Abstract
Background
Benzodiazepines are a class of medications that are being frequently prescribed in Canada but carry significant risk of harm. There has been increasing clinical interest on the potential “sparing effects” of medical cannabis as one strategy to reduce benzodiazepine use. The objective of this study as to examine the association of medical cannabis authorization with benzodiazepine usage between 2013 and 2021 in Alberta, Canada.
Methods
A propensity score matched cohort study with patients on regular benzodiazepine treatment authorized to use medical cannabis compared to controls who do not have authorization for medical cannabis. A total of 9690 medically authorized cannabis patients were matched to controls. To assess the effect of medical cannabis use on daily average diazepam equivalence (DDE), interrupted time series (ITS) analysis was used to assess the change in the trend of DDE in the 12 months before and 12 months after the authorization of medical cannabis.
Results
Over the follow-up period after medical cannabis authorization, there was no overall change in the DDE use in authorized medical cannabis patients compared to matched controls (− 0.08 DDE, 95% CI: − 0.41 to 0.24). Likewise, the sensitivity analysis showed that, among patients consuming ≤5 mg baseline DDE, there was no change immediately after medical cannabis authorization compared to controls (level change, − 0.04 DDE, 95% CI: − 0.12 to 0.03) per patient as well as in the month-to-month trend change (0.002 DDE, 95% CI: − 0.009 to 0.12) per patient was noted.
Conclusions
This short-term study found that medical cannabis authorization had minimal effects on benzodiazepine use. Our findings may contribute ongoing evidence for clinicians regarding the potential impact of medical cannabis to reduce benzodiazepine use.
Highlights
• Medical cannabis authorization had little to no effect on benzodiazepine usage among patients prescribed regular benzodiazepine treatment in Alberta, Canada.
• Further clinical research is needed to investigate the potential impact of medical cannabis as an alternative to benzodiazepine medication.
Similar content being viewed by others
Background
Benzodiazepines are anxiolytic medications which are known for their sedative properties in the treatment of anxiety [1]. When first introduced on the market, clinicians enthusiastically prescribed benzodiazepines, quickly becoming one of the most widely prescribed medications [2]. Benzodiazepines have a relaxing or calming effect, which is beneficial in the treatment of anxiety. Benzodiazepines can also relieve severe emotional distress, such as panic attacks. Alongside its benefits, also comes a list of side effects associated with the medication [3]. The most reported side effect is drowsiness and hence they are often used as sleep aids. Other side effects include impaired coordination, slurred speech, confusion, disorientation, dizziness, decreased blood pressure and respiratory rate, and memory problems [4]. Long-term use of the medication, particularly in the elderly population, has been associated with cognitive impairment and increased risk of falls [5].
To date, an increasing number of benzodiazepines are being misused by patients and prescription percentages have aligned with patients’ increased risk of dependence on this medication [6]. While over 1 million benzodiazepine prescriptions were dispensed in Alberta in 2021 alone [7]. Prescribing are seemingly decreasing (4% of Albertans received a benzodiazepine or Z-drug [zopiclone, zaleplon, and zolpidem] prescription in 2021 compared to 9.1% in 2016 – a drop of almost one fifth), in which medical cannabis use may be playing a role in circumventing benzodiazepine usage [7]. Nevertheless, benzodiazepine prescribing continues to be high in Alberta.
Among the top reasons for medical cannabis use has been an increasing clinical interest in its “sparing effect” on reducing the use of other medications, specifically benzodiazepines (as well as opioids) [8]. Literature that supports the use of medical cannabis as a substitution for benzodiazepines is currently low; and studies assessing medical cannabis’ association with anxiety report inconclusive or mixed results [9,10,11]. One small randomized controlled trial (RCT) investigating 24 patients with generalized social anxiety disorder showed a reduction in public speaking anxiety with the use of cannabidiol (CBD), a therapeutic component of cannabis [12]. Conversely, there are concerns cannabis can actually increase anxiety levels. One study reported cannabis use increased the risk for more severe anxiety symptoms [13], however, a meta-analysis showed that cannabis was only a minor risk factor for increased anxiety [14]. This lack of consensus of cannabis use for anxiety may also be attributed to the inconsistent nature of the current available literature. Previous studies either tend to strongly focus on the negative effects of cannabis and anxiety (rather than searching for how cannabis may improve anxiety) [15,16,17,18], consist of age-specific and small cohort sizes [13, 19,20,21,22,23], did not differentiate cannabis from other illicit substances [24, 25], or cannot accurately distinguish cannabis for medical purposes versus recreational where non-medical use which often occur in the context of other drug use [26, 27]. Consequently, the current clinical practice guidelines for medical cannabis for Canadian physicians do not support its use for anxiety and other mental health conditions [28].
The legalization of recreational cannabis in October 2018 has led to an increased interest in medical cannabis use, including its use for anxiety and its “sparing effect” for benzodiazepines (and opioids) [29]. Concurrent with the high prevalence of benzodiazepine prescribing, it is imperative to fully investigate the harms and benefits of medical cannabis in order for clinicians and patients to make the best-informed decisions. Thus, the purpose of this study was to examine the association of medical cannabis authorization on benzodiazepine usage in the Alberta population. We hypothesize that medical cannabis authorization would be associated with a reduction in chronic benzodiazepine use (i..e, reduction in daily dose).
Methods
Study design
A matched cohort study with patients on regular benzodiazepine treatment authorized to use medical cannabis and controls who do not have authorization for medical cannabis.
Data source
The College of Physicians and Surgeons of Alberta provided the medical cannabis patient identifiers as they are the regulatory entity for cannabis authorization in the province. Through the use of unique lifetime personnel health numbers, all patients were linked to the administrative databases of Alberta Health which captures all healthcare utilization for all patients in the province of Alberta as part of the universal health insurance plan for residents. These databases included provincial health care registry, vital statistics, all inpatient hospitalizations, ambulatory emergency department visits, all community pharmacy drug dispensations, and physician claims data, providing at least one-year of longitudinal follow-up data following the index date for both patients authorized to access medical cannabis and high dimensional propensity score matched controls as outlined below. All data was de-identified prior to its released to the researchers.
Population
Inclusion criteria
The exposed group were all patients prescribed regular benzodiazepine treatment and authorized for medical cannabis in Alberta between March 31, 2013 and March 31, 2021. Medical cannabis authorization in Canada is defined as a patient being granted authorization by their healthcare provider to access cannabis for medical purpose (i.e., patients self-treating with cannabis for medicinal purposes were not included). Participants were of 18 years of age and older, any sex, ethnicity, and socioeconomic status who received authorization for medical cannabis for any indication (acute and chronic). The index date for each patient was the first recorded date of medical cannabis authorization at the clinics. Regular benzodiazepine treatment was defined as those who had:
-
1.
Benzodiazepine dispensation within 30 days prior to the first date of medical cannabis authorization (index date); and
-
2.
A total of 120 or more cumulative calendar days of benzodiazepines prescriptions based on days supply; or 10 or more dispensations in the year prior index date [29].
The unexposed control group met the same above criteria as the exposed group, with the exception of not having medical cannabis authorization. The index dates of the unexposed group were randomly assigned based on the distribution of exposed group’s index dates.
Exclusion criteria
All patients who were not eligible to receive health benefits in Alberta were excluded (e.g., out of province patients). In addition, to ensure sufficient follow-up time to assess the effects of medical cannabis authorization on regular benzodiazepine use, all patients had to have at least 1 year follow-up time, maintain eligibility for Alberta Health benefits (i.e., did not move out of province) and did not die within 1 year after the index date. Any patients not meeting these criteria were excluded.
Propensity score matched controls
To construct the propensity score, high-dimensional propensity score (HDPS) was used as the approach is known to balance the potential confounders (baseline covariates) and thus, significantly reduce bias by confounding. HDPS can also reduce confounding by some unmeasured characteristics depending on the underlying correlations with known variables. All patients authorized for medical cannabis (n = 9690) were matched with one unique unexposed control group patient using the high dimensional propensity score (HDPS) matching. We selected the matched control for each cannabis user using the nearest neighbour approach with 1: 1 ratio and a caliper set at 0.2. Based on this algorithm, we were successful in identifying 1 control for each cannabis users. Balance in confounders was fully assessed, and no imbalances were noted (all standardized mean differences < 0.1 as recommended). Variables incorporated into the HDPS matching method included: sex, age, year of index date (categorical), baseline benzodiazepine duration, social deprivation index, age group, CNS medications, living area (rural/urban), comorbidities associated with cannabis use, and all healthcare resource utilization variables (all within the year prior to the index date). This includes healthcare utilization (all hospitalizations with up to 10 CCI (Canadian Classification of Health Interventions) procedure codes and 25 diagnostic ICD-10 codes, emergency visit with up to 10 ICD-10 diagnostic code, physician claims with CCI procedure code and with up to 3 ICD-9 diagnostic codes) and all prescription drugs dispensed to a patient at baseline. Notably, the entire healthcare dataset reported greater than 1000 different variables and categories which were included in the HDPS. The HDPS matching technique used the SAS packages proposed by Rassen et al. [30] and Schneeweiss et al. [31].
Outcomes
All benzodiazepine doses were converted into a defined daily dose (DDD) based on the drug’s day supply, dispensation amount, and strength. Using DDD allowed us to estimate the average maintenance dose per day for the different types of benzodiazepines. To standardized the DDD, as benzodiazepines can be short- or long-acting, the strength of each benzodiazepine was then converted to a diazepam equivalence using known pharmacologic conversion factors [1, 32]. The primary outcome was the difference in the daily average diazepam equivalence (DDE) between the medically authorized patients and the matched control group in the 12 months prior to index and 12 months following medical cannabis authorization (or equivalent index date for controls).
Ethics approval
This study was approved by the University of Alberta Health Research Ethics Board (PRO 00084689). As the study relied on secondary use of de-identified health data (i.e. administrative data), a waiver for informed consent was provided by the Ethics Board.
Statistical analysis
All data were expressed descriptively using means (standard deviations [SD]) or count (proportions [%]), as appropriate. To assess the effect of medical cannabis use on DDE, interrupted time series (ITS) analysis was used to assess the change in the trend of diazepam equivalence in the 12 months before and 12 months after the authorization of medical cannabis (or pseudo index for matched controls). ITS is a quasi-experimental design that allows comparison of trends in an outcome before and after an intervention [33, 34]. This specific analysis was chosen for its effectiveness in clear differentiation between population-level health pre-intervention and post-intervention periods. The controlled ITS employed in this study included an additional control series to account for temporal changes that may have occurred within the population. Controlled ITS has been shown to provide similar results as those observed in RCTs [35, 36], which highlights the validity of the approach [37, 38].
DDE was assessed in 30-day windows for each patient (i.e., month-to-month average diazepam equivalence). The absolute effect of medical cannabis authorization on average monthly DDE was calculated, which summarizes both the immediate level change (i.e. within the first month following the index date) and change in trend over the 1 year follow-up period with the multivariate delta method used to construct 95% confidence intervals around the estimate [39].
Sensitivity and stratification analysis
Further stratification was conducted on both authorized medical cannabis patients (n = 9690) and matched controls in 4 subgroups according to baseline DDE as any change in DDE would be expected to be affected by the initial starting DDE:
-
1.
DDE ≤ 5 mg
-
2.
DDE between 5 and 10 mg
-
3.
DDE between 10 and 15 mg
-
4.
DDE > 15 mg
Results
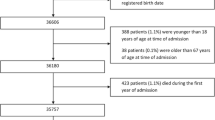
In total, 9690 medically authorized cannabis patients and 123,899 eligible controls were identified (Fig. 1). All 9690 patients were matched to one control, and following HDPS matching, all covariates were well balanced after matching between the groups (standardized difference < 10%; a threshold recommended for declaring imbalance in pharmacoepidemiologic research) [40] (Table 1).
Over the 1-year follow up period after medical cannabis authorization, there was no overall change in the DDE use in authorized medical cannabis patients compared to matched controls (− 0.08 DDE, 95% CI: − 0.41 to 0.24). Additionally, there was no effect in the month-to-month change in average DDE after cannabis authorization (0.04 DDE, 95% CI: − 0.01 to 0.09). When both the initial change and the longer month to month change were combined, no overall effect was observed in the absolute difference in the total monthly DDE (0.32, 95% CI: − 0.23 to 0.87) per patient between cases and controls (Table 2; Fig. 2). Assessments on the type of benzodiazepines dispensed also indicated there was no change in the most frequently used benzodiazepines used before and after cannabis authorization (p > 0.05).
Sensitivity analyses results
Among patients consuming ≤5 mg baseline DDE, there was no change immediately after medical cannabis authorization compared to controls (level change, − 0.04 DDE, 95% CI: − 0.12 to 0.03) per patient as well as in the month-to-month trend change (0.002 DDE, 95% CI: − 0.009 to 0.12) per patient was noted. Overall, there was no change in the absolute difference in the total monthly DDE among medically authorized patients after accounting for both immediate and overall trend during follow-up (− 0.02 DDE, 95% CI: − 0.16 to 0.11) compared to controls (Table 3). Results observed among patients consuming 5–10 DDE, 10–15 mg DDE, and > 15 mg DDE were similar with no immediate change, month-to-month trend change, nor overall absolute difference in the total monthly DDE per patient (Table 3).
Discussion
In this retrospective, observational, population-based study, short-term analysis demonstrated that medical cannabis authorization had little to no effect on benzodiazepine usage among patients prescribed regular benzodiazepine treatment in Alberta, Canada. There were no differences observed across a wide range of initial DDE at baseline. Notably, there were no statistically significant differences when comparing different categories of benzodiazepine DDE groups and any small increases or decreases are likely clinically inconsequential. Collectively, these results may suggest that for the majority of patients on regular benzodiazepine treatment, medical cannabis use is unlikely to alter future benzodiazepine use.
Regarding the literature on benzodiazepine use, more studies are now supporting the role of medical cannabis as an adjunct to benzodiazepine tapering and cessation. Also known as a “sparing effect treatment,” recent studies are reporting that concurrent use with medical cannabis can reduce future benzodiazepine use [41]. Particularly, Purcell et. al’s work found that 45.2% patients successfully discontinued their pre-existing benzodiazepine therapy over 2 months of medical cannabis therapy [42]. However, it is important to note that in this study, the sample size was much smaller and had more frequent follow-ups with physicians compared to the larger sample in our study. Additionally, another study [43] on perioperative cannabis use on surgical patients showed that concurrent use decreased overall benzodiazepine and opioid use. Although our study showed no effect, subgroup effects may still exist where certain patients on benzodiazepine treatment were able to successfully decrease their benzodiazepine dosage through medical cannabis use.
A significant strength of this study is that it is currently, to our knowledge, the largest and longest population-based study of medical cannabis users in Canada. It uses robust measures to track medical cannabis authorization and current benzodiazepine treatment. However, our study is not without limitations. It is an observational study, which can be prone to potential spectrum bias as our cohort of patients were those who individually sought medical cannabis authorization. Secondly, there is a lack of insight into the patient’s adherence to their authorized medical cannabis treatment. The cannabis may have been taken differently than as indicated and/or alternative therapies may have been used to circumvent benzodiazepine usage. Notably, we do not know whether patients were using cannabis prior to authorization. Further, we do not know whether legalization of cannabis during this period impacted the number of patients seeking medical cannabis authorization. In this case, we may expect non-differential misclassification of the control group due to increased widespread cannabis legalization after 2018. For example, some controls may report not having been medically authorized for cannabis, but after legalization of cannabis, were accessing recreational cannabis via storefront for other reasons. The extent of this occurrence is unknown but notably the majority of patients in our study were derived prior to the legalization change in 2018 (i.e., 2013–2018). Furthermore, given the wide variability of medical cannabis products available in Canada, we could not analyze specific strains, modes of consumption, or dosing regimens in this study. All cannabis products were treated as equals, despite there being known clinical difference between products and regimens. Our study is therefore limited by the lack of these clinical details of medical cannabis, in addition to the lack of concomitant use with other non-prescription benzodiazepines agents.
Conclusion
This study found that medical cannabis authorization had minimal effects on benzodiazepine use. Although the clinical importance of medical cannabis as a benzodiazepine sparing treatment is unclear, our findings contribute ongoing evidence for clinicians regarding the association between medical cannabis on benzodiazepine use.
Availability of data and materials
The data that support the findings of this study are available from College of Physicians & Surgeons of Alberta (CPSA) and the Alberta SPOR SUPPORT Unit (https://absporu.ca) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. We had full permission to use this data, however, specific restrictions do apply to the public availability of these data, which are under data access agreements for the current study.
References
Howard P, Twycross R, Shuster J, Mihalyo M, Wilcock A. Benzodiazepines. J Pain Symptom Manag. 2014;47(5):955–64. https://doi.org/10.1016/j.jpainsymman.2014.03.001.
Wick JY. The history of benzodiazepines. Consult Pharm. 2013;28(9):538–48. https://doi.org/10.4140/TCP.n.2013.538.
Votaw VR, Geyer R, Rieselbach MM, McHugh RK. The epidemiology of benzodiazepine misuse: a systematic review. Drug Alcohol Depend. 2019;200:95–114. https://doi.org/10.1016/j.drugalcdep.2019.02.033.
Edinoff AN, Nix CA, Hollier J, et al. Benzodiazepines: Uses, Dangers, and Clinical Considerations. Neurol Int. 2021;13(4):594–607. https://doi.org/10.3390/neurolint13040059.
Gray SL, Lai KV, Larson EB. Drug-induced cognition disorders in the elderly: incidence, prevention and management. Drug Saf. 1999;21(2):101–22. https://doi.org/10.2165/00002018-199921020-00004.
Panes A, Verdoux H, Fourrier-Reglat A, Berdai D, Pariente A, Tournier M. Misuse of benzodiazepines: prevalence and impact in an inpatient population with psychiatric disorders. Br J Clin Pharmacol. 2020;86(3):601–10. https://doi.org/10.1111/bcp.14165.
Alberta T. Hot off the press: The 2021 Opioid & Benzodiazepine/Z-drug and Antibiotic Prescription Atlases. . 2021. Accessed February 13, 2023. https://cpsa.ca/news/hot-off-the-press-the-2021-opioid-benzodiazepine-z-drug-and-antibiotic-prescription-atlases/#:~:text=Over%20one%20million%20benzodiazepine%2FZ,drop%20of%20almost%20one%20fifth.
Clarke H, Fitzcharles M. The evolving culture of medical cannabis in Canada for the management of chronic pain. Front Pharmacol. 2023;14:1153584. https://doi.org/10.3389/fphar.2023.1153584.
Sharpe L, Sinclair J, Kramer A, de Manincor M, Sarris J. Cannabis, a cause for anxiety? A critical appraisal of the anxiogenic and anxiolytic properties. J Transl Med. 2020;18(1):374. https://doi.org/10.1186/s12967-020-02518-2.
Van Ameringen M, Zhang J, Patterson B, Turna J. The role of cannabis in treating anxiety: an update. Curr Opin Psychiatry. 2020;33(1):1–7. https://doi.org/10.1097/YCO.0000000000000566.
Berger M, Amminger GP, McGregor IS. Medicinal cannabis for the treatment of anxiety disorders. Aust J Gen Pract. 2022;51(8):586–92. https://doi.org/10.31128/AJGP-04-21-5936.
Bergamaschi MM, Queiroz RH, Chagas MH, et al. Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naive social phobia patients. Neuropsychopharmacoly. 2011;36(6):1219–26. https://doi.org/10.1038/npp.2011.6.
Gobbi G, Atkin T, Zytynski T, et al. Association of Cannabis Use in Adolescence and Risk of Depression, Anxiety, and Suicidality in Young Adulthood: A Systematic Review and Meta-analysis. JAMA Psychiatry. 2019;76(4):426–34. https://doi.org/10.1001/jamapsychiatry.2018.4500.
Twomey CD. Association of cannabis use with the development of elevated anxiety symptoms in the general population: a meta-analysis. J Epidemiol Community Health. 2017;71(8):811–6. https://doi.org/10.1136/jech-2016-208145.
Hill KP. Cannabis Use and Risk for Substance Use Disorders and Mood or Anxiety Disorders. JAMA. 2017;317(10):1070–1. https://doi.org/10.1001/jama.2016.19706.
Mammen G, Rueda S, Roerecke M, Bonato S, Lev-Ran S, Rehm J. Association of Cannabis With Long-Term Clinical Symptoms in Anxiety and Mood Disorders: A Systematic Review of Prospective Studies. J Clin Psychiatry. 2018;79(4) https://doi.org/10.4088/JCP.17r11839.
Moore TH, Zammit S, Lingford-Hughes A, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319–28. https://doi.org/10.1016/S0140-6736(07)61162-3.
Di Blasi M, Cavani P, Pavia L, et al. Mediating effects of global negative effect expectancies on the association between problematic Cannabis use and social anxiety. Front Psychiatry. 2017;8:249. https://doi.org/10.3389/fpsyt.2017.00249.
Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219–27. https://doi.org/10.1056/NEJMra1402309.
Lum HD, Arora K, Croker JA, et al. Patterns of marijuana use and health impact: a survey among older Coloradans. Gerontol Geriatr Med. 2019;5:2333721419843707. https://doi.org/10.1177/2333721419843707.
Pedersen ER, Miles JN, Osilla KC, Ewing BA, Hunter SB, D'Amico EJ. The effects of mental health symptoms and marijuana expectancies on marijuana use and consequences among at-risk adolescents. J Drug Issues. 2015;45(2):151–65. https://doi.org/10.1177/0022042614559843.
Esmaeelzadeh S, Moraros J, Thorpe L, Bird Y. The association between depression, anxiety and substance use among Canadian post-secondary students. Neuropsychiatr Dis Treat. 2018;14:3241–51. https://doi.org/10.2147/NDT.S187419.
Butler A, Patte KA, Ferro MA, Leatherdale ST. Interrelationships among depression, anxiety, flourishing, and cannabis use in youth. Addict Behav. 2019;89:206–15. https://doi.org/10.1016/j.addbeh.2018.10.007.
Villarosa-Hurlocker MC, Bravo AJ, Pearson MR. Protective strategies study T. The relationship between social anxiety and alcohol and marijuana use outcomes among concurrent users: a motivational model of substance use. Alcohol Clin Exp Res. 2019;43(4):732–40. https://doi.org/10.1111/acer.13966.
Degenhardt L, Chiu WT, Sampson N, et al. Toward a global view of alcohol, tobacco, cannabis, and cocaine use: findings from the WHO world mental health surveys. PLoS Med. 2008;5(7):e141. https://doi.org/10.1371/journal.pmed.0050141.
Wall MM, Liu J, Hasin DS, Blanco C, Olfson M. Use of marijuana exclusively for medical purposes. Drug Alcohol Depend. 2019;195:13–5. https://doi.org/10.1016/j.drugalcdep.2018.11.009.
Smith JM, Mader J, Szeto ACH, Arria AM, Winters KC, Wilkes TCR. Cannabis use for medicinal purposes among Canadian University students. Can J Psychiatr. 2019;64(5):351–5. https://doi.org/10.1177/0706743718818420.
Allan GM, Ramji J, Perry D, et al. Simplified guideline for prescribing medical cannabinoids in primary care. Can Fam Phys. 2018;64(2):111–20.
Lee C, Lin M, Martins KJB, et al. Opioid use in medical cannabis authorization adult patients from 2013 to 2018: Alberta Canada. BMC Public Health. 2021;21(1):843. https://doi.org/10.1186/s12889-021-10867-w.
Rassen JA, Glynn RJ, Brookhart MA, Schneeweiss S. Covariate selection in high-dimensional propensity score analyses of treatment effects in small samples. Am J Epidemiol. 2011;173(12):1404–13. https://doi.org/10.1093/aje/kwr001.
Schneeweiss S, Rassen JA, Glynn RJ, Avorn J, Mogun H, Brookhart MA. High-dimensional propensity score adjustment in studies of treatment effects using health care claims data. Epidemiol. 2009;20(4):512–22. https://doi.org/10.1097/EDE.0b013e3181a663cc.
Ashton HC. Benzodiazepines: How They Work and How to Withdraw. 2013. https://benzo.org.uk/manual/. Accessed 12 Mar 2024.
Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–55. https://doi.org/10.1093/ije/dyw098.
Hamilton I, Lloyd C, Hewitt C, Godfrey C. Effect of reclassification of cannabis on hospital admissions for cannabis psychosis: a time series analysis. Int J Drug Policy. 2014;25(1):151–6. https://doi.org/10.1016/j.drugpo.2013.05.016.
St. Clair T, Hallberg K, Cook TD. The validity and precision of the comparative interrupted time-series design: three within-study comparisons. J Educ Behav Stat. 2016;41(3):269–99.
St. Clair T, Cook TD, Hallberg K. Examining the internal validity and statistical precision of the comparative interrupted time series design by comparison with a randomized experiment. Am J Eval. 2014;35(3):311–27. https://doi.org/10.1177/1098214014527337.
Fretheim A, Zhang F, Ross-Degnan D, et al. A reanalysis of cluster randomized trials showed interrupted time-series studies were valuable in health system evaluation. J Clin Epidemiol. 2015;68(3):324–33. https://doi.org/10.1016/j.jclinepi.2014.10.003.
Fretheim A, Soumerai SB, Zhang F, Oxman AD, Ross-Degnan D. Interrupted time-series analysis yielded an effect estimate concordant with the cluster-randomized controlled trial result. J Clin Epidemiol. 2013;66(8):883–7. https://doi.org/10.1016/j.jclinepi.2013.03.016.
Zhang F, Wagner AK, Soumerai SB, Ross-Degnan D. Methods for estimating confidence intervals in interrupted time series analyses of health interventions. J Clin Epidemiol. 2009;62(2):143–8. https://doi.org/10.1016/j.jclinepi.2008.08.007.
Stuart EA, Lee BK, Leacy FP. Prognostic score-based balance measures can be a useful diagnostic for propensity score methods in comparative effectiveness research. J Clin Epidemiol. 2013;66(8 Suppl):S84–S90 e1. https://doi.org/10.1016/j.jclinepi.2013.01.013.
Pottie K, Thompson W, Davies S, et al. Deprescribing benzodiazepine receptor agonists: evidence-based clinical practice guideline. Can Fam Phys. 2018;64(5):339–51.
Purcell C, Davis A, Moolman N, Taylor SM. Reduction of benzodiazepine use in patients prescribed medical Cannabis. Cannabis Cannabinoid Res. 2019;4(3):214–8. https://doi.org/10.1089/can.2018.0020.
Stewart C, Fong Y. Perioperative Cannabis as a Potential Solution for Reducing Opioid and Benzodiazepine Dependence. JAMA Surg. 2021;156(2):181–90. https://doi.org/10.1001/jamasurg.2020.5545.
Acknowledgements
This study is based in part on data provided by Alberta Health, Alberta Health Services and by the College of Physicians & Surgeons of Alberta (CPSA). The interpretation and conclusions contained herein are those of the researchers and do not necessarily represent the views of the Government of Alberta, Alberta Health Services or CPSA. Neither the Government of Alberta, Alberta Health, Alberta health Services nor CPSA expresses any opinion in relation to this study.
Patient and public involvement
Patients were not involved in the design, conduct and reporting of this research project as it was not applicable to this project. The College of Physicians & Surgeons of Alberta (CPSA) is a public body that was involved in the project in terms of our access to the data. As mentioned in our “Acknowledgements,” although the data was provided by the CPSA, neither the Government of Alberta, Alberta Health, Alberta Health Services, nor CPSA expresses any opinion in relation to this study. Further, the CPSA was not involved in the analysis or reporting of the research project’s outcomes.
Transparency declaration
DTE affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and if relevant) have been explained.
Funding
Production of this study has been made possible through a CIHR Catalyst Grant for Cannabis Research in Urgent Priority Areas, funded by the Canadian Centre on Substance Use and Addiction using Health Canada Cannabis Research Initiative funds (CCSA 163022). The views expressed herein do not necessarily represent the views of CIHR or CCSA or its funders. The funders did not participate in the design of the study, collection, analysis, interpretation of the data, and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
DTE, JRBD, JGH, EH, SWK, and LR designed the study and DTE, JRBD, KJBM acquired the data. ML was the primary analyst for the data. CD, DTE, and HF drafted the manuscript. All other authors revised it critically for important intellectual content and approved the final version to be published. All authors are accountable for the work and integrity of the work. The corresponding author and guarantor accepts full responsibility of the work and/or conduct of the study, had access to the data and controlled the decision to publish. DTE attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the University of Alberta Health Research Ethics Board (PRO 00084689). As the study relied on secondary use of de-identified health data (i.e. administrative data), a waiver for informed consent was provided by the Ethics Board.
Informed consent
The data that support the findings of this study are available from the College of Physicians & Surgeons of Alberta (CPSA) and the Alberta SPOR SUPPORT Unit (https://absporu.ca). We had full permission to use this data, however, but restrictions apply to the public availability of these data, which are under data access agreements for the current study. Patients and the public were not involved in the design, conduct and reporting of this research project as it was not applicable to this project.
Consent for publication
Not applicable.
Competing interests
JRBD was a former member of the board of directors for Aurora Cannabis Inc., which is a for-profit, company licensed for the cultivation and sale of medical cannabis. JRBD currently has no financial interest in Aurora Cannabis Inc. In the past, JGH has worked as a paid advisor and speaker for Canadian Cannabis Clinics- however, currently has no clinical or financial ties. DTE and JRBD held a Mitacs Grant with Aurora as a partner. Mitacs is a national, not-for-profit organization that works with universities, private companies, and both federal and provincial governments, to build partnerships and administer research funding that supports industrial and social innovation in Canada. DTE does not have any past or present financial interest in the companies involved. KJBM, SWK, and LR are members of the Alberta Real World Evidence Consortium, an academic entity that conducts research including investigator-initiated industry-funded studies. All other authors have no conflicts of interest to declare. Moreover, the research funders and companies listed were not involved in any aspect of the design or write-up of the study and all analysis was performed independent from the funders and companies.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dubois, C., Fernandes, H., Lin, M. et al. Benzodiazepine use in medical cannabis authorization adult patients from 2013 to 2021: Alberta, Canada. BMC Public Health 24, 859 (2024). https://doi.org/10.1186/s12889-024-18356-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18356-6