Abstract
Background
Oral Contraceptive Pills (OCPs) are among the most commonly used forms of contraception, but they are associated with several health benefits and risks. This study aims to determine the gap in knowledge of the underlying health benefits and risks of OCPs among Lebanese women and to identify the factors that might influence their beliefs.
Methods
A questionnaire was completed by 817 Lebanese women aged 18–64 years old and assessed sociodemographic details, medical information, contraceptive practices, knowledge of underlying health benefits and risks, and information needs related to OCPs.
Results
Among the total participants, 41.5% of women reported using OCPs at some point in their lives yet 46.6% denied receiving information about their benefits and 48% denied receiving information about their risks. The mean total OCP knowledge score was 5.70 out of 25, the mean OCP risk knowledge score was 4.09 out of 15, and the mean OCP benefit knowledge score was 0.77 out of 6. Sociodemographic factors associated with greater total knowledge, risk knowledge and benefit knowledge included OCP usage, being a student, confidence in one’s knowledge and satisfaction with one’s information. Both the total and risk knowledge scores were found to be higher in women who found that receiving information related to OCPs was important. Finally, participants who lived in central governates had greater total knowledge scores, whereas those with higher levels of education and a family history of endometrial cancer demonstrated better benefit knowledge.
Conclusions
This study highlighted the poor knowledge of health benefits and risks associated with OCP use among Lebanese women and the associated sociodemographic factors that might influence their beliefs.
Similar content being viewed by others
Background
Oral Contraceptive Pills (OCPs) are not only used for family planning and pregnancy prevention [1,2] but also for their non-contraceptive benefits like in the setting of hormonal imbalances and menstrual and gynecological disorders [3,4,5]. In addition, OCPs have been shown to have protective roles against endometrial cancer and ovarian cancer [6,7,8,9] that a majority of women are not aware of, as shown in a Canadian study [10]. On the other hand, they have significant health risks including venous thromboembolism, hypertension, stroke, cervical cancer, and possibly breast cancer [4,11,12]. Interestingly, a study in Saudi Arabia showed that 61.6% of uneducated women and 51.4% of educated women did not consider thromboembolism as a side effect of OCPs [13]. Furthermore, previous studies showed that many women have refrained or discontinued OCPs for reasons like concerns about side effects, [14,15,16] the desire to conceive, [2] inconvenience and forgetfulness, [17,18,19] religious constraints, [20] cultural restrictions, [21] as well as fear of fertility changes [19]. In addition, some beliefs that women have about OCPs including fear of subfertility after discontinuation or weight gain have been reported as misconceptions due to their lack of scientific evidence [22,23]. This was noted in a study in Turkey that reported that 13.4% of women believed such misconceptions while another 41.9% were not sure of the risk of infertility due to OCPs [22].
These beliefs can be explained by an inadequate knowledge [4,11,12] which can promote the haphazard use of OCPs and amplify the underlying health risks and side effects [18,24]. Studies addressing knowledge, attitude, and practice towards OCPs have been conducted in many countries and have highlighted the influence of socio-demographic, cultural, and educational differences on those variables and most have found a positive correlation between OCP knowledge and higher educational levels, being married, longer duration of use and older age [2,12,18,25,26]. Research regarding knowledge about the benefits and harms of OCPs is minimal in the Arab region [24] and when it comes to Lebanon, previous studies have evaluated the extent of knowledge and the practice of contraception exclusively among Lebanese university students [5,27]. However, limited data is found on Lebanese women’s awareness on the potential benefits and harms of OCPs. In addition, no prior research in Lebanon has evaluated the differences between the perceived knowledge and actual knowledge regarding OCPs and the sociodemographic factors that might influence them.
Given that poor knowledge can be associated with negative outcomes on women and reproductive health, we conducted this study to assess the knowledge of Lebanese women regarding the health benefits and risks associated with OCPs and to determine the factors that may influence their beliefs.
Materials and methods
Study design
We conducted a cross-sectional study over a period of 3 months, from January 2023 to March 2023, to assess the knowledge of health benefits and risks of OCPs among Lebanese women.
Participants and sample size
Women aged 18–65, with Lebanese citizenship and residing in Lebanon are eligible to participate in this study, with no a priori exclusion criteria. The sample size was calculated using Epi Info™ (Center for Disease Control, Atlanta, GA, USA. Available from: http://wwwn.cdc.gov/epiinfo). Based on the 2022 population statistics (Available from: http://cas.gov.lb), the estimated population in Lebanon is 6,825,445 with 80% being Lebanese. From a total of 5,460,356 Lebanese, 51.1% are females of which 56.4% are between 19 and 64 years of age. This yields a target population of approximately 1,618,340 Lebanese women. With a 95% confidence interval (CI) and a ± 3.5% margin of error, a minimum sample size of 784 participants is needed.
Procedure
The Institutional Review Board at the Lebanese American University gave approval for the study (LAU.SOM.MC1.19/Dec/2022), and informed consent was obtained from all participants. Participation was voluntary, anonymous, and confidential. Detailed information and explanation of the scope and objectives of the study were included in the invitation to participate. Collected data was encrypted and downloaded on password protected computers and was available as de-identified electronic data in Microsoft Excel spreadsheets and SPSS files.
Materials
Data was collected through an anonymous online questionnaire via Google Forms constructed based on “Women’s Knowledge Beliefs and Information Needs in Relation to the Risks and Benefits Associated With Use of The Oral Contraceptive Pill” [6] after receiving approval from one of the authors.
The questionnaire was available in both English and Arabic and was electronically distributed via social media platforms such as emails, WhatsApp groups and Instagram.
Before administration, the questionnaire was pilot-tested with a sample of 20 Lebanese women to identify any ambiguities or issues in the questions.
Then, with the help of an expert in reproductive health, the questionnaire was reviewed to ensure it covers the relevant content adequately. As such, the questionnaire was tailored to address the cultural nuances of our study population.
Initially, sociodemographic, medical characteristics and information about the practice of OCPs were gathered. Participants were then asked whether they have received information related to OCPs and discussed using them with a health professional. The perceived knowledge of the health benefits and risks of OCPs was assessed with a 5-point scale and the actual knowledge was determined by asking participants to indicate whether they thought OCP use decreased, increased, or did not affect the risk of 25 different medical conditions. Finally, feedback on information needs related to OCPs was determined by assessing the perceived importance on receiving information with a 5-point scale, their main source of information, the satisfaction with their information with a 5-point scale, and their preferred methods for receiving information.
Knowledge was defined as the ability to correctly identify the health benefits and risks of OCPs. A total knowledge score, a benefit knowledge score and a risk knowledge score were computed and accounted for 1 point for the correct answer and no point for an incorrect answer. The total knowledge score ranged from 0 to 25, the benefit knowledge score ranged from 0 to 6 and the risk knowledge score ranged from 0 to15 with higher values indicating better OCP knowledge.
Statistical analysis
The collected data was available as de-identified electronic data in Microsoft Excel spreadsheets and SPSS files.
Descriptive statistics were performed using frequencies and percentages for categorical variables and means and standard deviations for continuous variables.
The mean knowledge scores were determined, and bivariate analysis was performed to determine differences in the knowledge and attitudes of participants towards OCPs according to sociodemographic characteristics. The student t-test was used to compare two means of continuous variables between dichotomous groups, ANOVA to compare between three or more means and the chi-square test to compare percentages. All variables that showed a p-value of < 0.25 in the bivariate analysis were included in the multivariable analyses to avoid potential confounders. Separate multivariable analyses to determine key factors associated with better knowledge among respondents were done using linear regression analysis and three models were analyzed for the total knowledge, health risks knowledge and health benefits knowledge scores, respectively. Data was presented along with 95% confidence intervals and a p value of < 0.05 was considered statistically significant.
Results
Sociodemographic characteristics
A total of 852 Lebanese women participated in this study, of whom 35 were excluded due to incompatibility with the inclusion criteria thus yielding a total of 817 participants between the ages of 18 and 64 who were willing to participate after filling an informed consent.
The sociodemographic characteristics are summarized in Table 1.
Practice of OCPs
Among the total participants, 339 (41.5%) of women reported OCP use at some point in their lives. The mean age of onset of OCP use was 24 years (SD = 6.7) with approximately one third of participants using them for over 6 months (35.7%). The main reasons for OCP use (N = 339) were for menstrual cycle regulation (48.4%) followed by pregnancy prevention (44%). Most participants who discontinued (33%) or stopped (30.8%) OCPs were concerned about side effects. The mains reasons for OCP use, discontinued use, and nonuse are summarized in Table 2.
Information related to oral contraceptive pills
Among responders (N = 817), 46.6% denied receiving information about the health benefits of OCPs and 48% denied receiving information about the health risks of OCPs. Most participants (53%) reported never discussing OCP use with healthcare professionals although the main source of information was from healthcare professionals (42.1%) and the majority preferred receiving information through medical consultations (66%).
Self-assessment of knowledge of health benefits and health risks of OCPs
The mean knowledge score was 5.70 (SD = 4.88) out of 25, the mean risk knowledge score was 4.09 (SD = 3.88) out of 15, and the mean benefit knowledge score was 0.77 (SD = 1.17) out of 6. Furthermore, 35.3% of participants felt fairly confident with their knowledge, more than 60% indicated they were not satisfied with their knowledge but 77.5% of women found that receiving information related to OCPs was extremely important (Fig. 1).
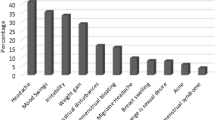
Women were aware that OCP use increased the risk of depression (52%), nausea (40.4%), headaches and migraines (43.3%). However, when it comes to serious health risks, few women knew the increased risks of hypertension (28.4%), thromboembolism (25.1%), cervical cancer (26.2%), and breast cancer (29%) associated with OCP use. Similarly, few participants were aware of their non-contraceptive use against acne (23%), dysmenorrhea and menorrhagia (26.6%) as well as their protective role against endometrial cancer (12%), ovarian cancer (8.8%), pelvic inflammatory disease (4.5%), and benign breast disease (2.4%). The results of the self-assessment regarding the association between OCPs and different medical conditions are summarized in Fig. 2A and B.
Correlates of knowledge
The results of the bivariate analyses are shown in Table 3. Higher OCP knowledge scores were seen in OCP users (mean = 7.05, SD = 4.7), young adults (mean = 6.64, SD = 5.14), single women (mean = 6.39, SD = 5.12), women without children (mean = 6.42, SD = 5.2), students (mean = 6.90, SD = 5.12), and participants with post-graduate degrees (mean = 6.13, SD = 4.85).
The results of the multivariable analysis are shown in Table 4.
In the first model, the dependent variable is the total knowledge score of OCPs whereas the independent variables are the following sociodemographic factors: age, OCP use, occupation, governate of residence, family history of heart disease, confidence in knowledge, importance of receiving information and satisfaction with information.
Based on this model, living in central governates such as Beirut and Mount Lebanon (B = 0.575, p = 0.044), using OCPs (B = 1.632, p < 0.001), and being a student (B = 2.240, p < 0.001) were associated with a higher OCP knowledge score whereas older age (B = -0.891, p < 0.001), being unemployed (B = -1.004, p = 0.007), and having a family history of heart disease (B = -0.483, p = 0.024) were associated with a lower OCP knowledge score.
In addition, the knowledge score also increased for every unit increase in the confidence in OCP knowledge (B = 1.184, p < 0.001), the perceived importance of receiving information related to OCPs (B = 0.382, p = 0.01), and the satisfaction with the information related to OCPs (B = 0.915, p < 0.001).
In the second model, the dependent variable is the risk knowledge score of OCPs whereas the independent variables are the following sociodemographic factors: age, OCP use, occupation, family history of heart disease, confidence in knowledge, importance of receiving information and satisfaction with information.
Based on that model, OCP use (B = 0.822, p < 0.001) and being a student (B = 1.322, p < 0.001) were associated with a higher risk knowledge score, whereas older age (B= -0.781, p < 0.001) and having a family history of heart disease (B = -0.437, p = 0.014) were associated with a lower risk knowledge score. Results of the self-assessment (Fig. 2B) showed significantly high percentages of incorrect answers although most participants felt reasonably confident about their knowledge in OCPs.
The risk knowledge score also increased with the confidence in OCP knowledge (B = 0.851, p < 0.001), the perceived importance of receiving information related to OCPs (B = 0.303, p = 0.01), and the satisfaction with the information related to OCPs (B = 0.649, p < 0.001).
In the third model, the dependent variable is the benefit knowledge score of OCPs whereas the independent variables are the following sociodemographic factors: OCP use, level of education, parental status, family history of endometrial, confidence in knowledge and satisfaction with information.
For the that model, the results showed that OCP use (B = 0.467, p < 0.001), being a student (B = 0.313, p = 0.005), having a higher level of education (B = 0.220, p < 0.001), and having a family history of endometrial cancer (B = 0.095, p = 0.021) were associated with a higher benefit knowledge score (p < 0.001) whereas having children (B = -0.179, p = 0.068) was associated with a lower benefit knowledge score.
Similarly, the benefit knowledge score also increased with the confidence in OCP knowledge (B = 0.161, p < 0.001) and the same can be said about satisfaction with the information related to OCPs (B = 138, p < 0.001).
Collinearity was checked by examining the Correlation Matrix of the independent variables and high correlations [28] (close to 1 or -1) between pairs of variables were not detected. Moreover, based on the collinearity statistics report, the calculated VIF for each predictor in the model was around 1.0. Commonly, a VIF greater than 10 is often considered an indicator of problematic collinearity and it was not found in our results.
Discussion
This study highlighted shortcomings in the knowledge of health benefits and risks related to OCPs among Lebanese women, despite OCPs being the most widely used contraceptive method. In addition, it identified several sociodemographic factors associated with better total, risk and benefit knowledge.
Our findings showed that most participants were aware of the association between OCP use and depression, nausea, headaches, and migraines which can be due to them being more commonly experienced and more spoken about among Lebanese women, as demonstrated by Abi Tayeh et al. [5] However, few women were able to identify important risks associated with OCPs like cardiovascular conditions and cancer. Similarly, few women were aware of the non-contraceptive benefits, even though a significant portion used them for such purposes. These findings are comparable to other studies conducted by Gaudet et al., Machado et al., and in Saudi Arabia [13,29]. It’s also important to consider that some medical conditions might not be well-understood by participants [14].
Similar to other studies, [14,30] a lot of participants believed the misconceptions associated with OCP use like infertility and weight gain, despite the lack of scientific evidence [22,23].
Furthermore, our study found that following the self-assessment, most participants indicated that they were unsatisfied with their knowledge but demonstrated a positive attitude given that the vast majority deemed receiving information related to OCPs extremely important.
These findings highlight the need to promote health education on overlooked health benefits and health risks but also to address common misconceptions.
Several variables were found to be independently associated with knowledge of the health benefits and risks of OCPs. For instance, women living in central Lebanese areas like Beirut and Mount Lebanon were found to be more knowledgeable about OCPs which can be due to easier access to sources of information and greater ability to afford OCPs [31]. Also, OCP users demonstrated greater knowledge scores which can be attributed to their personal experience or from information provided by physicians [6,19]. Furthermore, higher OCP benefit knowledge scores were found to be associated with higher educational levels and a family history of endometrial cancer. This can be explained by the fact that women with a higher education are more capable of grasping and applying gained information to promote good health [6,12,32,33]. Furthermore, participants with a family history of endometrial cancer are more likely to research their relatives’ illness and thus be aware of the non-contraceptive benefits of OCPs. Finally, confidence in OCP knowledge, the importance of receiving information about OCPs, and the satisfaction with information related to OCPs were correlated with higher knowledge scores, as seen with Philipson et al. [6]
In contrast, our study showed that variables like older age and unemployment were associated with lower OCP knowledge. This suggests that women past the reproductive age are less likely to be taking OCPs and therefore less informed about them [34]. However, this finding is contradicting with a study conducted by Al-Mass et al. in 2018 [24]. In addition, unemployed women with limited access to OCPs or lower income are less likely to be informed about OCPs [34]. Unexpectedly, women with a family history of heart disease appeared to be less knowledgeable about OCPs and this can be partially explained by the high prevalence of heart diseases in Lebanon which can lead to the underestimation of the seriousness of these diseases and the lack of awareness of the negative association with less standard risk factors such as OCP use. Parental status was also found to be associated with a lower benefit knowledge score; this suggests that women with children are no longer interested in family planning and thus unaware of the non-contraceptive benefits of OCPs [35].
Monthly income also showed a statistically significant correlation with the knowledge score (p = 0.011) and benefit knowledge score (p < 0.001). However, it was not included in the multivariable linear regression due to the ongoing economic collapse in Lebanon.
Finally, most participants did not discuss OCP use with healthcare professionals, despite considering them their main source of information. As such, this unilateral approach of doctor-patient relationship reveals a gap in OCP knowledge. To optimize a patient’s health decisions and treatment plan, there must be a two-sided relationship between the patient and their healthcare professional with both parties engaging in gaining knowledge and making informed decisions. Although it is the health professional’s responsibility to provide the necessary information, the patient must be willing to obtain and process what is provided to make sound decisions and be aware of the health benefits and risks of OCPs; this is known as health literacy [36,37]. Prior studies have demonstrated the inadequate health literacy among Lebanese women as well as its negative association with low education [38] and socioeconomic status [39]. Therefore, proper health literacy serves as a valuable complement to health professionals in providing the necessary information and securing a greater knowledge of the health benefits and risks of OCPs. Patients can increase their health literacy through several practical measures such as proactively seeking answers through medical consultations or other reliable sources. In addition, participating in campaigns can promote self-awareness, foster knowledge about OCPs and encourage discussions with other attendees and health professionals.
Strength and limitations
To our knowledge, this study is the first to assess the knowledge of health benefits and risks of OCPs and their association with sociodemographic factors to address information needs among Lebanese women. A strong aspect of this study was its large sample size and the inclusion of women from different governates. Another important consideration is the well-constructed questionnaire that was used in a previous study conducted by Philipson et al. [6] which included important knowledge parameters. Furthermore, when analyzing key determinants that predict knowledge scores, 3 different models were computed for the total knowledge, health risks knowledge and health benefits knowledge scores, respectively.
The limitations of the study are inherent due to the cross-sectional design of our study. Although we had a relatively big sample size including women across Lebanon, yet the sample may not be representative of all the Lebanese population due to selection bias.
In addition, the distribution of the online questionnaire through social media may be limited to those with internet access.
Conclusion
In conclusion, there’s poor knowledge about the health benefits and risks of OCPs especially among women with sociodemographic factors like older age, unemployment, a family history of heart disease, and parenthood. This limited awareness can influence both attitude and views, adversely affecting reproductive health.
In addition, health literacy plays a fundamental role in helping individuals understand health information, make informed decisions about their treatment plans, and communicate effectively with their healthcare providers.
As such, additional research should focus on assessing the impact of low OCP knowledge and low health literacy on reproductive health. This emphasizes the need to address this issue on a national level by implementing strategies to raise awareness and educate Lebanese women, while considering sociodemographic factors that might influence their beliefs.
Future prospective studies are warranted to evaluate the efficacy and outcomes of such strategies in improving the gap in knowledge of OCPs.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- OCP:
-
Oral Contraceptive Pill
References
Jones R. Beyond Birth Control: The Overlooked Benefits Of Oral Contraceptive Pills.; 2011.
Mubashar H, Almushait M, Sukit B, Shaamash A, Handady S, Almutawa N, Knowledge. Attitude and Practice of Contraceptives among Saudi women in Aseer Region, Saudi Arabia. Bangladesh J Med Sci (Ibn Sina Trust) 2016 Nov 3,;15(3):430–4.
Schindler AE. Non-contraceptive benefits of oral hormonal contraceptives. Int J Endocrinol Metabolism. 2013;11(1):41–7.
Dokras A. Noncontraceptive use of oral combined hormonal contraceptives in polycystic ovary syndrome—risks versus benefits. Fertil Steril. 2016;106(7):1572–9.
Abi Tayeh G, Khalil K, Khoury A, Maalouf S, Mansour F, Attieh E et al. Contraception knowledge and practices among students in Lebanese universities. J Biosocial Sci 2022 Jun 15,:1–11.
Philipson S, Wakefield CE, Kasparian NA. Women’s Knowledge, Beliefs, and Information Needs in Relation to the Risks and Benefits Associated with Use of the Oral Contraceptive Pill. Journal of women’s health (Larchmont, N.Y. 2002) 2011 Apr 1,;20(4):635–642.
Machado RB, de Melo NR, Prota FE, Lopes GP, Megale A. Women’s knowledge of health effects of oral contraceptives in five Brazilian cities. Contracept (Stoneham). 2012;86(6):698–703.
Davidson BA, Moorman PG. Risk-benefit assessment of the combined oral contraceptive pill in women with a family history of female cancer. Exp Opin Drug Saf. 2014;13(10):1375–82.
Iversen L, Sivasubramaniam S, Lee AJ, Fielding S, Hannaford PC. Lifetime cancer risk and combined oral contraceptives: the Royal College of General Practitioners’ Oral Contraception Study. American journal of obstetrics and gynecology 2017;216(6):580.e1-580.e9.
Gaudet LM, Kives S, Hahn PM, Reid RL. What women believe about oral contraceptives and the effect of counseling. Contracept (Stoneham). 2004;69(1):31–6.
Carlton C, Banks M, Sundararajan S. Oral Contraceptives and Ischemic Stroke Risk. Stroke (1970) 2018;49(4):e157-e159.
Alameer MI, Muqri KY, Awlaqi AA, Azyabi FY, Yaqoub AM, Suhail HM et al. Knowledge, attitude and practices regarding contraceptive pill and its side effects among women in Jazan Region, Saudi Arabia. Clin Pract 2022 Apr 29,;12(3):268–75.
Alshardan A, Bari M, AlSinan I, AlMuqhim M, AlRazeyg N. Knowledge and use of contraceptives among women in Al-Kharj City, Saudi Arabia. Int J Med Developing Ctries 2020:902–9.
Vogt C, Schaefer M. Disparities in knowledge and interest about benefits and risks of combined oral contraceptives. Eur J Contracept Reproductive Health care. 2011;16(3):183–93.
Bardaweel SK, Akour AA, Kilani MZ. Current knowledge, attitude, and patterns of oral contraceptives utilization among women in Jordan. BMC Women’s Health 2015 Dec 14,;15(1):117.
Stewart M, Black K. Choosing a combined oral contraceptive pill. Australian Prescriber. 2015;38(1):6–11.
Rosenberg MJ, Waugh MS. Oral contraceptive discontinuation: a prospective evaluation of frequency and reasons. Am J Obstet Gynecol. 1998;179(3):577–82.
Lee J, Jezewski MA. Attitudes toward oral contraceptive use among women of reproductive age: a systematic review. Adv Nurs Sci. 2007;30(1):E85–E103.
Hall KS, Castaño PM, Westhoff CL. The Influence of Oral Contraceptive Knowledge on Oral Contraceptive Continuation Among Young Women. Journal of women’s health (Larchmont, N.Y. 2002) 2014 Jul 1,;23(7):596–601.
Nsubuga H, Sekandi JN, Sempeera H, Makumbi FE. Contraceptive use, knowledge, attitude, perceptions and sexual behavior among female University students in Uganda: a cross-sectional survey. BMC Women’s Health 2016 January 27,;16(6):6.
Lim HJ, Kazumi U, Cho YH. A comparative study of knowledge and attitude on oral contraceptive between Korean and Japanese University students. Yŏsŏng Kŏn’gang Kanho Hakhoe Chi. 2002;8(4):471.
Küçük M, Aksu H, Sezer SD. Misconceptions about the side effects of combined oral contraceptive pills. Gynecol Endocrinol. 2012;28(4):282–5.
Gallo MF, Lopez LM, Grimes DA, Carayon F, Schulz KF, Helmerhorst FM et al. Combination contraceptives: effects on weight. Cochrane Database of Systematic Reviews 2014 Jan 29,;2014(1):CD003987.
Al-Mass AA, Al-Shahrani BS, Al-Mweisheer AN, Tulbah SA, Syed S, Razique A, et al. User experience, knowledge and practice of oral. Contraceptive: a study from Riyadh, Saudi Arabia. Annals of Medical and Health Sciences Research. 2018;8(6):411–9.
Chopra S, Dhaliwal L. Knowledge, attitude and practices of contraception in urban population of North India. Arch Gynecol Obstet. 2010;281(2):273–7.
Gothwal M, Tak A, Aggarwal L, Rathore A, Singh P, Yadav G et al. A study of knowledge, attitude, and practice of contraception among nursing staff in all India Institute of Medical Sciences, Jodhpur, Rajasthan. J Family Med Prim Care 2020 Febr 1,;9(2):706–10.
Barbour B, Salameh P. Knowledge and practice of university students in Lebanon regarding contraception. East Mediterr Health J. 2009;15(2):387–99.
Cohen JA, Power Primer. Psychol Bull 1992 Jul 1,;112(1):155–9.
Al Basri SF, Al Abdali JA, Alzubaidi HM, Almarhabi AA, Alzubaidi MA, Al Qarni G et al. Knowledge of Reproductive Age Women about oral contraceptive pills in Al-Qunfudah, Saudi Arabia. Open Access Journal of Clinical Trials 2022 Jan 1,;13:61–71.
Picardo CM, Nichols M, Edelman A, Jensen JT. Women’s knowledge and sources of information on the risks and benefits of oral contraception. J Am Med Womens Assoc (1972) 2003;58(2):112–116.
Mahadeen AI, Khalil AO, Hamdan-Mansour AM, Sato T, Imoto A. Knowledge, attitudes and practices towards family planning among women in the rural southern region of Jordan/ Connaissances, attitudes et pratiques des femmes en matiere de planification familiale dans le sud rural de la Jordanie. East Mediterranean Health J 2012 Jun 1,;18(6):567.
Al-Shaikh GK, Mayet AY, Alshaikh MK, Hamad AF, Mahmoud MA, Aljadhey HS. Knowledge on adherence and safety of the oral contraceptive pill in Saudi women. Saudi Med J. 2012;33(6):665–70.
Amwonya D, Kigosa N, Kizza J. Female education and maternal health care utilization: evidence from Uganda. Reproductive Health 2022 Jun 20,;19(1):1–142.
Shamrani HM, Shamrani AF, Alsaggaf AE, Khojah MI, Alafif MM, Tayeb SO et al. Knowledge, attitude and practice of women in Jeddah towards the use of oral contraceptive pills. Saudi J Intern Med 2017 Dec 31,;7(2):5–10.
Phipps MG, Matteson MDMPH, Fernandez KAMDMPH, Chiaverini GEMD, Weitzen LMPH. S, PhD. Characteristics of women who seek emergency contraception and family planning services. Am J Obstet Gynecol 2008 Aug 1,;199(2):111.e1-111.e5.
Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, Brand H, HLS-EU) Consortium Health Literacy Project European. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. https://doi.org/10.1186/1471-2458-12-80.
Bouclaous C, Haddad I, Alrazim A, Kolanjian H, El Safadi A. Health literacy levels and correlates among refugees in Mount Lebanon. Public Health (London). 2021;199:25–31.
El Khoury G, Salameh P. Assessment of the awareness and usages of family planning methods in the Lebanese community. BMJ Sex Reproductive Health 2019 Oct 1,;45(4):269–74.
Bouclaous Carmel H, Samer S, Ahmad G, Namir S, El HJ, Bou MM, et al. Health Literacy Levels and predictors among Lebanese adults visiting outpatient clinics in Beirut. HLRP: Health Literacy Research and Practice. 2021;5(4):e295–e309.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MI and LK designed and coordinated the study and were major contributors in interpreting the data and writing the manuscript. GB and YG collected data and contributed to the literature review. MC performed the statistical analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board at the Lebanese American University gave approval to conduct this study (LAU.SOM.MC1.19/Dec/2022), and informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ibrahim, M.J., Khalife, L.E., Ghanem, Y.D. et al. Gap in knowledge of health benefits and risks of combined oral contraceptives among Lebanese women. BMC Public Health 24, 60 (2024). https://doi.org/10.1186/s12889-023-17439-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17439-0