Abstract
Background
Recent studies suggested inconclusive associations between bisphenols exposure and hyperuricemia risk. Our objective was to assess the potential association of bisphenol A (BPA) and its substitutes bisphenol S and F (BPS and BPF) exposure with serum uric acid (SUA) levels, hyperuricemia, and gout prevalence among US adults within the NHANES 2013-2016 datasets.
Methods
Multivariable linear and logistic regression models were used to explore the associations of urinary bisphenols concentrations with SUA levels, hyperuricemia, and gout prevalence, in total population and different sex groups. The restricted cubic spline (RCS) model was used to explore the dose-response relationship.
Results
In total population, doubling of urinary BPS and ∑BPs concentrations showed associations with an increase of 2.64 μmol/L (95% CI: 0.54, 4.74) and 3.29 μmol/L (95% CI: 0.59, 5.99) in SUA levels, respectively. The RCS model indicated a significantly “J”-shaped dose-response relationship between BPS exposure and SUA levels. Compared to the reference group of urinary BPS, males in the highest quartile displayed a 13.06 μmol/L (95% CI: 0.75, 25.37) rise in SUA levels. For females, doubling of urinary BPS concentrations was associated with a 3.30 μmol/L (95% CI: 0.53, 6.07) increase in SUA levels, with a significant linear dose-response relationship. In total population, doubling of urinary BPA concentrations showed a 1.05-fold (95% CI: 0.97, 1.14) adjusted risk of having hyperuricemia, with an inverted “U” curve. Doubling of urinary ∑BPs concentrations was associated with a 1.05-fold (95% CI: 0.96, 1.14) adjusted risk of hyperuricemia in total population, with a significant monotonic dose-response relationship. In females, doubling of urinary BPS concentrations was associated with a 1.45-fold (95% CI: 1.01, 2.08) adjusted increased risk of having gout, with a “J” shaped relationship.
Conclusions
BPA and BPS exposure to some extent were associated with elevated SUA levels and increased risk of hyperuricemia, with different dose-response relationships and sex differences.
Similar content being viewed by others
Introduction
Uric acid, derived from purine metabolism, contributed to approximately 50% of the antioxidant capacity in plasma. However, it also has harmful pro-oxidant effects including oxidative damage, inflammatory response, and endothelial dysfunction [1]. Excessive uric acid production or reduced urate excretion is an essential prerequisite for hyperuricemia and gout. Hyperuricemia and gout are risk factors for hypertension, hyperlipidemia, diabetes, kidney dysfunction, and lead to excessive premature death and disability [2, 3]. The prevalence of hyperuricemia has demonstrated an escalating trend in recent years, with rates of 11.4%, 15.1%, and 20.1% in Korea, China, and America, respectively [4,5,6]. Due to the increasing prevalence and severe implications, an investigation into potential risk factors of hyperuricemia and gout is imperative. Hyperuricemia is a multifaceted disease with many risk factors. Traditional risk factors such as gender, age, genetics, and lifestyles cannot entirely elucidate the magnitude and alarming spread of the hyperuricemia epidemic. Although the evidence was inconclusive, environmental pollutants including arsenic and lead had been linked to hyperuricemia and gout [7, 8].
Bisphenol A (BPA) is a highly versatile industrial compound. BPA is not only an important precursor for synthesizing polycarbonate and epoxy resin, but also can be used to produce chemical products such as plasticizers, heat stabilizers, flame retardants, coatings. BPA have been widely employed in food packaging materials, medical consumables, sports equipment, and various daily necessities [9]. Due to the wide application of BPA, it can be detected in various environmental media (water, soil, atmosphere, indoor dust, etc.) and foods [10]. In daily life, consuming food and drinking water, dermal contact with thermosensitive paper, and inhaling suspended particulate matter in the air can all cause BPA exposure [10]. However, numerous epidemiological studies have linked BPA exposure to infertility, obesity, diabetes, and cardiovascular diseases [11]. In light of the negative effects of BPA, many countries had successively imposed restrictions on its usage while proactively pursuing substitute substances. At present, bisphenol analogs are applied in chemical products, while bisphenol S (BPS) and bisphenol F (BPF) emerged as the primary alternatives to BPA. Nowadays, BPS and BPF are prevalent in various environmental media, foods, and biological samples [12]. Unfortunately, increasing literature manifested that the hormonal activities exhibited by BPS and BPF were comparable to, or even surpassed the levels of BPA [13].
Recent studies indicated that bisphenols exposure was inconclusively associated with the risk of hyperuricemia. Ma et al. revealed that BPA exposure increased uric acid synthesis via enhancing xanthine oxidase (XO) [14]. Hu et al. revealed an elevated risk of hyperuricemia development among subjects with increased serum BPA levels in China [15]. However, serum BPA had lower sensitivity than urine BPA to reflect the body burden [16]. Lee et al. conducted an assessment on the association between BPA, BPS, and BPF exposure and serum uric acid (SUA) concentrations in a sample of 489 Korean children aged 6 years. Results indicated that only BPS exposure exhibited a significant association with elevated SUA levels [14]. Hyperuricemia and gout mainly occur in adults with risk factors. However, there is limited evidence available regarding the association between bisphenols exposure and the prevalence of hyperuricemia and gout in the adult population. Herein, we conducted a nationally representative cross-sectional study to examine the relationship of BPA, BPS, and BPF exposure with SUA levels, hyperuricemia, as well as gout prevalence in the US adult population. The epidemiological evidence provided in this study will provide important clues for health risk assessment of bisphenols, as well as the prevention and treatment of hyperuricemia and gout.
Methods
Study population
The National Health and Nutrition Examination Survey (NHANES) is an ongoing nationally representative cross-sectional survey that uses a complex, stratified, multistage probability design to assess the health and nutritional status of the US non-institutionalized population [17]. The study protocol was approved by the research ethics review board of the National Center for Health Statistics of the Centers for Disease Control and Prevention.
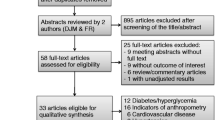
Participants aged 20 years or older from NHANES 2013-2014 and 2015-2016 cycles (BPS and BPF were detected from 2013) with available information on SUA concentration (n = 3367), gout (n = 3495), urinary bisphenols and creatinine levels (n = 3495) were included. Considering the established links between chronic kidney disease and both hyperuricemia and gout, we excluded participants who received dialysis (n = 7) or had an estimated glomerular filtration rate (eGFR) less than 10 mL/min/1.73 m2 (n = 1) [7]. Finally, 3359 adults were eligible for the association of bisphenols exposure with SUA levels and hyperuricemia prevalence, while 3487 adults were eligible for the association with gout prevalence. The study protocol was approved by the research ethics review board of the National Center for Health Statistics of the Centers for Disease Control and Prevention. All participants provided written informed consent. Our study followed the guideline for strengthening the reporting of observational studies in epidemiology statement (STROBE) [18]. A STROBE checklist had been displayed in the Supplementary materials Table S1.
Serum uric acid levels measurement, hyperuricemia and gout diagnosis
SUA concentrations were analyzed by a timed endpoint colorimetric method [19]. SUA is oxidized by the uricase to form allantoin and H2O2. The intensity of the red color formed is proportional to the concentration of SUA. The inter-assay coefficient of variation for SUA was less than 2.5% for NHANES 2013-2016. Hyperuricemia was defined as a SUA concentration exceeding 7 mg/dL in males and 6 mg/dL in females [20]. Gout has been defined as either self-reported physician diagnosis or anti-gout medication use. This is a sensitive case definition method and has been applied in extensive epidemiologic studies [7, 21]. Anti-gout medication including allopurinol, alloxanthine, colchicine, probenecid, and febuxostat use during the medical history.
Urinary bisphenols measurement
Urine specimen was collected in urine collection cups with teflon-coated stoppers. Urinary bisphenols concentrations were analyzed by online solid phase extraction coupled to high performance liquid chromatography–isotope dilution tandem mass spectrometry with peak focusing. Further information regarding the methodology is accessible online [22]. The spiked recoveries of BPA, BPS, and BPF were 99%-104%, 104%-107%, and 91%-103%, respectively. The inter-assay coefficients of variation for the three bisphenol in quality control pools with high and low concentration levels were less than 10%. The lower limits of detection (LLOD, in μg/L) for BPA, BPS, and BPF were 0.2, 0.1, and 0.2, respectively. As NHANES protocol suggested, urine specimens with analytes concentrations below the LLOD were imputed as the LLOD divided by the square root of 2 (https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/EPHPP_H.htm). In our study, the detection rates of BPA, BPS, and BPF were 94.3%, 90.8%, and 55.6%, respectively.
In consideration of urine dilution, urinary creatinine levels were determined on a Roche Cobas 6000 Analyzer using the sarcosine oxidase method. The inter-assay coefficient of variation for urinary creatinine was less than 2.0%.
Covariates
Information on sociodemographic (age, sex, race/ethnicity, educational attainment, income level) were collected during household interviews. Lifestyle factors (smoking, alcohol intake and physical activity), body height and weight were obtained at the mobile examination center. Race/ethnicity was categorized into non-Hispanic black, non-Hispanic white, Mexican American, and other (including multi-racial and other Hispanic group). Smoking status was categorized into never, former, and current (smoked at least 100 cigarettes during the lifetime and still smoke) [17]. Drinking status was categorized into never (had less than 12 alcohol drinks during the lifetime), former (had at least 12 alcohol drinks during the lifetime and not drink alcohol over past 12 months), as well as current mild (1 drinks/day for female, ≤ 2 drinks/day for male, or binge drinking 1 day/month), moderate (≥ 2 drinks/day for female, ≥ 3 drinks/day for male, or binge drinking ≥ 2 days/month), and heavy drinkers (≥3 drinks/day for female, ≥ 4 drinks/day for male, or binge drinking 5 days/month) [23].
Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared (kg/m2), and was categorized into three levels (< 25, 25-30, or ≥ 30) [17]. Physical activity was calculated according to the metabolic equivalent (MET), weekly frequency, and duration of each activity [24]. Estimated glomerular filtration rate (eGFR) was calculated according to the CKD-EPI creatinine equation [25]. Hyperlipidemia, diabetes, and hypertension were defined if participants self-reported a physician diagnosis, had deviant indexes (serum lipid, plasma glucose, or blood pressure), or current use of corresponding anti-hyperlipidemia, anti-diabetic, or anti-hypertensive medications [26,27,28,29].
Statistical analysis
To account for the complex study design, specific subsample weights for urinary environmental phenols, stratum, and PSU variables were incorporated into all analyses. Statistical analysis was separately conducted for males and females, considering the significant disparity in their SUA levels and gout prevalence.
The associations of urinary bisphenols concentrations with SUA levels were evaluated by the coefficient and 95% confidence interval (CI) in multivariable linear regression models. The associations of urinary bisphenols concentrations with hyperuricemia and gout prevalence were assessed by multivariable logistic regression models, and the odds ratio (OR) and 95% CI were calculated. Model 1 adjusted for urinary creatinine. Model 2 further adjusted for age, sex, BMI. Model 3 further adjusted for ethnicity, smoking and drinking status, education, income, hyperlipidemia, diabetes, hypertension, and eGFR. Urinary bisphenols concentrations were respectively examined as categorical (grouped into quartiles) and continuous (log2 transformed) variables in the models. In the categorical model, the linear trend was examined by using the median value of each quartile as a continuous variable. Because BPF (55.6%) was not detected in over three quarters, an ordinal four-category variable was constructed as: individuals with BPF concentrations lower than the limit of detection were classified as the reference, individuals with detectable levels (> LLOD) were equally divided into three groups. Besides, the mass concentration of BPA, BPS, and BPF was summed to represent the total concentrations of bisphenols (∑BPs). To explore the dose-response relationship of bisphenols exposure with SUA levels, hyperuricemia, and gout prevalence, weighted restricted cubic spline (RCS) model was constructed in the “rms” R package. A covariate was incorporated into the regression model upon fulfilling any of the three criteria: a) had been selected in previous related literature; b) caused more than 10% change in the estimated exposure-effect (OR or coefficient) [30]; c) had biological relevance with hyperuricemia or gout. Urinary creatinine levels were compulsively incorporated into all models to correct urine dilution as suggested [31]. Participants with missing data on covariates were excluded from the corresponding model.
Two sensitivity analyses were designed to test the robustness of our results. First, anti-gout medication use decreases SUA concentration which might blunt bisphenols’ effects. We repeated the regression model after excluding individuals with anti-gout treatment. Second, high-purine foods and drinks are risk factors for hyperuricemia and gout. We further adjusted drinks, internal organ and seafood intake in our analyses (over 20% of participants missing data about purine intake). Bisphenols exposure was suggested to be associated with impaired renal function (decreased eGFR), which affects the excretion of uric acid and leads to hyperuricemia [32]. Hence, we assessed the mediating role of eGFR on the association between urinary bisphenol and SUA levels.
All these statistical analyses were performed on the R software (version 4.2.1). A two-tailed P-value < 0.05 was regarded as statistically significant.
Results
Characteristics of the study population
Table 1 presents the characteristics and urinary bisphenols distributions of the study population. Among these participants, 4.4% (155/3487) were diagnosed with gout, 20.6% (692/3359) were diagnosed with hyperuricemia. The mean age for the non-gout, gout, and hyperuricemia group were 46.9, 62.4, and 51.6, respectively. The median concentration of SUA in the non-gout, gout, and hyperuricemia group was 3.2, 3.9, and 4.3 μmol/L, respectively. The median concentration of BPA, BPS, and ∑BPs in gout group were higher than that in non-gout group, although statistical significance was not observed (P > 0.05). The concentration of BPA, BPF, and ∑BPs in hyperuricemia group were significantly higher than that in non-hyperuricemia group (P < 0.05).
Bisphenols exposure and serum uric acid levels
In total population, after adjusting for multiple potential confounders (Model 3), doubling of urinary BPS and ∑BPs concentrations were significantly associated with 2.64 μmol/L (95% CI: 0.54, 4.74) and 3.29 μmol/L (95% CI: 0.59, 5.99) increased uric acid levels (Table 2). In the categorical model, individuals in the highest quartile of urinary ∑BPs had a 12.02 μmol/L (95% CI: 2.71, 21.33) increased SUA levels. The RCS model indicated a significantly “J”-shaped dose-response relationship between BPS exposure and SUA levels, and a linear dose-response relationship between ∑BPs exposure and SUA levels (Fig. 1).
In males, individuals in the highest quartile of urinary BPS had a 13.06 μmol/L (95% CI: 0.75, 25.37) increased SUA levels. In females, doubling of urinary BPS concentrations was associated with a 3.30 μmol/L (95% CI: 0.53, 6.07) increased SUA levels. Doubling of urinary ∑BPs concentrations was respectively associated with a 3.83 μmol/L (95% CI: –0.50, 8.15) and 2.67 μmol/L (95% CI: –1.24, 6.58) increased SUA levels in males and females. The RCS model manifested a significantly monotonic dose-response relationship between ∑BPs exposure and SUA levels in both genders (Fig. 1).
Bisphenols exposure and hyperuricemia prevalence
In total population, doubling of urinary BPA concentrations was associated with a 1.05-fold (95%CI: 0.97, 1.14) adjusted risk of having hyperuricemia (Table 3). The RCS model manifested a significantly inverted “U” shaped non-monotonic dose-response (NMDR) relationship between BPA exposure and hyperuricemia prevalence (Pnon-linear = 0.003) (Fig. 2). Doubling of urinary ∑BPs concentrations was associated with a 1.05-fold (95% CI: 0.96, 1.14) adjusted risk of having hyperuricemia in total population, with a significant monotonic dose-response relationship (Fig. 2). Doubling of urinary BPS concentrations was associated with a 1.13-fold (95% CI: 1.00, 1.28) and 1.09-fold (95% CI: 0.99, 1.21) adjusted risk of having hyperuricemia in male and female group (Table 3), with no significant dose-response relationships (Fig. 2).
Bisphenols exposure and gout prevalence
In total population, no significant associations and dose-response relationships between bisphenols exposure and gout prevalence were established (Table 4 and Fig. 3). In males, individuals with higher BPA levels pretended to have high gout prevalence (Ptrend = 0.036), with an NMDR relationship (Pnon-linear = 0.011). In females, doubling of urinary BPS concentrations was linked to a 1.45-fold (95% CI: 1.01, 2.08) adjusted increased risk of having gout, with a “J” shaped NMDR relationship (Pnon-linear = 0.026).
The dose-response relationships of urinary bisphenols concentrations with the risk of gout. Models were adjusted for urinary creatinine, age, sex, BMI, ethnicity, smoking and drinking status, education, income, hyperlipidemia, diabetes, hypertension, and eGFR. Color should be used for all figures in print
Sensitivity and mediation analyses
The associations of bisphenols exposure with SUA levels and hyperuricemia prevalence remained robust while excluding individuals with anti-gout treatment (Table S2 and S3). After further adjusting purine intake in the regression model, BPS exposure still was positively associated with SUA levels, but the associations of ∑BPs exposure with SUA levels, hyperuricemia, and gout prevalence tended to be nonsignificant (Table S4-S6).
In total population, urinary BPS concentrations exhibited a positive association with eGFR levels (Ptrend = 0.023) (Table S7). In male group, both urinary BPS and ∑BPs concentrations were positively associated with eGFR levels. However, no mediating effects of eGFR on the associations between urinary bisphenols and SUA levels were found (Table S8).
Discussion
In the present study, urinary BPA, BPF, and ∑BPs in hyperuricemia group were significantly higher than those in non-hyperuricemia group. After adjustment for potential confounders, BPS and ∑BPs exposure exhibited a positive association with SUA levels in total and female population. BPA exposure was to some degree associated with hyperuricemia prevalence in total population with an inverted “U” shaped dose-response relationship.
In accordance with previous research, our findings indicate a positive correlation between BPA exposure and the prevalence of hyperuricemia. Ma et al. enrolled 80 patients with hyperuricemia and matched 160 subjects without hyperuricemia based on age and gender [33]. Serum BPA concentration in patients with hyperuricemia (1.83 ± 1.91 ng/mL) was significantly higher than that in non-hyperuricemia subjects (1.15 ± 1.52 ng/mL). After adjusting for confounders, serum BPA concentration was associated with a 1.93-fold (95% CI: 1.16, 2.84) increased risk of developing hyperuricemia. Furthermore, this research group designed a prospective study to confirm BPA as an independent risk factor of hyperuricemia [15]. At baseline, participants with higher serum BPA concentrations exhibited significantly elevated SUA levels. After six-year follow-up, participants within the high BPA group had a 2.42-fold (95% CI: 1.07, 5.48) increased risk of having hyperuricemia. However, those two studies both used serum BPA concentration (only reflecting the active part of BPA) to represent BPA exposure, which might underestimate the human body burden and its adverse effects [16]. Lee et al. measured urinary BPA, BPS, and BPF concentrations to reflect the body burden in children [14]. The median concentration was 1.58 μg/L for BPA, the detection rate of BPS and BPF was 41.9% and 23.5%, respectively. After adjusting for confounders, boys in the high BPS group had 0.41 mg/dL (95%CI: 0.16, 0.66) increased SUA levels. But the relatively small sample size (n = 489) restricted the extrapolation of the finding. In our study, significant associations were observed between BPS and ∑BPs exposure and SUA levels. Our findings along with the aforementioned studies, further substantiate the detrimental impact of bisphenols on purine metabolism.
BPS and BPF were recently introduced as alternatives to BPA, resulting in a comparable yet relatively lower body burden. In the present study, the median concentrations of BPA, BPS, and BPF in total population were 1.2 μg/L, 0.5 μg/L, and 0.3 μg/L, respectively. The median concentrations of BPA, BPS, and BPF for general individuals in Wuhan, China were 0.60 μg/L, 0.27 μg/L, and 0.26 μg/L, respectively [9]. Similar distribution also can be found in India, Japan, and other countries [34, 35]. With the volume production and widespread application of BPS and BPF as substitutes for BPA, their increased body burden and potential adverse effects deserve more attention. Although some reviews had summarized the similarities among BPA, BPS, and BPF, their disparities worth deeply exploring. The oral systemic bioavailability of BPS was 250 times greater than that of BPA [36]. BPS exerted the greatest efficacy on 17α-OH progesterone while BPF exhibited the highest efficacy on progesterone. BPS was predicted to serve as a substrate for CYP2C9, while BPA and BPF were anticipated to act as substrates for CYP3A4 [37]. Liu et al. indicated that BPF rather than BPA and BPS had the highest risk quotient on the ecosystem [38]. Thoene et al. summarized that dietary BPS exposure caused more pathologies in the reproductive system compared to BPA and other analogs [38]. Considering the equal or higher toxicity of BPS and BPF, they should be under same legal supervision as BPA.
We found an NMDR relationship between BPA exposure and hyperuricemia prevalence. Calabrese and Baldwin inferred that about 40% of the dose-response relationships within the realm of endocrine disrupters were non-monotonic [39]. The established mechanisms of NMDR include but not limited to cytotoxicity, cell and tissue specific receptors and cofactors, receptor selectivity, receptor competition, receptor down-regulation, desensitization, negative feedback loops, and other downstream mechanisms [40]. The prevailing regulations and acceptable daily intake of BPA around the world are based on an assumption of monotonicity. However, the effects observed at high doses under NMDR curves do not accurately predict the effects of low doses, which are typically encountered by the general population. There is an urgent need for fundamental reform in chemical toxicity assessment and exposure standards.
Although the precise mechanism underlying the relationship between bisphenols exposure and hyperuricemia remains uncertain, enhanced activity of XO is presumed to play a vital role. XO, a rate-limiting enzyme in the liver for uric acid synthesis, exerted increased activity in response to BPA exposure, leading to heightened uric acid levels in serum and liver, but not in urine [33]. Furthermore, the circular dichroism and molecular docking analyses indicated that BPA altered the secondary structures of XO by binding to its Asp360 and Lys422 sites. Additionally, BPA has the potential to metabolize into bisphenol A 3,4-quinone, which could potentially enhance XO activity and subsequently increase uric acid synthesis [16]. ATP-binding cassette subfamily G member 2 (ABCG2) is identified as a high-capacity urate transporter and its dysfunction is linked to elevated SUA levels and an increased risk of hyperuricemia. Some studies had found down-regulated ABCG2 protein expression and damaged function after BPA treatment [41, 42]. Decreased renal function impedes uric acid excretion, resulting in its accumulation and consequent hyperuricemia. Environmental bisphenols exposure impairs renal function by reducing kidney tubule formation, inducing ferroptosis, increasing tubular injury, and might contribute to urate underexcretion [32, 43, 44]. Besides, bisphenols-induced oxidative stress could worsen renal function and further restrict urate excretion [44, 45]. No mediating effects of eGFR were found on the associations between bisphenols exposure and SUA levels, suggesting the presence of alternative, more specific mechanisms underlying these relationships.
Sex differences were noticed in our findings. Although urinary BPS concentrations were higher in males, the relationship between BPS exposure and SUA levels, as well as the prevalence of hyperuricemia, exhibited greater significance in females. In our study, females were older and have less physical activity in comparison to males. These detrimental factors could potentially amplify the impacts of BPS on females (Table S9). Besides, the higher prevalence of hyperuricemia among males can be attributed mainly to inherent genetic variants rather than external factors [46, 47]. Additional hypothesis-driven research is needed to further understand the sex-specific effects of BPS.
The strengths of our study included standardized laboratory analysis and the nationally representative of the subjects. However, the cross-sectional study design limits the ability to determine causality in the observed associations. Nonetheless, considering the numerous documented experiments and epidemiologic studies, it is more reasonable to hypothesize that bisphenols exposure influences uric acid levels, rather than the other way around. Second, bisphenols exposure conditions were assessed only in one urine sample, potential non-differential exposure misclassification could weaken the risk estimates. Consequently, in prospective studies, utilizing repeated urine samples to ascertain bisphenols exposure levels is recommended to validate our findings.
Conclusions
Environmental BPS and ∑BPs exposure showed positive associations with SUA levels in total and female population among US adults. The dose-response relationship between BPA exposure and hyperuricemia prevalence in total population conformed to an inverted “U” curve. Given the widespread use and adverse effects, our findings underline the need for the government to reassess the presence of bisphenols in daily life. Additional prospective studies and mechanical research are required to verify our findings and shed light on the precise mechanisms involved.
Availability of data and materials
The datasets presented in this study are accessible via online repositories (https://www.cdc.gov/nchs/nhanes/).
References
Rock KL, Kataoka H, Lai JJ. Uric acid as a danger signal in gout and its comorbidities. Nat Rev Rheumatol. 2013;9(1):13–23.
Kuo CF, Grainge MJ, Zhang W, Doherty M. Global epidemiology of gout: prevalence, incidence and risk factors. Nat Rev Rheumatol. 2015;11(11):649–62.
Dalbeth N, Gosling AL, Gaffo A, Abhishek A. Gout. Lancet. 2021;397(10287):1843–55.
Kim Y, Kang J, Kim G-T. Prevalence of hyperuricemia and its associated factors in the general Korean population: an analysis of a population-based nationally representative sample. Clin Rheumatol. 2018;37(9):2529–38.
Piao W, Zhao L, Yang Y, Fang H, Ju L, Cai S, Yu D. The Prevalence of Hyperuricemia and Its Correlates among Adults in China: Results from CNHS 2015-2017. Nutrients. 2022;14(19):4095. https://doi.org/10.3390/nu14194095.
Chen-Xu M, Yokose C, Rai SK, Pillinger MH, Choi HK. Contemporary Prevalence of Gout and Hyperuricemia in the United States and Decadal Trends: The National Health and Nutrition Examination Survey, 2007–2016. Arthritis Rheumatol. 2019;71(6):991–9.
Krishnan E, Lingala B, Bhalla V. Low-level lead exposure and the prevalence of gout: an observational study. Ann Intern Med. 2012;157(4):233–41.
Kuo CC, Weaver V, Fadrowski JJ, Lin YS, Guallar E, Navas-Acien A. Arsenic exposure, hyperuricemia, and gout in US adults. Environ Int. 2015;76:32–40.
Jiang S, Liu H, Zhou S, Zhang X, Peng C, Zhou H, Tong Y, Lu Q. Association of bisphenol A and its alternatives bisphenol S and F exposure with hypertension and blood pressure: a cross-sectional study in China. Environ Pollut. 2020;257:113639.
Almeida S, Raposo A, Almeida-González M, Carrascosa C. Bisphenol A: food exposure and impact on human health. Compr Rev Food Sci Food Saf. 2018;17(6):1503–17.
Cimmino I, Fiory F, Perruolo G, Miele C, Beguinot F, Formisano P, Oriente F. Potential Mechanisms of Bisphenol A (BPA) Contributing to Human Disease. Int J Mol Sci. 2020;21(16):5761. https://doi.org/10.3390/ijms21165761.
Ye X, Wong L-Y, Kramer J, Zhou X, Jia T, Calafat AM. Urinary concentrations of bisphenol A and three other bisphenols in convenience samples of US adults during 2000–2014. Environ Sci Technol. 2015;49(19):11834–9.
Chen D, Kannan K, Tan H, Zheng Z, Feng YL, Wu Y, Widelka M. Bisphenol Analogues Other Than BPA: Environmental Occurrence, Human Exposure, and Toxicity-A Review. Environ Sci Technol. 2016;50(11):5438–53.
Lee YJ, Lim YH, Shin CH, Kim BN, Kim JI, Hong YC, Cho YM, Lee YA. Relationship between bisphenol A, bisphenol S, and bisphenol F and serum uric acid concentrations among school-aged children. PLoS One. 2022;17(6):e0268503.
Hu J, Peng C, Li J, Gao R, Zhang A, Ma L, Zhang L, Yang Y, Cheng Q, Wang Y, et al. Serum Bisphenol A is an independent risk factor of hyperuricemia: A 6-year prospective study. Semin Arthritis Rheum. 2019;48(4):644–8.
Aekplakorn W, Chailurkit LO, Ongphiphadhanakul B. Association of serum bisphenol a with hypertension in thai population. Int J Hypertens. 2015;2015:594189.
Jiang S, Sun M, Zhou X, Xu Y, Ullah H, Niu X, Feng C, Gao Q. Association between blood manganese levels and depressive symptoms among US adults: a nationally representative cross-sectional study. J Affect Disord. 2023;333:65–71.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet (London, England). 2007;370(9596):1453–7. https://doi.org/10.1016/S0140-6736(07)61602-X.
Laboratory Procedure Manual for Uric Acid, NHANES 2015-2016. https://wwwn.cdc.gov/nchs/data/nhanes/2015-2016/labmethods/BIOPRO_I_MET_URIC_ACID_DXC800and660i.pdf. Accessed 17 Oct 2022.
Chittoor G, Voruganti VS: Chapter 53 - Hyperuricemia and Gout. In: Principles of Nutrigenetics and Nutrigenomics. edn. Edited by Caterina RDE, Martinez JA, Kohlmeier M. London: Elsevier, Academic Press, an Imprint of Elsevier; 2020. p. 389–394.
Choi HK, Atkinson K, Karlson EW, Willett W, Curhan G. Purine-rich foods, dairy and protein intake, and the risk of gout in men. N Engl J Med. 2004;350(11):1093–103.
Laboratory Procedure Manual for Personal Care and Consumer Product Chemicals and Metabolites [https://wwwn.cdc.gov/nchs/data/nhanes/2015-2016/labmethods/EPHPP_I_MET.pdf].
Rattan P, Penrice DD, Ahn JC, Ferrer A, Patnaik M, Shah VH, Kamath PS, Mangaonkar AA, Simonetto DA. Inverse Association of Telomere Length With Liver Disease and Mortality in the US Population. Hepatol Commun. 2022;6(2):399–410.
Tian X, Xue B, Wang B, Lei R, Shan X, Niu J, Luo B. Physical activity reduces the role of blood cadmium on depression: a cross-sectional analysis with NHANES data. Environ Pollut. 2022;304:119211.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, et al. A new equation to estimate glomerular filtration rate. Ann Internal Med. 2009;150(9):604–12.
Bakris G, Ali W, Parati G. ACC/AHA Versus ESC/ESH on Hypertension Guidelines: JACC Guideline Comparison. J Am Coll Cardiol. 2019;73(23):3018–26.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, Federici M, Filippatos G, Grobbee DE, Hansen TB, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1046–81.
Nelson RH. Hyperlipidemia as a risk factor for cardiovascular disease. Prim Care. 2013;40(1):195–211.
Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79(3):340–9.
Barr DB, Wilder LC, Caudill SP, Gonzalez AJ, Needham LL, Pirkle JL. Urinary creatinine concentrations in the US population: implications for urinary biologic monitoring measurements. Environ Health Perspect. 2004;113(2):192–200.
Kataria A, Trasande L, Trachtman H. The effects of environmental chemicals on renal function. Nat Rev Nephrol. 2015;11(10):610–25.
Ma L, Hu J, Li J, Yang Y, Zhang L, Zou L, Gao R, Peng C, Wang Y, Luo T, et al. Bisphenol A promotes hyperuricemia via activating xanthine oxidase. FASEB J. 2018;32(2):1007–16.
Asimakopoulos AG, Xue J, De Carvalho BP, Iyer A, Abualnaja KO, Yaghmoor SS, Kumosani TA, Kannan K. Urinary biomarkers of exposure to 57 xenobiotics and its association with oxidative stress in a population in Jeddah. Saudi Arabia Environ Res. 2016;150:573–81.
Liao C, Liu F, Alomirah H, Loi VD, Mohd MA, Moon HB, Nakata H, Kannan K. Bisphenol S in urine from the United States and seven Asian countries: occurrence and human exposures. Environ Sci Technol. 2012;46(12):6860–6.
Gayrard V, Lacroix MZ, Grandin FC, Collet SH, Mila H, Viguié C, Gély CA, Rabozzi B, Bouchard M, Léandri R, et al. Oral Systemic Bioavailability of Bisphenol A and Bisphenol S in Pigs. Environ Health Perspect. 2019;127(7):77005.
Rosenmai AK, Dybdahl M, Pedersen M. Alice van Vugt-Lussenburg BM, Wedebye EB, Taxvig C, Vinggaard AM: Are structural analogues to bisphenol a safe alternatives? Toxicol Sci. 2014;139(1):35–47.
Liu J, Zhang L, Lu G, Jiang R, Yan Z, Li Y. Occurrence, toxicity and ecological risk of Bisphenol A analogues in aquatic environment - A review. Ecotoxicol Environ Saf. 2021;208:111481. https://doi.org/10.1016/j.ecoenv.2020.111481.
Vandenberg LN, Maffini MV, Sonnenschein C, Rubin BS, Soto AM. Bisphenol-A and the great divide: a review of controversies in the field of endocrine disruption. Endocr Rev. 2009;30(1):75–95.
Vandenberg LN, Colborn T, Hayes TB, Heindel JJ, Jacobs DR Jr, Lee DH, Shioda T, Soto AM, vom Saal FS, Welshons WV, et al. Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic dose responses. Endocr Rev. 2012;33(3):378–455.
Nickel S, Mahringer A. The xenoestrogens ethinylestradiol and bisphenol A regulate BCRP at the blood-brain barrier of rats. Xenobiotica. 2014;44(11):1046–54.
Sieppi E, Vähäkangas K, Rautio A, Ietta F, Paulesu L, Myllynen P. The xenoestrogens, bisphenol A and para-nonylphenol, decrease the expression of the ABCG2 transporter protein in human term placental explant cultures. Mol Cell Endocrinol. 2016;429:41–9.
Bao L, Zhao C, Feng L, Zhao Y, Duan S, Qiu M, Wu K, Zhang N, Hu X, Fu Y. Ferritinophagy is involved in Bisphenol A-induced ferroptosis of renal tubular epithelial cells through the activation of the AMPK-mTOR-ULK1 pathway. Food Chem Toxicol. 2022;163:112909.
Yoo MH, Lee SJ, Kim W, Kim Y, Kim YB, Moon KS, Lee BS. Bisphenol A impairs renal function by reducing Na(+)/K(+)-ATPase and F-actin expression, kidney tubule formation in vitro and in vivo. Ecotoxicol Environ Saf. 2022;246:114141.
Huang M, Liu S, Fu L, Jiang X, Yang M. Bisphenol A and its analogues bisphenol S, bisphenol F and bisphenol AF induce oxidative stress and biomacromolecular damage in human granulosa KGN cells. Chemosphere. 2020;253:126707.
Zhang L, Spencer KL, Voruganti VS, Jorgensen NW, Fornage M, Best LG, Brown-Gentry KD, Cole SA, Crawford DC, Deelman E. Association of functional polymorphism rs2231142 (Q141K) in the ABCG2 gene with serum uric acid and gout in 4 US populations: the PAGE Study. Am J Epidemiol. 2013;177(9):923–32.
Bhole V, de Vera M, Rahman MM, Krishnan E, Choi H. Epidemiology of gout in women: Fifty-two–year followup of a prospective cohort. Arthritis Rheum. 2010;62(4):1069–76.
Acknowledgements
The authors would like to thank all contributors and participants in NHANES and thank Zhang Jing (Shanghai Tongren Hospital) for his work on the NHANES database. We sincerely thank Tabatha McNeill (National Center for Health Statistics, Division of Research Methodology) for her help in obtaining bisphenols data.
Funding
This research was supported by the Shandong Provincial Natural Science Foundation (ZR2021QH249), Research Fund for the Lin He’s Academician Workstation of New Medicine and Clinical Translation in Jining Medical University (JYHL2021MS20), PhD Research Foundation of Affiliated Hospital of Jining Medical University (2021-BS-006), Natural Science Foundation of Xinjiang Uygur Autonomous Region (2021D01A02), and 2022 key research and development program of Jining Science and Technology Bureau (2022YXNS031).
Author information
Authors and Affiliations
Contributions
Shunli Jiang: Conceptualization, Methodology, Validation, Data Curation, Writing-original draft, Writing-review & editing, Supervision, Funding acquisition. Yongxin Wang and Zengliang Wang: Methodology, Software, Formal analysis, Data curation, Writing - Review & Editing. Yaru Xu, Xi Li, and Mingjia Sun: Methodology, Writing - Review & Editing. Bo Li: Conceptualization, Methodology, Validation, Supervision, Writing-review & editing.
Corresponding authors
Ethics declarations
Ethics approval consent to participate
The study protocol was approved by the research ethics review board of the National Center for Health Statistics of the Centers for Disease Control and Prevention. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. STROBE Checklist for Cross-sectional Studies. Table S2. Associations of urinary bisphenols concentrations with serum uric acid levels (μmol/L), excluding individuals with anti-gout treatment. Table S3. Associations of urinary bisphenols concentrations with hyperuricemia prevalence, excluding individuals with anti-gout treatment. Table S4. Associations of urinary bisphenols concentrations with serum uric acid levels (μmol/L), adjusting drinks, organ and seafood intake. Table S5. Associations of urinary bisphenols concentrations with hyperuricemia prevalence, adjusting drinks, organ and seafood intake. Table S6. Associations of urinary bisphenols concentrations with gout prevalence, adjusting drinks, organ and seafood intake. Table S7. Associations of urinary bisphenols concentrations with eGFR levels. Table S8. Mediating effects of eGFR on the associations between urinary bisphenols and serum uric acid levels (μmol/L). Table S9. Sex difference of the study population, NHANES 2013-2016.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiang, S., Wang, Y., Wang, Z. et al. Bisphenol A and its alternatives bisphenol S and F exposure with serum uric acid levels, hyperuricemia, and gout prevalence among US adults: a nationally representative cross-sectional study. BMC Public Health 24, 370 (2024). https://doi.org/10.1186/s12889-024-17883-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-17883-6