Abstract
Introduction
Early screening and identification are crucial for fall prevention, and developing a new method to predict fall risk in the elderly can address the current lack of objectivity in assessment tools.
Methods
A total of 132 elderly individuals over 80 years old residing in some nursing homes in Shanghai were selected using a convenient sampling method. Fall history information was collected, and gait data during a 10-meter walk were recorded. Logistic regression was employed to establish the prediction model, and a nomogram was used to assess the importance of the indicators. The Bootstrap method was utilized for internal validation of the model, while the verification set was used for external validation. The predictive performance of the model was evaluated using the area under the ROC curve, calibration curve, and decision curve analysis (DCA) to assess clinical benefits.
Results
The incidence of falls in the sample population was 36.4%. The Tinetti Gait and Balance Test (TGBT) score (OR = 0.832, 95% CI: 0.734,0.944), stride length (OR = 0.007, 95% CI: 0.000,0.104), difference in standing time (OR = 0.001, 95% CI: 0.000,0.742), and mean stride time (OR = 0.992, 95% CI:0.984,1.000) were identified as significant factors. The area under the ROC curve was 0.878 (95% CI: 0.805, 0.952), with a sensitivity of 0.935 and specificity of 0.726. The Brier score was 0.135, and the Hosmer-Lemeshow test (χ2 = 10.650, P = 0.222) indicated a good fit and calibration of the model.
Conclusion
The TGBT score, stride length, difference in standing time, and stride time are all protective factors associated with fall risk among the elderly. The developed risk prediction model demonstrates good discrimination and calibration, providing valuable insights for early screening and intervention in fall risk among older adults.
Similar content being viewed by others
Introduction
Fall is defined as an accident where subjects come into contact with the ground, floor, or a lower level [1], posing a significant threat to life and health of the aged. The primary injuries resulting from falls include brain contusions, dural hematomas, joint dislocations, and tears [2, 3]. Additionally, 5-10% of falls result in major injuries such as fractures or traumatic brain injuries. Falls among the elderly have become a global public health issue, with over one-third of elderly individuals experiencing falls annually worldwide [4]. In China, the incidence of falls among individuals over 80 years old is as high as 27.3%, with 22.49% of them requiring hospitalization for further treatment and 0.92% succumbing to their injuries, placing a substantial burden on families and society [5, 6].
As individuals aging, there are changes in muscle function, balance ability, proprioception, and vestibular stability of the lower limbs [7]. The walking mobility decreases with age, consequently increasing the risk of falling. To predict fall risk, scholars have developed various assessment scales, including the Morse Fall Risk Assessment Scale (MFS), the Berg Balance Scale, the Fall Risk Assessment Scale for the Elderly, and other subjective or semi-subjective rating tools [8, 9]. Gait impairment has been identified as a significant risk factor for falls [10]. Gait analysis can be used to predict the likelihood of falls [11], and examining gait from the perspective of kinematics provides a quantitative and objective assessment of fall risk factors [12, 13].
Current research on gait assessment employs semi-quantitative methods, such as the Tinetti Gait and Balance Test (TGBT) and the Timed Up and Go test (TUG), as well as quantitative parameters, such as 3 m walking speed. The assessment tools mentioned above possess a certain degree of reliability and validity, but they do have some limitations. On the one hand, its results are greatly influenced by the subjective factors of the researcher, and on the other hand, the simple quantitative parameters are difficult to comprehensively and accurately reflect the dynamic walking status of the subjects and are not sensitive enough for the elderly. Studies have also demonstrated that action mode adopted when walking could influence fall incidents in the elderly [14], and meta-analyses have indicated that interventions targeting gait characteristics can reduce fall rates [15]. Studies utilizing three-dimensional motion capture systems have revealed that as walking speed increases, gait variability in the sagittal and horizontal planes of the lower limbs in the elderly also increases, leading to decreased stability [16]. Analysis using the Ariel performance analysis system (APAS)sports video analysis system has demonstrated that the moving speed of the hip joint across the leg and the acceleration of the ankle joint of the swinging leg are significantly reduced during obstacle crossing, thereby elevating the risk of falling [17].
The onset of falls is typically sudden, and these age-related declines in musculoskeletal and neuromuscular function are not always detectable through clinical assessments due to their subclinical nature and the limitations of assessment tools [18]. Identifying individuals at higher risk of falling before an injurious fall occurs is critical to fall prevention, particularly in seemingly asymptomatic populations such as older adults living in the community or nursing homes. Previous studies have primarily diagnosed falls in problematic populations, such as postoperative, hospitalized, and demented older adults. However, predicting falls is crucial at every stage of the ‘no fall - fall - fall prognosis’ process. Early detection and intervention before a fall occurs can significantly reduce the incidence of falls, improve life safety, and even lower mortality.
According to the literature review, Early screening and identification are crucial for fall prevention, and developing a new method to predict fall risk in the elderly can address the current lack of objectivity in assessment tools. Previous studies have effectively evaluated fall risk in the elderly by assessing their static and dynamic balance abilities and muscle strength. However, relying solely on these indicators may not accurately reflect the actual condition of the elderly [14]. The gait instability during walking has more reference significance [19], and abnormal gait patterns, such as stride variability [20], pace [21], and gait [22], have been shown to be indicative of fall risk. In order to further study the effects of gait changes, we hope to quantitatively characterize the gait features by means of more accurate instrumentation, which relies on the extraction of temporal and spatial gait parameters in the walking cycle, including step length, step length, step frequency, step speed, etc. and quantitatively analyzes the cadence, temporal phase, asymmetry, variability, posture, etc., in the gait features, based on the characteristics reflected by the various parameters. This may require a new type of objective assessment tool.
Consequently,, it is crucial to establish a specific fall prediction model based on daily walking activities to identify elderly individuals at high risk of falling and implement appropriate preventative treatment strategies. This study collects gait data and fall history information from the elderly population and employs the Logistic regression method to develop a risk prediction model, thereby facilitating early identification and prevention of falls among the elderly.
Research objects and methods
Subject recruitment
A total of 132 elderly individuals aged over 80 years were recruited from Shanghai Yinkang Nursing Home, Shanghai Xinqiao Service Center for the Aged, and Zhongfuhui Nursing Home in Qingpu District of Shanghai. This study was conducted in August 2023 for completion. The recruitment process involved administering the Montreal Cognitive Assessment Test (MOCA), Activity of Daily Living Scale (ADL), ACSM’s Guidelines for Exercise Testing and Prescription, and collecting basic information. The participants were randomly divided into a modeling group and a verification group in a 7:3 ratio. The modeling group consisted of 93 individuals (31 falls), while the verification group included 39 individuals (17 falls). There was no significant difference in the incidence of falls between the modeling and verification groups (χ2 = 1.249, P > 0.05). All participants provided informed consent.
Inclusion criteria
-
1
Age ≥ 80 years old and in good health;
-
2
Normal cognitive function and ability for daily living (ADL scale score < 26);
-
3
No contraindication to exercise based on ACSM’s Guidelines for Exercise Testing and Prescription, no regular physical exercise, and capable of completing walking activities under exercise monitoring;
-
4
No bad habits such as drinking or smoking excessively, and no major organic diseases;
-
5
Normal binocular vision or corrected vision, conscious, able to communicate, and understand experimenters’ instructions;
-
6
Signed informed consent form.
Exclusion criteria
-
1
Severe cardiovascular diseases;
-
2
Severe myopathy, lumbar dysfunction or injury, severe osteoporosis, or other diseases unsuitable for prolonged standing;
-
3
Undergoing invasive treatment within the past 6 weeks or planned for such treatment within the next 10 weeks;
-
4
Severe cognitive impairment, mental illness or other neurodegenerative diseases;
-
5
Long-term or recent use of psychotropic drugs, drugs affecting physical activity, cholinesterase inhibitors, or other relevant medications.
Test Flow
The tests were conducted at Shanghai Yinkang Nursing Home, Shanghai Xinqiao Service Center for the Aged, and Zhongfuhui Nursing Home in Qingpu District, Shanghai. During the testing period, the subjects remained indoors within the nursing homes and received care from professional caregivers. The tests, including questionnaire surveys, gait information collection, and lower limb muscle strength evaluation, were conducted between 2:00 pm and 5:00 pm. Refer to Fig. 1 for the detailed test flow.
Questionnaire survey
-
1
ACSM’s Guidelines for Exercise Testing and Prescription: The ACSM questionnaire encompasses 9 medical histories such as one-time heart attack and heart surgery, 9 symptoms including chest discomfort during exertion, dyspnea with unknown reasons, and 7 other health problems such as diabetes, asthma, or other lung diseases. This tool, jointly developed by the American College of Sports Medicine and the American Heart Association, serves to assess individuals’ disease or health risks before undergoing exercise tests [23].
-
2
Montreal Cognitive Assessment (MoCA): MoCA encompasses eight specific cognitive function evaluations, yielding a total score of 30 points. A higher score indicates superior overall cognitive function. The scale exhibits a sensitivity and specificity of 92.4% and 88.4%, respectively, in evaluating the overall cognitive function of the elderly, with a Cronbach’s α coefficient of 0.933 [24].
-
3
Activities of Daily Living Scale (ADL): ADL evaluates the tester’s daily living abilities and comprises 14 items categorized into 2 dimensions (IADL and BADL). Scores range from 1 to 4, with higher scores indicating greater difficulty in mobility for the elderly. A higher total score reflects worse daily living abilities among the elderly. The α coefficients for the 14 items in the questionnaire are 0.93, IADL (8 items) exhibit a Cronbach’s α of 0.94, and BADL (6 items) demonstrate a Cronbach’s α of 0.85. All scale and subscale items exhibit α coefficients exceeding 0.80, indicating robust internal consistency [25].
-
4
International Physical Activity Questionnaire-Chinese Version (IPAQ): This questionnaire investigates the physical activities of elderly individuals in nursing homes over the past week, encompassing daily work and life, transportation, physical exercise, and leisure activities. By assigning intensity levels to physical activities, the data analysis and guidelines categorize physical activity intensity into low, medium, and high levels. Higher scores indicate higher physical activity levels. IPAQ is an internationally accepted and effective adult physical activity level measurement questionnaire, exhibiting a Cronbach’s α of 0.90 [26].
-
5
The Tinetti Gait and Balance Test (TGBT): TGBT primarily predicts the fall risk of the elderly by evaluating their balance ability and gait. The scale comprises 16 tests, including sitting balance, standing balance, and standing with eyes closed, of which 9 are balance tests with a maximum score of 16, and 7 are gait tests with a maximum score of 12. The internal consistency Cronbach’s α of the Tinetti total scale is 0.887, while the balance and gait tests exhibit Cronbach’s α coefficients of 0.872 and 0.718, respectively [13].
Testing
-
1
Evaluation of Lower Limb Muscle Strength: Five Times Sit to Stand Test (FTST). The subjects were instructed to perform five consecutive sit-to-stand movements, and the time taken to complete the action was recorded by the researchers. The test was conducted three times, and the average of the three tests was considered the final score. During the test, the subjects sat on a chair with a height of approximately 42 cm, crossed their hands on the abdomen, maintained an upright posture with the abdomen tucked in and the back close to the chair, and positioned their feet shoulder-width apart. The subjects were required to fully straighten their knees when standing up.
-
2
Gait Feature Collection: The gait analysis was conducted using the whole-body motion capture and three-dimensional gait analysis system provided by Shanghai Nuocheng Electric Co., Ltd. The research subjects wore wearable devices equipped with motion sensors, which transmitted gait information to a computer for analysis. During the test, the subjects were instructed to maintain their normal walking speed and posture for a 10-meter walking test. Data collection started after the second step, and it was completed before the subjects stopped walking, minimizing data errors caused by acceleration during the start and stop phases. Gait test data included total steps, stride uniformity, left-right uniformity, stride time, standing time, swinging time, stride length, stride frequency, stride speed, and stride width. Two researchers were involved in the process, with one responsible for timing records and the other ensuring the safety of the elderly subjects by following them from the right rear side.
Collection and assessment of information on falls
During the baseline falls history survey, falls were evaluated through face-to-face interviews. The test subjects were interviewed about any falls they experienced in the past year, and the patients underwent detailed standardized interviews. Each subject was contacted by a trained interviewer or caregiver. The survey aimed to record falls, including the location and impact on the subjects’ health and healthcare system. It also collected data on soft tissue injuries, fractures, and head trauma, as well as patients’ use of general practitioners and emergency services, and the need for further surgery or hospitalization after a fall. For this study, a history of falls was defined as experiencing at least one fall within the past year during the baseline survey. Additionally, at least one fall within the past year was used as a regression outcome in the follow-up survey.
Statistical methods
SPSS 24.0 software was used for random grouping, and data distribution was assessed using frequency histograms. Normally distributed or approximately normally distributed measurement data were described using mean and standard deviation (x ± SD), and the independent sample t-tests were used for group comparisons. Measurement data with a significantly skewed distribution were described using median (Interquartile Range) [M (P25, P75)], and Mann-Whitney U nonparametric tests were used for group comparisons. Counting data were presented as n (%) and compared between groups using the χ2 test.
Data analysis was performed using R 4.2.1 software. This study utilizes the gait asymmetry index for calculations, defined by the formula: (left foot swing phase duration - right foot swing phase duration) / (left foot swing phase duration + right foot swing phase duration). All data were standardised prior to regression analysis. The severity of multicollinearity in the model was quantified using the eigenroot value method. Variables with maximum variance explained ratios greater than 40% and any variables with root eigenvalues less than 0.01 were excluded. We also used gender, height, and weight as control variables. Binary logistic stepwise regression analysis was used to establish prediction models, and nomograms were created. Internal model validation was conducted using bootstrap resampling (1000 times), while the validation group data were used for external validation. The discrimination and consistency of the model were assessed using Receiver Operating Characteristic (ROC) curves and calibration curves. Model calibration was evaluated using the calibration curve and Brier score (less than 0.25 indicates appropriate calibration). The goodness of fit of the model was tested using the Hosmer-Lemeshow test, with P > 0.05 indicating a good fit, and Decision Curve Analysis (DCA) was performed to evaluate the clinical benefit.
Results
Baseline characteristics
The subjects were randomly grouped into three groups. Among them, 48 (36.4%) had a history of falling, with 31 (33.3%) in the modeling group and 17 (43.6%) in the verification group. After random grouping, there were no significant differences in all indexes between the two groups (P > 0.05) (Table 1).
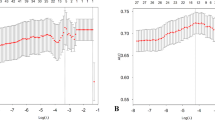
Evaluation of test efficiency of the elderly fall risk prediction model
In the modeling group, the area under the ROC curve was 0.878 (95% CI: 0.805, 0.952), with a Youden index of 0.661, sensitivity of 0.935, and specificity of 0.726, indicating high discrimination of the model. In the validation group, the area under the ROC curve was 0.845 (95% CI: 0.707, 0.983), with a Youden index of 0.661, sensitivity of 0.706, and specificity of 0.955, indicating high discrimination of the validation model (Fig. 2).
Internal verification using the bootstrap method with 1000 resamples in the modeling group showed that the predicted fall risk by the model was consistent with the actual situation, with a Brier score of 0.135. External verification using 39 cases in the validation group demonstrated good calibration of the model in predicting fall risk, and the predicted risks are in good agreement with the actual situation. with a Brier score of 0.148. The Hosmer-Lemeshow test revealed a good fit of the prediction model, with P-values of 0.222 in the modeling group (χ2 = 10.650), and 0.398 in the validation group (χ2 = 8.371) (Fig. 3).
Binary logistic regression analysis of elderly falls
An exploratory factor analysis based on gender, height and weight, and gait characteristics of older adults was performed using the root eigenvalue test. The variance explained by the first factor was 26.858%, which was less than the critical value of 40%, while the root eigenvalue of the smallest factor component was > 0.01, so the effect of multicollinearity was within acceptable limits. Binary logistic analyses were conducted using the history of falls in the past year (July 2022 to July 2023) of older adults as the dependent variable, categorizing the occurrence of falls into “yes” and “no” responses, and gait data as the independent variable. The results demonstrate that TGBT (OR = 0.832), Stride Length (OR = 0.007), Standing Time Difference (OR = 0.001), and Stride Time Mean (OR = 0.992) have a negative impact on the likelihood of falls. Specifically, an increase of one unit in these variables corresponds to a reduction in fall risk by factors of 0.832, 0.007, 0.001, and 0.992, respectively. The results indicated that TGBT (score), stride length (m), and standing time difference are protective factors that significantly reduce fall risk among the elderly. (Table 2).
Construction of the elderly fall risk prediction model
Based on the logistic regression model: log(1 − P(Y = 1)/P(Y = 1)) = 12.334 − 0.184*TGBT-4.932* stride length(m)-7.056* standing time difference (ms) -0.008* stride length time mean (ms), a nomogram for predicting falls in the elderly was developed using the above protective factors (Fig. 4). Each predictor is projected upwards to an exact point and the sum of all points in the nomogram model is transformed and converted into an individual’s risk of falling, further determining the patient’s level of fall risk.
Clinical benefit analysis of the elderly fall risk prediction model
The results indicated that the model provided high clinical benefit for elderly individuals at risk of falling when the threshold was set at a large range (modeling group: 18% ~ 92%; verification group: 0% ~ 80%). This suggests significant clinical significance of the model (Fig. 5).
Discussion
This study provides evidence that gait data is a superior predictor of fall risk compared to the scale, which is consistent with previous research findings [12, 27, 28]. Falls in the elderly are typically caused by multiple factors, and subtle changes in gait can significantly increase the risk of falling. However, the subjective evaluation of movement and balance provided by the Tinetti scale fails to capture these gait changes and lacks objective data support [29, 30].
Our research highlights the importance of stride length and stride time in predicting falls among the elderly. Smaller strides and shorter stride times are associated with a higher risk of falling [31,32,33]. Research has demonstrated that advancing age is associated with a decline in the regulatory capacity of both the central and peripheral nervous systems [34, 35], asymmetric input of proprioception information [36, 37], reduced muscle strength, osteoporosis, and unstable gait, all of which collectively contribute to alterations in stride length and stride time among the elderly [32, 38,39,40,41]. This research suggests that targeting joint force, moment, and muscle activation patterns as specific intervention goals may help modify gait and reduce the risk of falling. Previous studies have also shown that the fall group exhibits higher stride variation coefficients compared to the control group [37, 42]. Additionally, individuals at high risk of falling demonstrate increased variability in stride-trunk during daily walking, leading to a higher fall rate [12, 31]. Fallers also exhibit greater time variability in step size compared to non-fallers [43]. These findings highlight the importance of monitoring stride and stride time for medical staff or guardians in daily life, as decreases in these parameters may indicate early signs of falling.
Furthermore, our study reveals that a smaller asymmetry index of standing time is associated with a higher risk of falling. Specifically, a shorter standing time of the left foot is correlated with an increased risk of falling. This observation may be attributed to the prevalence of right-handedness in the middle-aged and elderly population. As muscle strength decreases with age, it may affect dominant lower limb standing phase and the stability of standing posture [30]. Throughout the walking cycle, the stance phase accounted for an average of 63% of the entire gait cycle, while the two double-limbed weight-bearing phases combined accounted for 26% of the full cycle. During the stance phase, the ground-following phase was shortened mainly due to the decreased regressive contractility of the tibialis anterior muscle. Additionally, the function of the calf triceps and platysma muscles declined, resulting in a significant lengthening of the mid-stance phase and a shortening of the acceleration phase. Due to aging, the lower limb muscles experience functional decline, resulting in shorter step length, lower foot lift, and poor joint stability, leading to imbalance issues in the elderly while walking [44]. There is also an effect of the overall steering strategy between the head and trunk, as well as between the head and pelvis, when controlling balance [45, 46].
Moreover, Motor performance, including balance and gait, is a complex process that requires the integration of sensory-motor and cognitive systems. Short standing times also involve cognitive processes, as individuals need to make quick and accurate decisions using executive function when encountering uneven ground, obstacles, or stairs [27]. In older adults, slowed cognitive processing can lead to compensation for damage to the sensorimotor system and impaired motor planning. Responses to maintaining balance in challenging environments may be associated with an increased risk of falls [47]. Research has demonstrated a strong correlation between impaired cognitive function and fall risk assessment, specifically the 10-meter walk test (10-MWT), which includes temporal orientation, attention/concentration, and verbal/visuospatial structure [48]. This association may also explain why individuals with dementia are at a higher risk for falls. However, it is important to note that the test population in this experiment was exclusively comprised of individuals over the age of 80. As cognitive decline is known to occur with increasing age, it is crucial to emphasize the potential effects of falls resulting from cognitive decline. Impaired cognitive function is strongly associated with decreased ability to make decisions, solve problems, and perform motor tasks, all of which may increase asymmetry index of standing time.
Finally, while the cost of implementing our model may be slightly higher than that of traditional clinical assessments, the use of wearable sensors can provide more objective and accurate data for fall risk prediction [49]. The collection of objective data is facilitated by the use of wearable devices. During our testing process, we were able to calibrate the sensor system and provide a prediction report in just 5 to 10 min. During gait analysis, it is possible to provide more objective data instead of relying solely on walking speed to assess falls. Furthermore, wearable exercise systems have the potential to be utilized in clinical practice and research due to their portability and user-friendliness.
It is important to acknowledge the limitations of this study. This study aims to construct a predictive model for assessing the fall risk among the elderly based on gait analysis and evaluate the effectiveness of the model in predicting fall risk. However, the results are limited and may require validation in other age groups in future studies. The study included elderly nursing home residents, a unique population that may pose challenges to generalizing the findings. The use of fall history as the predicted variable and gait data as the predictor variable creates the inconsistency over time, as falls occur before the development of the gait analysis-based prediction model. Future research should consider conducting cohort studies to further validate the association between gait parameters and fall risk, thereby improving the efficiency of fall risk prediction.
Conclusion
Gait serves as a sensitive indicator for predicting falls, as even subtle changes in the constituent systems that contribute to gait decline can reveal increased instability. The predictive model developed in this study plays a crucial role in assessing fall risk among the elderly. The TGBT score, stride length, difference in standing time, and stride time all emerge as protective factors for preventing falls among the elderly. This model not only identifies, prevents, and manages the elderly at risk of falling but also assists clinical medical staff in making timely clinical decisions and formulating necessary preventive measures for high-risk fallers.
Data availability
No datasets were generated or analysed during the current study.
References
Buchner DM, Hornbrook MC, Kutner NG, Tinetti ME, Ory MG, Mulrow CD et al. Development of the common data base for the FICSIT trials. J Am Geriatr Soc. 1993;41(3):297–308. Epub 1993/03/01. https://doi.org/10.1111/j.1532-5415.1993.tb06708.x. PubMed PMID: 8440854.
Lu ZM, Wang Y, Ye PP, Er YL, Duan LL. [Analysis on epidemiologic characteristics of fall in old people: results from Chinese National Injury Surveillance System, 2015–2018]. Zhonghua Liu Xing Bing Xue Za Zhi. 2021;42(1):137–41. https://doi.org/10.3760/cma.j.cn112338-20200424-00646. Epub 2021/01/28.
Ribeiro AP, Souza ERd, Atie S, Souza ACd, Schilithz AO. Ciênc saúde coletiva. 2008;13(4):1265–73. https://doi.org/10.1590/s1413-81232008000400023. PubMed PMID: SCIELO:S. A influência das quedas na qualidade de vida de idosos.
Sherrington C, Fairhall N, Kwok W, Wallbank G, Tiedemann A, Michaleff ZA, et al. Evidence on physical activity and falls prevention for people aged 65 + years: systematic review to inform the WHO guidelines on physical activity and sedentary behaviour. Int J Behav Nutr Phys Act. 2020;17(1):144. https://doi.org/10.1186/s12966-020-01041-3. Epub 2020/11/27.
Jiang J, Long J, Ling W, Huang G, Guo X, Su L. Incidence of fall-related injury among old people in mainland China. Arch Gerontol Geriatr. 2015;61(2):131–9. https://doi.org/10.1016/j.archger.2015.06.003. Epub 2015/06/25.
Cangning Y, Haijun Y, Xiaomin L, Yue Z, Gong C. Meta-analysis of the incidence rate of falls among elderly people in China. Chin J Evidence-Based Med. 2022;22(10):1142–8.
Yogev-Seligmann G, Hausdorff JM, Giladi N. The role of executive function and attention in gait. Mov Disord. 2008;23(3):329–42. https://doi.org/10.1002/mds.21720. quiz 472. Epub 2007/12/07.
Lima CA, Ricci NA, Nogueira EC, Perracini MR. The Berg Balance Scale as a clinical screening tool to predict fall risk in older adults: a systematic review. Physiotherapy. 2018;104(4):383–94. https://doi.org/10.1016/j.physio.2018.02.002. Epub 2018/06/28.
Anson E, Thompson E, Ma L, Jeka J. Reliability and fall risk detection for the BESTest and Mini-BESTest in older adults. J Geriatr Phys Ther. 2019;42(2):81–5. https://doi.org/10.1519/JPT.0000000000000123. Epub 2017/04/28.
Callisaya ML, Blizzard L, McGinley JL, Srikanth VK. Risk of falls in older people during fast-walking–the TASCOG study. Gait Posture. 2012;36(3):510–5. https://doi.org/10.1016/j.gaitpost.2012.05.003. Epub 2012/06/12.
Rietdyk S, Rhea CK. The effect of the visual characteristics of obstacles on risk of tripping and gait parameters during locomotion. Ophthalmic Physiol Opt. 2011;31(3):302–10. https://doi.org/10.1111/j.1475-1313.2011.00837.x. PubMed PMID: WOS:000289253800012.
Geerse DJ, Roerdink M, Marinus J, van Hilten JJ. Walking adaptability for targeted fall-risk assessments. Gait Posture. 2019;70:203–10. https://pubmed.ncbi.nlm.nih.gov/30901621/. Pubmed PMID: 30901621.
Canbek J, Fulk G, Nof L, Echternach J. Test-retest reliability and construct validity of the Tinetti performance-oriented mobility Assessment in People with Stroke. J Neurol Phys Ther. 2013;37(1):14–9. https://doi.org/10.1097/NPT.0b013e318283ffcc. PubMed PMID: WOS:000316217200004.
Bowen ME, Cacchione P. Changes in Motor Behavior Predict Falls and identify acute events. West J Nurs Res. 2022;44(12):1100–7. https://doi.org/10.1177/01939459211031981. PubMed PMID: WOS:000677104100001.
Okubo Y, Schoene D, Lord SR. Step training improves reaction time, gait and balance and reduces falls in older people: a systematic review and meta-analysis. Br J Sports Med. 2017;51(7):586–93. https://doi.org/10.1136/bjsports-2015-095452. Epub 2016/01/10.
Liu M, Li YR, Ma XW, Wang J, Wang T. SMART DX three-dimensional analysis of Gait variability in Elderly: gender, Gait Speed, and Lower Limb Dominance. J Tianjin Univ Sport. 2023;38(02):215–20. https://doi.org/10.13297/j.cnki.issn1005-0000.2023.02.014. DOI: CNKI:SUN:SPAN.0.2018-06-006.
Meng ZL, Zhang QL, Liu CY. Kinematic Characteristics Analysis of Gait Crossing Obstacles in Elderly with different fall risks in the community. Chin J Rehabilitation Theory Pract. 2020;26(01):110–4. DOI:CNKI:CDMD:2.1018.007559.
Bhatt T, Espy D, Yang F, Pai YC. Dynamic gait stability, clinical correlates, and prognosis of falls among community-dwelling older adults. Arch Phys Med Rehabil. 2011;92(5):799–805. PubMed PMID: 21530728.
Wang L, Yu WH. Progress in the application of Gait Analysis in Falls of the Elderly. Chin J Nurs. 2016;51(03):347–51. https://doi.org/10.3761/j.issn.0254-1769.2016.03.019
Middleton A, Fulk GD, Herter TM, Beets MW, Donley J, Fritz SL. Self-selected and maximal walking speeds provide Greater Insight into fall Status Than walking Speed Reserve among Community-Dwelling older adults. Am J Phys Med Rehabil. 2016;95(7):475–82. https://doi.org/10.1097/phm.0000000000000488. PubMed PMID: WOS:000378158400007.
Lipsitz LA, Manor B, Habtemariam D, Iloputaife I, Zhou J, Travison TG. The pace and prognosis of peripheral sensory loss in advanced age: association with gait speed and falls. BMC Geriatr. 2018;18. https://doi.org/10.1186/s12877-018-0970-5. 11PubMed PMID: WOS:000450259000002.
Hollman JH, McDade EM, Petersen RC. Normative spatiotemporal gait parameters in older adults. Gait Posture. 2011;34(1):111–8. https://doi.org/10.1016/j.gaitpost.2011.03.024. Epub 2011/05/03.
Riebe D, Franklin BA, Thompson PD, Garber CE, Whitfield GP, Magal M, et al. Updating ACSM’s recommendations for Exercise Preparticipation Health Screening. Med Sci Sports Exerc. 2015;47(11):2473–9. https://doi.org/10.1249/mss.0000000000000664. PubMed PMID: WOS:000362940900028.
Dalrymple-Alford JC, MacAskill MR, Nakas CT, Livingston L, Graham C, Crucian GP, et al. The MoCA Well-suited screen for cognitive impairment in Parkinson disease. Neurology. 2010;75(19):1717–25. https://doi.org/10.1212/WNL.0b013e3181fc29c9. PubMed PMID: WOS:000284473000012.
Book S, Luttenberger K, Stemmler M, Meyer S, Graessel E. The Erlangen test of activities of daily living in persons with mild dementia or mild cognitive impairment (ETAM) - an extended validation. BMC Psychiatry. 2018;18. https://doi.org/10.1186/s12888-018-1886-5. PubMed PMID: WOS:000445437900004.
Macfarlane D, Chan A, Cerin E. Examining the validity and reliability of the Chinese version of the International Physical Activity Questionnaire, long form (IPAQ-LC). Public Health Nutr. 2011;14(3):443–50. PubMed PMID: WOS:000288050600009.
Amboni M, Barone P, Hausdorff JM. Cognitive contributions to gait and falls: evidence and implications. Mov Disord. 2013;28(11):1520–33. Epub 2013/10/18. doi: 10.1002/mds.25674. PubMed PMID: 24132840; PubMed Central PMCID: PMCPMC4119872.
Knobe M, Giesen M, Plate S, Gradl-Dietsch G, Buecking B, Eschbach D, et al. The Aachen mobility and Balance Index to measure physiological falls risk: a comparison with the Tinetti POMA scale. Eur J Trauma Emerg Surg. 2016;42(5):537–45. PubMed PMID: WOS:000385176400002.
Bongers KT, Schoon Y, Graauwmans MJ, Schers HJ, Melis RJ, Olde Rikkert MG. The predictive value of gait speed and maximum step length for falling in community-dwelling older persons. Age Ageing. 2015;44(2):294–9. https://doi.org/10.1093/ageing/afu151. Epub 2014/10/18.
Bruijn SM, Meijer OG, Beek PJ, van Dieen JH. Assessing the stability of human locomotion: a review of current measures. J Royal Soc Interface. 2013;10(83). https://doi.org/10.1098/rsif.2012.0999. PubMed PMID: WOS:000318009300001.
Weiss A, Brozgol M, Dorfman M, Herman T, Shema S, Giladi N, et al. Does the evaluation of gait quality during daily life provide insight into fall risk? A novel approach using 3-day accelerometer recordings. Neurorehabil Neural Repair. 2013;27(8):742–52. Epub 2013/06/19. doi: 10.1177/1545968313491004. PubMed PMID: 23774124.
Creaby MW, Cole MH. Gait characteristics and falls in Parkinson’s disease: a systematic review and meta-analysis. Parkinsonism Relat Disord. 2018;57:1–8. https://doi.org/10.1016/j.parkreldis.2018.07.008. Epub 2018/07/26.
Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050–6. https://doi.org/10.1053/apmr.2001.24893. Epub 2001/08/09.
Peel NM, Kuys SS, Klein K. Gait Speed as a measure in Geriatric Assessment in Clinical settings: a systematic review. Journals Gerontology: Ser A. 2013;68(1):39–46. https://doi.org/10.1093/gerona/gls174
Taylor ME, Delbaere K, Lord SR, Mikolaizak AS, Brodaty H, Close JCT. Neuropsychological, physical, and functional mobility measures Associated with Falls in cognitively impaired older adults. Journals Gerontol Ser aBiological Sci Med Sci. 2014;69(8):987–95. https://doi.org/10.1093/gerona/glt166. PubMed PMID: WOS:000339668700009.
Espy DD, Yang F, Bhatt T, Pai YC. Independent influence of gait speed and step length on stability and fall risk. Gait 12 Posture. 2010;32(3):378–82. PubMed PMID: WOS:000283459100019.
Barbara RCS, Freitas SMSF, Bagesteiro LB, Perracini MR, Alouche SR. Gait characteristics of younger-old and older-old adults walking overground and on a compliant surface. Revista Brasileira De Fisioterapia. 2012;16(5):375–80. https://doi.org/10.1590/s1413-35552012005000039. PubMed PMID: WOS:000310326500005.
Franz JR. The Age-Associated reduction in Propulsive Power Generation in walking. Exerc Sport Sci Rev. 2016;44(4):129–36. https://doi.org/10.1249/jes.0000000000000086. PubMed PMID: WOS:000384449300002.
Callisaya ML, Blizzard L, McGinley JL, Schmidt MD, Srikanth VK. Sensorimotor factors affecting gait variability in older People-A Population-based study. Journals of Gerontology Series a-Biological sciences and Medical sciences. 2010;65(4):386–92. https://doi.org/10.1093/gerona/glp184. PubMed PMID: WOS:000276042200008.
Kobayashi Y, Hobara H, Heldoorn TA, Kouchi M, Mochimaru M. Age-independent and age-dependent sex differences in gait pattern determined by principal component analysis. Gait Posture. 2016;46:11–7. https://doi.org/10.1016/j.gaitpost.2016.01.021. PubMed PMID: WOS:000375468200003.
Marques EA, Mota J, Carvalho J. Exercise effects on bone mineral density in older adults: a meta-analysis of randomized controlled trials. Age. 2012;34(6):1493–515. https://doi.org/10.1007/s11357-011-9311-8. PubMed PMID: WOS:000310536200014.
Chan WC, Au-Yeung SSY. Recovery in the severely impaired arm Post-stroke after Mirror Therapy: a randomized controlled study. Am J Phys Med Rehabil. 2018;97(8):572–7. https://doi.org/10.1097/phm.0000000000000919. Epub 2018/03/10.
Callisaya ML, Blizzard L, Schmidt MD, Martin KL, McGinley JL, Sanders LM, et al. Gait, gait variability and the risk of multiple incident falls in older people: a population-based study. Age Ageing. 2011;40(4):481–7. https://doi.org/10.1093/ageing/afr055. Epub 2011/06/02.
Pol F, Forghany S, Hosseini SM, Taheri A, Menz HB. Structural and functional foot and ankle characteristics associated with falls in older people. Gait Posture. 2021;88:78–83. https://doi.org/10.1016/j.gaitpost.2021.05.012. Epub 2021/05/19.
Mahoney JR, Oh-Park M, Ayers E, Verghese J. Quantitative trunk sway and prediction of incident falls in older adults. Gait Posture. 2017;58:183–7. https://doi.org/10.1016/j.gaitpost.2017.07.115. Epub 2017/08/12.
Cocks AJ, Young WR, Ellmers TJ, Jackson RC, Williams AM. Concern about falling is associated with segmental control when turning in older adults. Gait Posture. 2021;88:105–8. https://doi.org/10.1016/j.gaitpost.2021.05.011. Epub 2021/05/24.
Davis JC, Best JR, Khan KM, Dian L, Lord S, Delbaere K, et al. Slow Processing Speed predicts Falls in older adults with a Falls history: 1-Year prospective cohort study. J Am Geriatr Soc. 2017;65(5):916–23. https://doi.org/10.1111/jgs.14830. Epub 2017/04/09.
Jeka JJ, Allison LK, Kiemel T. The dynamics of visual reweighting in healthy and fall-prone older adults. J Mot Behav. 2010;42(4):197–208. PubMed PMID: 20501430.
Pang I, Okubo Y, Sturnieks D, Lord SR, Brodie MA. Detection of Near Falls using Wearable devices: a systematic review. J Geriatr Phys Ther. 2019;42(1):48–56. Epub 2018/02/01. doi: 10.1519/JPT.0000000000000181. PubMed PMID: 29384813.
Acknowledgements
Consent for PublicationNo conflict of interest exits in the submission of this manuscript, and manuscript is approved by all authors for publication.
Funding
Supported by: The work was supported by Shanghai Key Lab of Human Performance (Shanghai University of Sport) (NO. 11DZ2261100). National Social Science Foundation of China (NO.22BTY076).
Author information
Authors and Affiliations
Contributions
The authors have developed the ideas and model described in this article in joint discussions. SJ, YS and XW: conception, design, and revision of the article, these authors contributed equally to this work. SJ has written a first draft of the manuscript that has then been revised (amended, commented, expanded) by YS. and XW. in two extensive rounds of revision. CG, PW, JW and SL: data acquisition and analysis. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Ethics Committee of Shanghai Institute of Physical Education (Approval No. 102772020RT059), and all participants provided informed consent.
Consent for publication
No conflict of interest exits in the submission of this manuscript, and manuscript is approved by all authors for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jia, S., Si, Y., Guo, C. et al. The prediction model of fall risk for the elderly based on gait analysis. BMC Public Health 24, 2206 (2024). https://doi.org/10.1186/s12889-024-19760-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19760-8