Abstract
Background
Despite the intended 50% reduction in anemia in women of reproductive age, this tendency has only worsened. Even though iron deficiency is the most prevalent cause of anemia, anemia and chronic illnesses like HIV are closely associated; in fact, 48.6% of people living with HIV who were 15 years of age or older had anemia. However, the burden of anemia among HIV-positive women in sub-Saharan African (SSA) countries is not well documented. Therefore, the goal of our research was to investigate anemia and the factors that are linked to it in SSA women who had HIV infections.
Methods
A cross-sectional study was conducted using demographic and health survey datasets from 18 SSA countries. A total of 7823 weighted samples were included. STATA version 16 software was used for analysis. A multilevel logistic regression model was fitted. An adjusted odds ratio with a 95% CI and a p-value < 0.05 was used to declare significantly associated factors.
Result
The overall prevalence of anemia was found to be 45.1% [95% CI: 43.97–46.18%]. Of those 5.05%, 37.97%, and 56.97% were severely, moderately, and mildly anemic, respectively. Education level of primary [AOR = 0.74, 95% CI: 0.62, 0.89], secondary [AOR = 0.81, 95% CI: 0.68, 0.98], and higher [AOR = 0.74, 95% CI: 0.55, 0.99], as well as current contraceptive use [AOR = 0.74, 95% CI: 0.63, 0.87] were negatively associated with anemia. While pregnancy [AOR = 1.51, 95% CI: 1.17, 1.94], breast feeding [AOR = 1.38, 95% CI: 1.17, 1.64], health insurance [AOR = 1.50, 95% CI: 1.25, 1.80], and menstruation within six weeks prior to data collection [AOR = 1.36, 95% CI: 1.20, 1.54] had a significant positive relation with anemia among HIV-infected women in SSA countries.
Conclusion
Anemia is a serious public health problem among HIV-infected women in SSA countries. Pregnancy, breast feeding, health insurance, and menstruation within six weeks prior to data collection were significant risk factors. On the other education and current contraceptive use were significant protective factors for anemia among HIV-infected women in SSA countries. Therefore, strategies aimed at early identification of anemia may lead to an improvement in the health of HIV-infected women.
Similar content being viewed by others
Introduction
When red blood cells or the amount of hemoglobin that carries oxygen to the organs and tissues within them are insufficient, it is referred to as anemia [1, 2]. Anemia is defined as having a hemoglobin concentration below 12 g/dl for a reproductive-aged non-pregnant woman and below 11 g/dl for pregnant women at sea level [3]. It is a serious threat to public health, particularly in low- and middle-income nations, and primarily affects women and young children [1, 2, 4,5,6]. It is a serious health issue that can lead to delayed development of the baby’s iron stores, low birth weight, preterm delivery, poor cognitive and motor development in children, and reduced work capacity in adults [1, 2, 6]. In 2019, anemia resulted in the loss of 50 million years of healthy life [1].
Although a 50% decrease in anemia among women of reproductive age was desired up to 2025 by the World Health Assembly (WHA) in 2012 [2], this trend has continued to worsen [7, 8]. The predominant causes of anemia include iron deficiency, which can result from various factors such as poor nutrition, infections (e.g., malaria), heavy menstruation, family history of anemia, and pregnancy [1]. Additionally, chronic conditions such as HIV are significantly associated with the development of anemia [9,10,11]. About 48.6% of HIV-positive people aged 15 and older [5] had anemia.
Anemia raises the probability that HIV infections in women may progress to AIDS, and its treatment reduces the chance of death and improves survival [11,12,13]. It is also associated with a lower quality of life [14, 15]. Similar multifactorial factors associated with non-infected people can also cause anemia in HIV-positive individuals. These include opportunistic infections leading to gastrointestinal blood loss from HIV infection-related complications like lymphoma, Kaposi’s sarcoma, mycobacterium avium, cytomegalovirus, mycobacterium tuberculosis, histoplasmosis, cryptococcus neoformans, and parvovirus B19, which indirectly suppress bone marrow through cytokine-mediated dysregulation of iron incorporation [11, 12]. Gastrointestinal tract lesions can also cause dietary deficits in folate and/or vitamin B12, which can lead to impaired erythropoiesis [11]. Furthermore, bone marrow suppression due to HIV-produced viral proteins [12, 16] or antiretroviral therapy [11, 17], cancer, blood loss, erythropoietin deficiency [12], hemolysis brought on by thrombotic thrombocytopenic purpura or microangiopathy, and disseminated intravascular coagulation [11, 12, 17, 18] can result in anemia.
Previous literature conducted revealed that age [11, 18], educational status [12, 17], marital status [19,20,21,22,23], residence [9, 20,21,22], wealth status [20, 24], residence [8, 9, 21], working status [19], family size [7, 8], source of drinking water [25, 26], latrine facilities [10], presence of health insurance [8], parity [9, 27], pregnancy [26,27,28], breast feeding status [10], current use of contraceptives [26,27,28], type of contraceptives [24, 29], menstruation in the last 6 weeks [7], abortion [30], age at first birth [4], distance to the health facilities [28], and maternal community literacy [8] were significantly associated with anemia among women.
Africa continues to be the region most severely affected by HIV, home to over two-thirds of all HIV-positive individuals globally [31,32,33]. In sub-Saharan Africa (SSA), where over 85% of the global new HIV infections occur among 15–19-year-old females, women would have accounted for 63% of all new HIV infections by 2021 [33]. Hematological issues like anemia are critical to a woman’s survival, given the greater incidence of HIV in this population. The burden of anemia among HIV-positive women in these regions, however, is not well documented.
In order to reduce the effects of anemia on women living with HIV, we need to be aware of the variables that may contribute to the issue. It is crucial to investigate how maternal, economic, structural, and sociodemographic factors interact to induce anemia in women living with HIV. To combat the issue, it is crucial to create context- and area-based interventions. Therefore, the current study used multilevel logistic regression analysis to investigate anemia and its associated factors among HIV-positive women in SSA.
Method and materials
Data sources and setting
Recent standard demographic and health survey datasets from 18 SSA nations, such as Burkina Faso (2021), Cote d’Ivoire (2021), the Democratic Republic of the Congo (2013/14), Ethiopia (2016), Gabon (2019-21), Ghana (2014), Guinea (2018), Lesotho (2104), Malawi (2015/16), Namibia (2013), Niger (2012), Senegal (2010/11), Sierra Leone (2019), South Africa (2016), Togo (2013/14), Tanzania (2022), Zambia (2018), and Zimbabwe (2015), were used as the basis for this study. Every country conducts these nationally representative household surveys every five years, and they yield a wealth of information on various aspects of health and related factors, including population and nutrition. Data was taken from http://www.dhsprogram.com with authorization and in accordance with an official online request. Datasets for a variety of populations, including men, women, children, births, households, and other anthropometric information like HIV and anemia, are available from the DHS [34].
Sampling design
Participants for each survey were typically chosen using a two-stage, stratified cluster sampling method. First, enumeration areas, clusters, or communities were created within each country. Then stratification was accomplished by dividing each cluster into urban and rural regions. In the first stage, the required number of enumeration areas was selected from both urban and rural enumeration areas with a probability proportional to the EA size. Following that, a sample of homes was chosen from the selected rural and urban enumeration areas [34].
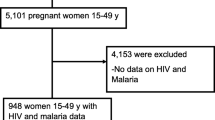
Participants
The individual record (IR) file for women and the AP file for HIV data sets served as the foundation for our investigation. Women aged 15–49 who were measured for anemia in households selected for anemia testing were included. A total of 7823 weighted samples of women with HIV infection diagnoses were included in our investigation.
Variables of the study
Outcome variable
In our investigation, anemia was the dependent variable, which is defined as a hemoglobin level < 11 g/dl for mothers who are nursing or pregnant and < 12 g/dl for women who are not breastfeeding or pregnant after the altitude effect is adjusted [3, 34]. Regarding the cut-offs defining levels of anemia, non-pregnant women (15 and above years of age) have 11–11.9 g/dl “mild,” 8–10.9 “moderate,” and < 8 g/dl < “severe,” while pregnant women have 10–10.9 g/dl “mild,” 7–9.9 g/dl “moderate, and < 7 g/dl “severe.” HIV-positive women who fell below the aforementioned cutoff points were therefore considered anemic [3].
Independent variables
We categorized the explanatory variables of this study into individual and community-level factors. Age, education level, marital status, mother’s occupation, exposure to mass media, wealth index, number of children born, family size, source of drinking water, toilet, health insurance, current state of pregnancy, status of breastfeeding, type of contraception used, menstruation during the previous six weeks, history of pregnancy termination, and distance to health facilities were among the individual-level factors. Community-level characteristics, including place of residence, community-level maternal education, community-level media exposure, and community-level poverty, were evaluated.
Measurements and operational definitions
Household media exposure is defined as “yes” if a woman has been exposed to at least one of these media and “no” if she has not. It is formed by combining participants’ reading of newspapers or magazines, listening to the radio, or watching television.
Community-level media exposure
The percentage of women who have been exposed to at least one media (newspaper, magazine, radio, or television) is known as community-level media exposure. This variable is aggregated from household media exposure and is classified as low (communities with < 50% of women exposed) or high (communities with ≥ 50% of women exposed) based on the median value.
Maternal education at the community level
Aggregate values are determined by taking the percentage of women who have completed at least primary school. This percentage is obtained from information on respondents’ educational backgrounds and is classified as low (communities where less than 50% of women have completed primary school) or high (communities where more than 50% of women have completed primary school).
The measure of poverty at the community level is derived from household wealth status, which is the percentage of women in the lowest and poorest quantiles. The measure is then aggregated and classified into two categories: low, which denotes communities where less than 50% of women live in poverty, and high, which denotes communities where more than 50% of women live in poverty.
Data management and analysis
The HIV dataset and the individual datasets were first combined for each of the eighteen nations. First, we came up with names that sounded similar for these identification variables based on the common case identifiers for each dataset. After sorting these IDs, we applied the relevant command. The specifics are provided elsewhere [35]. Individual datasets from these chosen nations were then appended. STATA version 16 was used for statistical analysis, data extraction, appending, and re-coding. Frequency, percentage, text, and tables were used to analyze and present descriptive statistics. A weighting factor (v005/1000000) has been applied to the datasets to account for under- and over-reporting in the surveys. We anticipated applying logistic regression because the dependent variable was binary. Furthermore, the hierarchical structure of DHS data goes against the presumption of observational independence because it increases the likelihood of close relationships between women in a given country or cluster compared to those in other clusters. Consequently, it makes sense to use a multilevel regression model as an analysis tool. To find related factors, a three-level mixed-effects logistic regression was used.
We calculated the intra-class correlation coefficient (ICC) and the median odds ratio (MOR) to highlight the unexplained heterogeneity of the outcome across clusters and countries. When two areas are randomly selected, the MOR is the median value of the OR between the areas with the highest and lowest risk [36]. The proportion of variance explained by higher-level units can be summarized by the ICC [37].
Model building process
A null model (Model 0) served as the starting point for the model-building process. Subsequently, more complicated models, such as a model containing only individual factors (Model I), a model containing only community factors (Model II), and a model with both individual and community-level factors (Model III), were constructed. Using log likelihood (LL), deviance, and information criteria (AIC), we compared these models. Model III was a better model. The factors linked to anemia in HIV-positive women were then determined by fitting a bivariable and multivariable two-level generalized linear mixed effect model. The variability in the odds of anemia explained by successive models was calculated using proportional change in variance (PCV) as follows:
Where VA and VB are the neighborhood variance in the empty model and the variance in the successive models [36]. Ultimately, significant factors were identified using adjusted odds ratios (OR) in the multivariable analysis of the chosen model, along with a 95% confidence interval (CI) and a p-value ≤ 0.05.
Survey datasets included and missing values
Demographic and health survey data, which also have HIV data, were included. Additionally, survey data sets were included in the individual dataset file that contained the most recent HIV test results. However, this analysis did not include survey data sets that did not have an HIV dataset or that did not provide anemia data or HIV test results in the individual dataset. Furthermore, our analysis only incorporates surveys completed after 2010. After checking the type and percentage, missing values were managed using the mode imputation technique. The “mdesc” STATA package was used to determine the percentage of missing values. Two variables, such as history of termination of pregnancy (1 observation (0.013%)) and current working status of a woman (5 observation (0.064%)), had missing values. Since the percentage of missing values is < 5%, we conducted a mode imputation [38] and then a sensitivity analysis.
Ethical considerations
Since the study was a secondary data analysis based on publicly accessible datasets (DHS records), participant participation and ethical approval were not required. Nevertheless, we asked the MEASURE DHS Program for the data, and we were permitted to utilize it.
Result
A total of 7823 weighted samples from 18 SSA countries were included in this study. About 23.29% of the participants were from Zambia, followed by Zimbabwe (18.52%). About 46.66% and 48.09% of the participants were 35 or older and attended secondary education, respectively. More than half (53.19% and 54.89%) were currently in union or living with a man and not working during the survey regarding their employment status, respectively. Almost three-fourths (74.92%) had no media exposure. About one-fourth (25.89%) of the participants were from households with a richer wealth quintile. More than half (51.05%) of the participants were living in urban areas (Table 1).
Prevalence of anemia
The overall prevalence of anemia was found to be 45.1% [95% CI: 43.97–46.18%]. Of those, 5.05% and 37.97% were severely and moderately anemic, while the rest, 56.97%, were mildly anemic. In terms of the distribution of the problem across countries, the highest prevalence was observed in Cote d’Ivoire (76.2%), while the lowest was observed in Ethiopia (32.6%). Half of the countries had more than 50% of the anemia prevalence among HIV-infected women (Fig. 1).
The magnitude of anemia shows a big difference (7.7%) between pregnant and non-pregnant HIV-infected women. This difference is statistically significant (P = 0.003) (Fig. 2).
Factors associated with anemia among HIV infected women
Random effect analysis
The estimated ICC for both cluster and country levels separately was 1% [95% CI: 0.0%, 3%] and 7% [95% CI: 3%, 13%], respectively. The combined cluster and country-level ICC was estimated to be 11% [95% CI: 8%, 14%]. This indicates that cluster-level clustering alone explains only 1% of the variation in anemia, while country-level clustering explains about 7% of the variation in anemia. The correlation of anemia between two women within a similar cluster is 0.01, while the correlation of anemia between two women from the same cluster within a country is 0.11. Women living in similar countries were more similar than women living in neighboring countries. A likelihood-ratio (LR) test comparing the model with ordinary logistic regression was also significant (chibar2 (01) = 47.40, P = 0.0000) The LR test shows that the three-level model is preferred to its single-level counterpart (chibar2 (01) = 47.46, P = 0.0000). The three-level model is also preferred to the two-level model (X2 = 43.08, P = 0.0000). Thus, a multilevel approach is favored over an ordinary approach and also over carrying out either of the potential two-level analyses. Thus, the clustering effect alone explained 11% of the variation in anemia among women living with HIV. The MOR was 1.78 [95% CI: 1.59, 1.97]. If we pick two clusters randomly from two countries with high and low prevalence of anemia and then move a woman from a low to high prevalence area and country, the probability of anemia increases by 1.78 fold. Candidate multilevel models such as the Null model, Model I (model with individual level factors), Model II (model with community level factors), and Model III (model with both individual and community level factors) were compared, and finally, Model III was selected since it showed a smaller deviance and AIC. The proportion of variance explained by the final model was 36.51%. Which indicates 36.51% of the variation in anemia status was explained by predictor variables included in the final model (Table 2).
Sensitivity analysis
We first looked at the parameter estimate and the standard error to assess the sensitivity of the results that were presented. Between complete case analysis and mode imputation, the estimated parameter and standard error did not differ much. The complete case analysis and the imputed data for the final model (Model III) were compared for their AIC values (Table 3).
Fixed effect analysis
Our study revealed that women with primary, secondary, and higher education levels had 26% [AOR = 0.74, 95% CI: 0.62, 0.89], 19% [AOR = 0.81, 95% CI: 0.68, 0.98], and 26% [AOR = 0.74, 95% CI: 0.55, 0.99] lower odds of anemia compared to non-educated women. Pregnant and breast-feeding women had 51% [AOR = 1.51, 95% CI: 1.17, 1.94] and 38% [AOR = 1.38, 95% CI: 1.17, 1.64] increased odds of anemia compared to their counterparts, respectively. Moreover, women who had health insurance and menstruation within six weeks prior to data collection indicated 50% [AOR = 1.50, 95% CI: 1.25, 1.80] and 36% [AOR = 1.36, 95% CI: 1.20, 1.54] higher odds of anemia compared to their counterparts, respectively. While current contraceptive users had a 26% decreased odds [AOR = 0.74, 95% CI: 0.63, 0.87] of anemia (Table 4).
Discussion
In this study, anemia prevalence and related factors among HIV-positive women living in SSA were investigated. Accordingly, findings from this study indicate that the overall prevalence of anemia was found to be 45.1% [95% CI: 43.97–46.18%]. Of those, 5.05% and 37.97% were severely and moderately anemic, while the rest, 56.97%, were mildly anemic. Anemia is a serious public health issue among HIV-positive women in SSA nations, according to the World Health Organization’s classification of public health relevance [3].
Based on the WHO classification of public health significance or the seriousness of anemia in the population, 15 out of 18 countries included in this study, such as Burkina Faso, Cote d’Ivoire, the Democratic Republic of the Congo, Gabon, Ghana, Guinea, Malawi, Niger, Senegal, Sierra Leone, South Africa, Togo, Tanzania, Zambia, and Zimbabwe, have a problem of severe public health significance that ranges from 40.6 to 76.2%. Nine countries had more than 50% and above anemia prevalence among HIV-infected women. While for the rest of the three countries (Ethiopia, Lesotho, and Namibia), the problem of anemia is a moderate public health problem and ranges between 32.6 and 35.5%.
This 45.1% prevalence of anemia among HIV-infected women is approximately similar to a finding from a systematic review and meta-analysis (46.6%) [5]. However, our finding is different from the global estimate of anemia among reproductive-aged women, which was 29.9% in 2019 [39] and 30% in 2023 [1]. This indicates that HIV hugely influences the hematological function of our body system due to different effects, like the effect of antiretroviral therapy or its negative effect on health, like diarrhea and other opportunistic infections [11, 12, 16, 17, 40]. However, our finding is lower than the previous study conducted in Johannesburg, South Africa (60%) [41]. This might be due to the population difference where the previous study was conducted among pregnant women. Our finding is also higher than findings from Ethiopia (38.6% [42], 34.8% [43]), and Uganda (16.8%) [20]. This might be due to age and sex differences across the two studies. The previous studies were conducted among adults and both sexes, given that age and sexes are strongly related to anemia [44, 45].
Our study revealed that women with formal education (primary, secondary, or higher education) had lower odds of anemia compared to non-educated women. This finding is also supported by a study conducted among reproductive-age women in middle- and low-income countries [46]. Education has a positive effect on nutritional knowledge, which means that as their education level increases, their nutritional knowledge also increases [47]. Moreover, education has a positive and long-term impact on individuals’ lifestyles and eating habits [48], dietary diversity, and healthy eating habits among women due to their exposure to nutritional messages through different media outlets [49]. Beyond iron deficiency, which is considered the most common nutritional deficiency leading to anemia, deficiencies in vitamin A, folate, vitamin B12, and riboflavin can also result in anemia due to their specific roles in the synthesis of hemoglobin and/or erythrocyte production [1]. Thus, education plays a vital role in reducing these and other nutritional deficiencies.
Pregnant and breast-feeding women had increased odds of anemia compared to their counterparts. Another study conducted in Zimbabwe also declared that breast-feeding HIV-infected women had a higher risk of anemia [50]. The reason behind this is maternal iron depletion during lactation as well as blood loss during childbirth among lactating mothers [51, 52], since breast milk is one source of iron for children [53]. Other studies also revealed a significant relationship between anemia and pregnancy [8,9,10, 19, 26,27,28, 54]. This is because pregnancy can cause major changes to the body, such as a 20–30% increase in blood volume (erythroid hyperplasia of the marrow and an increase in red blood cell mass), which raises the body’s iron reserves necessary for the fetus’s nourishment and hemoglobin production. When women do not acquire enough iron during the second and third trimesters, their plasma volume increases disproportionately, and hemodilution occurs [55, 56].
Women who had menstruated within the six weeks before data collection had increased odds of anemia. Previous reports [7, 56] also corroborate this finding. This could be due to the fact that iron insufficiency is brought on by severe menstrual bleeding [57, 58]. Furthermore, compared to their counterparts, women with health insurance had greater odds of anemia, according to our study. This is consistent with research that was done in Mali [8]. This demonstrates that having health insurance by itself does not ensure the prevention of anemia; rather, women living with HIV can prevent and halt the burden of anemia by making better and healthier eating choices. Despite our findings, research done on children in Ghana showed that health insurance had a protective impact [59].
Comparing current contraceptive users to non-users, the former had lower odds of anemia. It is also supported by earlier research [60, 61] that women who use some hormonal contraceptives can have decreased anemia. In addition, hormonal contraceptive techniques have been shown to lessen menstrual bleeding in women who experience periods of heavy bleeding [62]. This evidence also explains why women who had previously menstruated within six weeks of the data collection had a greater prevalence of anemia among women living with HIV. Furthermore, contraception has a vital role in reducing the number of pregnancies and prolonging the interval between pregnancies, birth, and breast feeding as well, which can significantly reduce iron-deficiency anemia [63]. Our findings imply that public health policy planners may benefit from taking maternal and obstetrics-related factors into account to reduce anemia among HIV-infected women. Additionally, it encourages health sector managers and health professionals to emphasize anemia among HIV-positive women during pregnancy and breast feeding.
Our study’s primary strength is the use of nationally representative, population-based samples that encompass both rural and urban areas. Because DHS employs a uniform methodology across countries, it facilitates the cross-national comparison of prevalence estimates. However, there are certain constraints to our study. Given the complex nature of the cause of anemia, several behavioral, lifestyle, and antiretroviral treatment-related factors may be strongly correlated with anemia. However, we are unable to investigate their effects because these significant variables are absent from the datasets. Due to this, the estimated prevalence and effect of factors included in our study may be affected.
Conclusion
Based on our findings, anemia is a serious public health problem among HIV-infected women in SSA countries. In 15 out of 18 countries included in this study, anemia is of severe public health significance. Pregnancy, breast feeding, health insurance, and menstruation within six weeks prior to data collection were significant risk factors. On the other hand, primary, secondary, and tertiary education levels and current contraceptive use were significant protective factors for anemia among HIV-infected women in SSA countries. Therefore, strategies aimed at early identification of anemia may lead to an improvement in the health of HIV-infected women in SSA countries.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- AIC:
-
Akaike Information Criteria
- AOR:
-
Adjusted Odds Ratio
- DHS:
-
Demographic and Health Survey
- HIV:
-
Human immunodeficiency Virus
- ICC:
-
Intraclass Correlation Coefficient
- LL:
-
Log-Likelihood Ratio
- MOR:
-
Median Odds Ratio
References
World Health Organizatio. Anaemia. 2023 [cited December 8, 2023; https://www.who.int/news-room/fact-sheets/detail/anaemia#:~:text=Globally%2C it is estimated that,due to disability in 2019
Pan American Health Organization. Anemia in women of reproductive age, and children under-five years in the Region of the Americas. 2022 [cited December 8, 2023; https://www.paho.org/en/enlace/anemia-women-and-children
world Health Organizatio. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity, Vitamin and Mineral Nutrition Information System. 2011 [cited December 8, 2023; http://www.who.int/vmnis/indicators/haemoglobin.pdf
Nti J, et al. Variations and determinants of Anemia among Reproductive Age women in five Sub-saharan Africa Countries. Biomed Res Int. 2021;2021:p9957160.
Cao G, et al. Prevalence of anemia among people living with HIV: a systematic review and meta-analysis. EClinicalMedicine. 2022;44:101283.
Rahman MM, et al. Maternal anemia and risk of adverse birth and health outcomes in low-and middle-income countries: systematic review and meta-analysis, 2. Am J Clin Nutr. 2016;103(2):495–504.
Tsegaye Negash B, Ayalew M. Trend and factors associated with anemia among women reproductive age in Ethiopia: a multivariate decomposition analysis of Ethiopian demographic and Health Survey. PLoS ONE. 2023;18(1):e0280679.
Armah-Ansah EK. Determinants of anemia among women of childbearing age: analysis of the 2018 Mali demographic and health survey. Archives Public Health. 2023;81(1):10.
Tirore LL, et al. Factors associated with anaemia among women of reproductive age in Ethiopia: Multilevel ordinal logistic regression analysis. Matern Child Nutr. 2021;17(1):e13063.
Kibret KT, et al. Spatial distribution and determinant factors of anaemia among women of reproductive age in Ethiopia: a multilevel and spatial analysis. BMJ Open. 2019;9(4):e027276.
O’Connell C, Levine AM. Managing Anemia in HIV-Positive women. Women’s Health. 2006;2(1):159–65.
O’Brien ME, et al. Anemia is an independent predictor of mortality and immunologic progression of disease among women with HIV in Tanzania. J Acquir Immune Defic Syndr. 2005;40(2):219–25.
Berhane K et al. Impact of highly active antiretroviral therapy on Anemia and Relationship between Anemia and Survival in a large cohort of HIV-Infected women: women’s interagency HIV Study. JAIDS J Acquir Immune Defic Syndr, 2004. 37(2).
Grossman HA, et al. Once-weekly epoetin alfa dosing is as effective as three times–weekly dosing in increasing hemoglobin levels and is associated with improved quality of life in anemic HIV-infected patients. JAIDS J Acquir Immune Defic Syndr. 2003;34(4):368–78.
Revicki DA et al. Recombinant human erythropoietin and health-related quality of life of AIDS patients with anemia. 1994, LWW. pp. 474–484.
Volberding PA, et al. Anemia in HIV infection: clinical impact and evidence-based management strategies. Clin Infect Dis. 2004;38(10):1454–63.
Bain BJ. Pathogenesis and pathophysiology of anemia in HIV infection. Curr Opin Hematol. 1999;6(2):89.
Sahud MA, et al. Von Willebrand factor-cleaving protease inhibitor in a patient with human immunodeficiency syndrome-associated thrombotic thrombocytopenic purpura. Br J Haematol. 2002;116(4):909–11.
Assefa E. Multilevel analysis of anemia levels among reproductive age groups of women in Ethiopia. SAGE Open Med. 2021;9:2050312120987375.
Kaudha R, et al. Anemia in HIV patients attending highly active antiretroviral therapy clinic at Hoima Regional Referral Hospital: prevalence, morphological classification, and Associated factors. HIV/AIDS-Research and Palliative Care; 2023. pp. 621–32.
Khan AS, Shahid M. Maternal and Newborn Care practices among the Muslim Slum Dwellers in India: does the popular common sense matter? Int J Community Social Dev. 2022;4(4):426–41.
Nagari SL et al. Anemia among women using Family Planning at Public Health Facilities in Ambo Town, Central Ethiopia: Multi-center Cross-sectional Study. J Blood Med, 2023: p. 83–97.
Woldu B, et al. Prevalence and Associated Factors of Anemia among Reproductive-aged women in Sayint Adjibar Town, Northeast Ethiopia: community-based cross-sectional study. Anemia. 2020;2020:p8683946.
Belay DG, et al. Geographically weighted regression analysis of anemia and its associated factors among reproductive age women in Ethiopia using 2016 demographic and health survey. PLoS ONE. 2022;17(9):e0274995.
Habyarimana F, Zewotir T, Ramroop S. Spatial distribution and analysis of risk factors associated with Anemia among women of reproductive age: case of 2014 Rwanda demographic and health survey data. Open Public Health J, 2018. 11(1).
Talukder A, et al. Risk factors associated with anemia among women of reproductive age (15–49) in Albania: a quantile regression analysis. Clin Epidemiol Global Health. 2022;13:100948.
Arabyat R, Arabyat G, Al-Taani G. Prevalence and risk factors of anaemia among ever-married women in Jordan. East Mediterr Health J, 2019. 25(8).
Shitu K, Terefe B. Anaemia and its determinants among reproductive age women (15–49 years) in the Gambia: a multi-level analysis of 2019–20 Gambian Demographic and Health Survey Data. Archives Public Health. 2022;80(1):228.
Sunuwar DR, et al. Factors affecting anaemia among women of reproductive age in Nepal: a multilevel and spatial analysis. BMJ Open. 2021;11(3):e041982.
Alem AZ, et al. Prevalence and factors associated with anemia in women of reproductive age across low- and middle-income countries based on national data. Sci Rep. 2023;13(1):20335.
Kharsany AB, Karim QA. HIV infection and AIDS in sub-saharan Africa: current status, challenges and opportunities. open AIDS J. 2016;10:34.
World Health Organization. THE GLOBAL HEALTH OBSERVATORY(HIV). 2022 July 2022 [cited 2023; https://www.who.int/data/gho/data/themes/hiv-aids
UNAIDS. Global HIV & AIDS statistics — Fact sheet. 2023; https://www.unaids.org/en/resources/fact-sheet
Croft TN, et al. Guide to DHS statistics. Rockville: ICF; 2018. p. 645.
Guide to DHS Statistics (Analyzing DHS Data). https://dhsprogram.com/data/Guide-to-DHS-Statistics/index.htm#t=Analyzing_DHS_Data.htm
Merlo J, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60(4):290–7.
Leyland AH, Groenewegen PP. Multilevel modelling for public health and health services research: health in context. Springer Nature; 2020.
Dettori JR, Norvell DC, Chapman JR. The sin of Missing Data: is all forgiven by way of Imputation? Global Spine J. 2018;8(8):892–4.
Organizatio WH. Anaemia in women and children(WHO Global Anaemia estimates). 2019 [cited December 8, 2023; 2021:[ https://www.who.int/data/gho/data/themes/topics/anaemia_in_women_and_children
Luther JM, et al. Utility of bone marrow biopsy for rapid diagnosis of febrile illnesses in patients with human immunodeficiency virus infection. South Med J. 2000;93(7):692–7.
Odhiambo C, et al. Anaemia in HIV-infected pregnant women receiving triple antiretroviral combination therapy for prevention of mother-to-child transmission: a secondary analysis of the Kisumu breastfeeding study (KiBS). Tropical Med Int Health. 2016;21(3):373–84.
Hadgu R, et al. Prevalence, severity and associated risk factors of anemia among human immunodeficiency virus-infected adults in Sawla General Hospital, Southern Ethiopia: a facility-based cross-sectional study. PLoS ONE. 2023;18(12):e0284505.
Zenebe WA, Anbese AT, Tesfaye TS. Anemia And Associated Factors Among Adult People Living With HIV/AIDS Receiving Anti-Retroviral Therapy At Gedeo Zone, SNNPR, Ethiopia, 2018 HIV/AIDS-Research and Palliative Care, 2019: pp. 351–356.
Krishnapillai A et al. The prevalence of Anemia and its Associated factors among older persons: findings from the National Health and Morbidity Survey (NHMS) 2015. Int J Environ Res Public Health, 2022. 19(9).
Akbarpour E, et al. Anemia prevalence, severity, types, and correlates among adult women and men in a multiethnic Iranian population: the Khuzestan Comprehensive Health Study (KCHS). BMC Public Health. 2022;22(1):168.
Hasan MM, et al. Anaemia in women of reproductive age in low-and middle-income countries: progress towards the 2025 global nutrition target. Bull World Health Organ. 2022;100(3):196.
Qiu Y et al. The Nutrition Knowledge Level and influencing factors among Chinese women aged 18–49 years in 2021: data from a nationally Representative Survey. Nutrients, 2023. 15(9).
Moscatelli F, et al. Assessment of Lifestyle, eating habits and the Effect of Nutritional Education among undergraduate students in Southern Italy. Nutrients. 2023;15(13):2894.
Makate M, Nyamuranga C. The long-term impact of education on dietary diversity among women in Zimbabwe. Rev Dev Econ. 2023;27(2):897–923.
Gona PN, et al. Intersection of HIV and Anemia in women of reproductive age: a 10-year analysis of three Zimbabwe demographic health surveys, 2005–2015. BMC Public Health. 2021;21(1):41.
Domellöf M, et al. Iron, zinc, and copper concentrations in breast milk are independent of maternal mineral status. Am J Clin Nutr. 2004;79(1):111–5.
Lakew Y, Biadgilign S, Haile D. Anaemia prevalence and associated factors among lactating mothers in Ethiopia: evidence from the 2005 and 2011 demographic and health surveys. BMJ Open. 2015;5(4):e006001.
Bodnar LM, et al. High prevalence of postpartum anemia among low-income women in the United States. Am J Obstet Gynecol. 2001;185(2):438–43.
Oladeinde BH, et al. Prevalence of HIV and anemia among pregnant women. N Am J Med Sci. 2011;3(12):548–51.
AMERICAN SOCIETY OF HEMATOLOGY. Anemia and Pregnancy. 2021; https://www.hematology.org/education/patients/anemia/pregnancy
Lara A, Friel. Anemia in Pregnancy. 2023 [cited December 18, 2023; https://www.msdmanuals.com/professional/gynecology-and-obstetrics/pregnancy-complicated-by-disease/anemia-in-pregnancy#:~:text=The most common causes of,pregnancy%2C consider treating women prophylactically
Munro MG, et al. The relationship between heavy menstrual bleeding, iron deficiency, and iron deficiency anemia. Am J Obstet Gynecol. 2023;229(1):1–9.
Munro MG. Heavy menstrual bleeding, iron deficiency, and iron deficiency anemia: framing the issue. Int J Gynecol Obstet. 2023;162(S2):7–13.
Anaba EA, et al. Association between health insurance membership and anaemia among children under-five years. Evidence from Ghana. PLoS ONE. 2020;15(9):e0238792.
Teshome AA, Berra WG, Huryi AF. Modern contraceptive methods predict hemoglobin levels among women of Childbearing Age from DHS 2016. Open Access J Contracept. 2022;13:1–8.
Organization WH. The global prevalence of anaemia in 2011 [Internet] World Health Organization, 2015. 2015.
Andrew M, Kaunitz. Patient education: Heavy or prolonged menstrual bleeding (menorrhagia) (Beyond the Basics). 2022 [cited December 18, 2023; https://www.uptodate.com/contents/heavy-or-prolonged-menstrual-bleeding-menorrhagia-beyond-the-basics/print#:~:text=Hormonal birth control — If you,bleeding during your menstrual period
Effects of contraceptives on hemoglobin and ferritin. Contraception, 1998;58(5):261–73.
Acknowledgements
For providing access to the DHS datasets, we are grateful for the MEASURE DHS initiative.
Funding
The author(s) received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
WMT conceptualized the idea, contributed to data curation, formal analysis, investigation, methodology, project administration, resources, software, supervision, validation, writing the original draft, and editing the final manuscript. ZAG, HG, and MBS helped with investigation, methodology, project administration, resources, supervision, validating, and editing the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was conducted based on the demographic and health survey datasets of the above-mentioned 18 countries. Permission was granted to use the datasets from the MEASURES DHS program.
Consent
Not applicable.
Conflict of interest
The authors declare no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tilahun, W.M., Gebreegziabher, Z.A., Geremew, H. et al. Prevalence and factors associated with anemia among HIV-infected women in sub-saharan Africa: a multilevel analysis of 18 countries. BMC Public Health 24, 2236 (2024). https://doi.org/10.1186/s12889-024-19758-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19758-2