Abstract
Background
Understanding the temporal and geographic distribution of disease incidences is crucial for effective public health planning and intervention strategies. This study presents a comprehensive analysis of the spatiotemporal distribution of disease incidences in Ethiopia, focusing on six major diseases: Malaria, Meningitis, Cholera and Dysentery, over the period from 2010 to 2022, whereas Dengue Fever and Leishmaniasis from 2018 to 2023.
Methods
Using data from Ethiopian public health institute: public health emergency management (PHEM), and Ministry of Health, we examined the occurrence and spread of each disease across different regions of Ethiopia. Spatial mapping and time series analysis were employed to identify hotspots, trends, and seasonal variations in disease incidence.
Results
The findings reveal distinct patterns for each disease, with varying cases and temporal dynamics. Monthly wise, Malaria exhibits a cyclical pattern with a peak during the rainy and humid season, while Dysentery, Meningitis and Cholera displays intermittent incidences. Dysentery cases show a consistent presence throughout the years, while Meningitis remains relatively low in frequency but poses a potential threat due to its severity. Dengue fever predominantly occurs in the eastern parts of Ethiopia. A significant surge in reported incident cases occurred during the years 2010 to 2013, primarily concentrated in the Amhara, Sidama, Oromia, Dire Dawa, and Benishangul-Gumuz regions.
Conclusions
This study helps to a better understanding of disease epidemiology in Ethiopia and can serve as a foundation for evidence-based decision-making in disease prevention and control. By recognizing the patterns and seasonal changes associated with each disease, health authorities can implement proactive measures to mitigate the impact of outbreaks and safeguard public health in the region.
Similar content being viewed by others
Introduction
Infectious diseases remain a significant public health concern in Ethiopia, and their impact on the population’s health and well-being cannot be underestimated. Among the array of infectious diseases that continue to pose challenges, Malaria, Meningitis, Cholera, Dengue fever, Dysentery and Leishmaniasis stand out due to their potential for widespread outbreaks and severe health consequences [1,2,3,4]. These diseases are among the climate sensitive that are dominant in Sub-Saharan countries. This vulnerability is particularly evident due to the region’s diverse climate zones and socio-economic challenges. Diseases like malaria and dengue fever flourish as warmer temperatures accelerate mosquito breeding, while cholera outbreaks coincide with heavy rainfall and flooding. Vector-borne diseases, waterborne diseases, respiratory ailments worsened by air quality changes, and malnutrition-linked illnesses further highlight the intricate links between climate and health in this context [5,6,7,8]. Addressing these challenges requires robust healthcare systems, improved sanitation, vector control, disease surveillance, and climate adaptation strategies to safeguard public health. Monitoring the spatiotemporal distribution of these diseases is vital for understanding their epidemiology, identifying high-risk regions, and formulating targeted interventions to effectively control and prevent disease outbreaks.
Over the past decade, Ethiopia has made commendable efforts to improve its healthcare infrastructure and strengthen disease surveillance systems. As a result, there has been notable progress in reducing the incidence of certain infectious diseases, such as Malaria [9]. Despite these achievements, the country still faces significant challenges in combating other infectious diseases, including Meningitis [10, 11] and Dysentery [12, 13]. Additionally, the frequent occurrence of Dengue Fever in specific areas, especially in easter part of Ethiopia has raised concerns about the potential for outbreaks [14].
Spatial and temporal analyses of disease outbreaks have emerged as essential tools in public health research, allowing for the identification of disease hotspots and trends that may not be evident through traditional epidemiological approaches [15,16,17,18]. These analytical techniques provide valuable insights into the underlying factors contributing to disease transmission and can significantly influence evidence-based policies and interventions.
Over the years, several research studies have focused on investigating the spatial distribution and epidemiology of specific infectious diseases in Ethiopia. For example, Alene et al. [19] utilized Bayesian model-based geostatistical framework for a survey of HIV, TB and malaria, harnessing the power of high-resolution spatial covariates to predict continuous prevalence surfaces specific to each disease, along with their co-distribution. The findings revealed significant association of the spatial distribution of the diseases with healthcare access, demographic and climatic factors. Another study by Warkaw et al. [20]. explored the spatial patterns and predictors of malaria distribution in Ethiopia. Their research utilized Global Moran’s I and Moran scatter plots and local Moran’s I statistic to determine the distribution and investigate the predictors of malaria. The study identified that the occurrence of malaria in Ethiopia exhibited a spatial arrangement linked to socio-economic, demographic, and geographic risk factors. Spatial clustering of malaria cases was evident across all regions, with variations in the risk of clustering observed among these regions. Likewise, in a study by Beyene et al. [21], a comprehensive analysis was undertaken to investigate the spatial, temporal, and spatiotemporal dynamics of under-five diarrhea in Southern Ethiopia. The study involved the calculation of annual diarrhea incidence rates at the district level, encompassing the utilization of incidence rate calculations and seasonal trend analysis. Utilizing data retrospectively obtained from the Health Management Information System (HMIS), covering under-five diarrheal morbidity reports from July 2011 to June 2017 in the Sidama Zone (current Sidama Region), the research discerned distinct patterns. The outcomes of this study underscored the non-random distribution of childhood diarrhea across space and time, revealing an overarching increasing trend marked by seasonal fluctuations.
These studies collectively demonstrate the importance of spatial and temporal analyses in understanding disease epidemiology in Ethiopia. By pinpointing high-risk areas and identifying contributing factors, these research endeavors have played a vital role in guiding public health policies and interventions for various infectious diseases in the country. However, there remains a gap in comprehensive research that simultaneously explores multiple diseases and their spatiotemporal patterns over an extended period.
The primary objective of this study is to conduct a comprehensive analysis of the spatiotemporal distribution of Malaria, Meningitis, Cholera, Dysentery, Leishmaniasis and Dengue fever Incidents between 2010 and 2023. By examining the temporal trends, seasonal variations, and geographic patterns of each disease, we aim to gain a deeper understanding of their dynamics and identify potential risk factors associated with disease transmission and incidences.
Through this research, we aspire to contribute valuable insights to the existing body of knowledge on disease epidemiology in Ethiopia. By shedding light on the spatiotemporal distribution of these infectious diseases, we hope to provide crucial information to public health policymakers and stakeholders. This, in turn, will aid in formulating targeted and efficient strategies for disease surveillance, prevention, and control, ultimately reducing the burden of infectious diseases on the Ethiopian population. In this paper, the term “disease incidence” encompasses any reported occurrence of a disease, whether it is a newly emerging one or one that has already occurred.
Methods
Ethical considerations
Approval for the research was granted by the ethical review board of the Jimma Institute of Technology, with the reference number RPD/JIT/172/15.
Data source
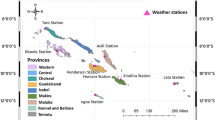
The main source of the study was a secondary data source collected from the Ethiopian public health institute (EPHI): public health emergency management (PHEM), and Ministry of Health (MoH). The EPHI dataset contains four diseases, including Malaria, Meningitis, Dysentery, and cholera/acute watery diarrhea (AWD). The dataset spans disease incidences across 12 regions of Ethiopia, encompassing Oromia, Southern Nations, Nationalities, and Peoples’ Region (SNNPR: which is now divided into South region, southwest region and central Ethiopia region), Amhara, Somali, Addis Ababa, Tigray, Afar, Benishangul Gumuz, Gambella, Sidama, Dire Dawa, and Harari. The disease incidences dataset comprised attributes including region name, zone name, woreda name, year, epidemic week, month, total malaria confirmed and clinical, total malaria outpatient cases, total malaria inpatient cases, total malaria inpatient deaths, total malaria suspected fever examined, post malaria rapid diagnostic tests (RDTs) or microscopy plasmodium falciparum (PF) outpatient cases, post malaria rapid diagnostic tests or microscopy plasmodium vivax (PV) outpatient cases, meningitis total cases, meningitis outpatient cases, meningitis inpatient cases, meningitis inpatient deaths, dysentery total cases, dysentery outpatient cases, dysentery inpatient cases, dysentery inpatient deaths’, cholera/AWD cases, cholera/AWD deaths. The Dengue Fever and Leishmaniasis data that span 2018 to 2023 was collected from MoH. The dataset spans disease incidences across three regions of Ethiopia, encompassing Amhara, Somali, and, Dire Dawa. The dataset comprises six attributes, including Religion, Disease, Zone, Year, Month, and Total Values.
Study setting and design
Utilizing a longitudinal retrospective design, this study examines the prevalence and diffusion of a range of diseases including malaria, meningitis, cholera, dysentery, leishmaniasis, and dengue fever, across diverse Ethiopian regions, integrating longitudinal analysis with geospatial mapping and temporal trend assessment, this investigation synthesizes epidemiological data to reveal intricate patterns.
Data preprocessing and analysis
The data pre-processing, visual inspection, and analysis of disease incidences datasets were conducted using Python. An analysis of missing values, outliers, and noisy data was conducted. The quality of the disease incidence data was examined using WHO data-quality review [22]. The disease incidence dataset was examined for completeness and timeliness, consistency, accuracy, and validity.
Further processing was performed on the EPHI disease incidence datasets columns, including total malaria confirmed and clinical, total malaria outpatient cases, total malaria inpatient cases, total malaria inpatient deaths, total malaria suspected fever examined, post malaria RDTs or microscopy PF outpatient cases, post malaria rapid diagnostic tests or microscopy PV outpatient cases, Meningitis total cases, outpatient cases, inpatient cases, inpatient deaths, dysentery total cases, dysentery outpatient cases, dysentery inpatient cases, dysentery inpatient deaths’, cholera/AWD cases, cholera/AWD deaths were further processed. Moreover, disease incidences with zero values were eliminated from the dataset. Whereas, seventy-five attributes were observed in the initial MoH Dengue Fever and Leishmaniasis disease incidence dataset, and six attributes remain after preprocessing.
The final disease incidence dataset that was used for analysis included the names of the region, zone name, woreda name, year, epidemic week, month, epidemic week, disease, category, type, and total value. Then, the occurrence and spread of each disease across different regions of Ethiopia was examined. Furthermore, spatial mapping and time series analysis were employed to identify hotspots, trends, and seasonal variations in disease incidence. The datasets from the two sources, such as EPHI and MoH, were integrated after the data preprocessing based on the religion, Disease, Zone, Year, Month, and Total Values attributes.
Results
Summary of regional disease incidence distribution
Within the total dataset of disease incidence, the greatest incidence was recorded in the regions of Amhara, SNNPR, and Oromia, constituting percentages of 28.39, 26.81, and 16.62%, respectively. Detailed insights into the distribution of disease incidents in regions of Ethiopian can be found in Figs. 1 and 2.
Comparison of total disease incidence distribution
In the data spanning from 2010 to 2022 (Fig. 3a), which includes information on malaria, dysentery, cholera, and meningitis, the highest observed incidences were related to malaria, accounting for 87.54%. Dysentery followed with a prevalence of 12.04%, while meningitis had the lowest reported incidence at just 0.12% of the total cases. In the case of leishmaniasis and dengue fever data (Fig. 3b) covering a five-year period from 2018 to 2023, dengue fever constituted the majority at 77.93%, whereas leishmaniasis accounted for approximately 22.07%.
Disease incidence trend
Malaria disease incidence in Ethiopia from 2010 to 2022
In Addis Ababa and Tigray, the peak of disease incidence was observed in October, while in Afar, it occurred in December, as illustrated in Table 1. The highest incidence of malaria incidences was noted in November in the regions of Amhara, Benishangul-Gumuz, Dire Dawa, Oromia, Sidama, and SNNPR. Harari and Somali, on the other hand, experienced their highest malaria incidences in June.
Figure 4 shows the average incidence of malaria at the Zone level in Ethiopia from 2010 to 2022. In the latter period (2016–2022), there was a reduction in incidence, with the zonal average maximum decreasing from 192,243 cases to 96,319 cases.
Dysentery disease incidence in Ethiopia from 2010 to 2022
As indicated in Table 2, the peak of dysentery incidence varied across regions: June in Addis Ababa, July in Amhara, August in Tigray and Afar, March in Benishangul-Gumuz, May in Oromia and Dire Dawa, April in Gambella, Harari, Sidama, and SNNPR, and December in Somalia.
Figure 5 demonstrates the Zone level average Dysentery incidence in Ethiopia between 2010 and 2022. A slight increment has been observed in the second period (2016–2022) in zones of eastern Amhara and the Somali region.
Cholera AWD disease incidence in Ethiopia from 2010 to 2022
As per the data presented in Table 3, the highest instances of Cholera Acute Watery Diarrhea (AWD) occurred in August in Addis Ababa, Dire Dawa, Harari, and Tigray. In Afar and Oromia, the peak was observed in June, while for Amhara and Sidama, it occurred in September. SNNPR, Gambella, Benishangul-Gumuz, and Somali reported their highest cases in January, November, October, and March, respectively.
Figure 6 depicts the average incidence of Cholera/AWD at the Zone level in Ethiopia from 2010 to 2022. During the latter period (2016–2022), the disease spread to most regions of Ethiopia.
Meningitis disease incidence in Ethiopia from 2010 to 2022
According to Table 4, cases of meningitis were reported relatively high in December in Addis Ababa, Amhara, Benishangul-Gumuz, Gambella, and Harari. November marked the peak in Oromia and Sidama. In Afar, SNNPR, Somalia, and Tigray, the highest occurrences were recorded in June, March, July, and August, respectively.
Figure 7 illustrates the average incidence of Meningitis at the Zone level in Ethiopia from 2010 to 2022. A more distribution has been observed in the latter period (2016–2022), in most Zones of the Somali region.
Dengue fever and leishmaniasis disease incidence in Ethiopia from 2018 to 2023
In Dire Dawa, the peak of dengue fever cases was observed in November, while in Somalia, it occurred in February, as indicated in Table 5. On the other hand, Leishmaniasis reached its highest incidence in the Amhara region in March.
Figure 8 shows the Dengue fever and Leishmaniasis Zone level average over five years incidences in Amhara region (Leishmaniasis), Somali region and the Dire Dawa city admisntration (Dengue fever) between 2018 and 2023.
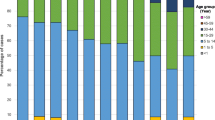
Disease incidence yearly trends in Ethiopia from 2010 to 2022/2023
Between the period of 2010 and 2022/2023, the highest historical disease incidence was observed in 2012 specifically in the Amhara and Afar regions for both malaria and Dysentery. Figures 9 and 10 demonstrate the regional and disease-specific yearly trends.
Discussion
This study presents a comprehensive analysis of the spatiotemporal distribution of disease incidences in Ethiopia, encompassing six major diseases: Malaria, Meningitis, Cholera, Dysentery, Dengue Fever and Leishmaniasis. The temporal and geographic distribution of disease incidences is a critical factor in effective public health planning and intervention strategies. Through an examination of data sourced from the Ethiopian Public Health Institute’s Public Health Emergency Management (PHEM), this study provides insights into the occurrence and propagation of each disease across different regions of Ethiopia. By employing spatial mapping and time series analysis, the study identifies hotspots, trends, and seasonal variations in disease incidence.
The findings of this analysis unveil distinct patterns for each disease, characterized by varying incidences and temporal dynamics.
Malaria is influenced by a complex interplay of environmental, social, and individual factors. Environmental factors such as climate, temperature, and rainfall impact the breeding and survival of the Anopheles mosquitoes, which transmit the malaria parasite [23]. Geographical location and landscape also play a role, as areas with stagnant water bodies are more conducive to mosquito breeding (Amhara, Oromia and Sidama regions are good examples). Socioeconomic factors, including poverty and limited access to healthcare, contribute to higher malaria risk, as vulnerable populations may lack the means for preventive measures and timely treatment. Individual factors such as age, immunity, and travel history also influence susceptibility. Additionally, the prevalence of drug-resistant malaria strains poses a significant risk in some regions. Effective malaria prevention and control strategies require addressing this multifaceted range of risk factors [24]. According to our finding, a prominent cyclical pattern emerges, characterized by its peak incidence coinciding notably with the rainy and humid season. This phenomenon aligns with the well-established trend often observed in vector-borne diseases, wherein the availability of breeding sites for disease vectors is augmented by the increased humidity and precipitation during this period [25,26,27]. The insight gained from this cyclical pattern not only substantiates existing knowledge but also serves as a critical point of reference for timing interventions and resource allocation to effectively mitigate Malaria incidences.
Cholera/Diarrhea risk factors include poor sanitation, inadequate access to clean water, overcrowded living conditions, low socioeconomic status, and individual behaviors like poor hygiene and improper food handling. Population density and increased mobility, particularly in close and crowded settings, facilitate the rapid spread of infectious diseases, heightening the risk in certain clusters with extensive human interaction for Cholera. Unique environmental conditions, including climate and weather factors including temperature and humidity, contribute to the prevalence and transmission of these pathogens causing meningitis in specific clusters [28, 29]. Socioeconomic factors, such as poor hygiene and sanitation practices, amplify the transmission risk, particularly in clusters with inadequate sanitation infrastructure [30], which is also the case for those areas where more incidences are reported in this paper. Additionally, the presence of animal reservoirs and zoonotic transmission which can elevate the risk in clusters with proximity to animals or specific animal-human interactions, could be the reasons origins of sporadic meningitis epidemics in those areas [31, 32]. Somali, Sidama and Dire Dawa are typical examples for this. Additionally, malnutrition, weakened immune systems, and pre-existing health conditions contribute to susceptibility [33]. Limited access to healthcare facilities and delays in diagnosis and treatment exacerbate the impact of meningitis incidences, particularly in clusters with poor healthcare infrastructure, potentially leading to more severe epidemics.
Dysentery risk factors encompass poor sanitation, crowded living conditions, malnutrition, compromised immune systems, age (with children being more vulnerable), prior infections increasing susceptibility, contaminated food and water consumption, poor personal hygiene practices, and close contact with infected individuals [34]. These factors contribute to the transmission of the bacteria or parasites responsible for dysentery, emphasizing the importance of preventive measures such as maintaining good hygiene, ensuring access to clean water, and avoiding contaminated food sources. Dysentery showcases a persistent presence throughout the study years. Given the consistent occurrence of Dysentery cases, it is evident that effective strategies to combat this ailment necessitate not only reactive responses but also a proactive approach centered around preventive measures, health education, and hygiene awareness campaigns.
When considering the geographical distribution, it becomes evident that the regions of Amhara, Sidama, SNNPR and Oromia are characterized by their substantial population densities, exhibit a pronounced prevalence of disease incidences during the period spanning from 2010 to 2022/2023. This heightened incidence within these regions can be attributed to their large and densely populated communities, which potentially create an environment conducive to disease transmission and propagation. The convergence of sizable populations with various social and environmental factors likely contributes to the increased vulnerability and susceptibility to disease incidences in these areas [35, 36]. Thus, the observation of heightened disease incidence in Amhara, Sidama SNNPR and Oromia underscores the intricate interplay between demographic dynamics and disease prevalence, shedding light on the necessity for tailored public health interventions and resource allocation. On the other hand, dengue fever exhibits a predominant prevalence within the eastern parts of Ethiopia, characterized by their hot climates and extended periods of drought. This observation aligns with the established understanding that dengue fever thrives in warm, tropical environments, giving rise to flu-like symptoms and, in some instances, progressing to a severe manifestation known as severe dengue [37].
Efforts to address these climate-sensitive diseases particularly in Ethiopia and Sub-Saharan countries, in general, require a multi-faceted approach. This includes strengthening healthcare systems, improving sanitation and water management, implementing effective vector control measures, enhancing disease surveillance, and promoting climate adaptation strategies to mitigate the impact of changing environmental conditions on public health.
In summary, this study serves as a foundational resource for evidence-based decision-making in disease prevention and control strategies. The complete investigation of the spatiotemporal dynamics of disease incidences yielded a detailed understanding of disease distribution that equips health authorities to engage pro-actively in preserving public health in the Ethiopian environment. By providing evidence-based insights into the spatio-temporal patterns associated with each disease, this study provides health authorities with the necessary tools to make informed decisions in the prevention and control of diseases. The findings of this study have the potential to guide policymaking and resource allocation, facilitating proactive measures that mitigate the repercussions of incidences and ensure the well-being of the population. The incorporation of these findings into public health policy can open the door for efficient interventions and, in the end, help to lessen the effects of disease on communities throughout the region.
Conclusion
Exploratory analysis illuminates the spatio-temporal dynamics of disease incidence distribution in Ethiopia, encompassing six significant diseases over a 13-year span. The distinct patterns observed for each disease, coupled with their varying prevalence and temporal behaviors, underscore the need for tailored interventions. The recurring pattern of Malaria underscores the significance of prompt interventions, whereas the continual occurrences of Dysentery underline the need for vigilance. The enduring cases of dengue fever in eastern Ethiopia and instances of Leishmaniasis in the Amhara region emphasize the ongoing importance of preventive measures and underscore the necessity for preparedness. The evident correlation between disease prevalence and regions with substantial populations, such as Oromia and Amhara, signifies the necessity for tailored interventions within these densely inhabited areas. The identification of high-risk regions provides a strategic foundation for resource allocation, targeted interventions, and proactive measures to mitigate outbreaks’ impact. By integrating these insights into policy and practice, Ethiopia can enhance its public health approach, effectively mitigating disease impact and fostering a more resilient society.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author up on a reasonable request and with a written permission from the original data sources.
References
Organization WH. Managing epidemics: key facts about major deadly diseases. World Health Organization; 2018.
Organization WH. World malaria report 2022. World Health Organization; 2022.
Meki CD, Ncube EJ, Voyi K. Frameworks for mitigating the risk of waterborne diarrheal diseases: a scoping review. PLoS ONE. 2022;17(12):e0278184.
Shrivastava SR, Shrivastava PS. Moving forward toward the goal of meningitis-free world by 2030: potential strategies. Indian J Health Sci Biomedical Res. 2022;15(3).
Abbass K, Qasim MZ, Song H, Murshed M, Mahmood H, Younis I. A review of the global climate change impacts, adaptation, and sustainable mitigation measures. Environ Sci Pollut Res. 2022;29(28):42539–59.
Yadav N, Upadhyay RK. Global effect of Climate Change on Seasonal cycles, Vector Population and Rising challenges of Communicable diseases: a review. J Atmospheric Sci Res. 2023;6(1).
Semakula HM, Song G, Achuu SP, Shen M, Chen J, Mukwaya PI, et al. Prediction of future malaria hotspots under climate change in sub-saharan Africa. Clim Change. 2017;143:415–28.
Kotir JH. Climate change and variability in Sub-saharan Africa: a review of current and future trends and impacts on agriculture and food security. Environ Dev Sustain. 2011;13:587–605.
Aregawi M, Lynch M, Bekele W, Kebede H, Jima D, Taffese HS, et al. Time series analysis of trends in malaria cases and deaths at hospitals and the effect of antimalarial interventions, 2001–2011, Ethiopia. PLoS ONE. 2014;9(11):e106359.
Tigabu A, Jember A, Nega T, Wubishet G, Misganaw H, Goshu T et al. Bacterial meningitis among adult patients at university of Gondar comprehensive specialized referral hospital. Infect Drug Resist. 2021:565–74.
Gudina EK, Tesfaye M, Adane A, Lemma K, Shibiru T, Pfister HW, et al. Challenges of bacterial meningitis case management in low income settings: an experience from Ethiopia. Tropical Med Int Health. 2016;21(7):870–8.
Bogale GG, Gelaye KA, Degefie DT, Gelaw YA. Spatial patterns of childhood diarrhea in Ethiopia: data from Ethiopian demographic and health surveys (2000, 2005, and 2011). BMC Infect Dis. 2017;17(1):426.
Fenta SM, Nigussie TZ. Factors associated with childhood diarrheal in Ethiopia; a multilevel analysis. Archives Public Health. 2021;79(1):123.
Gutu MA, Bekele A, Seid Y, Mohammed Y, Gemechu F, Woyessa AB, Tayachew A, Dugasa Y, Gizachew L, Idosa M, Tokarz RE, Sugerman D. Another dengue fever outbreak in Eastern Ethiopia-An emerging public health threat. PLoS Negl Trop Dis. 2021;15(1):e0008992. https://doi.org/10.1371/journal.pntd.0008992. PMID: 33465086; PMCID: PMC7845954.
Chan T-C, King C-C. Surveillance and epidemiology of infectious diseases using spatial and temporal lustering methods. Infectious disease informatics and biosurveillance: research, systems and case studies. Springer; 2010. pp. 207–34.
Jeefoo P, Tripathi NK, Souris M. Spatio-temporal diffusion pattern and hotspot detection of dengue in Chachoengsao Province. Thail Int J Environ Res Public Health. 2011;8(1):51–74.
Talisuna AO, Okiro EA, Yahaya AA, Stephen M, Bonkoungou B, Musa EO, et al. Spatial and temporal distribution of infectious disease epidemics, disasters and other potential public health emergencies in the World Health Organisation Africa region, 2016–2018. Globalization Health. 2020;16:1–12.
Christaki E. New technologies in predicting, preventing and controlling emerging infectious diseases. Virulence. 2015;6(6):558–65.
Alene KA, Elagali A, Barth DD, Rumisha SF, Amratia P, Weiss DJ et al. Spatial codistribution of HIV, Tuberculosis and malaria in Ethiopia. BMJ Glob Health. 2022;7(2).
Warkaw YM, Mitku AA, Zeru MA, Ayele M. Spatial pattern and predictors of malaria in Ethiopia: application of auto logistics regression. PLoS ONE. 2022;17(5):e0268186.
Beyene H, Deressa W, Kumie A, Grace D. Spatial, temporal, and spatiotemporal analysis of under-five diarrhea in Southern Ethiopia. Trop Med Health. 2018;46(1):18.
Organization WH. Data quality review: a toolkit for facility data quality assessment. Geneva: World Health Organization; 2017.
Mohammadkhani M, Khanjani N, Bakhtiari B, Sheikhzadeh K. The relation between climatic factors and malaria incidence in Kerman, South East of Iran. Parasite Epidemiol Control. 2016;1(3):205–10.
Castro MC. Malaria Transmission and prospects for Malaria Eradication: the role of the Environment. Cold Spring Harb Perspect Med. 2017;7(10).
da Silva AS, Andreoli RV, de Souza RAF, da Silva Chagas ÉC, de Moraes DS, de Figueiredo RC, et al. Impact of El Niño on the dynamics of American cutaneous leishmaniasis in a municipality in the western Amazon. Acta Trop. 2021;222:106032.
Sutherst RW. Global change and human vulnerability to vector-borne diseases. Clin Microbiol Rev. 2004;17(1):136–73.
Short EE, Caminade C, Thomas BN. Climate change contribution to the emergence or re-emergence of parasitic diseases. Infect Diseases: Res Treat. 2017;10:1178633617732296.
Al-Qahtani SM, Shati AA, Alqahtani YA, Ali AS, Etiology. Clinical phenotypes, Epidemiological Correlates, Laboratory biomarkers and Diagnostic challenges of Pediatric viral meningitis: descriptive review. Front Pediatr. 2022;10:923125.
Kinlin LM, Spain CV, Ng V, Johnson CC, White AN, Fisman DN. Environmental exposures and invasive meningococcal disease: an evaluation of effects on varying time scales. Am J Epidemiol. 2009;169(5):588–95.
Church DL. Major factors affecting the emergence and re-emergence of infectious diseases. Clin Lab Med. 2004;24(3):559–86. v.
Rahman MT, Sobur MA, Islam MS, Ievy S, Hossain MJ, El Zowalaty ME et al. Zoonotic diseases: etiology, impact, and control. Microorganisms. 2020;8(9).
van Samkar A, Brouwer MC, van der Ende A, van de Beek D. Zoonotic bacterial meningitis in human adults. Neurology. 2016;87(11):1171–9.
Nwokoro UU, Ugwa O, Onwuliri CD, Obi IF, Ngozi MO, Agunwa C. Water, sanitation and hygiene risk factors associated with diarrhoea morbidity in a rural community of Enugu, South East Nigeria. Pan Afr Med J. 2020;37:115.
Dejkam A, Hatam-Nahavandi K. Dysentery in children. Iran J Public Health. 2021;50(9):1930–1.
Viboud C, Simonsen L, Chowell G. A generalized-growth model to characterize the early ascending phase of infectious disease outbreaks. Epidemics. 2016;15:27–37.
Gwenzi W, Sanganyado E. Recurrent cholera outbreaks in sub-saharan Africa: moving beyond epidemiology to understand the environmental reservoirs and drivers. Challenges. 2019;10(1):1.
Sapuan I, Hassan NA, Rus RM, Aidid EM, Effect of climate variability on Dengue cases in pahang. Transforming medical healthcare through research (IIUM). 2023:2.
Acknowledgements
The necessary resources for this study were provided by the AI and Biomedical Imaging Research Lab at Jimma Institute of Technology, and Mega Research grant of Jimma University. We extend our gratitude to the Ethiopian Public Health Institute’s Public Health Emergency Management (PHEM) and the Ministry of Health of Ethiopia for granting us access to the valuable data required for this research.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research did not involve humans, animals, or other subjects. Approval for the research was granted by the ethical review board of the Jimma Institute of Technology, with the reference number RPD/JIT/172/15.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Simegn, G.L., Degu, M.Z., Gebeyehu, W.B. et al. Spatiotemporal distribution of climate-sensitive disease incidences in ethiopia: a longitudinal retrospective analysis of Malaria, Meningitis, Cholera, Dysentery, Leishmaniasis and Dengue fever between 2010 and 2022/2023. BMC Public Health 24, 697 (2024). https://doi.org/10.1186/s12889-024-18054-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18054-3