Abstract
Background
Health-seeking behavior (HSB) involves any action or inaction taken by individuals who perceive themselves to have a health problem or illness aimed at finding appropriate medical treatments. Studies suggest a positive relationship between the availability and quality of health services and their utilization. This study aimed to identify the factors influencing health-seeking behavior among Sudanese immigrants in Saudi Arabia, to improve healthcare access and health outcomes.
Method
A cross-sectional study was conducted targeting Sudanese residents of the Kingdom of Saudi Arabia (KSA). Participants were recruited using convenient sampling. A self-administered questionnaire was distributed electronically. A total of 494 participants were recruited for the study.
Results
This study showed that the majority of the participants (66.6%) visited a primary healthcare center when faced with a medical problem. However, the prevalence of self-medication in the past three months was 45.7%. Significant factors influencing health-seeking behavior included age (OR [95% CI]: 1.032 [1.000-1.066]) and lack of health insurance (OR = 1.01, 95% CI [1.00-1.02], p = 0.019).
Conclusions
This study emphasizes the importance of understanding healthcare-seeking behavior among immigrant groups, particularly Sudanese immigrants in Saudi Arabia. It highlights the significance of insurance as a determinant of healthcare-seeking behavior and calls for reforming current policies to reduce disparities in accessing healthcare services.
Similar content being viewed by others
Background
Health-seeking behavior (HSB) refers to actions taken by individuals when they perceive a health problem or illness, aiming to find an appropriate treatment option [1]. HSB is initiated by a decision-making process that is influenced by individual and/or familial behavior, community standards and norms, and provider-related features and behavior [2]. Various studies demonstrated that socioeconomic status, sex, age, social standing, type of disease, access to resources, and perceived quality of care all influence the decision to engage with a specific medical channel [3, 4]. This behavior, on an aggregate and global scale, has the potential to organize and strongly influence the demand for healthcare services [5].
Access to and use of treatment services are considered fundamental rights. Studies suggest that there is a positive relationship between the availability and quality of health services and their utilization [6,7,8,9]. However, inequalities in access to these services have been observed, indicating that patients from lower socioeconomic backgrounds, and certain nationalities and minority groups, benefit less from these services [10].
Migration defined as the movement of people across borders or within a country, presents additional challenges [11]. According to recent International Organization of Migration (IOM), there were approximately 281 million international migrants worldwide in 2020 [12]. These individuals face new social, economic, and political conditions in their host countries impacting their HSB. In particular, labor migration is associated with high stress levels, poor working conditions, and poor psychological and physical health [13]. Moreover, there is consistent evidence that immigrant groups face prejudice and have limited access to healthcare as seen in the Arab Gulf countries, where Immigrants community has less access to healthcare [14]. In Saudi Arabia, Immigrants are particularly socially disadvantaged because of their low average income and lack of knowledge local resources, struggle to access necessary health services [15].
The IOM classifies Sudan as a country with active migration movements both internally and internationally [16] In recent years, Sudanese migrants have primarily sought asylum in the oil-rich Gulf Arab countries [17]. According to official census data, there are 819,600 Sudanese migrants in Saudi Arabia, constituting 6.1% of the migrant population [18]. The ongoing war in Sudan has further exacerbated migration with over 1 million people fleeing the country into neighboring countries. If this conflict continues, it is estimated that almost 2 million refugees and migrants will be affected by the crisis [16, 17].
Sudanese immigrants face unique challenges accessing healthcare in Saudi Arabia. Cultural differences and lack of knowledge of the healthcare system are some of the barriers that can prevent them from seeking medical care. While most research on on immigrant health have focused on Western countries [19], there is a need to understand the unique challenges faced by immigrants in non-Western contexts.
The United Nation’s (UN’s) Sustainable Development Goal (SDG) 3.8, aims to “Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.” [20] However, immigrants tend to underutilize the healthcare services that are offered due to exclusion from local health systems [21,22,23]. Understanding the HSB of migrants can help achieve universal health coverage and meet SDG targets.
This study aims to identify the factors influencing health-seeking behavior among Sudanese immigrants in Saudi Arabia. By understanding these factors, policymakers and healthcare providers can develop targeted interventions to improve access to healthcare services for this population. This, in turn, can help reduce disparities in healthcare access and outcomes among Sudanese immigrants and move towards achieving universal healthcare coverage for all individuals, regardless of their nationality or immigration status.
Additionally, by promoting culturally sensitive healthcare interventions based on the findings of this study, healthcare providers can improve the overall quality of care provided to Sudanese immigrants in Saudi Arabia. This can lead to better health outcomes, increased trust in the healthcare system, and ultimately contribute to the goal of universal healthcare by ensuring that all individuals receive high-quality, equitable healthcare services.
This study fills a critical gap in the existing literature as it represents the first attempt to investigate HSB among Sudanese immigrants in Saudi Arabia. By focusing specifically on this demographic group, the research aims to provide a nuanced understanding of the unique factors influencing their healthcare utilization patterns. This approach is essential for developing culturally sensitive and tailored interventions that effectively address the healthcare needs of Sudanese immigrants in Saudi Arabia. Furthermore, the findings of this study can contribute to the broader body of knowledge on migrant health and serve as a foundation for future research in this underexplored area.
Overall, this study has the potential to inform policy decisions and healthcare practices that can help advance progress towards universal healthcare coverage, aligning with the global commitment to ensure health for all and leaving no one behind.
Methods
Study design and population
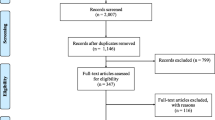
A community-based cross-sectional study was conducted using an online population survey. Participants were recruited using convenient sampling. Eligibility criteria included male and female Sudanese immigrants ≥ 18 years of age, residing in the Kingdom of Saudia Arabia (KSA) on a residence visa, at the time of the study. The exclusion criteria were Sudanese immigrants on a visiting visas, those coming for religious rites (Haj or Umrah), and individuals < 18 years of age. Data collection occurred between August 1st to September 1st, 2023. A total of 530 responses were collected during the study period. After excluding respondents with visiting visas, a total of 494 participants were included for analysis.
Data collection tools
A self-administered questionnaire was developed in Arabic using Google Forms. The questionnaire was reviewed and refined by two public health experts( S.A and E.M). A pilot study involving, 30 participants was conducted to test the questionnaire, and newcessary adjustments were made. The final questionnaire consisted of two parts: the first section captured demographic information, the length of residency in the KSA, and the health insurance status. The second section assessed the participants’ HSB and consisted of four questions. The first question asked about the first action taken after encountering a health problem, and the following three questions evaluated self-medication behavior.
Data collection method
The questionnaire was distributed electronically through Sudanese social groups on social media platforms such as Facebook and WhatsApp. This approach facilitated the efficient dissemination of the survey among the target population. Efforts were made to ensure a representative sample, by distributing the survey through multiple groups with diverse demographics in terms of age, sex, and occupation.
Data analysis
Data analysis was conducted using SPSS (version 26.0). Frequencies and percentages, were calculated to summarize categorical variables such as the participants demographics (age, sex, martial status, duration of residency, health insurance status) and HSB (initial action taken when encountering a health problem and self medication practices). Chi-square analysis was performed to determine any correlations between sociodemographic variables andhealth-seeking behavior. To identify significant predictors of health-seeking behavior, logistic regression analysis was performed. Variables found to be significant in the chi-square tests were included in the logistic regression model. The model provided odds ratios (OR) with 95% confidence intervals (CI) to quantify the strength of associations between predictor variables and the likelihood of positive HSB. The Hosmer and Lemeshow goodness-of-fit test assessed the model fit, with a p-value greater than 0.05 indicating an acceptable fit. A P value of ≤ 0.05 was considered significant.
Results
During the study period, a total of 494 participants were recruited. The majority of participants were males (86.6%), with a mean age of 36.5 years (+/- 9.25 years). Most participants were employed in the private sector (71.7%) and reported an average monthly income of 4467 Saudi Arabian Riyal (SAR) (+/- 4097 SAR). Nearly half of the respondents (44.1%) had no insurance or only informal insurance. Additionally, 20.3% of participants reported having a chronic disease, with hypertension (10.5%) or diabetes mellitus (7.9%) being the most common conditions (Table 1).
Health-seeking behaviour
Table 2 shows the first action taken by the respondents when they were confronted with health issues. The initial actions taken by participants when confronted with a health issue varied. The majority of respondents reported visiting a primary healthcare center (PHC), while only 3.4% taking a drug without a prescription. A total of 11.3% would self-diagnose using the internet, 10.7% claimed they would consult an acquainted doctor, and only 7.9% would consult a pharmacist.
Self-medication practices
Approximately half of the respondents (54.3%) denied taking any drugs without a doctor’s prescription in the last 3 months. Among those who engage in self-medication21.5% did so once, 10.1% twice, 5.5% three times, and 8.7% more than three times in the last three months (Table 3). Moreover, participants also cited various bases for their self-medication in the past three months: doctor’s orders (63.8%), previous experience (45.5%), advice from friends or relatives (16.2%), and information found on the internet (21.2%) (Table 4).
Factors influencing health-seeking behavior
Chi-squared test revealed significant associations between HSBs and several sociodemographic variables. Significant associations were found for age (χ2 (4, n = 494) = 16.148, p = 0.003), marital status [χ2 (1, n = 494) = 11.657, p = 0.001], duration of residency in Saudi Arabia [χ2 (3, n = 494) = 18.956, p < 0.001] and health insurance status [χ2 (6, n = 488) = 23.382, p = 0.001]. However, no significant associations were found between HSB and variables such as sex, occupation, monthly income, level of education, or the presence of a chronic disease, as shown in Table 5.
A logistic regression model further identified age and health insurance as significant predictors of HSB. The logistic regression model was statistically significant, χ2 (1 1, n = 494) = 42.820, p < 0.001, explaining 12.1% (Nagelkerke R2) of the variance in health-seeking behavior, and it correctly classified 69.4% cases. The Hosmer and Lameshow goodness of fit test indicated an acceptable fit (p = 0.366). Out of the 4 variables we entered into the logistic regression model, only age (OR [95% CI]: 1.032 [1.000-1.066]) and lack of health insurance (OR = 1.01, 95% CI [1.00-1.02], p = 0.019) were found to be significant predictors of HSB, as shown in Table 6. In contrast the duration of residency and marital status did not show significant associations with HSB.
Discussion
This study provides the first comprehensive analysis of health-seeking behavior among Sudanese immigrants in Saudi Arabia. Our findings demonstrate that age and health insurance status are significant predictors of HSB, with older participants and those with health insurance being more likely to seek appropriate medical care. We found a 66.6% rate of positive HSB. These results align with those of other studies performed in Malaysia (66.7%), Nigeria (63%) and India (74.6%) [24,25,26].
Insurance
Prior research indicates that health insurance lowers the cost of hospital stays and medication, allowing people to receive better medical care while treating various illnesses [27, 28]. However, other studies have demonstrated that insurance does not significantly increase the use of health services, particularly in situations where individuals still receive high-quality care even without insurance [29]. Nonetheless, the positive effect of insurance is more pronounced in marginalized populations [30].
This study revealed a strong association between health insurance status and health-seeking behavior. In this study, almost half of the participants (43.7%) had no or informal health insurance. This percentage is higher than that reported in a wider-scale study by Alkhamis et al., 2017, conducted on immigrants in Saudi Arabia, which found that only 30% were uninsured [15]. However, this discrepancy may be due to differences in demographics, as the study by Alkhamis et al., 2017, primarily included only males, non-Arab workers and did not specify the number of Sudanese participants.
Informal insurance is often considered as a way for companies and employers to evade authorities without providing workers with proper health insurance coverage. According to Saudi Arabian Labor Law, employers must bear the responsibility for paying all necessary medical expenses for their immigrant employees [31], yet many immigrant workers and their families remain uninsured.
The relationship between health insurance coverage and health-seeking behavior was corroborated by a similar study on Saudi and non-Saudi nationals in KSA. This study found that having health insurance increased the likelihood of attending a medical check-ups by approximately 13% among Saudi Arabians and 20% among non-Saudi [30]. These findings are consistent with a qualitative study on low-income Bangladeshi migrant workers in the United Arab Emirates, where participants cited insurance structures as barriers to achieving good health care [13].
AGE
The positive association between age and HSB indicates that older Sudanese immigrants are more likely to seek appropriate healthcare when faced with medical issues. This could be attributed to greater health awareness and the higher prevalence of chronic disease among older individuals, necessitating more frequent interactions with healthcare providers. In addition, older Sudanese immigrants are more likely experts in their professions and have better access to higher categories of health insurance. This positive association was similarly described in a study in Senegal that found an increase in the odds of seeking healthcare among people older than 40 years [9], contradicting the findings of another study conducted in Iran that revealed an inverse relationship between age and appropriate HSB, where older people were less likely to seek healthcare [10]. The practical implications of these findings suggest a need for targeted health education campaigns aimed at younger immigrants to promote proactive HSBs and early intervention. These campaigns could focus on raising awareness about the importance of regular medical check-ups and managing chronic conditions to improve overall health outcomes.
Monthly income
Although the association with insurance was significant, monthly income was not. This is contrary to the belief that better income will instantly mean better access to healthcare and affordability of health services. However, this finding aligns with that of another study that was conducted on both Saudi Arabian and non-Saudi Arabians in Al-Ahsa, which found that perceived economic status, rather than actual monthly income, significantly influenced HSB [32].
We believe that the immigration status of our participants may have influenced these results. Unlike Saudi Arabian citizens, non-Saudi Arabian citizens do not have access to free medical care in governmental facilities. Consequently, immigrants must obtain either health insurance or, if uninsured cover medical cost through out-of-pocket payments to receive medical care [30]. Nonetheless, the average monthly income for Saudi Arabians is approximately 10,000 SAR, and 94.5% of our participants had a monthly income below this average (4500 SAR). This disparity suggest that even a modest increase in monthly income for immigrants do not substantially impact their healthcare decisions of compared to the availability of insurance, which provides significantly more affordable healthcare services, even at its most basic levels. Therefore, enhancing health insurance coverage for expatriates may be a more effective strategy to improve healthcare access than merely increasing income levels.
Negative HSB
Despite a relatively high percentage of positive HSB in our sample, 45.7% of the participants practiced self-medication without a doctor’s prescription. This is a high percentage compared to that in other countries such as Malaysia (11.8%) [24]. However, it is considerably lower than the rate in Sudan. A recent study by Isameldin et al., 2020, reported the prevalence of self-medication In Sudan was 100% [33]. Another study assessed self-medication with antibiotics in Sudan and reported a rate of 87% [34]. These findings highlights the importance of healthcare system affordability and health insurance in promoting positive HSB, as well as the necessity for strict regulations to prevent pharmacists from dispensing medication without prescriptions.
Unexpectedly, very few of our participants reported using the Internet as a source of health and treatment information. This finding contrasts sharply with another study by Almuammar et al., 2021. Almuammar et al., 2021 found that 92.6% of participants in KSA used social media as a source of medical information [35]. Despite the lack of significant research discussing the online HSB of the Sudanese population, the low rate observed in our study suggests a significant gap. While this low rate of internet use might protect against misinformation and inappropriate self-medication, it also means that Sudanese immigrants are missing out on valuable online health awareness campaigns and health education resources. Therefore, efforts to integrate culturally appropriate online health education and awareness initiatives could enhance overall health outcomes for this population.
Implications
The findings of this study highlight health insurance as a crucial modifiable risk factor for negative health-seeking behavior. With 71% of our sample employed in the private sector, the lack of insurance coverage for employees and their families emerges as a significant issue contributing to suboptimal HSB among Sudanese immigrants. This inadequacy has detrimental effects on the well-being of these individuals. Therefore, urgent action is needed to enforce the Saudi Arabian labor law effectively to safeguard the health rights of vulnerable immigrant populations.
Furthermore, implementing interventions such as offering subsidized healthcare services in primary care facilities, maternal health, and mental health services could address the barriers faced by immigrants who are legally restricted from obtaining or maintaining health insurance. These targeted initiatives have the potential to improve access to essential healthcare services and enhance the overall health outcomes of immigrant communities.
Strength and limitations
As the first paper to be written on the health-seeking behavior of Sudanese immigrants, our study provides a foundation for future research and programs aimed at improving the health status and healthcare access of Sudanese immigrants and refugees worldwide. With the ongoing war in Sudan leading to a surge in refugees, our findings are particularly relevant and timely.
The limitations of our study primarily stem from the use of a convenient sampling technique. Limited resources compelled us to gather data solely from Sudanese social groups on Facebook and WhatsApp, resulting in a higher proportion of middle-aged male workers in our sample. Consequently, our study may have inadvertently excluded other segments of the population, such as females and young males. To address this limitation, we recommend that future research be conducted on a community or household basis to ensure a more representative sample and enhance the accuracy of the findings. It is important to note that the under-representation of females in our sample may also be attributed to the lower percentage of females among Sudanese immigrants and the low response rate in females-only Facebook and WhatsApp groups. Thus, there is a need for further investigation to explore the impact of gender on health-seeking behavior.
Furthermore, the cross-sectional design employed in this research captures a snapshot of the participants’ experiences at a specific point in time, limiting their ability to establish causal relationships or discern temporal patterns. Longitudinal studies would offer a more comprehensive understanding of how these factors evolve among the immigrant population.
Our study focused on health-seeking behavior toward any illness or medical issue, which may not fully capture the nuances of behavior toward specific illnesses. Factors such as severity and duration of the condition could potentially influence individuals’ responses and actions differently. Moreover, the retrospective nature of our study introduces the possibility of recall biases, as participants may not accurately remember past health-seeking experiences. Additionally, response bias cannot be ruled out, as participants may have provided answers that they perceived as more socially desirable. These limitations underscore the need for caution when interpreting our findings and highlight the importance of further research to explore these aspects in more detail.
Conclusion
Understanding the determinants of HSB among immigrant groups is crucial for improving healthcare access and resource allocation for this population. As inappropriate HSB has been linked to poorer health outcomes, identifying the factors that influence HSB can provide valuable insights into designing tailored health interventions to support the Sudanese immigrant community in KSA.
This study highlights the significance of insurance as a determinant of HSB, emphasizing the need for reforming current insurance policies that prioritize private companies over the health of immigrants. Further research is needed to explore the healthcare preferences and behaviors of Sudanese people and other migrants, particularly women and young people, to develop targeted policies aimed at reducing socioeconomic disparities in accessing healthcare services. By promoting universal health coverage, these policies can contribute to achieving sustainable development goals and improving the overall health and well-being of immigrant populations.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- HSB:
-
Health-seeking behavior
- KSA:
-
Kingdom Saudi Arabia
- SDG:
-
Sustainable development goal
- IOM:
-
International organization of migration
- KSA:
-
Kingdom of Saudi Arabia
- SAR:
-
Saudi Arabian Riyal
- UN:
-
United Nations
- PHC:
-
Primary health care
References
Latunji OO, Akinyemi OO, FACTORS INFLUENCING HEALTH-SEEKING. BEHAVIOUR AMONG CIVIL SERVANTS IN IBADAN, NIGERIA.
Kenya. Do you need up-to-date peer reviewed medical literature? KMA/GSK RESOURCE CENTRE. Vol. 28. 2002.
Cronin T, Sheppard J, de Wildt G. Health-seeking behaviour for schistosomiasis: a systematic review of qualitative and quantitative literature. 16, Pan Afr Med J. 2013.
Webair HH, Bin-Gouth AS. Factors affecting health seeking behavior for common childhood illnesses in Yemen. Patient Prefer Adherence. 2013;7:1129–38.
Ansong E. The Association between Household Consumer Durable Assets and maternal health-seeking behavior in Ghana. Women Health. 2015;55(5):485–504.
Akin JS, Guilkey DK, Denton EH, QUALITY OF SERVICES AND DEMAND FOR HEALTH. CARE IN NIGERIA: A MULTINOMIAL PROBIT ESTIMATION. 40, Soc Sci Med. 1995.
Anselmi L, Lagarde M, Hanson K. Health service availability and health seeking behaviour in resource poor settings: evidence from Mozambique. Health Econ Rev. 2015;5(1).
Mwabu G, Ainsworth M, Nyamete A. Board of Regents of the University of Wisconsin System Quality of Medical Care and Choice of Medical Treatment in Kenya: An Empirical Analysis [Internet]. Vol. 28, Source: The Journal of Human Resources. http://www.jstor.orghttp://www.jstor.org/stable/146295Accessed:11-12-201500:39UTC.
Lépine A, Le Nestour A. The determinants of health care utilisation in rural Senegal. J Afr Econ. 2013;22(1):163–86.
Rashidi S, Yazdanpanah A, Parvizaghayiibarzabad. Evaluating treatment-seeking behavior and the related factors among the dwellers of Safashahr city. Asian J Pharm Clin Res. 2017;10(1):144–9.
ILO LM. ILO global estimates on migrant workers: results and methodology. Geneva: International Labour Organisation (ILO); 2015.
International Organization of Migration [Internet]. 2022 [cited 2023 Sep 17]. World Migration Report 2022. https://worldmigrationreport.iom.int/wmr-2022-interactive/.
Jamil R, Kumar R. Culture, structure, and Health: narratives of low-income Bangladeshi migrant workers from the United Arab Emirates. Health Commun. 2021;36(11):1297–308.
Hussin AH, Ali FM. Examining Equal Access to Healthcare among Nationals and Expatriates: Evidence from Qatar’s World Health Survey [Internet]. https://ssrn.com/abstract=1532627
Alkhamis A, Cosgrove P, Mohamed G, Hassan A. The personal and workplace characteristics of uninsured expatriate males in Saudi Arabia. BMC Health Serv Res. 2017;17(1):1–12.
Shallal M. IJSR 3,2 SudaneSe immigrant familieS’ Structure and living arrangementS in the uae [Internet]. Vol. 3, International Journal of Sudan Research. 2013. http://www.worldsustainable.org.
IOM Revised response. Overview Sudan crisis and neighbouring countries. 2023.
Saudi Census [Internet]. 2022 [cited 2023 Sep 20]. Saudi Census 2022. https://portal.saudicensus.sa/portal/public/1/18/41?type=DASHBOARD.
Priebe S, Sandhu S, Dias S, Gaddini A, Greacen T, Ioannidis E et al. Good practice in health care for migrants: views and experiences of care professionals in 16 European countries. BMC Public Health. 2011;11.
UN. https://www.globalgoals.org/goals/3-good-health-and-well-being/. 2016. Sustainable development goal 3.
Xu H, Yang H, Wang H, Li X. The association of residence permits on utilization of health care services by migrant workers in China. Int J Environ Res Public Health. 2021;18(18).
Lebano A, Hamed S, Bradby H, Gil-Salmerón A, Durá-Ferrandis E, Garcés-Ferrer J et al. Migrants’ and refugees’ health status and healthcare in Europe: a scoping literature review. BMC Public Health. 2020;20(1).
Peng B, Ling L. Health service behaviors of migrants: a conceptual framework. Front Public Health. 2023;11.
Dawood OT, Jasim HH, Saleem F, Ibrahim IR. Assessment of health seeking behaviour and self-medication among general public in the state of Penang. Malaysia. 2017;15(3):1–7.
Latunji OO, Akinyemi OO, Health F, FACTORS INFLUENCING HEALTH-SEEKING BEHAVIOUR, AMONG CIVIL SERVANTS IN IBADAN. NIGERIA. 2018;16(1):52–60.
Podder D, Dasgupta A, Dobe M, Paul B, Bandyopadhyay L, Pal A. Health Care – Seeking Behavior in a Scheduled Tribe Community in India : A Mixed-Methods Research Using the Framework of Andersen ’ s Behavioral Model. 2021.
Levine D, Polimeni R, Ramage I. Insuring health or insuring wealth? An experimental evaluation of health insurance in rural Cambodia. J Dev Econ. 2016;119:1–15.
Cuong NV, Linh VH. The impact of Migration and remittances on Household Welfare: evidence from Vietnam. J Int Migr Integr. 2018;19(4):945–63.
Van De Raza WA, Bedi A, Rutten F. Impact of community-based health insurance on access and financial protection: evidence from three randomized control trials in rural India. Health Econ (United Kingdom). 2016;25(6):675–87.
Al-Hanawi MK, Mwale ML, Kamninga TM. The effects of health insurance on health-seeking behaviour: evidence from the Kingdom of Saudi Arabia. Risk Manag Healthc Policy. 2020;13:595–607.
Ministry of Labour Riyadh. Ministry of Labour, Labour Law. Riyadh; 2006. pp. 120–120.
Almaqhawi A, Alsayil S, Al Qadhib M, Alkhoufi A, Alkhalaf A, Al Khowildi Z. Patient’s Perspective on Factors Affecting Health-Seeking Behavior in Al-Ahsa, Saudi Arabia. Cureus. 2022.
Isameldin E, Saeed AA, Mousnad MA. Self-medication practice among patients living in Soba-. 2020;4:1–5.
Hussain MA, Mohamed AO, Abdelkarim OA, Yousef BA, Babikir AA, Mirghani MM et al. Prevalence and predictors of antibiotic self-medication in Sudan : a descriptive cross-sectional study. 2023;1–13.
Almuammar SA, Noorsaeed AS, Alafif RA, Kamal YF, Daghistani GM. The Use of Internet and Social Media for Health Information and its consequences among the Population in Saudi Arabia. 2021;13(9).
Acknowledgements
We would like to express our appreciation to Prof. Elfatih Malik (E.M.) and Dr. Sami Altalib (S.A.) Of the community medicine department, University of Khartoum, for their support. Many thanks go to all the respondents for their participation in this survey, and we sent them our hopes for a better and peaceful Sudan.
Funding
The authors received no funding for the conceptualization, design, data collection, analysis, decision to publish, or preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
N.E. conceptualized the research idea and collected the data.H.A. reported the results and prepared the tables.H.A., N.E. and A.E. analyzed the data and wrote the main manuscript text.All Authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Ethical approval for this study was obtained from the ethical committee at the University of Khartoum with an approval letter. The participants gave informed consent to participate in the study by signing an electronic consent form. The significance of the study and its goals were also conveyed. Individuals were made aware that participation in the study was optional and that they had the right to revoke consent at any time. Additionally, the confidentiality of the information gathered was emphasized.
Consent for publication
N/A.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Elfaki, N., Abdelgyoum, H. & Elhelali, A. Factors influencing health-seeking behavior among Sudanese immigrants in Saudi Arabia. BMC Public Health 24, 1666 (2024). https://doi.org/10.1186/s12889-024-19122-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19122-4