Abstract
Background
Coaching on Lifestyle (CooL) is a two-year healthcare intervention for people with overweight or obesity, stimulating weight reduction by promoting sustained healthier behavior. The objective of this study is to investigate the effects of CooL on participants’ anthropometrics, personal factors and behavioral factors over the two-year timeframe of CooL.
Methods
A descriptive case series study, using a broad set of routinely collected data on anthropometrics, personal factors and behavioral factors of adults living across the Netherlands. The data were collected between November 2018 and December 2021 among participants of CooL (N = 746) at three moments during the intervention: at baseline (T0), at 8 months (T1) after completion of phase 1 and at 24 months (T2) after ending CooL. Changes over time were analyzed using paired t-tests comparing baseline to T1 and baseline to T2. In addition, potential differences on outcomes in subgroups based on education level, weight status and group size were examined using paired t-tests and ANOVA-tests.
Results
The results showed positive changes on all outcomes at 24 months compared to baseline. The largest effects were on perceived health, attentiveness towards meal size and meal composition (large effect size). Mean weight loss was 4.13 kg (SD 7.54), and mean waist circumference decreased with 4.37 centimeters (SD 8.59), indicating a medium to large effect size. Changes were consistent across subgroups varying in educational level, BMI at baseline and group size.
Conclusion
The study demonstrated sustained weight-related effects of CooL over 24 months supporting its two-year duration. The results indicate that CooL, though not for every individual, is in general appropriate and effective for different group sizes and for a wide variety of participants regardless of level of education, or BMI at baseline.
Trial registration
Dutch Trial Register NTRNL6061 (13-01-2017). Registered at Overview of Medical Research in the Netherlands (OMON), via https://www.onderzoekmetmensen.nl/.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Obesity is considered a chronic disease according to the World Health Organisation (WHO) [1] and the Dutch Health council [2] and it is linked to many other diseases – both physical and mental [3] – and a diminished quality of life [4].
Overweight is more common among men (53%) than women (47%), obesity on the other hand is more prevalent in women (17%) than in men (12%). Approximately 41% of people with a higher level of education are overweight whereas this percentages rises to 60% for people with a lower level of education. The proportion of people with severe obesity is twice as high among people with a lower level of education (18%) compared to those with a higher level of education (10%) [5].
Consensus has been reached internationally on the importance of an integrated approach to target overweight and obesity, including limited energy intake, healthy food choices and regular physical activity [6]. The Dutch national guidelines have added stress management and sleep as additional essential elements to tackle overweight and obesity [7].
As of January 2019, Combined Lifestyle Interventions (CLIs) are part of basic health insurance. Having a basic health insurance is a legal obligation for every person living or working in the Netherlands, and as such a CLI is available for all adults meeting the inclusion criteria (i.e. being obese (BMI > 30) or being overweight (25 < BMI < 30) combined with comorbidity; and being sufficiently motivated). CLIs are two-year healthcare interventions for people with overweight or obesity, stimulating weight reduction by promoting sustained healthier behavior. Several CLIs are available in the Netherlands such as SLIMMER [8] and BeweegKuur [9]. Coaching on Lifestyle (CooL) is one of these CLIs. The set-up of CooL is in line with the recommendations of the WHO [10]. In addition, the outcomes of the first eight months of CooL, even during COVID-19 and its accompanying restrictions, showed substantial and promising results. The WHO-recommendations and the promising results from previous research make CooL an appropriate intervention for people that are overweight or obese [6, 11].
Research on long term effects of lifestyle and/or behavior change interventions has been done mainly on specific patient groups and disease related outcome measures [12]. The long-term effects of CLIs (including CooL) in the Netherlands are still unknown, mainly due to the short timespan that the CLI is currently running. So far, outcomes over the full intervention period are limitedly available and when outcomes are available, they are showing a stabilization or small relapse in the second year of the intervention both within the Dutch context [8] as well as in a more international setting [13,14,15]. All this resulted in the following research questions: What changes over time do we see with CooL-participants on the 2-year timespan? And how do they relate to the changes after the first 8 months of the intervention? Related to this, we are curious about the efficacy of the intervention and especially the potential in real life as the two-year timespan of the intervention will more likely result in dropouts than interventions with a shorter time span. This is the first research on the changes over time on participants over the full CooL-intervention course of 24 months.
We suspect the changes in outcomes to vary with differences in participants and with differences in the context in which the intervention is executed.
Several studies show similar outcomes for participants with a lower level of education and a higher level of education, once enrolled in the program and given that the program fits the needs of this target group [16, 17]. We suspect however that the CooL intervention is less effective for people with a lower level of education in line with research indicating that level of education shows a strong and positive correlation with health, health related behaviors [17, 18] and health literacy [19]. Especially since CooL strongly relies on self-management skills which are less prevalent among people with low health-literacy [20, 21].
A lower BMI at baseline has previously been associated with better program adherence [22] and a higher BMI is associated with unhealthier food choices, i.e. less fruit and vegetable, less fiber, and more fried food consumption [23] whereas on the other hand health interventions seem equally appropriate for different BMI-categories at baseline [24]. These contradictory findings sparked our interest to investigate the relationship between BMI at baseline and differences in effect sizes on the outcomes of CooL as well. Furthermore, we are interested in the differences in effect of a large versus a small group size on the CooL outcomes. No consensus has yet been reached on the optimal group size for group interventions, while in CooL these group sizes vary per context. Research in education has shown that a group size of five, compared to fifteen members, enhances participation and satisfaction of the group members [25] whereas groups of nine or more participants bring diversity of thought, experiences, and viewpoints, thereby stimulating active participation of group members [26]. Group lifestyle interventions are usually offered in groups of 10 up to 15 participants [27, 28]. These mixed findings do not provide a clear picture on the optimal group size for health interventions. In our definition, aligned with the practice of CooL, large groups consist of 10 or more participants whereas small groups have less than 10 participants. We hypothesize that participants in small CooL groups show larger effect sizes on the outcomes of CooL because a smaller group provides the coach with more time and focus per participant, thereby stimulating active participation and behavior change.
In summary, we want to investigate the impact of the context of participants on CooL-outcomes on three different topics, resulting in the following research questions: Do we find differences in changes over time of the CooL-intervention for people with a lower level of education compared to people with a medium or higher level of education? In addition, are there any differences for the BMI-classes: BMI 25–30, BMI 30–35, BMI 35–40 and BMI 40+? And lastly, does a group size of 10 or more participants generate differences in changes over time compared to a group size of less than 10 participants?
Our objective is to study the effects of CooL after 24 months on anthropometrics, personal factors and behavioral factors of the participants. In addition, we want to analyze potential differences on the outcomes for people with lower education compared to medium or higher education, people with a lower BMI at baseline compared to a higher BMI and for people participating in CooL in groups under or over 10 participants.
Materials and methods
CooL-intervention
CooL is a Combined Lifestyle Intervention (CLI) including a one-hour intake followed by two consecutive intervention phases. Phase 1 (8 months) focuses on the initiation of behavioral change, followed by phase 2 (16 months) in which both behavioral change and behavioral maintenance are targeted. The intervention consists of individual sessions (6 h in total) and 8 group sessions (1,5 h each) both in phase 1 and phase 2, resulting in a higher density of sessions in phase 1 compared to phase 2. CooL aims at changes in anthropometrics (i.e. weight, BMI and waist circumference) and at an increase in perceived quality of life by stimulating healthier eating habits, less sitting time, more physical activity and attention for sufficient relaxation and high-quality sleep.
CooL is an open CLI, i.e. an intervention without a strict protocol. Coaches may adapt the intervention to the target group and context as long as the essential effective elements of CooL (e.g., goal setting, mobilizing social support, positive psychology, self-management and self-monitoring) are respected in implementation. The CooL-coach is a trained and licensed professional who coaches participants towards a predefined set of final objectives on health-related skills and knowledge. Participants are stimulated to take responsibility for their personal lifestyle changes by addressing motivation, personal objectives and behavioral changes. The CooL-group sessions are focused on experience-oriented and practical learning, learning from peers and providing a strong incentive for behavioral change for all lifestyle aspects. For example, physical activity is not part of the regular CooL-intervention as it is not to be reimbursed via health insurance. Instead, CooL focuses on stimulating participants in being (more) physically active. Thereby enabling a fit between the objectives, starting point and daily pattern of each participant on activity, frequency and intensity. The objective is not to provide an activity program only for the duration of CooL but a sustained behavioral change towards a more active life.
The main objective is to coach and activate participants to a sustained healthier lifestyle in line with their individual needs and personal goals.
Study design and population
As CooL is part of regular health care in the Netherlands, a control group receiving no treatment would be both unethical and impractical, making a descriptive case series study the appropriate study design in the Dutch context. The participants are adults living throughout the Netherlands. All participants met the inclusion criteria for participating in a CLI and were referred to CooL by their general practitioner, practice nurse or internist. The decision on a proper fit for inclusion was up to the participant, the referrer and the coach. All participants signed an informed consent regarding data collection for this study.
Data collection
We used a lifestyle questionnaire and anthropometric measurements to collect a broad set of data. The lifestyle questionnaire was based on existing validated questionnaires. The outcome measures can be divided into the categories: anthropometrics (i.e. weight/BMI and waist circumference), control and support (i.e. self-mastery and social support), physical activity (i.e. sedentary time and active minutes), diet attentiveness, alcohol use and smoking, perceived fitness (i.e. perceived health, fitness and impact of stress on daily functioning), sleep and stress.
During the course of the study, the questionnaire was extended with additional questions covering changes in context (e.g. COVID-19) and adjusted with textual simplifications in both questions and answers preserving the original essence as much as possible.
Datasets
Data collection on the CooL intervention is ongoing as CooL is part of basic healthcare. Data is collected via the CooL questionnaire, filled out by participants at T0 (baseline), T1 (after 8 months) and at T2 (after 24 months) and handed over to the CooL-coach who stores the data in line with privacy regulations. Data is transferred to the researchers at T1, containing both data on baseline and T1, and at T2, containing data on T0, T1 and T2. Before sending the data to the researchers, the CooL-coach anonymizes the data. The CooL database contains consequently datasets on T0 -T1 and on T0-T1-T2 from the participants that sent in their data. Once sent in, datasets cannot be matched due to the necessary anonymization by the CooL-coach.
Data for this study were collected from November 2018 until December 2021 at three moments in time: at baseline, during the intake (T0), after completion of phase 1 (T1) and after ending CooL (T2). No information is available on the exact number of participants starting with or dropping out of the intervention as data is submitted only by participants who agreed to share data. In addition, data collection is restricted to two moments during the intervention: after 8 months (at T1) and when ending CooL (at T2). The data at T2 contains participants that completed the intervention (sent in after approximately 24 months) and participants that dropped out earlier in time (sent in at the moment of dropout, which could be at any moment during the two-year intervention). Participants with a T2 measurement were included in the dataset if their (estimated) completion date of CooL was or would have been before the end of the data collection period, i.e. December 31st 2021.
All analyses were performed between May 2022 and May 2023 and were done on the full dataset (A, n = 746) consisting of program finishers and dropouts, to provide a realistic reflection of the potential intervention effects in practice. In addition, we analyzed a cleaned dataset (B, n = 396) including all participants that completely finished the two-year intervention, to portray efficacy of the intervention. Changes over time were measured from baseline to T1 and from baseline to T2.
Demographics
At baseline, participants reported their personal characteristics such as gender, date and country of birth, highest completed education, marital status, living situation and occupational status. Educational level was categorized in line with the Dutch Central Bureau of Statistics (CBS) into low (i.e., no education or primary education), intermediate (e.g., secondary education) and high (e.g., tertiary education). The living situation was divided into living together with someone (married or cohabiting) with or without kids and living alone (divorced, unmarried or widowed) with or without kids. The occupational status was categorized into working (e.g. paid work, voluntary work or self-employed) and not working (e.g. stay-at-home, unemployed, retired or student). Country of birth was categorized into Dutch or non-Dutch.
Anthropometrics
Under normal conditions anthropometric data (weight, length and waist circumference) were measured by the CooL-coaches with professional equipment according to the guidelines provided by the Dutch Association of General Practitioners (Dutch: Nederlands Huisartsen Genootschap, NHG) [29]. Body weight (kg) was measured in kilogram, rounded off the nearest decimal. Height (m) was measured to the nearest centimeter without shoes. Waist circumference measurements were obtained to the nearest centimeter with a tape measure. As COVID-19 restrictions could have changed the measurement method, additional information, gathered from the CooL-coaches that were the main data suppliers (representing data of 227 participants), confirmed that in general, physical measurements took place either by the coach or on a distance of 1.5 m under direct supervision of the coach.
Control and support
The self-mastery questions in the questionnaire were based on the short version of the Pearlin Mastery Scale using four questions (for example “I have little control over the things that happen to me”) and a 5-point Likert scale ranging from strongly agree (1) to strongly disagree (5) [30]. To identify social support, we questioned the perceived support of close ones using a 5-point Likert scale ranging from no support at all (1) to a lot of support (5).
Physical activity
The outcome measurements on physical activity, diet and personal factors were defined in cooperation with the Dutch Association of Lifestyle Coaches (BLCN) with the objective to capture the essence and map the desired outcomes of lifestyle coaching in a minimum set of questions. Physical activity used questions on sedentary behavior, both on most and least active days (“What is the average number of hours you spent sitting on the day of the week you sit the most?”) and the number of physical activity minutes per day (“What is the average minutes per day that you are physically active (in minimum bouts of 10 minutes)?”).
Diet attentiveness, alcohol and smoking
We defined questions on dietary attentiveness, in line with the input of the BLCN, based on the idea that deliberate behavior changes start with being aware of one’s own behavior. We used questions on the attentiveness of participants towards meal composition and meal quantities and attentiveness during the actual consumption of food using a 5-point Likert scale from very little attention (1) to a lot of attention (5). At T1 and T2 an additional question was added regarding changes in eating pattern: a reflection of the perception on healthy diet improvements compared to baseline (“How much healthier have you been eating since the intake of this program?”) with the answers ranging from much healthier (1) to much unhealthier (5). The amount of alcohol and smoking was questioned by numerical values.
Perceived fitness
Perceived fitness existed of questions, in line with the input of the BLCN, on perceived fitness when waking up and during the day, the impact of stress on daily functioning and on perceived health (i.e. feeling good about oneself, the extent of self-care invested and the perception of one’s general health). Questions were answered using a 5-point Likert scale, ranging from not good at all (1) to very good (5).
Sleep
We defined a specific set of questions around the sub-constructs: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication and daytime dysfunction, analogous to the validated and widely used PSQI-questionnaire [31]. Each subconstruct was covered by one or two question(s) using a numerical value or a 4-point Likert scale, ranging from ‘never’ (1) to ‘three times per week or more frequently’ (4).
Stress
For stress, the validated Perceived Stress Scale questionnaire was used, which exists of ten questions using a 5-point Likert scale from never (1) to always (5) [32].
Statistical analyses
Data preparation
We recoded some of the variables to facilitate interpretation in the sense that a higher/positive score refers to a desirable trend and a lower/negative score to an undesirable trend in the variable. For constructs based on validated questionnaires (i.e. sleep and stress) we adopted the accompanying approach without recoding. Secondly, we performed an exploratory factor analysis and calculated McDonald’s omega to assess the internal structure of items regarding several constructs such as perceived health, self-mastery, sleep and stress in line with Crutzen et al. [33]. These analyses justified summarizing all lifestyle constructs by item score means. Missing data were excluded from the statistical analyses.
Effect sizes
For all items and constructs, we ran descriptive statistics. Changes over time were analyzed using paired t-tests comparing baseline to T1 and baseline to T2. Effect sizes were calculated and interpreted in accordance with Lipsey’s guidelines for each pair of items or constructs, i.e. an effect size smaller than 0.32 is considered small, an effect size between 0.33 and 0.55 is considered medium and an effect size above 0.56 is considered large [34]. To improve comprehensibility effect sizes were represented such that positive values represented change in the desired direction whereas negative values represented change in an undesired direction. All T-tests were performed using SPSS-software (version 27). Missing data were excluded from the statistical analyses.
To be considered successful the target for the CLI (including CooL) is an average 5% weight loss for all participants, as set by the Dutch Partnership Overweight (Dutch: PON), an advisory body for the Dutch government on obesity related health issues. We categorized the outcomes on weight: 5% weight loss or more, between 0 and 5% weight loss, weight stabilization and weight gain, to map the percentage of participants that comply with this target.
Subgroup analyses
We compared different subgroups in sequence to explore potential differences in outcomes, i.e. subgroups based on educational level of the participants, on BMI at baseline and on group size at the start of CooL. Subgroup analyses were done on the full dataset (A) including program finishers and dropouts. To enable subgroup comparison, we calculated the difference (delta) between T0 and T2 for each construct or variable. As a higher starting weight usually requires less effort to lose a certain amount of weight, we looked at relative (%) weight loss compared to baseline for the BMI-subgroup comparison. For the construct ‘eating pattern’ we used the construct itself as it already includes changes in eating pattern compared to baseline in the formulation of the questions. When comparing two subgroups we performed independent t-tests comparing all delta-variables. In case of multiple subgroups, we ran an ANOVA test on the delta-variables followed by post-hoc Tukey tests to analyze potential differences in effect.
Drop-outs
We used logistic regression analysis to determine the main factors related to drop-out. The predictor variables in the logistic regression were based on the pre-defined subgroups of interest (i.e. based on group size, BMI at baseline and educational level) and two additional demographic variables (i.e. age category and gender). For the dropout analysis we used the full dataset (A) excluding the participants (n = 22) that could not be assigned as program finisher or dropout due to missing information.
The dropout analysis showed no distinct pattern in dropout profiles. However, specific subcategories of some of the constructs were less likely to drop out in comparison to the reference category, i.e. a BMI of 35–40 compared to BMI < 30, participating in a group of over 10 compared to less than 10 and a higher level of education compared to a lower level of education all were less likely to drop out. The constructs gender and age showed no differences in dropout. See Additional File 1 for the details on dropout percentages and related analyses.
As CooL is part of basic health insurance and data is gathered from all participants, provided that they gave written consent for the use of their anonymized data, selection bias is limited. In addition, we tried to minimize bias by ensuring a check on all analyses by a second researcher, by including both program finishers and dropouts in our analyses and by presenting a complete set of outcomes on all variables and analyses.
Ethics
This study was submitted to and approved by the Research Ethics Committee of the Faculty of Health, Medicine and Life Sciences of Maastricht University (FHML-REC/2019/073). All participants gave their written informed consent for their anonymized personal data to be used for research purposes. Data retrieved prior to 2019 fell in scope of the CooL pilot project which was submitted to the Medical Research Ethics Committee of Maastricht University (METC 14-5-021) and qualified by this Committee as exempt from review, as it does not fall within the scope of the Dutch Medical Research Involving Human Subjects Act (Central Committee on Research Involving Human Subjects, 2015). All participants signed an informed consent prior to starting with CooL.
Results
Datasets
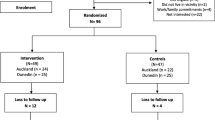
We collected data from in total 3780 participants that started CooL between November 2018 and December 2021. See Fig. 1 for a graphical representation of the dataset selection steps.
Demographics
Of all participants in the full dataset (A, n = 746) a total of 28% were male and 72% female. This ratio is in line with the data from the national CLI-monitor [35]. Most participants (93%) had a Dutch background. In total, 69% of the participants had a lower or intermediate level of education; 30% did not have a steady job (anymore) and approximately two third of the participants were living together with a partner (see Table 1).
The cleaned dataset (B, n = 396), containing only respondents that finished the intervention, showed in general a similar demographic picture except for the educational level of the participants: this dataset contained relatively more participants with a higher-level education and less participants with a lower-level education.
All results on the anthropometric and personal factors in the full dataset (A) are summarized in Table 2 whereas more detailed information is provided in additional file 2
Anthropometrics
The anthropometric measurements, i.e. weight, BMI and waist circumference, all showed a medium effect size in the desired direction at T1 increasing slightly at T2. Participants showed on average a decrease of 4.1 kg weight, 1.4 BMI point and 4.4 cm waist circumference after two years of CooL.
Three quarters of all participants showed weight loss during 24 months of CooL and 32% of all participants showed more than 5% weight loss. On average participants lost 3.8% weight during these 24 months.
The CooL finishers (dataset B) showed slightly better outcomes at T2, i.e. an average weight loss of 4.7 kg, a decrease of 1.6 BMI point and a decline of 5.5 cm in waist circumference at T2 (all large effect sizes).
Personal factors and feeling fit
Participants experienced an increased feeling of self-mastery at T2 (small effect size) and an improvement in perceived health both at T1 and T2 (large effect size). Feeling fit when waking up, showed an improvement with a small effect size both at T1 and T2 whereas feeling fit during the day showed no effect at T1 and a small effect size at T2. No effect was found on perceived support and influence of stress on daily functioning both at T1 and T2 compared to baseline.
The CooL finishers (dataset B) showed similar effects and effect sizes.
Behavioral factors
No effect was found at T1 for sedentary time (both least and most active days) and a small effect was found at T2: participants spent around half an hour less time on sitting both on least and most active days. Physical activity showed a small effect size both at T1 and T2 with an average increase of 18 min at T2. The outcomes on sleep showed that participants experienced a higher quality of sleep at T1 and T2, both with a small effect size. In addition, participants experienced less stress at T1 and T2 (both medium effect size) and participants smoked less at T1 and T2 (small effect size).
The dietary outcomes showed that participants paid more attention to meal composition and to the amount of food they consume compared to baseline, both constructs showed a large effect size at T1 and T2. In addition, participants were more attentive during actual consumption of food both at T1 and T2 (both medium effect size). When drinking alcohol, participants consumed on average one unit less alcohol at T1 (small effect size) and this effect was sustained until T2 (small effect size).
Regarding change in eating pattern compared to baseline, participants indicated an improvement at T2 compared to T1 with a small effect size.
The CooL finishers (dataset B) showed deviating outcomes on physical activity (no effect at T1) and smoking (no effect at T1 or T2).
Subgroup analyses
We compared subgroups based on the categorization of different constructs, i.e. educational level, BMI at baseline and group size at the start of the two-year CooL-intervention. All subgroup analyses were done on the full dataset (A).
Subgroup: educational level
Comparing participants with a lower level of education (LLE) to an intermediate or higher level of education (IHLE) showed in general no differences in effects. The only difference between both subgroups was found in active minutes. Participants with a lower level of education showed a larger increase from baseline to T2: 49 min of increased physical activity compared to 7 min for participants with a medium to higher level of education. See Tables 2 and 3 for the p-values on the subgroup comparison on educational level and additional file 3 for more detailed outcomes of the subgroup analysis.
Subgroup: BMI at baseline
For most constructs no differences in effects were observed between participants of different BMI-categories. The comparison showed differences only on change in BMI, percentage weight loss and meal composition between T0 and T2. See Tables 2 and 3 for the p-values on the subgroup comparison on BMI-category and additional file 4 for more detailed outcomes of the subgroup analysis. Looking into more detail, these differences were found for a limited number of categories (see additional file 4, table b).
The outcomes for participants with a larger BMI at baseline showed equal effect sizes on most constructs and better outcomes on weight loss percentage/BMI. The only exception was the attentiveness to meal composition: participants with a BMI < 30 at baseline showed more improvement on this construct compared to participants with a BMI 40+.
Subgroup: Group size at baseline
A comparison between the outcomes of participants that start in small groups (group size < 10) versus large groups (group size 10+) showed similar results. Only for two constructs differences were observed, i.e. the influence of stress on daily functioning (Table 2) and the number of daily active minutes (Table 3). For participants in smaller groups (< 10) the influence of stress on daily functioning showed an increase at T2 compared to baseline (i.e. a more positive influence of stress on daily functioning) whereas for participants in larger groups (10+) the influence of stress showed a decrease at T2 (i.e. a more negative influence). For participants in smaller groups the physical active minutes increased on average at T2 with 38 min whereas for participants in larger groups the physical active minutes increased with 9 min compared to baseline. See additional file 5 for more detailed outcomes of the subgroup analysis on group sizes.
Discussion
The study results indicated positive changes in all measured values at 24 months compared to baseline. The largest effect sizes were observed in perceived health, attentiveness to meal size and meal composition (large). Weight loss/BMI and waist circumference had medium to large effect sizes. Medium effect sizes were noted for attentiveness to consuming food, alcohol intake and stress perception. The remaining behaviors showed small effect sizes with very few outcomes showing no effect.
Looking at changes in the timeframe of baseline to 8 months, the pattern is similar to the outcomes from previous CooL-research [11]. In addition, the present study showed sustained and improved results in CooL-participants, including enlarged weight loss over the full term of 24 months, even though they were exposed to the COVID-19 pandemic and restrictions. Durable weight loss (i.e. weight maintenance) can be defined as intentional weight loss that has been maintained for at least 6 months [36]. In general, initial weight loss is considered relatively easy whereas the opposite is true for durable weight loss. Follow-up measurements of lifestyle programs usually report weight regain compared to baseline after one year [8, 13,14,15] underlining the importance of the 24 months duration of CooL with a continued focus on behavior change and behavior maintenance in phase 2 of the program.
Despite the on average positive outcomes of CooL, the individual outcomes show quite some variation, pointing out that CooL is not necessarily a good match for all individuals. A clearer picture on the characteristics and contexts of high-performing versus low-performing participants might provide clues for improvements in the intervention and the inclusion policy of eligible candidates for CooL.
The results of the full dataset compared to the cleaned dataset were quite similar, indicating limited selective dropout. Participants that finished CooL show in broad terms slightly improved outcomes compared to the participants in the full dataset, probably because, on average, dropouts participated 11 months in CooL, whereas participants that finished CooL received additional months of guidance and support. In addition, the dropout-group consisted of participants with a range of results on both ends: participants with such positive results early in the program needing no further assistance in behavior maintenance and participants with such negative or less encouraging results wishing no longer to continue the intervention. These results on both ends of the spectrum, seem a reasonable explanation for the average result on the dropout group in total.
Despite the cut-off date that was applied to balance the dropouts in the dataset, the number of dropouts was still relatively high compared to earlier research on CooL [37]. As we suspected the COVID-19 pandemic and its restrictions to have a major influence on dropout rates, a quick analysis on the monthly dropouts from June 2019 until June 2021 showed that dropouts more than doubled when restrictions resulting from the COVID-19 pandemic came into effect starting March 2020.
Although the group of lower educated was somewhat overrepresented in the dropout group, the educational level did not seem to interfere with the achieved effects as participants with a lower level of education showed identical effects in outcomes as participants with higher educational levels. This finding is not in line with our hypothesis, stating that participants with a lower level of education show smaller changes over time, but it is similar to the outcomes of comparable health interventions [16, 17]. Tentatively, the present study provides indications that CooL does not enlarge health inequalities and even shows potential to decrease these inequalities, under the conditions that participants with a lower level of education can be guided to the intervention and towards sustained participation in CooL. Apparently, once the participant with a lower level of education has made the choice to start with the CooL-intervention, the open nature of CooL provides enough flexibility for the CooL-coach to fit the intervention to the needs of these participants. Physical active minutes provided the only exception, in the range of similar outcomes, as participants with a lower level of education showed a larger increase despite more physical active minutes at baseline, which might be due to a confusing question on (bouts of) active minutes generating a mix of active minutes or bouts of 10 min.
Participants with a lower level of education were more likely to dropout during CooL which is in line with a higher dropout rate of MetSLIM, a CLI for low SES, compared to the regular SLIMMER CLI [16] and with earlier findings illustrating that higher education serves as a protective factor against dropout [38]. In conclusion, CooL is just as effective for participants with a lower level of education, though extra effort is needed to prevent dropout for this target group.
The outcomes for participants with a larger BMI at baseline showed equal effect sizes on most constructs and even better outcomes on weight loss/BMI with attentiveness to meal composition as the only exception. These outcomes indicate that the CooL-intervention is appropriate and effective for all BMI-categories. This finding is in line with earlier research showing equal effects for different BMI-categories [24] and at the same time feeds the desire to analyze the impact of BMI at baseline to the program adherence of CooL, as these differences were indicated in earlier research [22].
When comparing the outcomes of participants in small groups versus large groups, the similarities stand out, as only differences were found on the impact of stress on daily functioning and on physical active minutes, both in favor of a smaller group size possibly related to the enhancement of participation and satisfaction within a small group [25]. However, a smaller group size is related to more dropouts, potentially due to the fact that a larger group size increases the chance of finding a suitable buddy or role model among the group as group participants and CooL-coach stay together from start to end. A larger CooL-group may provide more diversity and increases active participation in line with Lohman [26]. These findings leave the ideal group size for CooL undecided leaving room for the CooL-coach to act on personal preferences as an extra group member provides more income but requires extra effort in individual support and group dynamics.
Limitations and strengths
A control group for comparison was no option, as the CLI CooL is part of basic health care in the Netherlands. Therefore, the results of CooL should be labelled as changes over time instead of effects as we cannot rule out interference with other factors and variables. We are less hesitant in addressing these changes to CooL given the average effect size of the changes, previous results of CooL and the comparison to similar interventions.
During the time of the study the questionnaire was revised with minor changes. We intended to keep the line of questioning and answering the same, but we cannot rule out any effect on the study. The impact of COVID-19 on the intervention, coaches and participants can be considered a second limitation though the results of the CooL-intervention on participants during COVID-19 are substantial and encouraging [11].
We cannot distinguish between dropouts and loss to follow-up as we are dependent on the respondents to hand-over their results. As a consequence, we cannot provide exact numbers on participants and dropouts of CooL. We compared the cleaned dataset with the full dataset, the latter including dropouts. The comparison is insightful but does not support firm conclusions on the (missing) effects of dropouts.
Conversely, there are several strengths to this study. This is the first study with a two-year follow-up measurement in participants of CooL: the outcomes in the long run, the nationwide inclusion and the broad scope of the research provide valuable insights on the long-term effects of CooL. In addition, the study is based on data provided by people that participate in CooL in a real-life setting. As CooL is part of basic health care insurance, it is accessible to everybody meeting the criteria and the outcomes are generalizable to those participating in real life. Another strength is the open nature of the CooL-intervention as it provides flexibility for the coaches to adapt the program to the target group and context, enabling a fit with a variety of target groups. On the other hand, this calls upon the knowledge and skills of the coach to adapt the program but still secure the identity of the intervention by ensuring the program includes the essential active elements and facilitates the realization of the end goals for the participants.’
Recommendations for future research
This research provides an overview of the changes over a two-year time frame of the participants of CooL, showing more and less expected outcomes. Our recommendations for future research seize on these current outcomes:
-
More research on the two-year follow-up of CLIs in the Netherlands.
-
More research into the optimal group size for health interventions, in support of explicit guidelines for the healthcare workers.
-
In-depth research into dropouts of the CLI, providing an overview of risk factors for dropout as well as recommendations to prevent dropout.
-
Research into the qualifications and characteristics of CooL-coaches comparing high-performers to medium or low-performers.
-
Research into the characteristics and contexts of high-performing versus low-performing participants.
Conclusion
The effects of CooL on its participants show sustained and even enlarged weight loss when comparing phase 1 to phase 2 of CooL. This supports the two-year set-up of CooL with frequent contact moments and more attention for behavioral maintenance in the second part of the intervention. Although CooL is not a one-size-fits all intervention for each individual, CooL seems appropriate and effective for different group sizes and for participants varying in of BMI and educational level, indicating that the open nature of the intervention matches its intention.
Data availability
The datasets generated and/or analysed during the current study are not publicly available. The raw data used for the research on CooL contains privacy-sensitive information on anthropometrics, perceptions and behaviors. CooL-participants sign an informed consent in which they grant access to their (anonymized) data for research purposes concerning evaluation, effect studies and further development of the CooL-intervention. In case a request to the corresponding author matches aforementioned purposes, the request will be qualified as reasonable and access to the raw data will be provided. Data retrieved prior to 2019 fell in scope of the CooL pilot project which was submitted to the Medical Research Ethics Committee of Maastricht University (METC 14-5-021) and qualified by this Committee as exempt from review, as it does not fall within the scope of the Dutch Medical Research Involving Human Subjects Act (Central Committee on Research Involving Human Subjects, 2015). All participants signed an informed consent prior to starting with CooL.
Abbreviations
- ΔT0T1:
-
delta T0T1, timeframe between T0 (baseline) and T1
- ΔT0T2:
-
delta T0T2, timeframe between T0 (baseline) and T2
- ANOVA:
-
analysis of variance
- BLCN:
-
Beroepsvereniging Leefstijlcoaches Nederland
- BMI:
-
Body Mass Index
- CBS:
-
Central Bureau of Statistics
- CLI:
-
Combined Lifestyle Intervention
- CooL:
-
Coaching op Leefstijl
- COVID-19:
-
Corona virus disease 19
- IHLE:
-
intermediate to higher level of eduation
- LLE:
-
lower level of education
- NHG:
-
Nederlands Huisarts Genootschap
- PON:
-
Partnerschap Overgewicht Nederland
- PSQI:
-
Pittsburgh Sleep Quality Index
- P-value:
-
probability value
- RIVM:
-
Rijksinstituut voor Volksgezondheid en Milieu
- SD:
-
standard deviation
- SPSS:
-
Statistical Package for the Social Sciences
- WHO:
-
World Health Organisation
References
James WPT. WHO recognition of the global obesity epidemic. Int J Obes. 2008;32(7):S120–6.
Overgewicht en obesitas. Den Haag: Gezondheidsraad 2003.
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–9.
Taylor VHAPMDP, Forhan MAPP, Vigod SNAPMD, McIntyre RSPMD, Morrison KMAPMD. The impact of obesity on quality of life. Best Pract Res Clin Endocrinol Metab. 2013;27(2):139–46.
How many adults are overweight? The Hague. Central Bureau of Statistics; 2022 [ https://longreads.cbs.nl/nederland-in-cijfers-2022/hoeveel-volwassenen-hebben-overgewicht/
Organization WH. Factsheet Obesity and overweight 2021 [updated 09-06-2021. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
Bos V, van Dale D, Leenaars K. Werkzame Elementen Van Gecombineerde Leefstijlinterventies. Rijksinstituut voor Volksgezondheid en Milieu; 2019.
Duijzer G, Haveman-Nies A, Jansen SC, Beek JT, van Bruggen R, Willink MGJ, et al. Effect and maintenance of the SLIMMER diabetes prevention lifestyle intervention in Dutch primary healthcare: a randomised controlled trial. Nutr Diabetes. 2017;7(5):e268.
Schutte BA, Haveman-Nies A, Preller L. One-year results of the BeweegKuur Lifestyle intervention implemented in Dutch primary Healthcare settings. Biomed Res Int. 2015;2015:484823.
Obesity and overweight: World Health Organization (WHO). 2021, June 9. [cited 2023 January 24]. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
Janssen E, Philippens N, Kremers S, Crutzen R. The combined lifestyle intervention CooL in times of COVID-19: a descriptive case series study. 2023.
Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the look AHEAD trial. Arch Intern Med. 2010;170(17):1566–75.
Skender ML, Goodrick GK, Del Junco DJ, Reeves RS, Darnell L, Gotto AM, et al. Comparison of 2-year weight loss trends in behavioral treatments of obesity: diet, exercise, and combination interventions. J Am Diet Assoc. 1996;96(4):342–6.
Jehn ML, Patt MR, Appel LJ, Miller ER 3. One year follow-up of overweight and obese hypertensive adults following intensive lifestyle therapy. J Hum Nutr Diet. 2006;19(5):349–54.
Lindström J, Louheranta A, Mannelin M, Rastas M, Salminen V, Eriksson J, et al. The Finnish diabetes Prevention Study (DPS): lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care. 2003;26(12):3230–6.
Bukman AJ, Teuscher D, Meershoek A, Renes RJ, van Baak MA, Feskens EJ. Effectiveness of the MetSLIM lifestyle intervention targeting individuals of low socio-economic status and different ethnic origins with elevated waist-to-height ratio. Public Health Nutr. 2017;20(14):2617–28.
Wikström K, Peltonen M, Eriksson JG, Aunola S, Ilanne-Parikka P, Keinänen-Kiukaanniemi S, et al. Educational attainment and effectiveness of lifestyle intervention in the Finnish diabetes Prevention Study. Diabetes Res Clin Pract. 2009;86(1):e1–5.
Wardle J, Steptoe A. Socioeconomic differences in attitudes and beliefs about healthy lifestyles. J Epidemiol Community Health. 2003;57(6):440–3.
Liu Y-B, Liu L, Li Y-F, Chen Y-L. Relationship between Health Literacy, Health-related behaviors and Health Status: a Survey of Elderly Chinese. Int J Environ Res Public Health. 2015;12(8):9714–25.
van der Heide I, Uiters E, Rademakers J, Struijs JN, Schuit AJ, Baan CA. Associations among Health Literacy, diabetes knowledge, and self-management behavior in adults with diabetes: results of a Dutch cross-sectional study. J Health Communication. 2014;19(sup2):115–31.
Kim S, Love F, Quistberg DA, Shea J. Association of Health Literacy with self-management behavior in patients with diabetes. Diabetes Care. 2005;27:2980–2.
Burgess E, Hassmén P, Pumpa KL. Determinants of adherence to lifestyle intervention in adults with obesity: a systematic review. Clin Obes. 2017;7(3):123–35.
Moore CJ, Cunningham SA. Social position, psychological stress, and obesity: a systematic review. J Acad Nutr Diet. 2012;112(4):518–26.
Barte JC, Veldwijk J, Teixeira PJ, Sacks FM, Bemelmans WJ. Differences in weight loss across different BMI classes: a meta-analysis of the effects of interventions with diet and exercise. Int J Behav Med. 2014;21(5):784–93.
Kooloos JGM, Klaassen T, Vereijken M, Van Kuppeveld S, Bolhuis S, Vorstenbosch M. Collaborative group work: effects of group size and assignment structure on learning gain, student satisfaction and perceived participation. Med Teach. 2011;33(12):983–8.
Lohman MC, Finkelstein M. Designing groups in problem-based learning to promote problem-solving skill and self-directedness. Instr Sci. 2000;28:291–307.
The Diabetes Prevention Program (DPP). Description of lifestyle intervention. Diabetes Care. 2002;25(12):2165–71.
Wadden TA, West DS, Delahanty L, Jakicic J, Rejeski J, Williamson D, et al. The look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obes (Silver Spring). 2006;14(5):737–52.
Protocol, BMI en middelomtrek meten. : Nederlands Huisartsen Genootschap 2016 [cited 2023 January 12]. https://www.cvrmindehuisartsenpraktijk.nl/downloads
Eklund M, Erlandsson L-K, Hagell P. Psychometric properties of a Swedish version of the Pearlin Mastery Scale in people with mental illness and healthy people. Nord J Psychiatry. 2012;66(6):380–8.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Cohen S, Kamarck T, Mermelstein R. A Global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96.
Crutzen R, Peters G-JY. Scale quality: alpha is an inadequate estimate and factor-analytic evidence is needed first of all. Health Psychol Rev. 2017;11(3):242–7.
Lipsey MW. Design sensitivity: statistical power for experimental research. Newbury Park, CA: Sage; 1990.
Oosterhoff M, de Weerdt A, Feenstra T, de Wit A. Jaarrapportage monitor GLI 2022. Stand van zaken gecombineerde leefstijlinterventie. Annual report – Monitor Combined lifestyle intervention 2022 Combined lifestyle intervention progress report: Rijksinstituut voor Volksgezondheid en Milieu RIVM; 2022.
Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6(1):67–85.
van Rinsum C, Gerards S, Rutten G, Philippens N, Janssen E, Winkens B et al. The Coaching on Lifestyle (CooL) Intervention for Overweight and Obesity: A Longitudinal Study into Participants’ Lifestyle Changes. Int J Environ Res Public Health. 2018;15(4).
Moroshko I, Brennan L, O’Brien P. Predictors of dropout in weight loss interventions: a systematic review of the literature. Obes Rev. 2011;12(11):912–34.
Acknowledgements
The authors like to thank the CooL-coaches and the CooL-participants for their efforts to make this research possible.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conceptualization, N.P., E.J., R.C. and S.K.; Methodology, N.P., E.J., R.C. and S.K.; Validation, R.C. and S.K.; Formal Analysis, N.P., E.J. and R.C; Investigation, N.P. and E.J.; Data Curation, N.P. and E.J.; Writing—Original Draft Preparation, N.P. and E.J.; Writing—Review and Editing R.C., and S.K.; Visualization, N.P. and E.J.; Funding Acquisition, not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was submitted to and approved by the Research Ethics Committee of the Faculty of Health, Medicine and Life Sciences of Maastricht University (FHML-REC/2019/073). All participants gave their written informed consent for their anonymized personal data to be used for research purposes. All participants in CooL are adults except one minor who started the intervention at the age of 16. In the Netherlands adolescents from the age of 16, have the legal right to decide for themselves on medical treatments as they have the same patient rights as adults.
Consent for publication
Not applicable.
Competing interests
Not applicable for S.K. and R.C. Both main authors (E.J. and N.P.) are co-owner of the CooL-intervention.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Philippens, N., Janssen, E., Kremers, S. et al. Keep it CooL! Results of a two-year CooL-intervention: a descriptive case series study. BMC Public Health 24, 2138 (2024). https://doi.org/10.1186/s12889-024-19661-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19661-w