores had a 2.79-fold increased risk of mortality and a 7.76-fold increased risk of CVD events. These findings highlight the strong joint effect of adverse SES and lower cardiovascular health and the significant health risks associated with it. This result is consistent with evidence from developing and developed countries [9, 10], suggesting that more attention should be paid to this population.
In addition to this large-scale prospective cohort study, our study also employed a comprehensively measured SES using a reliable algorithm. Furthermore, this study provides the first insights into the mediation effects of LE8 and the combined effects of SES and LE8 on CVDs and all-cause mortality in a developing country. However, this study has some limitations. First, although a reliable classification method was employed for SES, potential misclassification may still exist. However, since SES was measured at baseline and any misclassification is unrelated to follow-up outcomes, it is considered non-differential. This type of misclassification may attenuate the observed association between SES and follow-up outcomes, potentially leading to an underestimation of the true effect size. Second, the association between time-varying SES and LE8 was not observed in the current study. Moreover, the participants were exclusively Chinese adults from the Kailuan community in northern China. Although this community includes residents with various occupations, the majority of participants are coal miners. Therefore, caution should be exercised when generalizing these findings to other populations. Finally, although we adjusted for significant covariates, residual confounding may still be present.
Conclusion
Our study reveals that low SES is positively associated with the risks of CVDs and mortality, and this association is mediated by LE8. In lower-middle-income countries, individuals with a higher SES may experience greater benefits from maintaining a high LE8 score. Moreover, the combined effects have been found, in which individuals with low SES and LE8 have the highest risks of CVDs and mortality.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- SES:
-
Socioeconomic Status
- CVD:
-
Cardiovascular disease
- LIC:
-
Low-income countries
- MIC:
-
Middle-income countries
- HIC:
-
High-income countries
- AHA:
-
The American Heart Association
- CVH:
-
Cardiovascular health
- AF:
-
Atrial fibrillation
- CHF:
-
Congestive heart failure
- PA:
-
Physical activity
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- LE8:
-
Life’s Essential 8
- MI:
-
Myocardial infarction
- FBG:
-
Fasting blood glucose
- TC:
-
Total Cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- SD:
-
Standard deviation
- CIs:
-
Confidence intervals
- HR:
-
Hazard ratio
- LMIC:
-
Low- and middle-income countries
References
Global burden of 369. diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222, https://doi.org/10.1016/s0140-6736(20)30925-9 (2020).
Roth GA, et al. Global, Regional, and National Burden of Cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70:1–25. https://doi.org/10.1016/j.jacc.2017.04.052.
W. Report on Cardiovascular Health and diseases in China 2022: an updated Summary. Biomed Environ Sci 36, 669–701, https://doi.org/10.3967/bes2023.106 (2023).
Yusuf S, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395:795–808. https://doi.org/10.1016/S0140-6736(19)32008-2.
Stringhini S, et al. Socioeconomic status and the 25 x 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1.7 million men and women. Lancet. 2017;389:1229–37. https://doi.org/10.1016/S0140-6736(16)32380-7.
Zhang YB, et al. Overall lifestyles and socioeconomic inequity in mortality and life expectancy in China: the China health and nutrition survey. Age Ageing. 2022;51. https://doi.org/10.1093/ageing/afac167.
Islam SJ, et al. Association between Early Trauma and Ideal Cardiovascular Health among Black americans: results from the Morehouse-Emory Cardiovascular (MECA) Center for Health Equity. Circ Cardiovasc Qual Outcomes. 2021;14:e007904. https://doi.org/10.1161/circoutcomes.121.007904.
Lloyd-Jones DM et al. Life’s Essential 8: Updating and Enhancing the American Heart Association’s Construct of Cardiovascular Health: A Presidential Advisory From the American Heart Association. Circulation 146, e18-e43, https://doi.org/10.1161/cir.0000000000001078 (2022).
Zhang YB, et al. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: two prospective cohort studies. BMJ. 2021;373:n604. https://doi.org/10.1136/bmj.n604.
Eggink E, et al. Attitudes and views on healthy lifestyle interventions for the prevention of dementia and cardiovascular disease among older people with low socioeconomic status: a qualitative study in the Netherlands. BMJ Open. 2022;12:e055984. https://doi.org/10.1136/bmjopen-2021-055984.
Foster HME, et al. The effect of socioeconomic deprivation on the association between an extended measurement of unhealthy lifestyle factors and health outcomes: a prospective analysis of the UK Biobank cohort. Lancet Public Health. 2018;3:e576–85. https://doi.org/10.1016/s2468-2667(18)30200-7.
Rosengren A, et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the prospective urban rural epidemiologic (PURE) study. Lancet Glob Health. 2019;7:e748–60. https://doi.org/10.1016/S2214-109X(19)30045-2.
Lewer D, et al. Premature mortality attributable to socioeconomic inequality in England between 2003 and 2018: an observational study. Lancet Public Health. 2020;5:e33–41. https://doi.org/10.1016/S2468-2667(19)30219-1.
Koohsari MJ, et al. Local-area walkability and socioeconomic disparities of Cardiovascular Disease Mortality in Japan. J Am Heart Assoc. 2020;9:e016152. https://doi.org/10.1161/JAHA.119.016152.
Goyal A, et al. Attained educational level and incident atherothrombotic events in low- and middle-income compared with high-income countries. Circulation. 2010;122:1167–75. https://doi.org/10.1161/circulationaha.109.919274.
Hurt LS, Ronsmans C, Saha S. Effects of education and other socioeconomic factors on middle age mortality in rural Bangladesh. J Epidemiol Community Health. 2004;58:315–20. https://doi.org/10.1136/jech.2003.007351.
de Bastos A. Family income and survival in Brazilian peritoneal Dialysis Multicenter Study patients (BRAZPD): time to revisit a myth? Clin J Am Soc Nephrol. 2011;6:1676–83. https://doi.org/10.2215/cjn.09041010.
Agarwal A, et al. Association between socioeconomic position and cardiovascular disease risk factors in rural north India: the Solan Surveillance Study. PLoS ONE. 2019;14:e0217834. https://doi.org/10.1371/journal.pone.0217834.
Pan Y, et al. Socioeconomic deprivation and mortality in people after ischemic stroke: the China National Stroke Registry. Int J Stroke. 2016;11:557–64. https://doi.org/10.1177/1747493016641121.
Chen R, et al. Socioeconomic deprivation and survival after stroke in China: a systematic literature review and a new population-based cohort study. BMJ Open. 2015;5:e005688. https://doi.org/10.1136/bmjopen-2014-005688.
Ying X, et al. Prevalences of metabolic syndrome and its sex-specific association with socioeconomic status in rural China: a cross-sectional study. BMC Public Health. 2021;21(2033). https://doi.org/10.1186/s12889-021-12074-z.
Li L, et al. Associations of Socioeconomic Status and Healthy Lifestyle with incidence of Dyslipidemia: a prospective Chinese Governmental Employee Cohort Study. Front Public Health. 2022;10:878126. https://doi.org/10.3389/fpubh.2022.878126.
Yang G, et al. Rapid health transition in China, 1990–2010: findings from the global burden of Disease Study 2010. Lancet. 2013;381:1987–2015. https://doi.org/10.1016/S0140-6736(13)61097-1.
Jin C, et al. Longitudinal change in fasting blood glucose and myocardial infarction risk in a Population without Diabetes. Diabetes Care. 2017;40:1565–72. https://doi.org/10.2337/dc17-0610.
Zhou YF, et al. Effectiveness of a Workplace-Based, Multicomponent Hypertension Management Program in Real-World practice: a propensity-matched analysis. Hypertension. 2022;79:230–40. https://doi.org/10.1161/HYPERTENSIONAHA.121.18305.
World Medical Association. Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4. https://doi.org/10.1001/jama.2013.281053.
Quaglia A, Lillini R, Mamo C, Ivaldi E, Vercelli M. Socio-economic inequalities: a review of methodological issues and the relationships with cancer survival. Crit Rev Oncol Hematol. 2013;85:266–77. https://doi.org/10.1016/j.critrevonc.2012.08.007.
Ni Y, Tein JY, Zhang M, Yang Y, Wu G. Changes in depression among older adults in China: a latent transition analysis. J Affect Disord. 2017;209:3–9. https://doi.org/10.1016/j.jad.2016.11.004.
Jin C, et al. Life’s essential 8 and 10-Year and lifetime risk of atherosclerotic Cardiovascular Disease in China. Am J Prev Med. 2023. https://doi.org/10.1016/j.amepre.2023.01.009.
Xing A, et al. Life’s essential 8 Cardiovascular Health with premature Cardiovascular Disease and all-cause mortality in young adults: the Kailuan prospective cohort study. Eur J Prev Cardiol. 2023. https://doi.org/10.1093/eurjpc/zwad033.
Wu S, et al. Association of Trajectory of Cardiovascular Health Score and Incident Cardiovascular Disease. JAMA Netw Open. 2019;2:e194758. https://doi.org/10.1001/jamanetworkopen.2019.4758.
Zhang Q, et al. Ideal cardiovascular health metrics and the risks of ischemic and intracerebral hemorrhagic stroke. Stroke. 2013;44:2451–6. https://doi.org/10.1161/strokeaha.113.678839.
Liu X, et al. Cumulative exposure to Ideal Cardiovascular Health and Incident Diabetes in a Chinese Population: the Kailuan Study. J Am Heart Assoc. 2016;5. https://doi.org/10.1161/jaha.116.004132.
Wu S, et al. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern Chinese industrial city. Circ Cardiovasc Qual Outcomes. 2012;5:487–93. https://doi.org/10.1161/circoutcomes.111.963694.
Wang X, et al. Tea consumption and the risk of atherosclerotic cardiovascular disease and all-cause mortality: the China-PAR project. Eur J Prev Cardiol. 2020;27:1956–63. https://doi.org/10.1177/2047487319894685.
Wu Z, et al. Longitudinal patterns of blood pressure, Incident Cardiovascular events, and all-cause mortality in Normotensive Diabetic people. Hypertension. 2016;68:71–7. https://doi.org/10.1161/hypertensionaha.116.07381.
Ma C, et al. Low-density lipoprotein cholesterol and risk of intracerebral hemorrhage: a prospective study. Neurology. 2019;93:e445–57. https://doi.org/10.1212/wnl.0000000000007853.
Zhao M, et al. Associations of type 2 diabetes Onset Age with Cardiovascular Disease and Mortality: the Kailuan Study. Diabetes Care. 2021;44:1426–32. https://doi.org/10.2337/dc20-2375.
Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. J Am Coll Cardiol. 2007;50:2173–95. https://doi.org/10.1016/j.jacc.2007.09.011.
Tunstall-Pedoe H, et al. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90:583–612. https://doi.org/10.1161/01.cir.90.1.583.
Stroke–1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO Task Force on Stroke and other Cerebrovascular disorders. Stroke. 1989;20:1407–31. https://doi.org/10.1161/01.str.20.10.1407.
Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(1):62–9. https://doi.org/10.2337/dc10-S062.
James PA, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–20. https://doi.org/10.1001/jama.2013.284427.
Hosmer DW, Lemeshow S. Confidence interval estimation of interaction. Epidemiology. 1992;3:452–6. https://doi.org/10.1097/00001648-199209000-00012.
Kawachi I, Adler NE, Dow WH. Money, schooling, and health: mechanisms and causal evidence. Ann N Y Acad Sci. 2010;1186:56–68. https://doi.org/10.1111/j.1749-6632.2009.05340.x.
Mosquera PA, et al. Income-related inequalities in cardiovascular disease from mid-life to old age in a Northern Swedish cohort: a decomposition analysis. Soc Sci Med. 2016;149:135–44. https://doi.org/10.1016/j.socscimed.2015.12.017.
Meneton P, et al. Unemployment is associated with high cardiovascular event rate and increased all-cause mortality in middle-aged socially privileged individuals. Int Arch Occup Environ Health. 2015;88:707–16. https://doi.org/10.1007/s00420-014-0997-7.
Diez Roux AV, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106. https://doi.org/10.1056/NEJM200107123450205.
Qiu S, et al. Solid fuel use, socioeconomic indicators and risk of cardiovascular diseases and all-cause mortality: a prospective cohort study in a rural area of Sichuan, China. Int J Epidemiol. 2022;51:501–13. https://doi.org/10.1093/ije/dyab191.
Miller V, et al. Fruit, vegetable, and legume intake, and cardiovascular disease and deaths in 18 countries (PURE): a prospective cohort study. Lancet. 2017;3:2037–49. https://doi.org/10.1016/S0140-6736(17)32253-5.
Kim S, Symons M, Popkin BM. Contrasting socioeconomic profiles related to healthier lifestyles in China and the United States. Am J Epidemiol. 2004;159:184–91. https://doi.org/10.1093/aje/kwh006.
Allen L, et al. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Glob Health. 2017;5:e277–89. https://doi.org/10.1016/S2214-109X(17)30058-X.
Eguchi E, Iso H, Honjo K, Yatsuya H, Tamakoshi A. No modifying effect of education level on the association between lifestyle behaviors and cardiovascular mortality: the Japan Collaborative Cohort Study. Sci Rep. 2017;7:39820. https://doi.org/10.1038/srep39820.
Acknowledgements
We appreciate those who were involved in the Kailuan study.
Funding
This research received no specific grants from the public, commercial, or not-for-profit funding agencies.
Author information
Authors and Affiliations
Contributions
JZ and QC carried out the studies, participated in collecting data, and drafted the manuscript. WZ and SC performed the statistical analysis and participated in its design. SW and SD helped to draft the manuscript and performed the data analysis. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study adhered to the guidelines of the Declaration of Helsinki [14] and was approved by the ethics committee of the Kailuan General Hospital (No.2006-05). Each participant signed informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhong, J., Cai, Q., Zheng, W. et al. Association of socioeconomic status and life’s essential 8 with cardiovascular diseases and all-cause mortality in north China: Kailuan study. BMC Public Health 24, 2709 (2024). https://doi.org/10.1186/s12889-024-20205-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-20205-5