Abstract
Background
Homeless shelters have emerged as components of the social services network, playing an important role in providing health care to the homeless population. The aim of this study was to evaluate an individualized physical therapy intervention for people experiencing homelessness and to determine the relationship between self-perceived variables.
Methods
Pre and post study, setting at the “Santa y Real Hermandad de Nuestra Señora del Refugio y Piedad” homeless shelter in Zaragoza, Spain. Participants were people experiencing homelessness with musculoskeletal disorders who attended a physical therapy service at shelter facilities. A physical therapy program was implemented including health education, exercise and manual therapy, electrotherapy, thermotherapy and bandaging. Demographic variables (age and gender), nationality, employment situation, educational level, pain location, number of painful areas, feeling of loneliness (3-Item Loneliness Scale; values from 3 to 9), pain intensity (Numerical Pain Rating Scale [NPRS]; from 0 to 10) and self-perceived health (Clinical Global Impression [CGI]; from 1 to 7).
Results
Sixty-four homeless people (age of 46.4 ± 10.9 years) participated in the study. Musculoskeletal pain was reported by 98.4% of subjects, with moderate pain intensities (6.1), and 48.4% presenting with pain at multiple sites. Perceptions of loneliness were low (3.7 ± 2.5) and self-perceived health status was moderately ill (3.5 ± 1.7). Positive significant correlations were identified between pain intensity and self-perceived health. The average number of sessions was 1.5 (± 0.8), with manual therapy (35.6%) followed by health education (23.5%) being the most frequently used techniques. Both pain and self-perceived health improved after treatment, even following a brief intervention.
Conclusions
This study demonstrates the potentially negative impact of untreated pain on the self-perceived health of homeless individuals with musculoskeletal disorders that should be targeted for consideration. The findings suggest that a paradigm shift in pain management, including a physical therapy service in shelters, is needed to address the rehabilitation demands of these individuals in a real-life context. This study was approved by the Aragon Ethics Committee (PI19/438) and performed according to the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) statement.
Similar content being viewed by others
Introduction
Worldwide, 1.6 billion people live in inadequate housing conditions, and about 15 million are evicted each year [1]. The homeless population consists of people with no fixed abode, living on the streets, housed in a shelter or in some unstable or non‐permanent situation [2]. Specifically in Spain, sororities and homeless shelters have emerged as components of the social services network, playing an important role in providing health care to the homeless population. In 2022, the Spanish National Institute of Statistics estimated that there had been 28,552 cases of homeless people being treated in homeless shelters [3].
Persons experiencing homelessness (PEH) are exposed to conditions that lead to vulnerability, premature mortality, and difficulty accessing basic services [4, 5]. PEH use emergency services more frequently than other adults [6], with a significantly higher number of visits [7]. However, the low utilization of non-emergency primary health care by this population, is likely due to the differences in social status, the perception of being judged, which can lead to relational barriers, or perhaps the fact that PEH prioritizes finding shelter and food over accessing health and social services, in part because of bureaucracy and rigid hours of operation, among other factors [8].
Despite the high prevalence of musculoskeletal problems among PEH [6], specific physical therapy programs [9] are very scarce. Only two mixed-method studies have conducted a physical therapy intervention with homeless people, with a larger qualitative design focused on qualitative analysis [10, 11]. Location of services and transportation difficulties, as well as cost and waiting times, were the main barriers to accessing physical therapy services [10, 11]. It seems that providing physical therapy services directly at the shelters increase the percentage of people who completed more than one session [10], with the recommendations to work with essentials and take a more flexible approach to provide walk-in physical therapy services [11]. Only one study assessed the effectiveness of treatment based on improvement in quality of life [11].
On the other hand, few studies have focused on the study of pain in these individuals, as the presence of potentially serious pathologies and difficult access to medical services have relegated the examination of pain to the background [12]. However, it has been reported that PEH often suffer to a high degree from pain that limits them physically. PEH are known to report a greater number of barriers which are associated with increased pain intensity and subjective feelings of loneliness and helplessness, which alter subjective perceptions of their health status [13]. These include stress related to shelter life and poor sleeping conditions.
Self-perceived health (SPH) or self-rated health is a subjective measure of a person´s health status, that includes psychosocial and physical aspects as well as cultural and socioeconomic factors in the general population [13]. It is closely related to morbidity and disability, although it can also be a robust predictor of mortality and measure a global health status [13]. Among objective determinants of health, the presence of a chronic disease is one of the greatest predictors of worse self-perceived health for both females and males aged 50–64 years old [14]. Furthermore, the impact of health conditions is mediated through symptoms: the health conditions themselves are likely less important than their symptoms for determining SPH. In particular, pain is a relevant factor in those with the worst SPH [15]. Among social determinants of SPH, age plays a relevant role, but low educational level, unemployment, and low levels of physical activity are associated with poor SPH regardless of generation and gender [16,17,18]. This underlies the impact of social inequalities in SPH [19]. Factors associated with better SPH in PEH are being male; living abstinently; holding a health card [20]; adequate sleep; and having fewer chronic health conditions [21].
There is a gap in the literature, where authors such as Kiernan et al., propose that measurement methods should be evaluated specifically for these individuals, as well as research into appropriate rehabilitation and support interventions for this vulnerable population [22]. To the authors' knowledge, there are few studies that have performed a quantitative analysis of a comprehensive physical therapy intervention in shelters for PEH with musculoskeletal disorders; and none evaluated the SPH of these PEH in a musculoskeletal clinical context [4]. Our proposal was to develop a standard physical therapy intervention that was accessible to PEH by applying it in response to immediate demand in shelters.
The aim of this study is to evaluate an individualized physical therapy intervention for people experiencing homelessness and to determine the relationship between self-perceived variables (loneliness and helplessness, pain, and self-perceived health status).
Material and methods
Study design
A pre-post intervention study was performed according to the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) statement [23]. This study was approved by the Aragon Ethics Committee (PI19/438).
Participants
Subjects eligible for this study were homeless and temporarily sleeping in a homeless shelter (“Santa y Real Hermandad de Nuestra Señora del Refugio y Piedad”) in Zaragoza, Spain. They were invited by the medical staff to participate in the study if they met the eligibility criteria. All participants provided signed informed consent before the start of the evaluation process.
Inclusion criteria were the following: 1) age over 18 years; 2) people experiencing homelessness 3) having an identifiable musculoskeletal disorder that can be treated by physical therapy according to medical criteria (for example, pain, muscle tenderness or atrophy, joint sprain, or loss of range of motion). The exclusion criteria were: 1) inability to follow instructions or cooperate in the performance of the examination, either due to language barrier or because of cognitive impairment; 2) presence of signs indicative of a medical emergency (for example, signs of fracture, acute disc extrusion, acute medullary or nerve compression); 3) presence of severe psychiatric disorders (for example, schizophrenia, bipolar disorder, substance abuse, etc.) The above criteria were assessed by medical examination at the shelter consultation and by clinical history of the homeless people.
Variables and data measurements
Data were collected by physical therapy staff between March 2018 and February 2020 through interviews in the following standardized order.
Sociodemographic and clinical assessment
At the beginning of physical therapy session, sociodemographic data such as age, gender, nationality, education level, and employment situation were collected.
A clean body chart (anterior and posterior views) was used to document pain and symptom localization [24]. Subsequently, the body charts were divided into different sections to obtain two variables: (i) pain/symptom localization, a qualitative record of the name of the area(s) in which participants reported the presence of pain/symptoms (e.g., cervical spine or upper extremity), and (ii) the number of painful areas, a numerical measure of the number of different areas in which participants marked the presence of pain [24]. The multisite pain category was used when participants reported pain in more than one area [25, 26].
Self-perceived outcomes
Feelings of loneliness and helplessness was assessed with the Three Item Loneliness Scale. This scale has satisfactory reliability and both concurrent and discriminant validity [27]. It also explores objective and subjective social isolation and is appropriate in this context because it measures general loneliness well using three items and a simplified set of response categories [28]. The scale asks how often respondents feel they have no company; feel excluded; and feel isolated from others. Items are rated on a scale of 1 (almost never) to 3 (often) and summed to a score of 3 to 9, with higher scores reflecting greater loneliness [29].
The intensity of musculoskeletal pain was assessed with the 11-point Numerical Pain Rating Scale (NPRS) [24], commonly used to assess pain with scores from 0 to 10 and definitions of 0 = no pain and 10 = worst pain imaginable. Participants were asked to rate the mean pain intensity to evaluate the current pain experience. Self-perceived health status was assessed using the Clinical Global Impression Scale (CGI). The CGI is a classic instrument used to assess psychiatric disorders with strong validity, although it has also been used in other clinical settings [30]. The CGI asked participants to assess their self-perceived health status at that time. The CGI comprises two companion one-item measures with a 7-point Likert rating scale evaluating the following: (a) independent severity of illness (assessment of a patient's current symptom severity) (CGI-S) from 1 to 7, where 1 = normal, not ill, 2 = borderline ill, 3 = minimally ill, 4 = moderately ill, 5 = markedly ill, 6 = severely ill, and 7 = among the most extremely ill patients; and (b) change from the initiation of treatment (CGI-I) on a similar seven-point scale, where 1 = very much improved, 2 = much improved, 3 = minimally improved, 4 = no change, 5 = minimally worse, 6 = much worse and, 7 = very much worse [31, 32]. The question used for the CGI-S was: “How sick do you currently feel? and for the CGI-I: “How much change have you felt after the received care?”. The CGI will be classified into the following categories based on CGI-S scores: normal (1), low (2–3), moderate (4), and severe (5–7) self-perceived health status.
As these are subjective assessments, the assessors were trained to homogenize the explanations they give to the patients.
Treatment satisfaction
To assess satisfaction with the physical therapy program, participants were presented with an ad-hoc 5-point Likert questionnaire, between 1 = none and 5 = very much.
The questions were: a) General: 1) The intervention performed was appropriate for me; 2) The professionalism of the physical therapists was appropriate; and 3) The attitude, interest, and treatment of the physical therapists were appropriate. Physical factors were assessed in section b): 4) I experienced an improvement in my general condition; 5) My pain, tension, etc. reduced. Psychological factors were assessed in section c): 6) I gained personal satisfaction from participating in this project; 7) My expectations from the intervention carried out were met; and d) Educational factors: 8) I increased my knowledge about health; and 9) I will be able to use the acquired knowledge later.
Procedure
Patients were treated in the shelter facilities. The physical therapy program took place twice a week during the medical consultation hours. The number of sessions was based on the length of stay in the facility, which was a maximum of 1 month for each person (maximum of eight sessions). The sessions lasted about 20 to 30 min, depending on the needs identified and the type of therapy carried out.
To determine the appropriate type of intervention, a routine examination was performed in which functional tests were performed, such as active movement without pain, final sensation during passive movement, translational joint play, muscle assessment (length, and strength per the Medical Research Council Scale), and provocation-relief tests.
The number and type of techniques used were recorded.
Intervention
The intervention was carried out by 5 physical therapists trained in musculoskeletal physical therapy and based on standard physical therapy sessions.
According to the results of the assessment, different physical therapy techniques were selected and applied for each subject, who could receive one or more interventions in the same session: 1) Health education, with analysis of postural habits and promoting awareness behaviors [33]; 2) Exercise therapy, featuring movement as a therapeutic intervention and focusing on therapeutic exercise to recover flexibility, strength and endurance [34]; 3) Manual therapy, for the treatment of musculoskeletal pain [35]; 4) Electrotherapy using transcutaneous electrical nerve stimulation (TENS) as an analgesic technique [36]; 5) Thermotherapy, or the application of heat with Infra-Red (IR) light to increase blood circulation in the affected areas [37], and 6) Bandaging with functional and neuromuscular bandages as required [38].
Statistical analysis
Statistical analysis was conducted using IBM SPSS Statistics for Windows, Version 28.0 (IBM Corp, Armonk, NY, USA), and SigmaPlot, Version 14.0 (Systat Software, Canada). For the descriptive analysis, numbers (percentages), mean and standard deviation (SD), or median and interquartile range were used.
The normality of the quantitative data was checked for using the Shapiro–Wilk test.
Differences between variables by nationality and gender were analyzed using the Mann–Whitney U test or the Chi-square test, depending on the nature of the variables.
Spearman’s rank correlations were carried out to examine the relationship between variables. The strength of correlations was interpreted as either low (0.00 – 0.25), fair (0.26 – 0.50), moderate to good (0.51 – 0.75), and good to excellent (> 0.75) [39].
The Wilcoxon test was applied to highlight the differences between pre- and post-intervention data measurements. The Cohen effect size was also calculated with the following interpretation: trivial (< 0.2), small (0.2 to 0.5), moderate (> 0.5 to 0.8), and large (> 0.8) [40].
The statistical analysis was conducted at a 95% confidence level. Statistical significance was set at p < 0.05.
Results
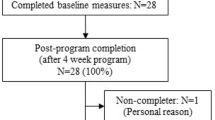
Sixty-four homeless individuals who required physical therapy were included in this study (Fig. 1). Almost all participants had musculoskeletal pain without any other serious diagnosis, except for three individuals with pain due to stroke, knee sprain, and ankle fracture, respectively.
Baseline sociodemographic and clinical characteristics
Baseline and clinical demographic characteristics of the participants by gender and nationality are shown in Table 1. No statistically significant differences were found between genders and nationalities (p > 0.05).
The mean age of participants was 46.4 ± 10.9 years (range: 39.5 to 54.5 years), with four (6.2%) females (age 44.8 ± 3.8 years) and 60 (93.8%) males (age 46.5 ± 11.3 years). Regarding nationality, most (54.7%) had been born in Spain, followed by Algeria (12.5%), Colombia (9.4%), Morocco (6.3%), Romania (6.3%), or other countries (10.8%). All participants had no qualifications or had only completed primary education. Of all participants, 41 (64.04%) were unemployed, 13 (20.3%) had temporary employment, four (6.3%) were retired, and six (9.4%) had a disability (Table 1).
Sixty-three participants (98.4%) reported musculoskeletal pain at baseline with a mean intensity of 6.1 ± 2.1, and 44% of participants reported severe pain (≥ 7/10 in the NPRS).
The body region most affected by musculoskeletal pain was the lower limbs (35.9% of participants), followed by the cervical spine (23.4%), upper extremities (23.4%), and finally lower back (18.8%) and chest (18.8%). 48.4% reported multisite pain. The mean number of painful areas for each participant was 1.6 ± 0.8 (Table 1).
Regarding health status at baseline, 54.6% of participants scored 3 or higher on the CGI-S scale, with a mean score value of 3.5 ± 1.7 (moderately ill), indicating poor self-perceived health status in the sample. Although females reported worse health status, with a status of "severely ill" as opposed to a status of "moderately ill" in men, this difference was not statistically significant (p > 0.05). Self-perceived health status did not differ between Spanish and non-Spanish individuals.
Regarding perceptions of loneliness and helplessness, feelings of loneliness were not prevalent in this study sample. The mean score on the three-item loneliness scale was 3.7 ± 2.5, with females scoring higher. Spanish participants had a higher score (+ 0.4) than participants born elsewhere (Table 1).
Correlations
A moderate to good statistically significant correlation was observed between pain intensity (NPRS) and perception of health status (CGI-S). More severe musculoskeletal pain was associated with a worse perception of health status at baseline (rho = 0.539, p < 0.001).
There were no other significant correlations among the other variables (p > 0.05).
When the ranges of health state perception scores were compared with pain intensity, the highest pain intensity scores were found for moderate and severe CGI-S scores (Table 2).
Changes to NPRS and CGI following physical therapy intervention
A total of 230 physical therapy interventions were performed, with manual therapy being the most used (82 interventions), followed by health education (54 interventions), bandages (36 interventions), thermotherapy (32 interventions), exercise therapy (17 interventions), and electrotherapy (9 interventions).
Overall, the average number of interventions for each participant was 1.5 ± 0.8 sessions: 59.4% of participants received one session (n = 38); 34.4% (n = 22) received two sessions; 3.1% (n = 2) received three sessions; and 1.6% (n = 1) received five sessions. The number of sessions each participant received was unrelated to baseline variables or pre-and post- intervention variables. There was also no difference between participants who attended only one intervention (59.4%) and those who attended more than one (40.6%).
Despite not being statistically significant, all females (n = 4) attended only one session. The attendance of Spanish and non-Spanish subjects was similar (p > 0.05).
Regarding pain intensity according to the NPRS, the mean score at the end of treatment was 4.2 ± 2.3 (median 4, IQR 2.8–6). There was a statistically significant reduction of 1.9 ± 1.7 points (p < 0.001) with a moderate magnitude in terms of effect size (d = 0.633) (Fig. 2).
When considering the whole sample, there was a statistically significant improvement in mean self-perceived health status of 0.9 ± 2.0 points (p = 0.005) from moderately ill (3.5 ± 1.7; median 4, IQR 2–5) to moderately better (2.5 ± 1.1; median 2, IQR 2–3). The effect size indicated a small difference between the baseline score and the score after the physical therapy intervention (d = 0.352) (Fig. 3). A strong correlation was found, indicating greater improvement in self-perceived health among those who reported poorer health status at baseline (rho = 0.84, p < 0.001), and a moderate association with relief of musculoskeletal pain (rho = 0.41, p < 0.01).
Although not statistically significant, females reported greater positive effects of the intervention compared with males, both in terms of self-perceived health status and musculoskeletal pain intensity (p > 0.05). However, Spanish, and non-Spanish participants experienced similar improvements after the intervention with no differences (p > 0.05).
Treatment satisfaction
The mean evaluation score of the intervention and the professionalism of the physical therapy team was 4.7 ± 0.3 out of 5. In relation to physical, psychological, and educational factors, the mean scores were 4.6 ± 0.4, 4.7 ± 0.3, and 4.5 ± 0.4, respectively, out of 5.
Discussion
This is the first study to specifically examine self-perceived variables in PEH attending a physical therapy consultation at shelter facilities which also evaluated the effectiveness of physical therapy interventions. Sixty participants (93.8%) were male and four (6.2%) were female, with an overall mean age of 46.4 years. Pain at baseline was present in 98.4% of participants. The level of basal pain intensity was moderate (6.1). Pain at multiple sites was reported by 48.4% of participants. At baseline, there was a low perception of loneliness (3.7) and a moderate perception of illness (3.5). Homeless individuals who were not born in Spain did not have greater pain, were not lonelier, and did not have worse self-perceived health than Spanish PEH. There was a significant association between pain and self-perceived health status.
Pain
Of the selected participants, all but one reported musculoskeletal pain, and in almost half of them the pain was severe, with pain intensity equal or greater than 7 points on the NRPS. We found lower intensity of pain compared to the other studies of PEH, which were focused on chronic pain [12, 41]. The most affected body regions were the lower limbs, followed by the spine, which is consistent with previous findings and may be due to the lack of a permanent residence, which means having to stand and walk for long periods and carry the weight of one´s belongings [12, 42]. Both the intensity and location of pain are important variables in the study of people living with pain. In particular, the presence of pain at multiple locations is considered to be a prognostic factor for chronic conditions [43, 44]. The present study provides new data on this: multisite pain was present in 48.4% of patients, which is higher than the figures obtained in the general population and similar to the elderly [45]. Pain improvement after therapy was at the limit of minimal clinically relevant change (1.9 ± 1.7 points), but significant, even after a short treatment (many cases only received one session). The same outcome measurement was used by Oosman [11], the only study that has reported differences in pain before and after a session of physical therapy, where pain intensity was assessed as a subdomain of the EQ-5D-5L and minimal clinically non-relevant changes were noted after treatment (0.25 points in the pain domain of 5D-QoL). The results of our study highlight the need to identify and treat pain in this underserved population from another approach. Pharmacological treatments in this group may not be a princeps treatment due to difficulties in prescribing psychotropic drugs in PEH, who are especially vulnerable to the mishandling of this type of substance. Pain cannot be disregarded in this population, as they can equally benefit from therapeutic strategies, especially given the extreme impact of pain and poor health in this vulnerable group.
Self-perceived health
Poor health perception was reported by most participants irrespective of age, nationality, or gender; worse health correlated with higher pain intensities. We observed poorer perceived health status in our sample compared with the limited research that exists measuring self-perceived health among homeless people. We reported 54.6% with poor or very poor SPH (moderate and severe illness perception) compared to the 39.7% with poor or very poor SPH in a national survey study of 2,437 adults in Spain [20], or the 76% with good or very good SPH of 244 homeless adults living in an emergency shelter in Dallas [46]. Neither of these studies were performed in a clinical context, and our question differed because it related to the perception of severity of poor health when being in a health consultation and was not asked in a positive way (the question was made in terms of illness and not in terms of health). In another study of 421 individuals in Los Angeles (USA), it was found that self-rated general health status of PEH improved when they moved to permanent supportive housing. However, this was not the case if they suffered from physical limitations that did not improve until six months after moving to permanent supportive house, and poor self-perceived health was related to the number of chronic health conditions [21]. Of note in our study, not only was higher pain intensity associated with poorer SPH, but its improvement was also associated with lower perceived pain intensity after treatment.
The physical therapy intervention
A total of 230 physical therapy interventions were carried out. Manual therapy (35.6%) and health education (23.5%) were the most frequently used, the median number of sessions was 1.5 (± 0.8). It can be difficult to assess the impact of physical therapy treatments in PEH due to their unstable lifestyle, which makes it difficult to schedule sessions at a specific location, resulting in irregular attendance. This is an important aspect of the PEH condition that may affects the usual form of health care. However, the only two studies which evidence physical therapy interventions used the form of scheduled sessions, although the details of the interventions are not clearly explained. In our study 41% received at least two sessions despite not providing fixed appointments and left it to the demand or need of the patients themselves and/or the circumstances of their stay in the accommodation. Our design follows the recommendations of Oosman [11], who uses a non-schedule-based care model. It seems that the accessibility of place of care facilities is more important than the number of scheduled sessions in increasing participation. It is likely that rehabilitative needs are not being met through traditional models of care [47].
Our main intervention was manual therapy (35.65%) followed by health education, in contrast to Dawes [10] and Oosman [11], where health education and self-care strategies (advice and exercise), respectively, were most frequently used. The type of technique or treatment does not appear to have affected adherence, as the number of sessions was similar to those reported by Oosman [11] or Dawes [10] (both with a median of 2 visits per patient), with the location of use being more important than the type of treatment applied. As mentioned above, the type of intervention may have influenced the relevant improvement in pain observed in our study.
Limitations
This study has several limitations that we would like to highlight. Given the subjective nature of the assessment tools used, a qualitative assessment would have been interesting to contrast and complement the quantitative results obtained. We did not collect information on comorbidities or psychosocial factors that may affect pain severity and self-perceived health. We did not specifically evaluate neuropathic pain. The post-treatment evaluations have been adapted to the reality and availability of the PEH, so they had to be carried out just after the treatment session. Due to the multiplicity of consultations and taking into account the already expressed difficulty for this population to attend another new consultation, we have neither been able to solve the limitation of not using of separate researcher to administer the questionnaires. Further studies are needed to be conducted in different shelters in Spain, with a larger sample size, with a control group and a follow-up.
Conclusions
This study showed a significant improvement in pain and self-perceived health status after a physical therapy intervention, as well as a relationship between these variables. These results highlight the importance of including physical therapy in an accessible model of care service. Further research is needed to evaluate a specific approach to pain management from various perspectives that should be considered in this population.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
United Nations. Fifty-eighth session Commission for Social Development. 2020; Available from: https://www.un.org/development/desa/dspd/2020/02/csocd58-concluded/.Cited 2023 15 september 2023.
Omerov P, Craftman ÅG, Mattsson E, Klarare A. Homeless persons’ experiences of health- and social care: A systematic integrative review. Health Soc Care Community. 2020;28(1):1–11. https://doi.org/10.1111/hsc.12857.
INE. Instituto Nacional de Estadística. Encuesta sobre las personas sin hogar. 2013; Available from: http://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176817&menu=ultiDatos&idp=1254735976608.
Bedmar MA, Bennasar-Veny M, Artigas-Lelong B, Salvà-Mut F, Pou J, Capitán-Moyano L, et al. Health and access to healthcare in homeless people: Protocol for a mixed-methods study. Medicine (Baltimore). 2022;101(7):e28816. https://doi.org/10.1097/md.0000000000028816.
Hyun M, Bae SH, Noh D. Systematic review and meta-analyses of randomized control trials of the effectiveness of psychosocial interventions for homeless adults. J Adv Nurs. 2020;76(3):773–86. https://doi.org/10.1111/jan.14275.
Kale NN, Marsh J, Kale NK, Miskimin C, Mulcahey MK. Musculoskeletal Injuries and Conditions Among Homeless Patients. J Am Acad Orthop Surg Glob Res Rev. 2021;5(11). https://doi.org/10.5435/JAAOSGlobal-D-21-00241.
Dorney-Smith S, Schneller K, Swift A, Phelan H, Khan Z. Meeting the needs of homeless people attending the emergency department. Emerg Nurse. 2020;28(4):31–9. https://doi.org/10.7748/en.2020.e2025.
Davies A, Wood LJ. Homeless health care: meeting the challenges of providing primary care. Med J Aust. 2018;209(5):230–4. https://doi.org/10.5694/mja17.01264.
Fraser KA, Nguyen H, Kim S, Park F, Bernal J, Westberg AD, et al. Perceptions of nonopioid treatment for pain in a homeless population. J Osteopath Med. 2021;121(7):643–9. https://doi.org/10.1515/jom-2020-0239.
Dawes J, Deaton S, Greenwood N. Homeless people’s access to primary care physiotherapy services: an exploratory, mixed-method investigation using a follow-up qualitative extension to core quantitative research. BMJ Open. 2017;7(6):e012957. https://doi.org/10.1136/bmjopen-2016-012957.
Oosman S, Weber G, Ogunson M, Bath B. Enhancing Access to Physical Therapy Services for People Experiencing Poverty and Homelessness: The Lighthouse Pilot Project. Physiother Can. 2019;71(2):176–86. https://doi.org/10.3138/ptc.2017-85.pc.
Fisher R, Ewing J, Garrett A, Harrison EK, Lwin KK, Wheeler DW. The nature and prevalence of chronic pain in homeless persons: an observational study. F1000Res. 2013;2:164. https://doi.org/10.12688/f1000research.2-164.v1.
Wu S, Wang R, Zhao Y, Ma X, Wu M, Yan X, et al. The relationship between self-rated health and objective health status: a population-based study. BMC Public Health. 2013;13:320. https://doi.org/10.1186/1471-2458-13-320.
Gumà J. What influences individual perception of health? Using machine learning to disentangle self-perceived health. SSM Popul Health. 2021;16:100996. https://doi.org/10.1016/j.ssmph.2021.100996.
Olsson M, Currow DC, Ekström MP. Exploring the most important factors related to self-perceived health among older men in Sweden: a cross-sectional study using machine learning. BMJ Open. 2022;12(6):e061242. https://doi.org/10.1136/bmjopen-2022-061242.
Aguilar-Palacio I, Gil-Lacruz AI, Sánchez-Recio R, Rabanaque MJ. Self-rated health in Europe and its determinants: Does generation matter? Int J Public Health. 2018;63(2):223–32. https://doi.org/10.1007/s00038-018-1079-5.
Gumà J, Arpino B, Solé-Auró A. Determinantes sociales de la salud de distintos niveles por género: educación y hogar en España. Gac Sanit. 2019;33(2):127–33. https://doi.org/10.1016/j.gaceta.2017.11.010.
Gumà-Lao J, Arpino B. A machine learning approach to determine the influence of specific health conditions on self-rated health across education groups. BMC Public Health. 2023;23(1):131. https://doi.org/10.1186/s12889-023-15053-8.
Pedrós Barnils N, Eurenius E, Gustafsson PE. Self-rated health inequalities in the intersection of gender, social class and regional development in Spain: exploring contributions of material and psychosocial factors. Int J Equity Health. 2020;19(1):85. https://doi.org/10.1186/s12939-020-01202-7.
Fajardo-Bullón F, Esnaola I, Anderson I, Benjaminsen L. Homelessness and self-rated health: evidence from a national survey of homeless people in Spain. BMC Public Health. 2019;19(1):1081. https://doi.org/10.1186/s12889-019-7380-2.
Rhoades H, Wenzel SL, Henwood BF. Changes in Self-Rated Physical Health After Moving Into Permanent Supportive Housing. Am J Health Promot. 2019;33(7):1073–6. https://doi.org/10.1177/0890117119849004.
Kiernan S, Mockler D, C NC, Broderick J. Physical functioning limitations and physical activity of people experiencing homelessness: A scoping review. HRB Open Res. 2020;3:14. https://doi.org/10.12688/hrbopenres.13011.2.
Des Jarlais DC, Lyles C, Crepaz N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004;94(3):361–6. https://doi.org/10.2105/ajph.94.3.361.
Saltychev M, Laimi K. Predicting self-reported disability level by a number of pain sites marked on pain drawing. Int J Rehabil Res. 2018;41(3):276–9. https://doi.org/10.1097/mrr.0000000000000293.
Butera KA, Roff SR, Buford TW, Cruz-Almeida Y. The impact of multisite pain on functional outcomes in older adults: biopsychosocial considerations. J Pain Res. 2019;12:1115–25. https://doi.org/10.2147/jpr.S192755.
Ntani G, Coggon D, Felli VE, Harari F, Barrero LH, Felknor SA, et al. Patterns of change of multisite pain over 1 year of follow-up and related risk factors. Eur J Pain. 2022;26(7):1499–509. https://doi.org/10.1002/ejp.1978.
Elphinstone B. Identification of a Suitable Short-form of the UCLA-Loneliness Scale. Aust Psychol. 2018;53(2):107–15. https://doi.org/10.1111/ap.12285.
Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A Short Scale for Measuring Loneliness in Large Surveys: Results From Two Population-Based Studies. Res Aging. 2004;26(6):655–72. https://doi.org/10.1177/0164027504268574.
Robinson-Whelen S, Taylor HB, Feltz M, Whelen M. Loneliness Among People With Spinal Cord Injury: Exploring the Psychometric Properties of the 3-Item Loneliness Scale. Arch Phys Med Rehabil. 2016;97(10):1728–34. https://doi.org/10.1016/j.apmr.2016.04.008.
Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont). 2007;4(7):28–37.
Dixon S, Poole CD, Odeyemi I, Retsa P, Chambers C, Currie CJ. Deriving health state utilities for the numerical pain rating scale. Health Qual Life Outcomes. 2011;9:96. https://doi.org/10.1186/1477-7525-9-96.
Jones RM, Patel K, Moscovici M, McMaster R, Glancy G, Simpson AIF. Adaptation of the Clinical Global Impression for Use in Correctional Settings: The CGI-C. 2019;10(687). https://doi.org/10.3389/fpsyt.2019.00687.
Hernández Sánchez J, Lozano García L, Murillo Varela Y. Experiencias de educación para la salud en fisioterapia. Universidad y Salud. 2016;18(3):576–85. https://doi.org/10.22267/rus.161803.63.
Cuesta-Vargas AI, García Romero JC, Labajos Manzanares MT, González-Sánchez M. Patología musculoesquelética y ejercicio terapéutico: eficacia e implantación. Revista Internacional de Medicina y Ciencias de la Actividad Física y del Deporte. 2010;10(40):594–608.
Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Man Ther. 2009;14(5):531–8. https://doi.org/10.1016/j.math.2008.09.001.
Johnson M, Martinson M. Efficacy of electrical nerve stimulation for chronic musculoskeletal pain: a meta-analysis of randomized controlled trials. Pain. 2007;130(1–2):157–65. https://doi.org/10.1016/j.pain.2007.02.007.
Logan CA, Asnis PD, Provencher MT. The Role of Therapeutic Modalities in Surgical and Nonsurgical Management of Orthopaedic Injuries. J Am Acad Orthop Surg. 2017;25(8):556–68. https://doi.org/10.5435/jaaos-d-15-00348.
Mostafavifar M, Wertz J, Borchers J. A systematic review of the effectiveness of kinesio taping for musculoskeletal injury. Phys Sportsmed. 2012;40(4):33–40. https://doi.org/10.3810/psm.2012.11.1986.
Portney L, Watkins M. Foundations of Clinical Research: Applications to Practice 3rd. Edition. New York: Pearson/Prentice Hall Health; 2009. p. 892.
Fritz CO, Morris PE, Richler JJ. Effect Size Estimates: Current Use, Calculations, and Interpretation. J Exp Psychol Gen. 2012;141(1):30. https://doi.org/10.1037/a0026092.
Hwang SW, Wilkins E, Chambers C, Estrabillo E, Berends J, MacDonald A. Chronic pain among homeless persons: characteristics, treatment, and barriers to management. BMC Fam Pract. 2011;12:73. https://doi.org/10.1186/1471-2296-12-73.
de Campos AG, da Silva VE, Seeley M, Leão ER. Pain in Brazilian people experiencing homelessness. Pain Rep. 2019;4(6):e792. https://doi.org/10.1097/pr9.0000000000000792.
Fillingim RB, Loeser JD, Baron R, Edwards RR. Assessment of Chronic Pain: Domains, Methods, and Mechanisms. J Pain. 2016;17(9 Suppl):T10-20. https://doi.org/10.1016/j.jpain.2015.08.010.
Artus M, Campbell P, Mallen CD, Dunn KM, van der Windt DA. Generic prognostic factors for musculoskeletal pain in primary care: a systematic review. BMJ Open. 2017;7(1):e012901. https://doi.org/10.1136/bmjopen-2016-012901.
Bokermann J, König HH, Hajek A. Pain: its prevalence and correlates among the oldest old. Aging Clin Exp Res. 2024;36(1):2. https://doi.org/10.1007/s40520-023-02653-y.
Chang HL, Fisher FD, Reitzel LR, Kendzor DE, Nguyen MA, Businelle MS. Subjective sleep inadequacy and self-rated health among homeless adults. Am J Health Behav. 2015;39(1):14–21. https://doi.org/10.5993/ajhb.39.1.2.
Carroll Á, O'Brien S, Harrington D, Cheallaigh CN, Lawlee AM, Sukumar P. The Unmet Rehabilitation Needs in an Inclusion Health Integrated Care Programme for Homeless Adults in Dublin, Ireland. Int J Environ Res Public Health. 2021;18(15). https://doi.org/10.3390/ijerph18157917.
Acknowledgements
We would like to thank the services of the "Santa y Real Hermandad de Nuestra Señora del Refugio y Piedad" homeless shelter and the study participants for their time and for taking part in this study.
Funding
This project received a grant for the development of Service-learning projects awarded by the Universidad San Jorge and the Fundación Ibercaja, as well as the Universitate 2022 Award.
Author information
Authors and Affiliations
Contributions
SPP and CJS were involved in the concept and the design of the study. All of the authors contributed to the literature search. SPP and CJS executed the study and collected the data. CJS and RFR performed data management and statistical analysis. SPP, SCC and RFR drafted the manuscript. NBC, RLU and MFG contributed to revisions of the paper. All authors have read and approved the final version of the manuscript accepted for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Aragon Ethics Committee (PI19/438). Informed consent was obtained from all subjects involved in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiménez-Sánchez, C., la Cruz, N.Bd., Lafuente-Ureta, R. et al. Physical therapy interventions for people experiencing homelessness to improve pain and self-perceived health status. BMC Public Health 24, 993 (2024). https://doi.org/10.1186/s12889-024-18453-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18453-6