Abstract
Objective
This prospective study aimed to evaluate the effects of a health education intervention on cardiovascular disease (CVD) risk factors among school teachers.
Methods
The study, conducted from August 2016 to May 2017, involved teachers from four schools in Baruipur, West Bengal, India. It was a multicentric, quasi-experimental study with an intervention group receiving tailored health education promoting lifestyle modifications, while the control group received no intervention. Baseline and endline assessments included behavioural and biological characteristics related to cardiovascular health and risk assessment. Data were analysed using JAMOVI.
Results
The intervention group showed significant improvements in physical activity levels [Cohen’s d (Cd): 0.43, p = 0.006] and the consumption of fruits and vegetables (Cd: 1.00, p = < 0.001). Notably, there was a considerable reduction in the consumption of salt (Cd: -0.93, p = 0.039), oil (Cd: -0.98, p = < 0.001), fast food (Cd: -0.99, p = < 0.001), junk food (Cd: -0.99, p = < 0.001), and red meat (Cd: -1.00, p = < 0.001) among participants. However, there were no significant improvements in biological characteristics within the intervention group. In contrast, the control group exhibited no significant changes in behavioural and biological characteristics compared to baseline. The intervention group showed a minor non-significant reduction (3.0%) in their 10-year cardiovascular risk compared to baseline (Cd: -1.00, p = 0.50), while the control group had a negligible non-significant increase (0.7%) in their cardiovascular risk (Cd: 1.00, p = 1.00).
Conclusion
Health education intervention positively influenced behavioural characteristics, such as physical activity and dietary habits, among school teachers. However, no significant improvements were observed in biological characteristics or cardiovascular risk factors.
Similar content being viewed by others
Introduction
Cardiovascular diseases (CVDs) are a leading global cause of death, claiming over 17 million lives annually. They account for 32% of all deaths worldwide, surpassing other non-communicable diseases, cancers, respiratory diseases, and diabetes. By 2030, CVDs are projected to cause around 23.6 million deaths, with 80% occurring in low- and middle-income countries [1,2,3,4]. In India, non-communicable diseases, including CVDs, contribute to 60% of adult deaths, with CVDs alone responsible for 26% of these fatalities. Alarmingly, a significant proportion of CVD deaths occur in individuals aged 30 to 69 years, indicating an earlier onset compared to counterparts in economically developed countries. The prevalence of risk factors like sedentary lifestyles, overweight/obesity, and hypertension further exacerbates the situation [5,6,7].
Cardiovascular diseases (CVDs) encompass conditions affecting the heart, blood vessels, and brain, including heart attacks, strokes, and arterial diseases. CVD risk factors can be modifiable (e.g., tobacco use, physical inactivity, unhealthy diet, high blood pressure, obesity) or non-modifiable (e.g., age, gender, genetics). Lifestyle modifications are crucial for preventing and managing CVDs, and lifestyle programs involving healthy habits, dietary counselling, exercise training, and behavioural changes have proven effective in reducing heart disease, stroke, and diabetes. By addressing obesity, promoting healthy diets, and increasing physical activity, up to 80% of these diseases can be prevented. It is important to develop impactful strategies for screening, prevention, and intervention to combat CVDs [8,9,10].
Teaching, a sedentary occupation, increases the risk of non-communicable diseases, including cardiovascular diseases (CVDs) [11]. Limited research exists on CVD risk factors among teachers, despite their vulnerability to such diseases [12]. This study in Baruipur, India, aims to assess the impact of health education interventions on modifying CVD risk factors among school teachers. By improving knowledge and reducing risk factors, the study seeks to enhance intervention programs for teachers’ cardiovascular health, yielding positive outcomes. These findings can inspire policymakers to implement similar interventions for teachers and students, reducing the burden of non-communicable diseases, especially CVDs. With CVDs remaining a significant global health challenge, India has witnessed a rise in CVD-related deaths in urban and rural areas. Targeting modifiable risk factors becomes crucial for preventing and managing CVDs. Leveraging the influential role of school teachers provides a unique opportunity for interventions promoting healthier behaviours and reducing CVD risk factors.
Methods
Participants
This multicentric quasi-experimental study took place from August 2016 to May 2017 among teachers in four schools in Baruipur, a Kolkata suburb, West Bengal, India. We used simple random sampling (SRS) with replacement to select four clusters out of 18 in the Baruipur block, each containing an average of 18.5 ~ 19 schools. From each cluster, one school was chosen [13].
After securing permission and informed written consent from school heads, all teachers working in the study schools during baseline assessments were included. The four study schools were then randomly assigned to either the intervention or control group. Sample sizes were determined based on parameters from a similar study by Awosan et al. [12] in Nigeria since there were no prior Indian studies available. For systolic blood pressure (SBP), we estimated a mean difference of 2.87 with a standard deviation of 9.2, requiring a sample size of 66 per arm for 80% power and a 5% significance level. Similarly, for fasting blood sugar (FBS) and total blood cholesterol, sample sizes of 17 in each arm were calculated to detect differences of 6.69 mg/dl and 12.71 mg/dl, respectively, with their respective standard deviations [12]. We used the online sample size calculator Statulator [14] for these calculations.
The study enrolled 68 teachers in the intervention group and 62 in the control group, totalling 130 participants. Data collection schedules were coordinated with school authorities. We utilized a pre-designed, pretested, self-administered questionnaire, clinical examination, and laboratory blood investigations. Blood pressure and anthropometric measurements adhered to standard operating procedures. Female teachers received examinations with a female attendant to ensure privacy. Teachers arrived at school one hour before classes, following a 12-hour fasting period, for blood sample collection.
Intervention
We created an educational module covering key aspects of cardiovascular diseases (CVDs): common types, modifiable and non-modifiable risk factors, prevention, diabetes and obesity complications, and guidance on healthy diet, physical activity, stress management, and quitting addictions. This module adhered to guidelines from the National Institute of Nutrition, Indian Council of Medical Research (ICMR), and the World Health Organization (WHO) [15, 16]. We also prepared PowerPoint presentations (Annexure I) to enhance interactive lectures.
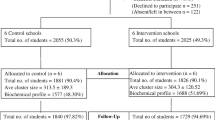
We conducted intervention sessions, approved by the Teacher-in-charge, in the teachers’ room or school auditorium using a laptop and projector, held on Saturdays after school hours without disrupting regular academic activities. We reinforced learning by repeating lectures twice per school with a one-month gap between. Interactive sessions addressed questions and clarified content. Handouts (Annexure II) aided retention. Three months post-intervention, we conducted an endline assessment using the same tools as the baseline, excluding background characteristics. Control schools received subsequent intervention sessions. Figure 1 illustrates the study processes.
Measures
Behavioural characteristics
Physical activity levels were assessed using the International Physical Activity Questionnaire Short Form (IPAQ-SF), with individuals reporting ≥ 600 metabolic equivalent (MET) per week classified as physically active [17, 18]. Meeting the recommended salt intake of < 5 g per day and consuming < 500 ml of oil per month aligned with guidelines [16, 19]. Meeting the recommendation for fruit and vegetable consumption meant consuming ≥ 400 g daily [19]. Tobacco users were defined as those reporting tobacco use in the past 30 days [20]. Stress levels were measured using the Perceived Stress Scale (PSS), consisting of four items, with higher scores indicating increased stress levels [21].
Biological characteristics
We adhered to standard operating procedures for measuring blood pressure, height, weight, waist circumference, and hip circumference. Fasting blood sugar (FBS) and lipid profiles, including total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglycerides, were assessed using established protocols [19, 20]. Individuals taking antihypertensive medication or with systolic blood pressure (SBP) ≥ 140 mm Hg and/or diastolic blood pressure (DBP) ≥ 90 mm Hg were classified as hypertensive. Those on antidiabetic medication or with FBS ≥ 126 mg/dl were considered diabetic. Obesity was defined as a body mass index (BMI) ≥ 25 kg/m², and central obesity as waist circumference > 80 cm for females and > 90 cm for males. A waist-hip ratio > 0.85 for females and > 90 cm for males indicated a higher risk.
Cardiovascular risk scores
We identified a higher risk for cardiovascular disease (CVD) as total cholesterol levels ≥ 200 mg/dl, LDL ≥ 130 mg/dl, and triglycerides ≥ 150 mg/dl, while a cardioprotective HDL level was defined as < 50 mg/dl for women and < 40 mg/dl for men [15, 19, 20, 22]. We calculated the Framingham 10-year cardiovascular risk score using age, sex, total and HDL cholesterol, smoking status, and blood pressure, following established calculation guidelines [23, 24]. The prevalence of metabolic syndrome was determined according to the new International Diabetes Federation (IDF) definitions [25].
Statistical analysis plan
We conducted data analysis using JAMOVI (version 2.3.26), an open-source statistical software [26]. Initially, we inputted the data into Microsoft Excel and then imported it into JAMOVI for analysis. Descriptive statistics included reporting quantitative and qualitative variables, using frequency (percentage) and median [interquartile range (IQR)]. To compare baseline and endline behavioural and biological characteristics related to cardiovascular health between the intervention and control groups, we employed the Mann-Whitney U test for qualitative variables and the Chi-square test for quantitative variables. Within each group, we used the Wilcoxon matched pair signed rank test for qualitative variables and McNemar’s test for quantitative variables to compare baseline and endline characteristics. We measured the effect size using Cohen’s D. In all quantitative analyses, a p-value < 0.05 was considered statistically significant, indicating significant differences between groups or within groups over time.
Results
In the intervention group, the median age of teachers was 36.5 years (IQR: 11), while in the control group, it was 37 years (IQR: 9). The median per capita monthly family income (PCMI) for the intervention and control groups was 143.2 USD (IQR: 116.2) and 147.7 USD (IQR: 120.5) respectively. Furthermore, the median years of experience for teachers in the intervention and control groups were 121.5 months (IQR: 116) and 107.7 months (IQR: 72) respectively. As for the median number of classes taught by them, it was 25 (IQR: 6) for the intervention group and 27 (IQR: 6) for the control group. It is important to note that there was a statistically significant difference in terms of background characteristics between the intervention and control groups. (Table 1)
The intervention group demonstrated significant improvements in physical activity levels (effect size: 0.43, p = 0.006) and increased consumption of fruits and vegetables (effect size: 1.00, p = < 0.001). Importantly, there was a notable decrease in the consumption of salt (effect size: -0.93, p = 0.039), oil (effect size: -0.98, p = < 0.001), fast food (effect size: -0.99, p = < 0.001), junk food (effect size: -0.99, p = < 0.001), and red meat (effect size: -1.00, p = < 0.001) among participants. However, when it came to biological characteristics, no significant improvements were noted in these parameters. In contrast, the control group did not show any significant changes in terms of behavioural and biological characteristics compared to the baseline assessments. Significant differences were observed between the intervention and control groups at baseline and at the end in terms of total cholesterol levels. Additionally, there were significant differences between the groups in baseline and endline measurements of FBS, WC, BMI, and triglycerides. (Tables 2 and 3)
There was a significant difference (effect size: 0.19, p = 0.035) in the 10-year cardiovascular risk between the intervention and control groups at baseline, with teachers in the intervention group having a higher risk. However, this difference became non-significant post-intervention (effect size: 0.14, p = 0.106). The intervention group exhibited a small non-significant decrease (3.0%) in their 10-year cardiovascular risk compared to baseline (effect size: -1.00, p = 0.50). In contrast, the control group showed a slight non-significant increase (0.7%) in their cardiovascular risk compared to baseline (effect size: 1.00, p = 1.00). (Table 4)
Discussion
The study aimed to assess the impact of an educational intervention program on cardiovascular disease (CVD) risk factors among school teachers, focusing on their background, behavioral, biological characteristics, and cardiovascular risk.
The intervention group displayed notable improvements in physical activity levels and increased consumption of fruits and vegetables, indicating the program’s effectiveness in promoting positive behavioral changes. These findings are consistent with prior research highlighting the success of health education interventions in encouraging physical activity and healthier dietary habits [27,28,29,30,31,32]. Moreover, the intervention group significantly reduced their consumption of salt, oil, fast food, junk food, and red meat, aligning with established recommendations for cardiovascular health [33, 34].
Despite these favourable behavioural changes, the study did not observe significant improvements in assessed biological characteristics. This suggests that while the intervention positively impacted behaviour, it did not produce notable physiological changes within the study’s timeframe. Similar observations in other studies emphasize the complexity of modifying biological markers through behavioural interventions alone [35, 36]. Meta-analysis findings also indicate that lifestyle modifications may require over twelve months to effectively reduce blood pressure, particularly among Asian populations [37]. Our study had a shorter post-intervention follow-up of six months, potentially insufficient to produce significant blood pressure changes compared to baseline. In contrast, a prior intervention study by Awosan et al. [12] in Nigeria reported significant reductions in blood pressure, fasting blood sugar (FBS), and total blood cholesterol at three months post-intervention. The differences could stem from Awosan et al.‘s [12] additional incorporation of exercise and dietary control in their intervention compared to our solely communication-focused approach. Moreover, the frequency of health communication sessions differed, with Awosan et al. [12] conducting fortnightly sessions for three months, while our study featured monthly sessions over the same duration.
Interestingly, the intervention group had a higher 10-year cardiovascular risk than the control group at baseline, which became non-significant post-intervention. Although the decrease in cardiovascular risk within the intervention group was not statistically significant, it indicated a positive trend. This aligns with previous studies demonstrating reductions in cardiovascular risk through lifestyle modifications, albeit potentially requiring longer-term follow-up to detect significant changes [12, 38]. Additionally, significant baseline differences between the intervention and control groups in total cholesterol, triglycerides, fasting blood sugar (FBS), waist circumference (WC), and body mass index (BMI) were observed. Most of these differences persisted at the end of the study, possibly explaining the absence of significant cardiovascular risk differences at the endline assessments across groups.
In future research, it is recommended to conduct randomized controlled trials (RCTs) instead of quasi-experimental designs to minimize bias and confounding variables, thus providing stronger evidence for the effectiveness of interventions. Furthermore, expanding the geographical scope of the study to include diverse populations with different socioeconomic backgrounds is crucial to enhance the generalizability of the findings. Moreover, longer intervention and follow-up periods should be implemented to assess the sustained effects of interventions and observe significant changes in biological characteristics. Additionally, it is suggested that future interventions should incorporate exercise schedules and dietary control alongside health communication to enhance their effectiveness in achieving desired outcomes. Lastly, the use of objective measurements, such as objective physical activity monitoring, dietary practices monitoring, and biomarkers, would greatly enhance the validity and reliability of the collected data. These recommendations will contribute to advancing knowledge in the field and improving the quality of cardiovascular health interventions.
The study had several limitations. Firstly, it adopted a quasi-experimental design instead of a randomized controlled trial, which introduces potential bias and confounding variables. This was due to limited resources caused by a lack of funding. Secondly, the study was conducted in a limited geographical area, specifically four schools located in Baruipur, a suburb on the outskirts of Kolkata, West Bengal, India. Therefore, caution should be exercised when generalizing the findings to other geographical locations or populations with different socioeconomic backgrounds. Thirdly, the intervention and follow-up period were relatively short, which might have restricted the ability to observe significant changes in certain biological characteristics, such as blood pressure. Fourthly, unlike some previous studies that incorporated exercise schedules and dietary control in addition to health communication, our intervention solely focused on health communication. The absence of dietary and exercise control elements may have influenced the effectiveness of the intervention in achieving specific outcomes. Lastly, some of the data collected, including physical activity levels and dietary habits, relied on self-reported information, which is susceptible to recall bias or social desirability bias. These potential biases could have impacted the accuracy of the results.
In summary, the intervention program yielded positive results in terms of behavioural characteristics, such as increased physical activity and healthier dietary habits, among school teachers. However, no significant improvements were noted in biological characteristics and cardiovascular risk factors. These findings underscore the necessity for further fine-tuning and tailoring of the intervention program to effectively target the physiological aspects associated with cardiovascular disease (CVD) risk. It is imperative that health professionals, educators, and policymakers collaborate to develop precise interventions that comprehensively address CVD risk factors and promote optimal cardiovascular health among school teachers.
Data Availability
The datasets utilized and analysed in the present study can be obtained from the corresponding author upon a reasonable request.
References
Global health estimates. : Leading causes of death. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death. Accessed 10 Jul 2023.
Cardiovascular diseases. https://www.who.int/health-topics/cardiovascular-diseases. Accessed 10 Jul 2023.
Cardiovascular diseases (CVDs). https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed 10 Jul 2023.
Mensah GA, Roth GA, Fuster V. The Global Burden of Cardiovascular Diseases and Risk factors: 2020 and Beyond. J Am Coll Cardiol. 2019;74:2529–32.
Cardiovascular diseases in India. World Heart Federation. https://world-heart-federation.org/resource/cardiovascular-diseases-in-india/. Accessed 10 Jul 2023.
Sreeniwas Kumar A, Sinha N. Cardiovascular Disease in India: a 360 degree overview. Med J Armed Forces India. 2020;76:1–3.
India Fact Sheet., National Family Health Survey – 5 (2019-21). 2022.
Global action plan for the prevention and control of. NCDs 2013–2020. https://www.who.int/publications/i/item/9789241506236. Accessed 10 Jul 2023.
Global atlas on cardiovascular disease prevention and control /. edited by: Shanthi Mendis …]. https://apps.who.int/iris/handle/10665/44701. Accessed 10 Jul 2023.
Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, Cardiovascular Disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. The Lancet. 2020;395:795–808.
Delfino LD, Tebar WR, Gil FC, De Souza JM, Romanzini M, Fernandes RA, et al. Association of sedentary behaviour patterns with dietary and lifestyle habits among public school teachers: a cross-sectional study. BMJ Open. 2020;10:e034322.
Awosan KJ, Ibrahim MTO, Makusidi MA, Essien E, Adeniji A. Impact of intervention on knowledge and risk factors of coronary Heart Disease among teachers in Sokoto, Nigeria. IJMMS. 2013;5:456–9.
Schools in Baruipur (South Twenty Four Pargan.) | Cluster wise List of Schools in Baruipur - South Twenty Four Pargan (West Bengal). https://schools.org.in/west-bengal/south--twenty-four-pargan/baruipur. Accessed 10 Jul 2023.
Singh ND. and M. Sample Size Calculator for Comparing Paired Differences. https://statulator.com/SampleSize/ss2PM.html. Accessed 11 Jul 2023.
Global recommendations on physical activity for health. https://www.who.int/publications-detail-redirect/9789241599979. Accessed 10 Jul 2023.
Dietary guidelines for Indians- A Manual. 2011. https://www.nin.res.in/downloads/DietaryGuidelinesforNINwebsite.pdf. Accessed 11 Jul 2023.
Oyeyemi AL, Oyeyemi AY, Adegoke BO, Oyetoke FO, Aliyu HN, Aliyu SU, et al. The Short International Physical Activity Questionnaire: cross-cultural adaptation, validation and reliability of the Hausa language version in Nigeria. BMC Med Res Methodol. 2011;11:156.
Guidelines for data processing and analysis of the International. Physical Activity Questionnaire (IPAQ): short and long forms. 2005.
WHO STEPS Surveillance. Part 3: Training and Practical Guides. Section 3: Guide to Physical Measurements (Step 2) Last Updated: 12 December 2008. 2008.
Noncommunicable Disease Surveillance., Monitoring and Reporting. World Health Organisation. https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps/manuals. Accessed 10 Jul 2023.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96.
Waist circumference and waist. -hip ratio: report of a WHO expert consultation. https://www.who.int/publications-detail-redirect/9789241501491. Accessed 10 Jul 2023.
Cardiovascular Disease. (10-year risk) | Framingham Heart Study. https://www.framinghamheartstudy.org/fhs-risk-functions/cardiovascular-disease-10-year-risk/. Accessed 10 Jul 2023.
D’Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General Cardiovascular Risk Profile for Use in Primary Care: the Framingham Heart Study. Circulation. 2008;117:743–53.
Ford ES. Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the U.S. Diabetes Care. 2005;28:2745–9.
jamovi - open. statistical software for the desktop and cloud. https://www.jamovi.org/. Accessed 10 Jul 2023.
Braksiek M, Pahmeier I, Gröben B, Lindemann U. Implementation of physical activity-based Health Promotion measures in schools—examples and evaluations from Germany. Sustainability. 2022;14:12327.
Polet J, Hassandra M, Lintunen T, Laukkanen A, Hankonen N, Hirvensalo M, et al. Using physical education to promote out-of school physical activity in lower secondary school students – a randomized controlled trial protocol. BMC Public Health. 2019;19:157.
Reis RS, Salvo D, Ogilvie D, Lambert EV, Goenka S, Brownson RC. Scaling up physical activity interventions worldwide: stepping up to larger and smarter approaches to get people moving. The Lancet. 2016;388:1337–48.
Pem D, Jeewon R. Fruit and Vegetable Intake: benefits and Progress of Nutrition Education interventions- Narrative Review article. Iran J Public Health. 2015;44:1309–21.
Kipping RR, Howe LD, Jago R, Campbell R, Wells S, Chittleborough CR, et al. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ. 2014;348(4):g3256–6.
LeFevre ML. Behavioral counseling to promote a Healthful Diet and Physical Activity for Cardiovascular Disease Prevention in adults with Cardiovascular Risk factors: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2014;161:587.
Lichtenstein AH, Appel LJ, Vadiveloo M, Hu FB, Kris-Etherton PM, Rebholz CM et al. 2021 Dietary Guidance to Improve Cardiovascular Health: A Scientific Statement From the American Heart Association. Circulation. 2021;144.
Abu Bakar NAF, Ahmad A, Wan Musa WZ, Shahril MR, Wan-Arfah N, Abdul Majid H, et al. Association between a dietary pattern high in saturated fatty acids, dietary energy density, and sodium with coronary Heart Disease. Sci Rep. 2022;12:13049.
Bassi N, Karagodin I, Wang S, Vassallo P, Priyanath A, Massaro E et al. Lifestyle Modification for Metabolic Syndrome: A Systematic Review. The American Journal of Medicine. 2014;127:1242.e1-1242.e10.
Sbruzzi G, Eibel B, Barbiero SM, Petkowicz RO, Ribeiro RA, Cesa CC, et al. Educational interventions in childhood obesity: a systematic review with meta-analysis of randomized clinical trials. Prev Med. 2013;56:254–64.
Li W, Liu H, Wang X, Liu J, Xiao H, Wang C, et al. Interventions for reducing blood pressure in prehypertension: a meta-analysis. Front Public Health. 2023;11:1139617.
Saffari M, Sanaeinasab H, Jafarzadeh H, Sepandi M, O’Garo K-GN, Koenig HG, et al. Educational intervention based on the Health Belief Model to modify risk factors of Cardiovascular Disease in police officers in Iran: a quasi-experimental study. J Prev Med Public Health. 2020;53:275–84.
Acknowledgements
The authors extend their sincere gratitude to the school heads and teachers at the participating schools for their invaluable cooperation throughout the study.
Funding
No financial support was received by the author(s) for the research, authorship, or publication of this article.
Author information
Authors and Affiliations
Contributions
A.K., A.B. and B.B. were responsible for conceptualizing, conducting, and writing the manuscript for the study. A.D. and L.B. provided valuable input in the study design and manuscript review. B.P. contributed to the statistical analysis and writing of the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research received approval from the Institutional Ethics Committee (IEC) at the All India Institute of Hygiene and Public Health (AIIH&PH), Kolkata. Each participant in the study provided informed written consent before their participation. Additionally, stringent measures were taken to uphold the confidentiality of the collected data during all stages of data collection, analysis, and reporting. The study was carried out in strict adherence to the principles outlined in the Declaration of Helsinki. The study did not involve any minors or individuals who were illiterate.
Consent for publication
Not applicable.
Competing interests
The authors affirm the absence of any conflicts of interest concerning this manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Karmakar, A., Bhattacharyya, A., Biswas, B. et al. Effect of educational intervention on risk factors of cardiovascular diseases among school teachers: a quasi-experimental study in a suburb of Kolkata, West Bengal, India. BMC Public Health 23, 2304 (2023). https://doi.org/10.1186/s12889-023-17227-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17227-w