Abstract
Background
This study aimed to investigate the knowledge, attitudes, and practices (KAP) toward cardiovascular complications among end-stage renal disease patients undergoing maintenance hemodialysis.
Methods
This web-based cross-sectional study was conducted at Guangdong Provincial People’s Hospital between December 2022, and May 2023.
Results
A total of 545 valid questionnaires were collected, with an average age of 57.72 ± 13.47 years. The mean knowledge, attitudes and practices scores were 8.17 ± 2.9 (possible range: 0–24), 37.63 ± 3.80 (possible range: 10–50), 33.07 ± 6.10 (possible range: 10–50) respectively. Multivariate logistic regression analysis showed that patients from non-urban area had lower knowledge compared to those from urban area (odds ratio (OR) = 0.411, 95% CI: 0.262–0.644, P < 0.001). Furthermore, higher levels of education were associated with better knowledge, as indicated by OR for college and above (OR = 4.858, 95% CI: 2.483–9.504), high school/vocational school (OR = 3.457, 95% CI: 1.930–6.192), junior high school (OR = 3.300, 95% CI: 1.945–5.598), with primary school and below as reference group (all P < 0.001). Besides, better knowledge (OR = 1.220, 95% CI: 1.132–1.316, P < 0.001) and higher educational levels were independently associated with positive attitudes. Specifically, individuals with a college degree and above (OR = 2.986, 95% CI: 1.411–6.321, P = 0.004) and those with high school/vocational school education (OR = 2.418, 95% CI: 1.314–4.451, P = 0.005) have more positive attitude, with primary school and below as reference group. Next, better attitude (OR = 1.174, 95% CI: 1.107–1.246, P < 0.001) and higher education were independently associated with proactive practices. Those with college and above (OR = 2.870, 95% CI: 1.359–6.059, P = 0.006), and those with high school/vocational school education (OR = 1.886, 95% CI: 1.032–3.447, P = 0.039) had more proactive practices, with primary school and below as reference group.
Conclusions
End-stage renal disease patients undergoing maintenance hemodialysis demonstrated insufficient knowledge, positive attitudes, and moderate practices regarding cardiovascular complications. Targeted interventions should prioritize improving knowledge and attitudes, particularly among patients with lower educational levels and income, to enhance the management of cardiovascular complications in end-stage renal disease.
Similar content being viewed by others
Background
End-stage renal disease is a widespread health problem affecting millions of individuals worldwide. Approximately 4 million patients worldwide are currently receiving kidney replacement therapy (KRT), with hemodialysis being the most prevalent form, constituting approximately 69% of all KRT and 89% of all dialysis procedures [1]. However, the rates of impaired quality of life, morbidity, and mortality among hemodialysis patients are alarmingly high [2]. Notably, cardiovascular complications emerge as a major concern. It was reported that cardiovascular disease affects more than two-thirds of individuals undergoing hemodialysis and stands as the leading cause of morbidity, contributing to nearly 50% of all mortalities in this population [1]. The high prevalence of cardiovascular disease among patients undergoing hemodialysis is likely due to various factors, including fluid and electrolyte imbalances, hemodynamic instability, and the presence of uremic toxins during the dialysis process [3,4,5]. These factors can exert significant strain on the cardiovascular system, contributing to the increased risk of cardiovascular complications in these patients. Managing these risks requires a comprehensive approach to optimize fluid balance, control comorbid conditions, and closely monitor cardiovascular health in hemodialysis patients [6]. The coexistence of end-stage renal disease and cardiovascular disease creates a complex clinical scenario, necessitating a comprehensive understanding of the interplay between these two conditions.
In the quest to improve the care and outcomes of maintenance hemodialysis patients, investigating their knowledge, attitudes, and practices (KAP) regarding cardiovascular complications is of paramount importance. The KAP framework provides valuable insights into how patients perceive and manage their health conditions, offering a comprehensive assessment of their awareness, attitudes towards risk reduction, and adherence to recommended practices [7]. By exploring the KAP of maintenance hemodialysis patients, healthcare providers can identify gaps in patient education and implement targeted interventions to address modifiable risk factors and enhance cardiovascular health.
Despite the wealth of research on cardiovascular complications in patients with end-stage renal disease undergoing hemodialysis, there is a critical gap in understanding how these patients perceive and manage their cardiovascular health. A study conducted in Finland revealed that there was a significant lack of knowledge concerning dialysis management among patients undergoing pre-dialysis or home dialysis [8]. Previous studies have highlighted the significant improvement with the knowledge-attitude-behavior education program for Chinese adults undergoing maintenance hemodialysis [9]. However, there remains a paucity of research focusing specifically on the KAP of maintenance hemodialysis patients regarding cardiovascular complications. Therefore, the primary objective of this study is to explore the KAP toward cardiovascular complications among end-stage renal disease patients undergoing maintenance hemodialysis.
Methods
Study design and patients
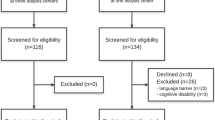
This cross-sectional study was conducted at the Blood Purification Center of Guangdong Provincial People’s Hospital between December 2022, and May 2023. The study enrolled maintenance hemodialysis patients with end-stage renal disease who met the following inclusion criteria: (1) End-stage renal disease patients receiving maintenance hemodialysis for three months or more; (2) Age ≥ 18 years; and (3) Signed informed consent form. Patients who were unable to independently complete the survey were excluded from the study.
This study was approved by the Ethics Committee of Guangdong Provincial People’s Hospital (KY-Q-2022-435-01) and obtained informed consent from the study subjects before completing the questionnaire.
Questionnaire and quality control
According to the Chinese Guidelines for the Management of Chronic Kidney Disease during Peri-dialysis Period [10], Chinese Guidelines for the Management of Chronic Heart Failure in Dialysis Patients [11], and the Clinical practice guidelines for renal anemia in China [12], a self-administered questionnaire consisting of four dimensions was developed and reviewed by three experts, including two nephrology specialists and one statistician, and incorporated for improvements. Similar questions were eliminated, and adjustments were made to clarify ambiguous statements. The final questionnaire consists of four sections: (1) Demographic characteristics include 8 items. (2) Knowledge dimension consists of 12 questions. A score of 2 signifies a high level of understanding, 1 is assigned for recognition (heard of), and 0 is allotted for incorrect or unclear answers. (3) Attitude dimension includes 10 questions. A five-point Likert scale was used, ranging from “very positive” (5 points) to “very negative” (1 point). (4) Practice dimension involves 10 questions, with the same five-point Likert scale, ranging from “always” (5 points) to “never” (1 point).
A small-scale pilot study involving 80 patients was conducted. The internal consistency of the questionnaire was evaluated good internal consistency with Cronbach’s α was 0.865. For data collection, an online questionnaire was developed using the Wen Juan Xing (WJX) platform (http s://www.wjx.cn), and a quick response (QR) code was generated for patients to access the questionnaire through WeChat. To ensure data quality and completeness, measures were taken to limit each IP address to a single submission, and all fields were made mandatory. Furthermore, the research team members meticulously examined the questionnaires for completeness, internal consistency, and reasonableness.
Statistical analysis
The statistical analysis software used was Stata 17.0 (Stata Corporation, College Station, TX, USA). Quantitative variables were described using mean ± standard deviation (SD), and between-group comparisons were conducted using t-tests or analysis of variance (ANOVA). Categorical variables were described using n (%) proportions. Pearson correlation analysis was used to assess the correlation between knowledge, attitude, and practice scores. Logistic regression analysis was employed for univariate and multivariate analyses of knowledge, attitudes and practices, with a cut-off value of 70% based on the score distribution [13]. In the multiple regression model, variables with a univariate P-value < 0.05 were included. Two-sided P-value < 0.05 was considered significantly different.
Results
Demographic characteristic
A total of 622 questionnaires were received. Subsequently, 66 of these were excluded from the analysis due to missing or abnormal values in the basic information, and 11 more questionnaires were excluded due to missing or abnormal KAP responses. As a result, the final analysis included 545 valid questionnaires. Among the patients, the average age was 57.72 ± 13.47 years, and the average dialysis duration was 5.00 ± 5.18 years. Among them, 306 (56.15%) were male, and 334 (61.28%) resided in urban areas. Moreover, 227 (41.65%) had an educational level of primary school and below, while only 54 (9.91%) were employed. Additionally, 287 (52.66%) reported a monthly per capita income < 2,000 CNY. Patients residing in urban areas and possessing higher education levels were more likely to demonstrate markedly higher knowledge (all P < 0.001), attitude (all P < 0.001), and practice (all P < 0.001) scores (Table 1).
The average knowledge, attitude and practice scores were 8.17 ± 2.9 (possible range: 0–24), 37.63 ± 3.80 (possible range: 10–50), 33.07 ± 6.10 (possible range: 10–50) respectively (Table 1). The distribution of knowledge indicated that patients did not attain a satisfactory level of knowledge concerning cardiovascular complications. The three knowledge items with the highest correctness rates were as follows: “Anemia significantly increases the risk of cardiovascular events and death in patients, severely affecting quality of life and survival rate.” with a correctness rate of 81.10%; “Anemia promotes the progression of chronic kidney disease and is significantly associated with heart failure in dialysis patients”, with a correctness rate of 79.45%; and “Advanced age, smoking, alcohol consumption, obesity, and diabetes are all risk factors for cardiovascular events such as heart failure”, with a correctness rate of 75.83%. However, the item with the lowest correctness rate was “The blood pressure control target for diabetic kidney disease patients on dialysis is < 140/90 mmHg”, with a correctness rate of 35.41%. The attitude distribution revealed that the majority of patients displayed a predominantly positive attitude towards cardiovascular complications, with “Agree” being the most commonly chosen response. Specifically, 34.68% of patients strongly agreed with the statement “I believe that preventing and treating the occurrence and progression of cardiovascular events is beneficial for prolonging life and improving quality of life”. Conversely, only 3.49% of patients strongly disagreed with the statement “If suspected of heart failure, I think following the doctor’s instructions for various tests is too cumbersome”. For the practices, most patients reported “Quitting smoking” (61.83%) and “Taking antihypertensive medication as prescribed by the doctor” (58.9%) as their primary actions. However, only 20.37% of patients chose “Always” in the statement “Adjusting diet, sodium intake of 5-6 g per day”, and a notable 22.39% indicated “Never” for the practice of “Quitting smoking.” (Table 2).
Pearson correlation analysis showed that knowledge was positively associated with attitude (r = 0.414, P < 0.001) and practice (r = 0.213, P < 0.001). Moreover, the analysis revealed that attitudes was positively associated with practice (r = 0.399, P < 0.001) (Table 3).
Multivariate logistic regression analysis showed that patients from non-urban area had lower knowledge compared to those from urban area (odds ratio (OR) = 0.411, 95% CI: 0.262–0.644, P < 0.001). Furthermore, higher levels of education were associated with better knowledge, as indicated by OR for college and above (OR = 4.858, 95% CI: 2.483–9.504), high school/vocational school (OR = 3.457, 95% CI: 1.930–6.192), junior high school (OR = 3.300, 95% CI: 1.945–5.598), with primary school and below as reference group (all P < 0.001). Besides, better knowledge (OR = 1.220, 95% CI: 1.132–1.316, P < 0.001) and higher educational levels were independently associated with positive attitudes. Specifically, individuals with a college degree and above (OR = 2.986, 95% CI: 1.411–6.321, P = 0.004) and those with high school/vocational school education (OR = 2.418, 95% CI: 1.314–4.451, P = 0.005) have more positive attitude, with primary school and below as reference group. Next, better attitude (OR = 1.174, 95% CI: 1.107–1.246, P < 0.001) and higher education were independently associated with proactive practices. Those with college and above (OR = 2.870, 95% CI: 1.359–6.059, P = 0.006), and those with high school/vocational school education (OR = 1.886, 95% CI: 1.032–3.447, P = 0.039) had more proactive practices, with primary school and below as reference group (Table 4).
Discussion
The study revealed that end-stage renal disease patients undergoing maintenance hemodialysis demonstrated inadequate knowledge, positive attitudes, and moderate practices toward cardiovascular complications. These findings underscore the importance of improving attitudes and providing educational support to encourage more proactive practices in managing cardiovascular risks among this patient group. Targeted interventions should prioritize enhancing knowledge and attitudes, particularly among patients with lower education levels and lower income, to enhance the management of cardiovascular complications in this population.
The findings from our study indicated that the average scores for KAP were generally below optimal levels, suggesting a widespread lack of adequate knowledge and appropriate practices concerning cardiovascular complications in patients with chronic kidney disease (CKD). Although the KAP of cardiovascular complications in patients with CKD or on hemodialysis was not established, it was reported that poor knowledge about CKD among the public and patients with CKD was widely reported in Iran [14], Hong Kong [15], and Northern Tanzania [16]. For example, a study conducted in Nigeria revealed that 65% of the patients with CKD exhibited poor knowledge about their condition [17]. Notably, research has demonstrated that patients’ knowledge is closely linked to improved self-management behaviors in patients on hemodialysis [18]. This study further showed a positive correlation between knowledge and practice scores, emphasizing the importance of enhancing the knowledge of patients on hemodialysis, particularly regarding cardiovascular complications. It is crucial to address this knowledge gap, as most therapies aimed at preventing kidney disease progression and reducing associated complications heavily rely on patients’ ability to effectively self-manage their condition.
Socioeconomic factors, such as residing in urban areas, higher education levels, and greater monthly per capita income, were associated with higher KAP scores. These findings suggest a socioeconomic disparity in cardiovascular health awareness and practices among maintenance hemodialysis patients. A study in United Kingdom reported that low socioeconomic status is related to severity of CKD [19]. Similarly, a study among US adults also showed that lower socioeconomic status including limited education or lower income is associated with greater risk of disability from CKD [20]. Moreover, a study of 2,171 patients with peritoneal dialysis in China showed that low personal income independently predicted the highest risks for all-cause or cardiovascular death compared with medium and high income [21]. Furthermore, the multivariate logistic regression analysis in this study identified higher attitude scores and higher education levels as independent predictors of more proactive practices. This finding highlights the significance of education in empowering individuals to engage in self-management behaviors to prevent the cardiovascular complications in their condition. Consistently, it was reported that the tertiary educational level was the only significant independent predictor of higher CKD knowledge (OR = 2.62 95%CI: 1.20–5.72, P = 0.02) [17]. It is likely due to the fact that individuals with more resources and access to educational opportunities are better equipped to the knowledge of measures and engage more effectively in preventing cardiovascular complications. Therefore, healthcare systems should focus on implementing targeted interventions that address the specific needs of patients from lower socioeconomic backgrounds.
In the context of preventing cardiovascular complications on maintenance hemodialysis, lifestyle modifications play a pivotal role, encompassing actions such as restricting dietary salt and water intake, engaging in regular exercise, and discontinuing smoking [22]. However, the current study reveals that patients with end-stage renal disease undergoing hemodialysis demonstrated only moderate adherence to practices aimed at mitigating cardiovascular complications. Specifically, a relatively modest portion of patients (20.37%) reported consistently adjusting their dietary habits to maintain a recommended sodium intake. Moreover, the cardiovascular care provided to hemodialysis patients should not only address their dietary salt but also ensure the promotion of good nutrition for those in the end-stage renal disease category. This dual focus is vital as cardiovascular complications may be interconnected with the malnutrition-inflammation-atherosclerosis syndrome in chronic kidney disease [23]. Nevertheless, a notable subset (22.39%) still expressed resistance to the practice of quitting smoking. It was widely established that smoking is associated with a markedly increased risk of heart disease in dialysis patients [24, 25]. Indeed, the findings of this study underscore the critical significance of lifestyle interventions for patients undergoing dialysis to effectively prevent cardiovascular complications. Besides education to the patients, it was also important for the doctors to maintaining good health practice upon themselves, and share experience to patients.
It is noteworthy that most participants in this study, who were undergoing maintenance hemodialysis for end-stage renal disease, were predominantly elderly, with lower educational attainment and reduced household income. This demographic profile correlated with demonstrated insufficient knowledge, positive attitudes, and moderate practices concerning cardiovascular complications. Given these findings, it is imperative to provide practical and easily understandable guidelines tailored to their unique circumstances. This could encompass straightforward dietary recommendations, simple exercise routines, and stress management techniques adapted to the lifestyle and resources of this population. Additionally, the establishment of community-based support groups is recommended. These groups can offer a platform for participants to share experiences, discuss challenges, and celebrate successes related to their health. Such forums serve as a valuable source of encouragement, fostering a sense of community and collective well-being among individuals facing similar health journeys.
The present study has several limitations. One limitation of this study was its cross-sectional design, which precludes the establishment of causal relationships between KAP scores and other factors. Longitudinal studies with interventions targeted at improving knowledge and attitudes are needed to further validate our findings and assess their impact on patients’ practices and cardiovascular outcomes over time. Certain questions may be deemed advanced for CKD patients, this is particularly evident due to the evolving nature of clinical practice guidelines and the ongoing debates among elite clinicians on topics such as blood pressure control targets and the role of anemia in CKD progression. However, it is crucial to acknowledge that participants’ responses to these questions may be influenced by their attentiveness to health education provided by medical personnel. Therefore, these questions can still be considered a valuable gauge of patients’ engagement with health education, providing insights into their understanding. Moreover, some terms (e.g., arrhythmias, heart failure, fatigue, etc.) used in the knowledge and attitude-related items could be considered technical for some patients. To ensure a clear understanding of the terms used in the questionnaire, oral explanations were provided to participants.
Conclusion
In conclusion, end-stage renal disease patients undergoing maintenance hemodialysis demonstrated inadequate knowledge, positive attitudes, and moderate practices related to cardiovascular complications. To enhance the management of cardiovascular complications in this patient group, it is crucial to implement targeted interventions aimed at improving knowledge and attitudes, particularly among those with lower education levels and lower income. By addressing these factors, better outcomes in the management of cardiovascular complications may be achieved among individuals undergoing hemodialysis for end-stage renal disease.
Data availability
All data generated or analysed during this study are included in this published article.
Abbreviations
- KRT:
-
Kidney replacement therapy
- KAP:
-
Knowledge, attitudes, and practices
- WJX:
-
Wen Juan Xing
- QR:
-
Quick response
- SD:
-
Standard deviation
- ANOVA:
-
Analysis of variance
- CKD:
-
Chronic kidney disease
References
Bello AK, Okpechi IG, Osman MA, Cho Y, Htay H, Jha V, et al. Epidemiology of haemodialysis outcomes. Nat Rev Nephrol. 2022;18:378–95.
Yoshikoshi S, Yamamoto S, Suzuki Y, Imamura K, Harada M, Osada S, et al. Associations between Dynapenia, cardiovascular hospitalizations, and all-cause mortality among patients on haemodialysis. J Cachexia Sarcopenia Muscle. 2022;13:2417–25.
Chirakarnjanakorn S, Navaneethan SD, Francis GS, Tang WH. Cardiovascular impact in patients undergoing maintenance hemodialysis: clinical management considerations. Int J Cardiol. 2017;232:12–23.
Ahmadmehrabi S, Tang WHW. Hemodialysis-induced cardiovascular disease. Semin Dial. 2018;31:258–67.
Penny JD, Moradshahi M, McIntyre CW. Assessment of microcirculatory function during hemodialysis. Curr Opin Nephrol Hypertens. 2022;31:553–9.
Canaud B, Chazot C, Koomans J, Collins A. Fluid and hemodynamic management in hemodialysis patients: challenges and opportunities. J Bras Nefrol. 2019;41:550–9.
Gawryś A, Gołębiowski T, Zielińska D, Augustyniak-Bartosik H, Kuriata-Kordek M, Szenborn L et al. Knowledge, attitudes and practices of Flu Vaccination in Hemodialysis patients. Vaccines (Basel). 2021;9.
Inkeroinen S, Koskinen J, Karlsson M, Kilpi T, Leino-Kilpi H, Puukka P, et al. Sufficiency of knowledge processed in Patient Education in Dialysis Care. Patient Prefer Adherence. 2021;15:1165–75.
Liu L, Liu YP, Wang J, An LW, Jiao JM. Use of a knowledge-attitude-behaviour education programme for Chinese adults undergoing maintenance haemodialysis: Randomized controlled trial. J Int Med Res. 2016;44:557–68.
Chinese Clinical Practice Guideline for the. Management of CKD-PeriDialysis-the Periods Prior to and in the early-stage of initial Dialysis. Kidney Int Rep. 2022;7:S531–58.
Chinese Society of Nephrology ZNBPIA. Guidelines for the management of chronic heart failure in dialysis patients in China. Chin J Nephrol. 2022;38:32.
Branch GWGoRAotCPAN. Clinical practice guidelines for renal anemia in China. Natl Med J China. 2021;101:40.
Lee F, Suryohusodo AA. Knowledge, attitude, and practice assessment toward COVID-19 among communities in East Nusa Tenggara, Indonesia: a cross-sectional study. Front Public Health. 2022;10:957630.
Roomizadeh P, Taheri D, Abedini A, Mortazavi M, Larry M, Mehdikhani B, et al. Limited knowledge of chronic kidney disease and its main risk factors among Iranian community: an appeal for promoting national public health education programs. Int J Health Policy Manag. 2014;2:161–6.
Chow KM, Szeto CC, Kwan B, Leung CB, Li PK. Public lacks knowledge on chronic kidney disease: telephone survey. Hong Kong Med J. 2014;20:139–44.
Stanifer JW, Turner EL, Egger JR, Thielman N, Karia F, Maro V, et al. Knowledge, attitudes, and practices Associated with chronic kidney disease in Northern Tanzania: A Community-based study. PLoS ONE. 2016;11:e0156336.
Okoro RN, Ummate I, Ohieku JD, Yakubu S, Adibe MO, Okonta MJ. Kidney Disease Knowledge and its determinants among patients with chronic kidney disease. J Patient Exp. 2020;7:1303–9.
Curtin RB, Sitter DC, Schatell D, Chewning BA. Self-management, knowledge, and functioning and well-being of patients on hemodialysis. Nephrol Nurs J. 2004;31:378 – 86, 96; quiz 87.
Bello AK, Peters J, Rigby J, Rahman AA, El Nahas M. Socioeconomic status and chronic kidney disease at presentation to a renal service in the United Kingdom. Clin J Am Soc Nephrol. 2008;3:1316–23.
Plantinga LC, Johansen KL, Schillinger D, Powe NR. Lower socioeconomic status and disability among US adults with chronic kidney disease, 1999–2008. Prev Chronic Dis. 2012;9:E12.
Xu R, Han QF, Zhu TY, Ren YP, Chen JH, Zhao HP, et al. Impact of individual and environmental socioeconomic status on peritoneal dialysis outcomes: a retrospective multicenter cohort study. PLoS ONE. 2012;7:e50766.
Sarnak MJ, Auguste BL, Brown E, Chang AR, Chertow GM, Hannan M, et al. Cardiovascular effects of Home Dialysis therapies: A Scientific Statement from the American Heart Association. Circulation. 2022;146:e146–64.
Zyga S, Christopoulou G, Malliarou M. Malnutrition-inflammation-atherosclerosis syndrome in patients with end-stage renal disease. J Ren Care. 2011;37:12–5.
Burmeister JE, Mosmann CB, Costa VB, Saraiva RT, Grandi RR, Bastos JP, et al. Prevalence of cardiovascular risk factors in hemodialysis patients - the CORDIAL study. Arq Bras Cardiol. 2014;102:473–80.
Di Benedetto A, Marcelli D, D’Andrea A, Cice G, D’Isa S, Cappabianca F, et al. Risk factors and underlying cardiovascular diseases in incident ESRD patients. J Nephrol. 2005;18:592–8.
Acknowledgements
The authors acknowledge the support and assistance of the blood purification center of Guangdong Provincial People’s Hospital for performing the study.
Funding
This study was supported by the Guangzhou Science and Technology Project (No. 202206080010) and the Guangdong Province High-Level Hospital Construction Project (No. DFJHBF202101).
Author information
Authors and Affiliations
Contributions
ZL carried out the studies, participated in collecting data, and drafted the manuscript. LS and DMC performed the statistical analysis and participated in its design. Others participated in acquisition, analysis, or interpretation of data and draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Guangdong Provincial People’s Hospital (KY-Q-2022-435-01) and all participants were informed about the study protocol and provided written informed consent to participate in the study. I confirm that all methods were performed in accordance with the relevant guidelines. All procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Z., Song, L., Hua, R. et al. Knowledge, attitudes, and practices toward cardiovascular complications among end-stage renal disease patients undergoing maintenance hemodialysis. BMC Public Health 24, 1448 (2024). https://doi.org/10.1186/s12889-024-18945-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18945-5