Abstract
Background
Composite Index of Anthropometric Failure (CIAF) combines all three forms of anthropometric failures to assess undernutrition status of children. There is no study on CIAF to identify the real and severe form of under nutrition among Ethiopian children that addressed community level factors. So, this study determined CIAF and identified important factors which helps to design appropriate intervention strategies by using multi-level advanced statistical model.
Methods
The study included 5,530 under five children and utilized a secondary data (EMDHS 2019) which was collected through community-based and cross-sectionally from March 21 to June 28, 2019. Composite index of anthropometric failure among under five children was assessed and a two-stage sampling technique was used to select the study participants. Descriptive summary statistics was computed. A multi-level binary logistic regression model was employed to identify important predictors of CIAF in under five children. Adjusted odds ratio with its 95% CI was estimated and level of significance 0.05 was used to determine significant predictors of CIAF.
Results
The prevalence of composite index of anthropometric failure (CIAF) was 40.69% (95% CI: 39.41, 42.00) in Ethiopia. Both individual and community level predictors were identified for CIAF in under five children. Among individual level predictors being male sex, older age, short birth interval, from mothers who have not formal education, and from poor household wealth quintile were associated with higher odds of CIAF among under five children. Low community women literacy and being from agriculturally based regions were the community level predictors that were associated with higher odds of CIAF in under five children in Ethiopia.
Conclusions
The burden of composite index of anthropometric failure in under five children was high in Ethiopia. Age of child, sex of child, preceding birth interval, mother’s education, household wealth index, community women literacy and administrative regions of Ethiopia were identified as significant predictors of CIAF. Therefore, emphasis should be given for those factors to decrease the prevalence of CIAF in under five children in Ethiopia.
Similar content being viewed by others
Background
Under-nutrition is a major public health concern in many developing nations, including Ethiopia, and is a global concern. Additionally, it is still one of the main causes of disease, early mortality, and morbidity in these countries' children [1,2,3].
Under-nutrition in the population of under-five children is commonly measured by three anthropometric indicators, namely stunting (low height for age), wasting (low weight for height), and underweight (low weight for age). Stunting and wasting are symptoms of chronic and acute dietary deficits, respectively. Additionally, both acute and chronic dietary deficiencies are reflected by underweight [4, 5]. This approach is used to evaluate the size, proportion and composition of the human body. Children's general health status, dietary sufficiency, and growth and development patterns can all be assessed using anthropometry [6, 7].
In order to address the issue of multiple nutritional failures and to report the prevalence of real data, the Composite Index of Anthropometric Failure (CIAF) method was developed. This method can be used to identify children who have one or more anthropometric failure(s) [8]. The CIAF is an anthropometric index that combines the three indices of weight-for-age, height/length-for-age, and weight-for height/length in order to assess the nutritional status of children under five years of age [9]. The combined index method of the Svedberg model creates six categories of undernourished children: A) without anthropometric failure; B) wasting only; C) wasting and underweight; D) wasting, underweight, and stunting; E) underweight and stunting; F) stunting only. Additionally, Nandy et al. added category Y), which is underweight only [10].
In 2019, globally there were 144 million stunted, 47 million wasted, and 38 million over weighted children under the age of five [11]. According to a World Bank report on under-five child malnutrition, Asian children account for 56% of stunted children, while African children for 37% of stunted children and 25% of wasted children [12]. Results from the Global Burden of Diseases, Injuries, and Risk Factors Study 2016 (GBD 2016) indicate that in Sub-Saharan Africa (SSA), an estimated 36.6% of children under five were stunted, 8.6% were wasting, and 19.5% were underweight in 2015 [13]. In Ethiopia according to EMDHS 2019 report, there were 37% stunted children under five, 7% wasted children, and 21% underweight children [14].
The majority of earlier research on undernutrition prevalence and contributing factors in Ethiopia has concentrated on a particular undernutrition indicator, such as stunting, wasting, and underweight [8, 15,16,17,18,19], separately proposed by the World Health Organization (WHO) [20]. But because the children in those conventional indices overlapped into numerous categories of anthropometric failure, they severely underestimated the prevalence and were unable to provide accurate estimates of the true cost of childhood undernutrition. This is due to the fact that the commonly used indices may overlap, making it possible for a single kid to exhibit signs of two or more undernutrition indicators at the same time. As a result, the indices may not be sufficient to accurately assess the true burden of undernutrition situations among children under five [3, 8, 16, 17, 19, 21,22,23,24,25,26]. By combining the common indicators of undernutrition measures, the creation of the composite index of anthropometric failure (CIAF) gets beyond these restrictions [8, 15,16,17, 27]. Literatures support the use of CIAF rather than using traditional (conventional) methods for the assessment of child undernutrion status [28, 29].
This study provides new estimates for the prevalence of undernutrition by aggregating traditional undernutrition indices which is important to capture the overall impact of under nutrition on a population unlike that of any of the three traditional indicators. Even if there was a limited study conducted regarding childhood under-nutrition using CIAF in Ethiopia which was a small scale surveys [30] limited in particular regions of the country. The current study was incorporates variables like region, residence, community women education level, and poverty level to determine how they affect CIAF. Therefore, to address the above identified gaps this study aim to assess undernutrition using the CIAF and its predictor on children under the age of five in Ethiopia using multi-level advanced statistical model.
Methods
Study design and setting
Community-based cross-sectional study design was employed among under five children in Ethiopia. Administratively, Ethiopia is divided into nine geographical regions and two administrative cities. Ethiopia is located in the horn of Africa covering 1,104, 300 km2 that ranks 10th in Africa in land coverage.
So far, in Ethiopia about six Demographic and Health Surveys (four main and two mini) conducted in Ethiopia. The 2019 EMDHS is the latest survey conducted in Ethiopia. The Ethiopian Public Health Institute (EPHI) conducted the survey at the need of Ethiopian Federal Ministry of Health (EFMoH). Financial support was provided by the government of Ethiopia, World Bank through the Ministry of Finance and Economic Development’s Enhancing shared Prosperity through Equitable Services (ESPES) and Promoting Basic Services (PBS) projects, the United Nations Children’s Fund (UNICEF), and the United States agency for International Development (USAID). Inner City Fund (ICF) provided technical support via the DHS program, which is funded by the USAID and offers support and technical assistance for the implementation of population and health surveys in countries worldwide. The 2019 Ethiopian Mini Demographic and Health Survey (EMDHS 2019) is the second Mini Demographic and Health Survey and the sixth Demographic and Health Survey conducted in Ethiopia, which was conducted from March 21, 2019 to June 28, 2019 [14].
Population
The source population is under five children in Ethiopia in EMDHS 2019 survey time. The study population is under five children who were living in the selected enumeration areas during EMDHS 2019 in Ethiopia. All under five children in Ethiopia were included to this study. All under five children who fulfill the inclusion criteria but children who had incomplete data [14].
Sample size and sampling procedures
Since this study used a secondary data and the study participants were 5,530 under five children. The data set is large and collected nationwide across all regions of Ethiopia. The sampling frame used for the 2019 EMDHS was a frame of all census enumeration areas (EAs) created for the 2019 Ethiopia Population and Housing Census (EPHC) and conducted by the Central Statistical Agency (CSA). The census frame was a complete list of the 149,093 EAs created for the 2019 EPHC. An EA is a geographic area covering an average of 131 households. The data from a DHS survey naturally forms a hierarchy of household within a cluster, household members within each household, interviewed women and men as a subset of household members, and children of each interviewed woman [14].
The 2019 EDHS sample was stratified and selected in two stages. Each region was stratified in to urban and rural areas, yielding 21 sampling strata. Samples of EAs were selected independently in each stratum in two stages. Implicit stratification and proportional allocation were achieved at each of the lower administrative levels by sorting the sampling frame within each sampling stratum before sample selection, according to administrative units in different units in different levels [14].
In the first stage, a total of 305 EAs (93 from urban and 212 from rural areas) were selected with probability proportional to EA size and with independent selection in each sampling stratum. A household listing operation was carried out in all selected EAs from January through April 2019. The resulting lists of households served as a sampling frame for the selection of households in the second stage. In the second stage of selection, a fixed number of 30 households per cluster were selected with an equal probability of systematic selection from the newly created household listing, and all under five children who were either permanent residents or visitors and slept in the household the night before the survey were eligible for an interview [14, 31].
Variables of the study
The theoretical framework how the individual and the community-level factors contribute to the Campsite Index of Anthropometric Failure (CIAF) supported by the ecological model that individual development is influenced by nested layers of the environment, from individual characteristics (like age) to broader societal factors (like socioeconomic status).
Composite Index of Anthropometric Failure (CIAF) is not solely determined by individual choices and behaviors. Social, economic, and environmental factors within communities significantly influence CIAF outcomes. By incorporating these community-level variables, we can move beyond individual-level explanations and uncover broader societal influences on CIAF.
Dependent variable
Children composite index of anthropometric failure coded as 1 = yes, 0 = no.
Stratifier variable
Cluster number (enumeration area) was the stratifier variable (v001 which ranges from 1 to 305 enumeration areas).
Independent variables
Level 1 factors: Individual level and household level characteristics
Mother’s education, Mother’s age, Mother’s BMI, child age, child sex, birth type, birth order, birth interval, mothers’ education, Wealth index, drinking water source, type of toilet facility.
Level 2 factors: Community level characteristics
Region, residence, community poverty level, community women literacy, community mass media exposure.
Operational definitions
Composite index of anthropometric failure (CIAF): is an anthropometric index that combines weight-for-age (WAZ), length/height-for-age (HAZ) and weight-for-length (WHZ) to determine the nutritional status of children under five. The category of undernutrition based on the CIAF is divided in to (“anthropometric failure” coded as 1) and no failure (“normal” coded as 0). The categories are grouped in to: A) no failure (normal); B) wasting only; C) wasting and underweight; D) wasting, underweight and stunting; E) underweight and wasting; F) stunting only; Y) underweight only (Table 1). The anthropometric failure is the total amount of undernutrition or sum of category of wasting only (B); wasting and underweight (C); wasting, underweight and stunting (D); underweight and wasting (E); stunting only (F); underweight only(Y). At the same time, the CIAF index can be used to detect some anthropometric failures [32].
Source: The concept of Composite index of Anthropometric Failure (CIAF) by Kuiti and Bose: Revisited and Revised (2018).
Region: Regions (Amhara, Tigray, Oromia, SNNP and Harari) which livelihood mainly based on agriculture classified as agrarian (coded as 2); regions (Afar, Somali, Gambella, and Benishangul-Gumuz) which livelihood mainly based on nomadism classified as pastoralist or emerging regions (coded as 1); and regions or city administrations (Addis Ababa and Dire Dawa) which livelihood mainly based on employment and trade classified as urban (coded as 0) [33, 34].
Community poverty level: The household wealth status of the community below the median was considered as poor or greater /equal to the median was considered as a rich community wealth index.
Community women literacy: Community considered as literate if at least 50% of women in the community attend at least primary education and illiterate if women in the community had no education or only less than half proportion of women in the community educated.
Data collection
Ethiopian Public Health Institute (EPHI) recruited and trained 151 health professional field staff for the main fieldwork to serve as female interviewers, female anthropometrics, female computer-assisted personal interview (CAPI) supervisors, field supervisors, regional coordinators, and their respective reserves. A household questionnaire, woman questionnaire and man questionnaire were completed at every selected household from each cluster. Questionnaires captured demographic, socio-economic and household characteristics, child characteristics, and child caring practices, and maternal caring practices data. Information on general demographics of the household was collected from the female head of the household. Child’s age was based on birth, health records available at the household or self-reports of the mother or caretaker using an event calendar. Anthropometric indicator length/height-for-age was determined for under five children using current WHO growth standards [14].
Anthropometric measurements
The length of children aged < 24 months was measured during the EDHS in a recumbent position to the nearest 0.1 cm using a locally made measuring board (Shorr Board®) with an upright wooden base and moveable headpieces. Children ≥ 24 months were measured while standing upright. The length/height-for-age Z-score, an indicator of nutritional status, was compared with reference data from the WHO Multicenter Growth Reference Study Group, 2006. Children whose height-for-age Z-score is < -2 SD from the median of the WHO reference population are considered stunted (short for their age) [14].
Weight: Weight measurement was taken after children were undressed (no shoes, dresses and wet hat). For a child who stands on the weighing scale calmly, the measurement was taken in the nearest 0.1 kg. In the time of refuse to be scaled, children’s mother carried and stood on the scale. Finally, the child actual weight was registered by subtracting mother’s weight from mother and child weight [14].
Quality assurance
The pretest for the 2019 EDHS was performed. EPHI recruited and trained the main field work to serve as team supervisors, field editors, interviewers, secondary editors, and reserve interviewers. In addition, individuals were recruited and trained on how to collect biomarker data, including taking height and weight measurements, testing for anemia by measuring hemoglobin levels.
Data processing and data analysis
The data management was done through STATA/MP 17.0 statistical analysis software package. The full data set was down loaded from MEASURE DHS website. Some continuous variables were recoded to categorical variables. Data cleaning was performed before any statistical analysis. The kids recode (KR) data set in STATA file is the data set containing the outcome and predictor variables of this study. The data was explored in different ways. The “SVY set” command was used for considering complex survey design. The “iweigh” and “pweight” commands were used for descriptive statistics and regression model respectively for sampling weigh adjustment.
This study was based on secondary data analysis of 2019 EDHS by adjusting sample weights. Categorical characteristics and outcome of the study was described in terms of percentage and frequencies. Tables, bar graph and pie chart were used to present the data for some selected variables which had significant association with CIAF. A bi-variable multi-level logistic regression analysis was carried out to see the crude effect of each independent variable on CIAF, and then variables with p. value of < 0.2 were entered to the multivariable multi-level binary logistic regression model. The subject matter knowledge, clinical and social significance, and evidence from the literature also considered for candidate variable selection.
The prevalence of CIAF was estimated with 95% of confidence interval. Summary statistic (mean, median, SD, and IQR) and AOR with 95% confidence intervals were estimated at 0.05 level of significance to identify important predictor variables of CIAF.
Intra class correlation (ICC); median odds ratio (MOR) and proportional change in variance (PCV) statistic were calculated to measure the variation between clusters (the random effect variable). The deviance information criterion (DIC) statistic was calculated for the different models (individual level, community level and both individual and community level) fitted with logit, probit and cloglog link functions. The DIC was used to evaluate and compare model performance of the full model and the reduced model. A model with lower DIC was considered as one with a better fit.
Results
Socio-demographic characteristics of respondents
A total of 5,530 under five children (weighted samples) were included in this study. From this study finding 2,521 (50.90%) children were males. Three thousand seven hundred twelve (74.06%) of the children was residing in rural area of Ethiopia. Two thousand nine hundred sixty two (59.82%) of the children were from 24–59 months, while 1469 (29.66%) of the children were 6–23 months. Three thousand seventy one (79.13%) of the children had short preceding birth interval (less than 24 months). Two thousand six hundred fifty four (53.59) of the children were from mothers who have no formal education. The median age of the children’s mothers were 28 years old (IQR = 8). 4755 (96.02%) of the mothers were married (Table 2).
Prevalence of composite index of anthropometric failure (CIAF) and subgroups of CIAF in under five children in Ethiopia
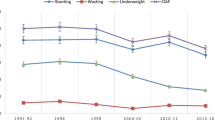
In this study the prevalence of CIAF was 40.69% (95% CI: 39.41%, 42.00%) in Ethiopia in 2019 which is the latest national data ( \* MERGEFORMAT Fig. 1). From this, the highest share of CIAF was from Oromia region (14.92%) followed by Amhara region (8.78%) and Southern Nations nationalities & people region (8.12%) in Ethiopia. While the lowest share was from Gambella region (0.11%) and Harari region (0.11%) ( \* MERGEFORMAT Fig. 2).
From the subgroups of anthropometric failures in under five children; subgroup F (stunting only) was the highest (37%), subgroup Y (underweight only) was the second (21%), and subgroup B (wasting only) was the third (7%). The top least were subgroup D (stunting and underweight and wasting) (3%) and subgroup G (stunting and wasting) (3%) ( \* MERGEFORMAT Fig. 3).
Predictors of composite index of anthropometric failure in under five children in Ethiopia
Random effect analysis and model fit statistics
All of the random effect analysis parameters favor the final model (model IV) as the best fit model. From the intra class correlation coefficient estimate indicates evidence of substantial clustering which is the proportion of the total variation attributable to variation between clusters, or as correlation between under five children with in the same cluster. The ICC in the model I (null model) indicates that about 11.79% (95% CI: 8.99%, 15.32%) of the variability in composite index of anthropometric failure (CIAF) was attributed to the community/cluster/enumeration area level variability. The MOR in the model I also revealed that if two under five children are taken from two different clusters i.e. one from a cluster with higher CIAF and one from a cluster with lower CIAF) the odds of having CIAF among who came from cluster with higher CIAF was 1.88 times higher as compared to their counter parts. Moreover, the PCV in the final model (model IV) showed that about 44.02% of the variability in the CIAF was explained by both community level and individual level factors. Regarding model fitness, model IV (full model) was the best fitted model since it had the lowest deviance and this model was used to assess predictors of CIAF (Table 3).
Fixed effect analysis
Bi-variable analysis was performed to identify potential candidate variables for the multivariable analysis using 0.2 level of significance. Multivariable analysis was performed to identify significant predictor variables of composite index of anthropometric failure (CIAF) among under five children in Ethiopia. Individual level (level 1) predictor variables and community level (level 2) predictor variables were assessed in model II and model III. Finally, model IV (full model) was fitted to identify important significant predictor variables of CIAF.
In the multivariable analysis, the odds of having CIAF was lower among females 0.71 (AOR: 0.71; 95% CI: 0.56, 0.89) as compared to males keeping the other covariates constant. The odds of having CIAF was higher among under five older age groups 6–23 months 1.64 (AOR: 1.64; 95% CI: 1.10, 2.44), 24–59 months 2.85 (AOR: 2.85; 95% CI: 1.85, 4.38) as compared with those whose ages were below 6 months. Children belonging to mothers with primary education, and no formal education was 1.80 (AOR: 1.80; 95% CI: 1.02, 3.17) and 2.15 (AOR: 2.15; 95% CI: 1.19, 3.89) respectively times higher odds of CIAF as compared to those who had secondary or higher education. Under five children from middle households and poorest households had 2.08 (AOR: 2.08; 95% CI: 1.12, 3.86) and 2.44 (AOR: 2.44; 95% CI: 1.22, 4.88) respectively times higher odds of CIAF as compared to those who were from richest households. Preceding birth interval less than 24 months had 1.27 (AOR: 1.27; 95% CI: 1.02, 1.58) times CIAF as compared to those who had greater than or equal to 24 months. In protestant religion followers the odds of CIAF was 0.69 (AOR: 0.69; 95% CI: 0.52, 0.92) times higher as compared to orthodox followers. Children belonging to divorced mothers had 0.47 (AOR: 0.47; 95% CI: 0.56, 0.92) times odds of CIAF as compared its counterpart married mothers. Regarding to the community level variables; children from high community women literacy had 0.74 (AOR: 0.74; 95% CI: 0.56, 0.98) times higher as it is compared to its counterpart. Regarding the Ethiopian administrative region, under five children from agriculturally based region had 1.89 (AOR: 1.89; 95% CI: 1.16, 3.07) times higher odds of CIAF as compared to under five children from the urban based region (Table 4).
Discussion
These results demonstrate that when conventional indices (stunting, wasting, and underweight) are used alone, they miss a significant number of under-five children who already have multiple anthropometric deficits. This is because conventional indices underestimate the prevalence of under-nutrition and do not provide the overall prevalence of under-nutrition in children. By using the CIAF aggregate measurements of malnutrition, this problem was avoided [29]. Studies conducted in Ethiopia [35,36,37] focused on either of the conventional indices may be suitable to inform interventions targeting at the reduction of each of the conventional indices alone, whereby, this study may help address the primary causes of undernutrition in the nation in all of its manifestations.
In Ethiopia, composite index of anthropometric failure (CIAF) still remains public health problem. Nationally, the prevalence of CIAF was high (nearly 41%). The finding is below to study findings previously done in Ethiopia (61.30% in 2000, 56.57% in 2005, 51.58% in 2011 and 46.58% in 2016) [38]. The figure is also lower than to the finding in southwest Ethiopia (50.80%)[30]. But similar to study finding in the rural area of the Bogor District in Indonesia (42.12%) [13]. However, the current study higher than those found in Tanzania (38.2%) [22] and various parts of India, including Parwano and Himacha Pradesh (31.9%) [39], rural areas of west Bengal (32.7%)[40]. When compared with the prevalence of under-nutrition among Argentineans (15.1%) [41] and Bangladesh 11.3%[42], in the current research, the prevalence of malnutrition was much higher. The variation with other previous studies may be due to the difference in socio-economic and socio-cultural characteristics of respondents between countries. And the study period is also matters the difference in the findings of different studies.
The findings showed that female children had a lower risk of having CIAF than male children from a similar socioeconomic background. This study is consistent with previous studies [38, 43], It could possibly be a factor in CIAF because of the biological growth and vulnerability of men and the fact that the percentage of male preterm births is higher than that of female preterm births [44].
The results showed that children in the older age group were more likely than those in the younger age group to have CIAF. This is in line with research done in other nations, such as Tanzania and Yemen [15, 22]. This may result from a child being fed a more balanced and nutrient-rich food when they are younger, but as a child gets older, breastfeeding may stop and their body's need for nutrients may rise.
Furthermore, a birth interval of less than 24 months raises the likelihood of being CIAF. The results of this investigation are in line with those of other investigations [45,46,47]. Individuals with short inter-birth intervals may experience negative effects on their children's nutrition as it might compromise the child's intrauterine growth and quality of care [48].
It was discovered that undernutrition in children was substantially correlated with the mother's educational attainment. Additionally, this conclusion is in line with earlier research showing that maternal education reduces childhood undernutrition [38, 42, 49]. One explanation could be that moms' formal education provides them with knowledge that enables them to practice healthy eating habits and other related behaviours that avoid undernutrition. Additionally, compared to mothers who lack education, educated mothers are more likely to seek medical attention for childhood ailments [50]. Greater use of health care, adoption of contemporary medical procedures, and more female autonomy are all correlated with better maternal education. These factors then impact decisions about health that enhance the nutritional outcomes for children [51].
According to the current study, children from lower-class families are more likely than their counterparts to be impacted by the CIAF. This is consistent with earlier research done in many nations [42, 43, 52]. This could be the case because the wealthiest households can afford to buy different types and amounts of food for their kids, while poorer homes may have less access to health care services than wealthier ones.
According to this study, the region of Ethiopia significantly affects the CIAF of children. Compared to children living in cities, children from rural backgrounds are more likely to have CIAF. A plausible rationale for this could be because youngsters residing in metropolitan areas have superior living standards and quicker access to sustenance [53]. Furthermore, the current research shows that children from high community women literacy had less likely to have CIAF than their counterparts from low community women literacy. This could be due to educated community women are more likely to follow basic nutrition and hygiene practices. Additionally, compared to their counterparts from low community women literacy, children from high community women literacy had a lower likelihood of having CIAF. This may be because community women with higher levels of education are more likely to adhere to basic cleanliness and dietary guidelines, which may lower the risk of anthropometric failure. Another reason could be that informed community women are aware of the importance of nutrition and are able to prevent undernutrition by understanding the information offered by the media or medical professionals.
Conclusions
This study found that composite index of anthropometric failure (CIAF) was high in Ethiopia. Factors both at the individual level and at the community level were predictors of composite index of anthropometric failure. Individual level predictors like age of child, sex of child, preceding birth interval, mother’s education, household wealth index were identified as important predictors of CIAF of the under five children. Whereas community level predictors such as community women literacy and administrative regions of Ethiopia were identified as predictors of CIAF in under five children.
Therefore, giving special attention to male children, older age of children, those children from mothers’ who had no formal education, and those who are from poor socioeconomic to decrease the burden of composite index of anthropometric failure in under five children in Ethiopia. Besides, increasing the community women literacy can decrease the CIAF in under five children. Attention is also should be given for agricultural based administrative regions of Ethiopia.
Availability data and materials
The dataset used during the current study is available from the corresponding author upon reasonable request.
Abbreviations
- BMI:
-
Body Mass Index
- BDHS:
-
Bangladesh Demographic and Health Survey
- CAPI:
-
Computer-Assisted Personal Interview
- CIAF:
-
Composite Index of Anthropometric Failure
- DIC:
-
Deviance Information Criterion
- EDHS:
-
Ethiopian Demographic and Health Survey
- EFMoH:
-
Ethiopian Federal Ministry of Health
- EMDHS:
-
Ethiopian Mini Demographic and Health Survey
- EPHI:
-
Ethiopian Public Health Institute
- GBD:
-
Global Burden of Diseases
- ICC:
-
Intra Class Correlation
- LMICs:
-
Low- and Middle-Income Countries
- MOR:
-
Median Odds Ratio
- PCV:
-
Proportional Change in Variance
- SDG:
-
Sustainable Development Goal
- SSA:
-
Sub-Saharan Africa
- UNICEF's:
-
United Nations Children's Fund
- WHO:
-
World Health Organization
References
Dl P. The relationship between child anthropometry and mortality in developing countries: implications for policy, progress and future research. J Nutr. 1994;124(Suppl):2047–81.
Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? The lancet. 2003;361(9376):2226–34.
Nandy S, Irving M, Gordon D, Subramanian S, Smith GD. Poverty, child undernutrition and morbidity: new evidence from India. Bull World Health Organ. 2005;83:210–6.
Osgood-Zimmerman A, Millear AI, Stubbs RW, Shields C, Pickering BV, Earl L, et al. Mapping child growth failure in Africa between 2000 and 2015. Nature. 2018;555(7694):41–7.
System UN. Nutrition and the Post-2015 Sustainable Development Goals. 2014.
Fryar CD, Gu Q, Ogden CL, Flegal KM. Anthropometric reference data for children and adults: United States, 2011–2014. Vital Health Stat. 2016;3(39):1–46.
Casadei K KJ. Anthropometric Measurement. Treasure Island: StatPearls Publishing; 2021.
Nandy S, Svedberg P. The Composite Index of Anthropometric Failure (CIAF): an alternative indicator for malnutrition in young children. Handbook of anthropometry: physical measures of human form in health and disease. 2012. p. 127–37.
Bose K, Mandal GC. Proposed new anthropometric indices of childhood undernutrition. Malays J Nutr. 2010;16(1):131–6.
Dipierri JE, Román EM, Abdo G. Composite index of anthropometric failure and geographic altitude in children from Jujuy (1 to 5 years old). Arch Argent Pediatr. 2014;112(6):526–31.
Unicef W, World Bank. Levels and trends in child malnutrition: Key findings of the 2020 Edition of the Joint Child Malnutrition Estimates. Geneva: WHO; 2020. p. 2020.
UNICEF/WHO/WorldBankGroup. Joint child malnutrition estimates. Levels and trends in child malnutrition. 2016.
Permatasari TAE, Chadirin Y. Assessment of undernutrition using the composite index of anthropometric failure (CIAF) and its determinants: a cross-sectional study in the rural area of the Bogor District in Indonesia. BMC nutrition. 2022;8(1):133.
EPHI. Ethiopia Mini Demographic and Health Survey. Addis Ababa and Rockville: The DHS Program ICF Rockville, Maryland, USA; 2019.
Al-Sadeeq AH, Bukair AZ, Al-Saqladi AWM. Assessment of undernutrition using Composite Index of Anthropo-metric Failure among children aged< 5 years in rural Yemen. Eastern Mediterranean Health Journal. 2018;24(12):1119–26.
Svedberg P. Poverty and undernutrition: theory, measurement, and policy. New York: Oxford University Press; 2000.
Rasheed W, Jeyakumar A. Magnitude and severity of anthropometric failure among children under two years using Composite Index of Anthropometric Failure (CIAF) and WHO standards. International journal of pediatrics & adolescent medicine. 2018;5(1):24.
Habyarimana F, Zewotir T, Ramroop S. A proportional odds model with complex sampling design to identify key determinants of malnutrition of children under five years in Rwanda. Mediterr J Soc Sci. 2014;5(23):1642.
Fenta HM, Workie DL, Zike DT, Taye BW, Swain PK. Determinants of stunting among under-five years children in Ethiopia from the 2016 Ethiopia demographic and health survey: application of ordinal logistic regression model using complex sampling designs. Clinical Epidemiology and Global Health. 2020;8(2):404–13.
de Onis M, Onyango A, Borghi E, Siyam A, Blössner M, Lutter C. Worldwide implementation of the WHO child growth standards. Public Health Nutr. 2012;15(9):1603–10.
Endris N, Asefa H, Dube L. Prevalence of malnutrition and associated factors among children in rural Ethiopia. Biomed Res Int. 2017;2017:6587853.
Khamis AG, Mwanri AW, Kreppel K, Kwesigabo G. The burden and correlates of childhood undernutrition in Tanzania according to composite index of anthropometric failure. BMC Nutrition. 2020;6(1):1–13.
Nandy S, Miranda JJ. Overlooking undernutrition? Using a composite index of anthropometric failure to assess how underweight misses and misleads the assessment of undernutrition in young children. Soc Sci Med. 2008;66(9):1963–6.
Shit S, Taraphdar P, Mukhopadhyay DK, Sinhababu A, Biswas AB. Assessment of nutritional status by composite index for anthropometric failure: a study among slum children in Bankura, West Bengal. Indian J Public Health. 2012;56(4):305–7.
Mandal G, Bose K. Assessment of overall prevalence of undernutrition using composite index of anthropometric failure (CIAF) among preschool children of West Bengal, India. 2009.
Sen J, Mondal N. Socio-economic and demographic factors affecting the Composite Index of Anthropometric Failure (CIAF). Ann Hum Biol. 2012;39(2):129–36.
Biswas S, Giri SP, Bose K. Assessment of nutritional status by composite index of anthropometric failure (CIAF): A study among preschool children of Sagar Block, South 24 Parganas District, West Bengal. India AnthropologicAl review. 2018;81(3):269–77.
Preedy VR. Handbook of anthropometry: physical measures of human form in health and disease. UK: Springer Science and Business Media; 2012.
Nandy S, Svedberg P. The Composite Index of Anthropometric Failure (CIAF): An alternative indicator for malnutrition in young children. In: Handbook of anthropometry: Physical measures of human form in health and disease. Springer; 2012. p. 127–37.
Bidira K, Tamiru D, Belachew T. Anthropometric failures and its associated factors among preschool-aged children in a rural community in southwest Ethiopia. PLoS ONE. 2021;16(11):e0260368.
Ethiopian Public Health Institute - EPHI, Federal Ministry of Health - FMoH, ICF. Ethiopia Mini Demographic and Health Survey 2019. Addis Ababa: EPHI/FMoH/ICF; 2021.
Bose K. The Concept of Composite Index of Anthropometric Failure (CIAF): Revisited and Revised. 2018.
Wado YD, Gurmu E, Tilahun T, Bangha M. Contextual influences on the choice of long-acting reversible and permanent contraception in Ethiopia: a multilevel analysis. PLoS ONE. 2019;14(1):e0209602.
Kesetebirhan A. National guideline for family planning services in Ethiopia. Ministry of Health: Federal Democratic Republic of Ethiopia; 2011. p. 20–3.
Akombi BJ, Agho KE, Merom D, Renzaho AM, Hall JJ. Child malnutrition in sub-Saharan Africa: a meta-analysis of demographic and health surveys (2006–2016). PLoS ONE. 2017;12(5):e0177338.
Fanzo J. The nutrition challenge in sub-Saharan Africa. Rome: United Nations Development Programme, Regional Bureau for Africa; 2012.
Lartey A. Maternal and child nutrition in Sub-Saharan Africa: challenges and interventions. Proceedings of the Nutrition Society. 2008;67(1):105–8.
Fenta HM, Zewotir T, Muluneh EK. Disparities in childhood composite index of anthropometric failure prevalence and determinants across Ethiopian administrative zones. PLoS ONE. 2021;16(9):e0256726.
Kansal A, Talwar I. Asseessment of Nutritional status by conventional Indices and the composite Index of Anthropometric Failure among children of Parwanoo town (Tehsil Kasauli), Himachal Pradesh, India. Ind J Phys Anthr Hum Genet. 2017;36:177–201.
Dasgupta A, Parthasarathi R, Biswas R, Geethanjali A. Assessment of under nutrition with composite index of anthropometric failure (CIAF) among under-five children in a rural area of West Bengal. Indian J Community Health. 2014;26(2):132–8.
Bejarano IF, Oyhenart EE, Torres MF, Cesani MF, Garraza M, Navazo B, et al. Extended composite index of anthropometric failure in Argentinean preschool and school children. Public Health Nutr. 2019;22(18):3327–35.
Chowdhury MRK, Khan HTA, Rashid M, Mondal MNI, Bornee FA, Billah B. Prevalence and correlates of severe under-5 child anthropometric failure measured by the composite index of severe anthropometric failure in Bangladesh. Front Pediatr. 2022;10:978568.
Tesfaw LM, Woya AA. Potential mediators of the link between wealth index and anthropometric indices of under-five children in Ethiopia. Front Public Health. 2022;10:981484.
Dewey KG, Brown KH. Update on technical issues concerning complementary feeding of young children in developing countries and implications for intervention programs. Food Nutr Bull. 2003;24(1):5–28.
Haile D, Azage M, Mola T, Rainey R. Exploring spatial variations and factors associated with childhood stunting in Ethiopia: spatial and multilevel analysis. BMC Pediatr. 2016;16(1):49.
Akombi B, Agho K, Hall J, Wali N, Renzaho A, Merom D. Stunting, wasting and underweight in sub-Saharan Africa: a systematic review. Int J Environ Res Public Health. 2017;14(8):863.
Ikeda N, Irie Y, Shibuya K. Determinants of reduced child stunting in Cambodia: analysis of pooled data from three demographic and health surveys. Bull World Health Organ. 2013;91:341–9.
Dewey KG, Cohen RJ. Does birth spacing affect maternal or child nutritional status? A systematic literature review. Matern Child Nutr. 2007;3(3):151–73.
Aparajita D, Sahoo SK, Pranita T, Preeti P, Dhiraj B, Amitava K, et al. Composite index of anthropometric failure and its important correlates: a study among under-5 children in a slum of Kolkata, West Bengal, India. International Journal of Medical Science and Public Health. 2015;4(3):414–9.
Assefa T, Belachew T, Tegegn A, Deribew A. Mothers'health care seeking bahavior for childhood illnesses in derra district,northshua zone, oromia regional state, Ethiopia. Ethiop J Health Sci. 2008;18(3):1–8.
Akombi B, Agho K, Merom D, Hall J, Renzaho A. Multilevel analysis of factors associated with wasting and underweight among children under-five years in Nigeria. Nutrients. 2017;9(1): 44.
Balogun OS, Asif AM, Akbar M, Chesneau C, Jamal F. Prevalence and potential determinants of aggregate anthropometric failure among pakistani children: findings from a community health survey. Children. 2021;8(11):1010.
Seboka BT, Hailegebreal S, Yehualashet DE, Demeke AD. Tracking progress in anthropometric failure among under-five children in Ethiopia: a geospatial and multilevel analysis. Archives of Public Health. 2021;79(1):1–17.
Acknowledgements
The authors would like to thank the MEASURE DHS program for providing the data for further analysis. We would also like to thank all who support us directly or indirectly.
Funding
We received funds for this particular study from Wollo University.
Author information
Authors and Affiliations
Contributions
All authors made a substantial contribution to this study. AA and AM: contribute to the conception or design of the work; AA, YAD, SW and AM: contribute to the acquisition, analysis and interpretation of data; AA, TDA, AG and FBG: have drafted the work or substantively revised it. All authors read, revised it critically for important intellectual content, and gave the final approval of the submitted manuscript version. All authors agreed to each contributions and integrity of any part of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Authorization letter was obtained from the MEASURE DHS program to download and use the data for our research purposes. Ethical clearance was obtained from Wollo University. The dataset is publicly available in the MEASURE DHS (www.measuredhs.com) program's official database, with no personal identifiers that can be linked to study participants.
Consent for publication
Not applicable as there is no image or other confidentiality related issues.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ayres, A., Dawed, Y.A., Wedajo, S. et al. Anthropometric failures and its predictors among under five children in Ethiopia: multilevel logistic regression model using 2019 Ethiopian demographic and health survey data. BMC Public Health 24, 1149 (2024). https://doi.org/10.1186/s12889-024-18625-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18625-4