Abstract
Background
Men experiencing infertility encounter numerous problems at the individual, family, and social levels as well as quality of life (QOL). This study was designed to investigate the QOL of men experiencing infertility through a systematic review.
Materials and methods
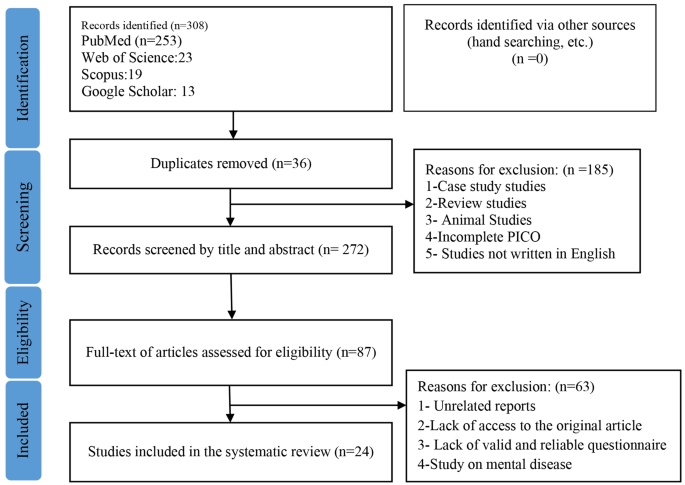
This systematic review was conducted without any time limitation (Retrieval date: July 1, 2023) in international databases such as Scopus, Web of Science, PubMed, and Google Scholar. The search was performed by two reviewers separately using keywords such as QOL, infertility, and men. Studies were selected based on inclusion and exclusion criteria. The quality of the articles were evaluated based on the Newcastle-Ottawa Scale. In the initial search, 308 studies were reviewed, and after removing duplicates and checking the title and abstract, the full text of 87 studies were evaluated.
Results
Finally, 24 studies were included in the final review based on the research objectives. Based on the results, men’s QOL scores in different studies varied from 55.15 ± 13.52 to 91.45 ± 13.66%. Of the total reviewed articles, the lowest and highest scores were related to mental health problems and physical dimensions, respectively.
Conclusion
The reported findings vary across various studies conducted in different countries. Analysis of the factors affecting these differences is necessary, and it is recommended to design a standard tool for assessing the quality of life of infertile men. Given the importance of the QOL in men experiencing infertility, it is crucial to consider it in the health system. Moreover, a plan should be designed, implemented and evaluated according to each country’s contex to improve the quality of life of infertile men.
Similar content being viewed by others
Introduction
Defined as the absence of pregnancy after one or two years of unprotected sexual intercourse (without the use of contraceptive methods) [1], infertility is recognized as both a medical and social issue [2]. Based on the latest Word Health Organization (WHO) report in 2023, the pooled lifetime and period prevalence of infrtility are reported as 17.5% and 12.6%, respectively [3]. In this regard, male factors play a role in 50% of infertilities [4].
Complicated treatment protocol, difficult treatment process, semen analysis, multiple ultrasounds, invasive treatments, long waiting lists, and high financial costs for the clients who seek assisted reproductive techniques have been described as psychological stresses for infertile couples [5, 6]. Moreover, the diagnosis and treatment of infertility can have negative impact on the frequency of sexual intercourse, self-esteem, and body image [5]. However, these men usually tend to suppress or deny their problems which may diminish their quality of life (QOL) over time [7]. This decreased QOL, in turn, can have a detrimental effect on their response to treatment [8].
The function of infertile people is under the influence of society, family, and the society culture. In many societies, infertility is primarily viewed as a medical problem, often neglecting its individual and social dimensions [9]. In other words, despite having the right attitude toward infertility, infertile people sometimes cannot adapt to the problem. Thus, non-compliance during the behavioral process may lead to additional problems and impair one’s QOL [10].
The WHO describes the QOL as people’s perspective of their life circumstances in terms of the cultural systems and standards of their environment, and how these perspectives are associated with their objectives, prospects, ideals, and apprehensions [11]. Recently, the QOL of men experiencing infertility as a main subject has been carefully considered by health investigators. Furthermore, because of men’s essential role in future phases of life, their QOL can significantly affect their health at both individual and societal levels [12].
Given the significance of QOL, its precise measurement is substantially important. In this regard, various tools have been designed and used in studies to examine this concept. A systematic study used the World Health Organization Quality Of Life )WHOQOL), 36-Item Short Form Survey (SF-36 ), and general QOL questionnaires. Based on the results, the QOL of men experiencing infertility was reported to be low in two studies that had used the SF-36 questionnaire. By contrast, the QOL of these men was high in a study that used the WHOQOL questionnaire. It was noted in this systematic review that although infertility has a negative effect on the mental health and sexual relationships of couples, there is no consensus regarding its effect on the QOL of infertile couples [13].
In Almutawa et al.‘s systematic review and meta-analysis 2023, it has been shown that the psychological disturbances in infertile women are higher than in men, and this difference in couples needs further investigation [14]. Chachavomich et al. 2010 showed that women’s quality of life is more affected by infertility than men study, which was a systematic review [12], . This study was conducted 14 years ago and due to the increase in the number of articles in this field, it needs to be re-examined.Given that no systematic review had been conducted to address the QOL of men experiencing infertility and considering the significance of this issue in therapeutic responses, this study examined the QOL of men experiencing infertility in the form of a systematic review.
Methods
Search strategy
To search and review the studies, reputable international databases and sites such as Scopus, Web of Science, PubMed, and Google Scholar were used. The search was performed using keywords such as QOL, infertility, and men (Table 1), without time limitation (Retrieval date: July 1, 2023), and using AND and OR operators, and specific search strategies were used for each database.
The search strategy of PubMed, Web of Science, and Scopus databases is as follows:
Pubmed (retrieval date: July 1, 2023)
Male [tiab] OR Males [tiab] OR Men [tiab] OR Man [tiab] OR Boy [tiab] OR Boys [tiab] AND Quality of Life [tiab] OR Health-Related Quality of Life [tiab] AND Infertility [tiab] OR Sterility OR Reproductive [tiab] OR Reproductive Sterility [tiab] OR Subfertility [tiab] Sub-Fertility [tiab].
Web of science (retrieval date: July 1, 2023)
((TI=(male OR males OR man OR men OR boy OR boys)) AND TI=(Quality of Life OR Health-Related Quality of Life OR Health-Related Quality of Life)) AND TI=(Infertility OR Sterility OR Reproductive OR Reproductive Sterility).
Scopus (retrieval date: July 1, 2023)
TITLE ( male OR males OR men OR man OR boy OR boys ) AND TITLE (quality AND of AND life OR health-related AND quality AND of AND life ) AND TITLE ( infertility OR sterility OR reproductive).
The method of presenting the article, describing the problem, data collection, data analysis, discussion, and conclusion of the findings were based on preferred reporting items for systematic reviews and meta-analyses (PRISMA) 2020 [15]. The reviews were conducted separately by two reviewers, and the third reviewer was also used in case of disagreement between them.
Inclusion and exclusion criteria
Those studies with the following criteria were included in the review: (1) Observational studies; (2) Cross-sectional data from longitudinal studies; (3) Using valid tools for measuring the QOL; (4) Studies conducted on men of infertile couples (by men experiencing infertility we mean those men whose unprotected sexual intercourse during the past year did not lead to any pregnancy); (5) Minimum sample size of 30 subjects; (6) Subjects with no chronic disease, and (7) those men of infertile couples who were within the diagnostic process for infertility and before starting infertility treatment. The search and review process for this study were conducted in English, and there were no restrictions imposed on the inclusion of open-access studies.
Exclusion criteria included: (1) Case report studies; (2) Review studies; (3) Animal studies; (4) Studies on mental syndromes; (5) Studies not written in English; (6) Lack of access to the full text of the article, and (7) Unrelated reports.
The patient, intervention, comparison, outcome, and study design (PICOS)
PICOS model was used to help break down the searchable elements of the research question into (P) participants: men experiencing infertility (primary or secondary infertility) (I) intervention/exposure: not applicable; (C) control group: not applicable; (O) outcomes: evaluate infertile men’s QOL, which was measured using standard tools such as general or specific QOL questionnaire and (S) study type: Observational studies and Cross-sectional data from longitudinal studies.
Data extraction
The two reviewers independently reviewed the titles and abstracts of the articles following the inclusion criteria, and the studies which did not have the required criteria were excluded. Then, the full text of the articles with inclusion criteria was reviewed and if appropriate, they were included in the study.
Required information, including authors’ names, year of publication, research location, sample size, QOL score, type of tool, type of infertility, mean age of men, and duration of infertility, were extracted from the studies.
Outcome measurement
The main outcome of this study was to evaluate QOL of men experiencing infertility, which was measured using standard tools such as a general or specific QOL questionnaire.
Quality evaluation
The Newcastle-Ottawa Scale checklist was used to assess the quality of nonrandomized studies in meta-analyses [16]. This checklist consists of 5 parts that are representativeness of the sample, sample size, non-respondents, ascertainment of anxiety, and quality of descriptive statistics reporting. Each part gets a score of zero and one. Given the fact that the checklist has 5 items, the minimum, and maximum scores are 0 and 5, respectively. Then, studies were divided into high- and low-risk groups if their scores were ≤ 3 and more than 3 [16]. The quality assessment in this study was performed by two reviewers independently, and in case of disagreement between them, the third reviewer was asked to help. The coefficient of agreement of 0.7 and more among the reviewers was acceptable.
Ethical consideration
Ethics approval was obtained from the Ethics Committee, Faculty of Pharmacy and Nursing.
Midwifery, Shahid Beheshti University (Ethical code: IR.SBMU.PHARMACY.REC.1400.214). All methods were carried out in accordance with relevant guidelines and regulations.
Results
After reviewing the title, abstract, and text of the articles in different stages (Fig. 1), finally, 24 articles were reviewed based on the inclusion criteria and research objectives and the coefficient of agreement among the reviewers was K = 0.81 (Table 2).
The smallest and largest sample size were 30 [19] and 1,000 [40], respectively. Seven studies were conducted in low- and middle-income countries, two studies in upper-middle-income, and 15 studies in high-income countries. High-income countries had a higher quality of life score compared to low- and middle-income countries countries. In all studies, QOL scores were calculated based on 100, and the highest score (91.45 ± 13.66%) obtained from the Fertility quality of life (FertiQoL) questionnaire in South Korea as a high-income country [25]. Most of the studies showed that education, family income and proper marital relations improved the quality of life of infertile men. Out of 24 reviewed articles, 12 articles used the FertiQoL questionnaire, 7 articles SF-36, and 6 articles WHOQOL-BREF. One study [36] used SF-36 and WHOQOL-BREF questionnaires simultaneously.
Out of the total articles reviewed, the lowest scores were attributed to different domains. Accordingly, the lowest score in 11 articles was related to mental health problems, in 8 articles it was related to social problems, and 3 articles to communication problems.Some articles did not report the scores based on the dimensions. Based on the results, men’s QOL scores in different studies varied from 55.15 ± 13.52 to 91.45 ± 13.66%. In the total reviewed articles, the lowest and highest scores were related to mental health problems and physical dimensions, respectively.
In most of the studies using the FertiQoL questionnaire, it was observed that the lowest scores belonged to the social and communication dimensions. The FertiQoL questionnaire was developed and psychometrically evaluated in a survey study conducted in the United States. FertiQoL is a 36-item scale with Six dimension: (1) Emotional; (2) Mind-body; (3) Relational; (4) Social; (5) Environment; and (6) Treatment tolerability. A 5-point Likert scale (0–4) was used in the questionnaire, and the total score was between 0 and 100, where the higher the score, the better was the QOL [41]. This questionnaire has been translated into different languages in the world and has obtained the required validity (content, face, and construct) and reliability (with Cronbach’s alpha of 0.7–0.9) in different populations [42,43,44,45].
In the studies where the SF-36 and WHOQOL-BREF questionnaires had been used, the lowest scores belonged to the dimensions of limitations in usual role activities because of emotional problems and social relationships. On the other hand, the highest scores in the questionnaires were related to physical dimensions. The SF-36 questionnaire has been considered for clinical investigation, health policy assessments, and surveys. The 8 dimensions of this questionnaire are as follows: Restrictions in physical activities; Restrictions in social activities; Restrictions in standard role activities; Physical pain; General mental health; Restrictions in standard role activities; Vitality; and Common health perceptions. The final scores of the questionnaire are standardized based on 100 [46]. This questionnaire has been translated into different languages in the world and has obtained validity (content and face) and reliability (Cronbach’s alpha of 0.8–0.95) in different populations [47,48,49,50,51,52]. The 26-item version of WHOQOL-BREF was developed in the following four dimensions: physical health, mental health, social connections, and environmental health, and two items associated with common QOL and general health [53]. The questionnaire has been translated into different languages of the world and has obtained validity (content and face) and reliability (Cronbach’s alpha of 0.74–0.88) in different populations [54,55,56,57].
Discussion
This systematic review study investigated the quality of life of infertile men. Based on the results, men’s quality of life scores in different studies varied from 55.15 ± 13.52 to 91.45 ± 13.66%. However, men’s quality of life scores was reported to be between 70 and 80% in the majority of the studies. As one of the health indicators with a combination of each person’s knowledge in different aspects of life and performance in human, work and social relations, quality of life is essentially important for the continuation of an optimal life and well-being of the individuals. Moreover, quality of life is strongly influenced by demographic, social, economic, and cultural variables, as well as the variables related to health and disease, and its measurement is, thus, substantially important [58]. Quality of life is a reflection of the desires, hopes, and expectations of individuals regarding their current and future life situation, and is influenced by factors such as age, personal and family characteristics, socio-economic status, and time [59].
In this systematic review, the lowest scores of men’s quality of life belonged to the psychological and emotional dimensions and then to the social and communication dimensions. Although the reviewed studies had used different tools, these tools were essentially similar in these dimensions, indicating the problems of men in these areas. Fertility is highly valued in most cultures and the desire for having a child is one of the human stimuli in the continuation of life. If efforts for fertility do not lead to success, they can have adverse effects on mental health as well as family and social relationships [60].
The reviewed studies indicated that education has a significantly positive effect on the quality of life of infertile men. Higher levels of education are associated with increased awareness and better decision-making abilities [25], and improved coping strategies for dealing with infertility-related challenges [38]. Infertile men with higher education are also more likely to seek treatment, and remain hopeful that treatment will improve their quality of life [28].
The results of most studies showed the positive and significant relationship between family income and quality of life.The costs of infertility treatment and the potential need for repeated treatment can lead to concerns and anxieties among men and reduce their quality of life [61]. If men have fewer concerns about the cost of treatment, they are more inclined to pursue infertility treatment. In the International Conference on Population and Development held in Cairo in 1994, addressing the issue of infertility was emphasized as an important health priority. However, it is unfortunate that infertility problems have been overlooked not only in developing countries but also at various levels of international health management [62].
The results of the study regarding the countries’ income showed that the quality of life score of men in infertile couples residing in low-income countries was lower compared to those in high-income countries. Current infertility policies in the treatment and distribution sector are uncoordinated, which has led to improper distribution of public and private centers in low- and middle-income countery [63]. This point of view is a kind of simplistic calculation of the problem of infertility that justifies the lack of public centers, inadwquate finantial sources, specialists and affordable treatment options [64], requireing serious attention and careful planning, especially in low- and middle-income countries.
The results of the studies showed that marital relationships have a positive and significant impact on the quality of life of infertile men. Sometimes, infertile men may experience a lack of sexual attraction, and due to irrational thoughts, they might abstain from having sexual relations with their partners or try to suppress their sexual desires. Sexual desire is a significant aspect of life that can affect the quality of life [65]. Some studies have indicated that the quality of marital relations is higher among infertile couples than the fertile ones, and infertility can bring couples closer together and encourage more open communication about their concerns and plans for the future [33, 66]. Further research is recommended to gain a deeper understanding in this area.
Infertility presents people with a new and challenging world [28]. In this regard, infertility is characterized as a long-term process that involves time-consuming treatments, fluctuations between hope and disappointment, loss of control over reproductive outcomes, inability to plan for future, and significant shifts in personal identity and worldview [28, 32, 63]. Long working hours, work-caused exhaustion, along with infertility, can exacerbate men’s problems. These problems affect their quality of life, though they may deny the problems [67].
Given the significance of quality of life, its accurate measurement is essentially important. In this regard, various tools have been designed to investigate this concept and have been used in several studies. The noteworthy point in this systematic review was the use of different measurement tools in various studies. In the majority of the studies, Boivin’s FertiQoL [41] was used as a specific tool for measuring the quality of life of infertile couples. Covering emotional, physical, communicational, social, environmental, and acceptability dimensions, this questionnaire has been designed for infertile couples and does not specifically assess the quality of life of infertile men. Other studies have used a general quality-of-life questionnaire (SF-36 and WHOQOL-BREF). WHOQOL questionnaire has been designed in 4 dimensions of physical health, psychological health, social relationships, and environmental health [53]. SF-36 questionnaire also has 8 dimensions of Limitations in physical activities because of health problems; 2) Limitations in social activities because of physical or emotional problems; 3) Limitations in usual role activities because of physical health problems; 4) Bodily pain; 5) General mental health (psychological distress and well-being); 6) Limitations in usual role activities because of emotional problems; 7) Vitality (energy and fatigue); and 8) General health perceptions [46]. The main drawback of these tools is that they ignore significant dimensions such as sexual and socio-economic dimensions which are important for certain groups including infertile men. Additionally, the other dimensions of the questionnaire are not sensitive enough to measure changes in the quality of life of people with various diseases [68].
Health researchers have recently paid much attention to the examination of the quality of life and the design of a questionnaire to measure this concept. This measurement can improve clinical decision-making, estimate healthcare in a particular population, perceive different health causes and consequences, and, finally, promote health policy. All of these objectives will be achieved in light of a specific tool in this regard. However, according to the review, no questionnaire has hitherto been designed to measure the quality of life in infertile men. Specific questionnaires for infertile couples or general quality of life questionnaires have been used in different studies. Given the concept of quality of life and its changes over time as well as the expansion of tool-making knowledge, there is a need to design specific tools to measure the quality of life of infertile men by using mixed methods. We hope that more attention will be given to this significant issue in future. Polit and Beck argue that one of the main applications of exploratory mixed methods is in instrument making. They maintain that when a new tool is developed to explain a health-related concept, the complexity of this concept must be carefully explained [69].
Furthermore, it seems that the concept of men’s quality of life needs more investigation and also this concept may change over time and impact on their life. Besides, the studies demonstrated specific concerns among infertile men such as decreased self-esteem, Fertility- related stress, masculinity identity, hiding the infertility problem, resistance to the treatment, and cost of treatment [70, 71]. These concerns could be the specific items for the infertile men-related quality of life questionnaire.
Research limitations
The impossibility of meta-analysis was because of several limitations in the study: (1) Variety of tools and small sample size in each subgroup; (2) Inaccurate report of information; and (3) -heterogeneity of the studies. Other limitation in this systematic review was that the reviewed papers were confined to English literature; thus, it is possible that some relevant non-English language studies were missed.
The systematic review strategies and solutions
The quality of life of men is one of the basic issues in their life. Assessing the quality of life of men should be done during the initial evaluation of infertility, and if necessary, interventions should be made to improve their quality of life. It is recommended that researchers, using qualitative-quantitative methods, first explain the concept of the QOL of men with infertility and then design and psychometrically evaluate the QOL tool for men experiencing infertility. Based on its context, each country should design a suitable program to improve the quality of life of men.
Conclusion
The reported findings vary across various studies conducted in different countries. Analysis of the factors affecting these differences is necessary, and it is recommended to design a standard tool for assessing the quality of life of infertile men. Given the importance of the QOL in men experiencing infertility, it is crucial to consider it in the health system. Moreover, a plan should be designed, implemented and evaluated according to each country’s contex to improve the quality of life of infertile men.
Data availability
All data related to this review is included in the result section of the manuscript. If any further data is needed it can be accessible via the corresponding author on request.
Abbreviations
- WHO:
-
World Health Organization
- NOS:
-
The Newcastle-Ottawa Scale
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- NA:
-
Not reported
- SF-36:
-
The Health Survey Short Form
- WHOQOL-BREF:
-
World Health Organization Quality of Life Instruments
- FertiQoL:
-
The Fertility Quality of Life tool
References
Berek JS. Berek & Novak’s gynecology. Lippincott Williams & Wilkins; 2019.
Kiani Z, Simbar M, Hajian S, Zayeri F. The prevalence of depression symptoms among infertile women: a systematic review and meta-analysis. Fertility Res Pract. 2021;7(1):1–10.
World Health Organization. Infertility prevalence estimates: 1990–2021. 2023.
Santi D, Granata A, Simoni M. FSH treatment of male idiopathic infertility improves pregnancy rate: a meta-analysis. Endocr Connections. 2015;4(3):R46–58.
Hayden RP, Flannigan R, Schlegel PN. The role of lifestyle in male infertility: diet, physical activity, and body habitus. Curr Urol Rep. 2018;19(7):1–10.
Kiani Z, Simbar M, Hajian S, Zayeri F, Shahidi M, Saei Ghare Naz M, et al. The prevalence of anxiety symptoms in infertile women: a systematic review and meta-analysis. Fertility Res Pract. 2020;6(1):1–10.
Ilacqua A, Izzo G, Emerenziani GP, Baldari C, Aversa A. Lifestyle and fertility: the influence of stress and quality of life on male fertility. Reproductive Biology Endocrinol. 2018;16(1):1–11.
https://www.skillsyouneed.com/ips/relationship-skills.html,Accessed, 14 September 2023.
Hasanpoor-Azghady SB, Simbar M, Abou Ali Vedadhir SAA, Amiri-Farahani L. The social construction of infertility among Iranian infertile women: a qualitative study. J Reprod Infertility. 2019;20(3):178.
Lawshe CH. A quantitative approach to content validity 1. Pers Psychol. 1975;28(4):563–75.
World Health Organization. The World Health Organization quality of life assessment (WHOQOL): development and general psychometric properties. Soc Sci Med. 1998;46(12):1569–85.
Chachamovich JR, Chachamovich E, Ezer H, Fleck MP, Knauth D, Passos EP. Investigating quality of life and health-related quality of life in infertility: a systematic review. J Psychosom Obstet Gynecol. 2010;31(2):101–10.
Luk BH-K, Loke AY. The impact of infertility on the psychological well-being, marital relationships, sexual relationships, and quality of life of couples: a systematic review. J Sex Marital Ther. 2015;41(6):610–25.
Almutawa YM, AlGhareeb M, Daraj LR, Karaidi N, Jahrami H, Karaidi NA. A systematic review and Meta-analysis of the Psychiatric morbidities and Quality of Life Differences between Men and Women in infertile couples. Cureus. 2023;15(4).
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372.
Zhang L, Fu T, Yin R, Zhang Q, Shen B. Prevalence of depression and anxiety in systemic lupus erythematosus: a systematic review and meta-analysis. BMC Psychiatry. 2017;17(1):1–14.
Andrei F, Salvatori P, Cipriani L, Damiano G, Dirodi M, Trombini E, et al. Self-efficacy, coping strategies and quality of life in women and men requiring assisted reproductive technology treatments for anatomical or non-anatomical infertility. Eur J Obstet Gynecol Reproductive Biology. 2021;264:241–6.
Warchol-Biedermann K. The etiology of infertility affects fertility quality of life of males undergoing fertility workup and treatment. Am J Men’s Health. 2021;15(2):1557988320982167.
Asazawa K, Jitsuzaki M, Mori A, Ichikawa T, Shinozaki K. Effectiveness of a spousal support program in improving the quality of life of male patients undergoing infertility treatment: a pilot study. Int J Community Based Nurs Midwifery. 2020;8(1):23.
Cusatis R, Fergestrom N, Cooper A, Schoyer KD, Kruper A, Sandlow J, et al. Too much time? Time use and fertility-specific quality of life among men and women seeking specialty care for infertility. BMC Psychol. 2019;7(1):1–9.
Asazawa K, Jitsuzaki M, Mori A, Ichikawa T, Shinozaki K, Porter SE. Quality-of‐life predictors for men undergoing infertility treatment in Japan. Japan J Nurs Sci. 2019;16(3):329–41.
Shahraki Z, Afshari M, Ghajarzadeh M, Tanha FD. How different are men with infertility-related problems from fertile men in prevalence of Depression, anxiety and quality of life? Maedica. 2019;14(1):26.
Jahromi BN, Mansouri M, Forouhari S, Poordast T, Salehi A. Quality of life and its influencing factors of couples referred to an infertility center in Shiraz. Iran Int J Fertility Steril. 2018;11(4):293.
Goker A, Yanikkerem E, Birge O, Kuscu NK. Quality of life in Turkish infertile couples and related factors. Hum Fertility. 2018;21(3):195–203.
Kim JH, Shin HS, Yun EK. A dyadic approach to infertility stress, marital adjustment, and depression on quality of life in infertile couples. J Holist Nurs. 2018;36(1):6–14.
Casu G, Ulivi G, Zaia V, Fernandes Martins MdC, Parente Barbosa C, Gremigni P. Spirituality, infertility-related stress, and quality of life in Brazilian infertile couples: analysis using the actor‐partner interdependence mediation model. Res Nurs Health. 2018;41(2):156–65.
Maroufizadeh S, Hosseini M, Foroushani AR, Omani-Samani R, Amini P. The effect of depression on quality of life in infertile couples: an actor-partner interdependence model approach. Health Qual Life Outcomes. 2018;16(1):1–7.
Zurlo MC, Della Volta MFC, Vallone F. Predictors of quality of life and psychological health in infertile couples: the moderating role of duration of infertility. Qual Life Res. 2018;27(4):945–54.
Madero S, Gameiro S, García D, Cirera D, Vassena R, Rodríguez A. Quality of life, anxiety and depression of German, Italian and French couples undergoing cross-border oocyte donation in Spain. Hum Reprod. 2017;32(9):1862–70.
Agostini F, Monti F, Andrei F, Paterlini M, Palomba S, La Sala GB. Assisted reproductive technology treatments and quality of life: a longitudinal study among subfertile women and men. J Assist Reprod Genet. 2017;34:1307–15.
El Kissi Y, Amamou B, Hidar S, Idrissi KA, Khairi H, Ali BBH. Quality of life of infertile Tunisian couples and differences according to gender. Int J Gynecol Obstet. 2014;125(2):134–7.
Huppelschoten AG, Van Dongen A, Verhaak C, Smeenk J, Kremer J, Nelen W. Differences in quality of life and emotional status between infertile women and their partners. Hum Reprod. 2013;28(8):2168–76.
Onat G, Beji NK. Effects of infertility on gender differences in marital relationship and quality of life: a case-control study of Turkish couples. Eur J Obstet Gynecol Reproductive Biology. 2012;165(2):243–8.
Herrmann D, Scherg H, Verres R, Von Hagens C, Strowitzki T, Wischmann T. Resilience in infertile couples acts as a protective factor against infertility-specific distress and impaired quality of life. J Assist Reprod Genet. 2011;28(11):1111–7.
Bolsoy N, Taspinar A, Kavlak O, Sirin A. Differences in quality of life between infertile women and men in Turkey. J Obstetric Gynecologic Neonatal Nurs. 2010;39(2):191–8.
Chachamovich JL, Chachamovich E, Ezer H, Cordova FP, Fleck MM, Knauth DR, et al. Psychological distress as predictor of quality of life in men experiencing infertility: a cross-sectional survey. Reproductive Health. 2010;7(1):1–9.
Chachamovich J, Chachamovich E, Fleck M, Cordova FP, Knauth D, Passos E. Congruence of quality of life among infertile men and women: findings from a couple-based study. Hum Reprod. 2009;24(9):2151–7.
Drosdzol A, Skrzypulec V. Quality of life and sexual functioning of Polish infertile couples. Eur J Contracept Reproductive Health Care. 2008;13(3):271–81.
Rashidi B, Montazeri A, Ramezanzadeh F, Shariat M, Abedinia N, Ashrafi M. Health-related quality of life in infertile couples receiving IVF or ICSI treatment. BMC Health Serv Res. 2008;8(1):1–6.
Ragni G, Mosconi P, Baldini MP, Somigliana E, Vegetti W, Caliari I, et al. Health-related quality of life and need for IVF in 1000 Italian infertile couples. Hum Reprod. 2005;20(5):1286–91.
Boivin J, Takefman J, Braverman A. The fertility quality of life (FertiQoL) tool: development and general psychometric properties. Hum Reprod. 2011;26(8):2084–91.
Hsu P-Y, Lin M-W, Hwang J-L, Lee M-S, Wu M-H. The fertility quality of life (FertiQoL) questionnaire in Taiwanese infertile couples. Taiwan J Obstet Gynecol. 2013;52(2):204–9.
Maroufizadeh S, Ghaheri A, Amini P, Samani RO. Psychometric properties of the fertility quality of life instrument in infertile Iranian women. Int J Fertility Steril. 2017;10(4):371.
Asazawa K, Jitsuzaki M, Mori A, Ichikawa T, Shinozaki K, Yoshida A, et al. Validity and reliability of the Japanese version of the fertility quality of life (FertiQoL) tool for couples undergoing fertility treatment. Open J Nurs. 2018;8(9):616–28.
Gao M, Ji X, Zhou L, Zhang Z. AB084. The fertility quality of life (FertiQol) in Chinese infertile women. Translational Androl Urol. 2016;5(Suppl 1).
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical care. 1992:473 – 83.
Jenkinson C, Stewart-Brown S, Petersen S, Paice C. Assessment of the SF-36 version 2 in the United Kingdom. J Epidemiol Community Health. 1999;53(1):46–50.
Alonso J, Prieto L, Anto J. The Spanish version of the SF-36 Health Survey (the SF-36 health questionnaire): an instrument for measuring clinical results. Medicina Clínica. 1995;104(20):771–6.
Shayan NA, Arslan UE, Hooshmand AM, Arshad MZ, Ozcebe H. The short form health survey (SF-36): translation and validation study in Afghanistan. East Mediterr Health J. 2020;26(8):899–908.
HÅvard Loge J, Kaasa S. Short form 36 (SF-36) health survey: normative data from the general Norwegian population. Scand J Soc Med. 1998;26(4):250–8.
Bjorner JB, Thunedborg K, Kristensen TS, Modvig J, Bech P. The Danish SF-36 Health Survey: translation and preliminary validity studies. J Clin Epidemiol. 1998;51(11):991–9.
Apolone G, Mosconi P. The Italian SF-36 Health Survey: translation, validation and norming. J Clin Epidemiol. 1998;51(11):1025–36.
Organization WH. WHOQOL-BREF: introduction, administration, scoring and generic version of the assessment: field trial version, December 1996. World Health Organization; 1996.
Kim WH, Hahn SJ, Im HJ, Yang KS. Reliability and validity of the Korean World Health Organization Quality of Life (WHOQOL)-BREF in people with physical impairments. Annals Rehabilitation Med. 2013;37(4):488.
Yao G, Chung C-W, Yu C-F, Wang J-D. Development and verification of validity and reliability of the WHOQOL-BREF Taiwan version. J Formos Med Assoc. 2002;101(5):342–51.
Usefy A, Ghassemi GR, Sarrafzadegan N, Mallik S, Baghaei A, Rabiei K. Psychometric properties of the WHOQOL-BREF in an Iranian adult sample. Commun Ment Health J. 2010;46(2):139–47.
Jaracz K, Kalfoss M, Górna K, Bączyk G. Quality of life in Polish respondents: psychometric properties of the Polish WHOQOL–Bref. Scand J Caring Sci. 2006;20(3):251–60.
Khayata G, Rizk D, Hasan M, Ghazal-Aswad S, Asaad M. Factors influencing the quality of life of infertile women in United Arab Emirates. Int J Gynecol Obstet. 2003;80(2):183–8.
Li Y, Zhang X, Shi M, Guo S, Wang L. Resilience acts as a moderator in the relationship between infertility-related stress and fertility quality of life among women with infertility: a cross-sectional study. Health Qual Life Outcomes. 2019;17(1):1–9.
Dyer S, Chambers GM, Adamson GD, Banker M, De Mouzon J, Ishihara O, et al. ART utilization: an indicator of access to infertility care. Reprod Biomed Online. 2020;41(1):6–9.
Kiani Z, Fakari FR, Hakimzadeh A, Hajian S, Fakari FR, Nasiri M. Prevalence of depression in infertile men: a systematic review and meta-analysis. BMC Public Health. 2023;23(1):1972.
Widge A, Cleland J. The public sector’s role in infertility management in India. Health Policy Plann. 2009;24(2):108–15.
Kiani Z, Simbar M, Hajian S, Zayeri F. Quality of life among infertile women living in a paradox of concerns and dealing strategies: a qualitative study. Nurs Open. 2021;8(1):251–61.
De Berardis D, Mazza M, Marini S, Del Nibletto L, Serroni N, Pino M, et al. Psychopathology, emotional aspects and psychological counselling in infertility: a review. Clin Ter. 2014;165(3):163–9.
Starc A, Trampuš M, Pavan Jukić D, Grgas-Bile C, Jukić T. Polona Mivšek A. Infertility and sexual dysfunctions: a systematic literature review. Acta Clin Croatica. 2019;58(3):508–15.
Drosdzol A, Skrzypulec V. Evaluation of marital and sexual interactions of Polish infertile couples. J Sex Med. 2009;6(12):3335–46.
Wischmann T, Thorn P. (Male) infertility: what does it mean to men? New evidence from quantitative and qualitative studies. Reprod Biomed Online. 2013;27(3):236–43.
Streiner D, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. Aust NZJ Public Health. 2016.
Polit D, Beck C. Essentials of nursing research: appraising evidence for nursing practice. Lippincott Williams & Wilkins; 2020.
Wu W, La J, Schubach KM, Lantsberg D, Katz DJ. Psychological, social, and sexual challenges affecting men receiving male infertility treatment: a systematic review and implications for clinical care. Asian J Androl. 2023;25(4):448–53.
Biggs SN, Halliday J, Hammarberg K. Psychological consequences of a diagnosis of infertility in men: a systematic analysis. Asian J Androl. 2024;26(1):10–9.
Acknowledgements
The authors would like to express their gratitude and thank to the cooperation and assistance of the officials of faculty, library and computer ward at Shahid Beheshti University of Medical Sciences.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
ZK: Project development, Data Collection, Manuscript writing MS: Project administration, writing-review, and editing, supervision FR: Project administration, writing-review, and editing, supervision FZ: Project development, Data Collection, Manuscript writing HB: Project development, Data Collection, Manuscript writing All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the Ethics Committee, Faculty of Pharmacy and Nursing.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kiani, Z., Simbar, M., Rashidi, F. et al. The quality of life of men experiencing infertility: a systematic review. BMC Public Health 24, 1236 (2024). https://doi.org/10.1186/s12889-024-18758-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18758-6