Abstract
Background
COVID-19 pandemic emerged worldwide at the end of 2019, causing a severe global public health threat, and smoking is closely related to COVID-19. Previous studies have reported changes in smoking behavior and influencing factors during the COVID-19 period, but none of them explored the main influencing factor and high-risk populations for smoking behavior during this period.
Methods
We conducted a nationwide survey and obtained 21,916 valid data. Logistic regression was used to examine the relationships between each potential influencing factor (sociodemographic characteristics, perceived social support, depression, anxiety, and self-efficacy) and smoking outcomes. Then, variables related to smoking behavior were included based on the results of the multiple logistic regression, and the classification and regression tree (CART) method was used to determine the high-risk population for increased smoking behavior during COVID-19 and the most profound influencing factors on smoking increase. Finally, we used accuracy to evaluated the performance of the tree.
Results
The strongest predictor of smoking behavior during the COVID-19 period is acceptance degree of passive smoking. The subgroup with a high acceptation degree of passive smoking, have no smokers smoked around, and a length of smoking of ≥ 30 years is identified as the highest smoking risk (34%). The accuracy of classification and regression tree is 87%.
Conclusion
The main influencing factor is acceptance degree of passive smoking. More knowledge about the harm of secondhand smoke should be promoted. For high-risk population who smoke, the “mask protection” effect during the COVID-19 pandemic should be fully utilized to encourage smoking cessation.
Similar content being viewed by others
Background
At the end of 2019, COVID-19 spread globally. In March 2020, WHO declared it a pandemic [1], which has led to significant years of life loss [2].and excess mortality [3]. Smoking is a closely related factor to COVID-19. On the one hand, smoking has been shown to upregulate ACE2 expression, increasing susceptibility to COVID-19 [4]. On the other hand, COVID-19 severity is significantly higher in smokers compared to non-smokers [5]. Therefore, it is necessary to reduce smoking behavior to promote health during the COVID-19 outbreak.
Some previous studies have reported changes in smoking behavior during the COVID-19 pandemic and identified influencing factors. Some studies suggest that smoking behavior has decreased during the pandemic due to concerns about the perceived harm of smoking during COVID-19 [6], difficulties purchasing cigarettes due to pandemic-related lockdowns, and the inability to smoke in public places due to mask-wearing requirements [7]. However, other studies have indicated a significant increase in smoking behavior during COVID-19 due to anxiety, depression, stress, and other factors [8, 9]. The multitude of factors influencing smoking during COVID-19 necessitates identifying high-risk populations and targeting the most significant influencing factors to reduce smoking behavior. However, none of these studies have investigated the primary influencing factors and high-risk populations for smoking behavior during the COVID-19 pandemic.
Classification and Regression Tree Analysis (CART) is a decision tree method developed by Breiman and colleagues. Using CART, it is possible to identify the most significant influencing factors for relative risk and explore the interaction between influencing factors and the most critical influencing factors to form the branches of the classification and regression tree, dividing the population into high-risk subgroups [10]. It is a nonparametric program that begins tree development by examining all predictor variables and selecting the variable (parent node) that can best predict the desired classification. The data in this parent node is divided into two classifications (child nodes): one predicts the response variable classification, and the other does not. This binary recursive splitting process is repeated for each child node until further splitting is no longer possible [11]. Over the years, as CART has developed, it has been increasingly used in the medical field [12,13,14,15], and in the smoking field, it is mainly used to identify high-risk populations for the use of tobacco substitutes [16], the combination of risk factors for smoking and the strongest predictive indicators [17], as well as the prediction of smoking cessation outcomes [18].
The present study
Overall, smoking is a risk factor for COVID-19 infection and severity. Prior studies have analyzed the influencing factors of smoking behavior during the pandemic, but these studies only explored the relationship between influencing factors and changes in smoking behavior. This study aims to address the limitations of these studies. Specifically, CART analysis was used to explore the factors that most deeply influence smoking behavior in the population and to analyze the interactions between this factor and other influencing factors to identify high-risk populations for increased smoking behavior.
Method
Data and procedure
The data used in this study is conducted in 23 provinces, 5 autonomous regions, and 4 municipalities directly under the central government from June 20, 2022, to August 31, 2022. In this time, China was still experiencing the peak of the COVID-19 pandemic, with an increase of 442 − 77,402 cases per day [19]. During the investigation, China implemented a dynamic “Zero-COVID” policy, taking prompt actions to contain the outbreak of COVID-19 in the local area [20]. The specific measures include medically lockdown those who have had close contact with confirmed cases; large-scale nucleic acid testing; citywide home quarantine; the use of electronic health codes when entering public places; travel restrictions; and advocating for mask-wearing in public spaces. In certain situations, staff will remind individuals to wear masks or they will be prohibited from entering. During the policy implementation, China rigorously enforced the policy, and the policy was well implemented [21, 22].
The survey used Equal-probability sampling and non-equal-probability sampling. Equal-probability sampling (stratified sampling) at the provincial, municipal, district, township/subdistrict, and community/village levels (stratified sampling) and non-equal-probability sampling (quota sampling) at the community/village to individual level At least one surveyor or a panel of surveyors were recruited in each city. Investigators set up questionnaire points at health service centers or relevant health service stations in the sampling communities under their responsibility to conduct face-to-face surveys. And if they cannot conduct them due to the epidemic, the user uses the Online Questionnaire Star platform (https://www.wjx.cn/) to distribute the electronic questionnaire to each person to collect data. All participants obtained the participating respondent and record the questionnaire number issued to that person. Subjects were included in the study if they were ≥ 12 years old, provided written informed consent, and volunteered to participate in the study. A total of 23,414 questionnaires were collected, and after identifying and removing duplicate values, missing values and outliers with logical problems, a final sample of 21,916 was obtained, with a valid response rate of 93.6%.
Variables
Characteristic variable
The characteristic variable in this study included respondents’ basic information (age stage, gender, education, chronic and current work status), family characteristics (family income) and personal health status (chronic), COVID-19 related (COVID-19 impact of lockdown on livelihoods, lockdown), Negative events, Smoking status (length of smoking), exposure to secondhand smoke (acceptation degree of passive smoking, acquaintance smoking, smoker smoked around, and stay in smoking area). See Supplementary Table S1 for details of definitions and classifications.
Self-efficacy
Self-efficacy was measured using the New General Self-Efficacy Scale short form (NGSES-SF3) [23]. The scale consists of 3 items, with a total score ranging from 0 to 12 points. See Table S2 in the Supplementary Material for details. In this study, the Cronbach coefficient for the NGSES-SF3 was 0.925.
Depression
Depression was measured using the Patient Health Questionnaire-9 (PHQ-9) [24]. It is a nine-item self-report scale developed to assess symptoms of depression. The items were rated on a scale of 0–3 (not done = 0), and the total scale score ranges from 0 to 27. Symptom severity can be illustrated through the total score, where 0–4 points are without depression; 5–9 points for mild depression; 10–14 points for moderate depression; 15–19 points for more severe depression; 20–27 points for severe depression. See Table S3 in the Supplementary Material for details.
Anxiety
Anxiety was measured using the Generalized Anxiety Disorder Questionnaire (GAD-7) developed by Robert L Spitzer [25]. The scale consists of seven items with Table S4 good reliability, as well as the validity of criteria, constructs, factors, and procedures. The cut-off point for optimal sensitivity (89%) and specificity (82%) was identified. See in the Supplementary Material for details.
Perceived social support
Social support was measured using the Perceived Social Support Scale short form (PSSS-SF3) based on the Zimet Perceived Social Support Scale [21]. A 3-item scale is divided into three dimensions: family support, friend support, and other supports, as shown in Table S5 in the Supplementary Material. These three items were rated on a scale of 1–7 (Strongly disagree = 1), with higher scores indicating a greater perception of social support. In this study, the Cronbach coefficient for the PSSS-SF3 was 0.943.
Statistical analysis
First, we used EmpowerStats for descriptive analysis. Continuous variables were presented as mean ± standard deviation and categorical variables were reported as frequency N (%) and assessed using t-tests for continuous variables and chi-square tests for categorical variables. Next, we conducted univariate and multivariate logistic regression using Stata version 16.0 to examine the relationships between each potential predictor (demographic characteristics, perceived social support, depression, anxiety, and self-efficacy) and smoking outcome. Than, based on the results of the multivariate logistic regression, variables related to smoking behavior were included and a CART analysis was performed using R to identify high-risk populations for increased smoking behavior during COVID-19 and the factors that most deeply influenced the increase in smoking behavior.
Finally, we used R to evaluate the performance of CART. We calculated sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of the CART model. In this study, sensitivity refers to the probability of correctly predicting smokers as smokers. Specificity refers to the probability of not predicting non-smokers as smokers. Positive predictive value represents the proportion of true smokers among the sample units predicted as smokers. Negative predictive value represents the proportion of true non-smokers among the sample units predicted as non-smokers. Accuracy refers to the proportion of correctly categorized smokers and non-smokers out of the total.
Results
Sample characteristics
A total of 21,916 valid data were collected. Table 1 showed the demographic, self-efficacy, anxiety, and perceived social support characteristics of the smoking and non-smoking population (P < 0.01). Compared to non-smokers, smokers are more anxious, more depressed, less accepting of secondhand smoke, experience more negative events, have more acquaintances smoking in front of them, perceive less social support, and have lower self-efficacy (P < 0.001). Both groups were predominantly aged 18–59 years, without chronic disease and COVID-19 lockdown measures (P < 0.01) (Table 1).
Univariate logistic regression analysis and multivariate logistic regression analysis
Univariate regression analysis showed that the COVID-19 Impact of lockdown on Livelihoods was not associated with smoking behavior during COVID-19 (P = 0.246) (Table 2). Multivariate logistic regression analysis showed that having a chronic disease, higher perceived social support, lower self-efficacy, 31–40 years of smoking, absence of acquaintance smoking in front of them, staying in the smoking area, and lower acceptance of secondhand smoke were associated with the rise of smoking behavior during COVID-19 (P < 0.05) (Table 3).
Classification and regression tree (CART) analysis
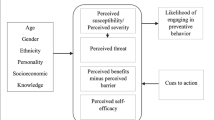
The CART analysis (Fig. 1) used a sample of smoking individuals and identified attitudes toward secondhand smoke as the strongest predictor. The 100% in the parent node of Fig. 1 represents the entire smoking population in this study, while the 0.15 represents the 15% of the overall population included in the study. The first branch divided the smoking population into those with an acceptation degree of passive smoking ≥ 12 (76%) and those with a degree < 12 (24%). The branch for those with a degree ≥ 12 and with no smoker smoked around (72%) led to a subgroup with a length of smoking of 30 years or more, accounting for 28% of the total smoking population. The branch for those with a score < 12 were non-chronic disease patients.
The branch for those with an acceptation degree of passive smoking of ≥ 12 indicates that no smokers smoked around. Among those with an acceptation degree of passive smoking of ≥ 12, have no smokers smoked around, and a length of smoking of ≥ 30 years, a subgroup leads to a terminal node, accounting for 28% of the total smoking population. This branching process is repeated until the sample is classified into 15 risk profiles (bottom row of Fig. 1). Currently, the subgroup with a high acceptation degree of passive smoking, have no smokers smoked around, and a length of smoking of ≥ 30 years is identified as the highest smoking risk (34%).
Performance evaluation of classification and regression tree (CART)
In this study, the CART model demonstrated high specificity (99%), high positive predictive value (71%), high negative predictive value (88%), and a high accuracy rate (87%). But sensitivity (20%) is low, it may be due to category imbalance that large sample size gap between smokers and non-smokers in this study (Table 4).
Discussion
Smoking is a closely related factor to COVID-19, and controlling smoking behavior is of great significance for the prevention and treatment of COVID-19. Identifying high-risk subgroups for smoking during the pandemic can enable targeted prevention and effective reduction in smoking behavior. Therefore, this study used CART analysis to identify high-risk subgroups for smoking behavior during COVID-19 and determine the factors that have the deepest influence.
Lockdown is an important factor influencing smoking behavior during COVID-19. It refers to the measures taken by various countries to prevent the spread of COVID-19, such as home quarantine, closure of entertainment venues, and isolation and quarantine measures [26]. Due to the differences in social background and lockdown measures, the impact of lockdown on smoking behavior may also vary [26]. In this study, lockdown mainly refers to three measures: home quarantine, activities within the community, and activities within the city. Previous studies have shown that during lockdown, stress and depression increase, and people tend to smoke more frequently, while the number of people attempting to quit smoking decreases [27]. However, the results of this study suggest that lockdown is associated with a decrease in smoking behavior. This may be due to the inability to purchase cigarettes during the home quarantine period [7] and an increase in motivation to quit smoking due to an increased perception of the harm of COVID-19 [28].
According to the CART model, currently, the subgroup with a high acceptation degree of passive smoking, have no smoker smoked around them, and a length of smoked of 30 years or more has the highest smoking rate during the COVID-19 pandemic. The acceptation degree of passive smoking is the main determinant of smoking behavior during the pandemic. This may be because people are more attentive to personal health protection during the COVID-19 pandemic and are more sensitive to the perceived harmfulness of tobacco [29], which may lead to a lower acceptance of secondhand smoke [30], resulting in a reduction in smoking behavior.
According to the CART model, during the COVID-19 pandemic, people are more likely to smoke when they are in the presence of have no smoker smoked around, which is contrary to previous research results. Previous studies have shown that individuals are more likely to start smoking when family and friends around them smoke [31, 32]. This may be due to an increase in personal protection awareness during the COVID-19 pandemic. As COVID-19 primarily affects the respiratory system, wearing a mask is an important preventive measure against COVID-19 [33]. During the period of this study, China was still experiencing the peak of the COVID-19 pandemic [19]. Despite the presence of individual variations, due to the Chinese government’s advocacy for mask usage and the concurrent increase in public health awareness among the population, there is a high level of acceptance and compliance with mask-wearing during the COVID-19 pandemic [34]. Even in 2023, when the COVID-19 pandemic has largely subsided, residents continue to exhibit good mask-wearing habits [35]. When people remove their masks to smoke, others may become more attentive to wearing masks due to fear of contracting COVID-19. Thus, when people are not smoking around them, individuals may be more likely to smoke. This conclusion needs to be verified in other countries. This result is opposite to our Logistic regression results, which may be due to CART examining the interaction between variables, which is why CART is widely used in exploring risk factors [36, 37]. Additionally, due to nicotine dependence, those with a longer smoking history have stronger nicotine dependence and more severe withdrawal symptoms, making it harder for them to reduce smoking behavior [38]. Therefore, our study shows that individuals with a length of smoking of 30 years or more are more likely to smoke during the COVID-19 pandemic. The group with a length of smoking of 40 years or more is not significant in the multiple regression results but is included in the CART model. There are two possible reasons for this. On the one hand, CART has greater resistance to multicollinearity compared to other parametric methods [36, 37]. On the other hand, CART is a decision tree model that only considers which variables can better predict the increase in smoking behavior during the COVID-19 pandemic and form the best classification, without considering variable significance issues.
Having a chronic illness is also a significant predictor, as non-chronically ill individuals are more likely to smoke. Smoking is strongly associated with chronic diseases [39], and China’s disease spectrum has shifted towards chronic, non-communicable diseases [40]. Additionally, chronic illness patients have a higher severe disease rate after contracting COVID-19 [41, 42]. To reduce the harm of chronic diseases, doctors are more likely to advise chronic illness patients to quit smoking, and patients are also more likely to accept smoking cessation advice from doctors [43, 44].
Regarding these issues, first, more attention should be paid to long-term smokers, and more specialized smoking cessation help should be provided to them. For example, the smoking cessation clinic actively promoted in China is an effective method [45]. Secondly, for individuals who are more exposed to secondhand smoke, tobacco education should be strengthened to enhance awareness of the hazards of secondhand smoke. Moreover, due to the requirement to wear masks in public areas during the COVID-19 period, smoking behavior has also been reduced. Therefore, during the COVID-19 pandemic, the “mask protection” effect can be fully utilized to guide smoking cessation behavior. Even if individuals around them are not smoking, environmental smoke may still carry and spread the virus, so it is necessary to wear masks and avoid smoking. Finally, doctors and non-chronically ill patients should also raise awareness of smoking cessation. Tobacco causes great harm to human health, and doctors’ smoking cessation advice is feasible in promoting patient smoking cessation [46], making doctors an important candidate in promoting smoking cessation, and doctors should also actively provide smoking cessation help to non-chronically ill patients.
Finally, this study explored the high-risk groups for smoking, and future studies should also delve deeper into the triggers for smoking cessation to provide a guiding direction for tobacco control policies and to form a continuity study to enrich policy guidelines.
Strength and limitation
Our study conducted a national survey using quota sampling, which can balance differences between regions and reflect the situation nationwide. Secondly, we focused on smoking behavior during the COVID-19 period and comprehensively analyzed the factors that influence smoking behavior in the context of epidemic prevention and control. Finally, our study results further revealed the mutual interactions between the most important risk factors and other influencing factors, thus identifying the high-risk group for smoking during the COVID-19 period.
However, this study also has some limitations. First, the study is a cross-sectional survey and does not establish causal relationships. Second, there may be other risk factors that affect smoking behavior during the COVID-19 period that were not included in this study. Finally, the sensitivity of CART in this study was relatively low, probably because of the small number of smokers in this study, which was large sample size gap between smokers and non-smokers. But even so, the accuracy of CART was high.
Conclusion
In general, this study was based on a national sample and used CART analysis to explore the high-risk population for increased smoking behavior during the COVID-19 period. The results showed that people with a high acceptation degree of passive smoking, have no smokers smoked around, and a length of smoking of ≥ 30 years were the subgroups with the highest smoking behavior during the COVID-19 period. Acceptation degree of passive smoking was the strongest predictor of smoking behavior during the COVID-19 period. It is important to pay more attention to long-term smokers and non-chronic disease patients, raise awareness of the hazards of smoking and secondhand smoke, and take advantage of the “mask effect” during the epidemic period to reduce smoking behavior during the COVID-19 pandemic.
Data Availability
All data generated or analyzed during this study are with the corresponding author. She is available to take any questions about the datasets. Persons who have made outstanding contributions or assisted in this study may apply for the use of the data only after submitting the study hypothesis and signing a data confidentiality agreement. There is no fee for the data opening plan. Publication of the study results will include processed data only, and personal information will remain anonymous.
References
Listings of WHO’s response to COVID-19. [https://www.who.int/news/item/29-06-2020-covidtimeline].
Pifarré IAH, Acosta E, López-Casasnovas G, Lo A, Nicodemo C, Riffe T, Myrskylä M. Years of life lost to COVID-19 in 81 countries. Sci Rep. 2021;11(1):3504.
14.9 million excess deaths associated with the COVID-19 pandemic in 2020. and 2021 [https://www.who.int/news/item/05-05-2022-14.9-million-excess-deaths-were-associated-with-the-covid-19-pandemic-in-2020-and-2021].
Sifat AE, Nozohouri S, Villalba H, Vaidya B, Abbruscato TJ. The role of Smoking and nicotine in the transmission and Pathogenesis of COVID-19. J Pharmacol Exp Ther. 2020;375(3):498–509.
Mahabee-Gittens EM, Mendy A, Merianos AL. Assessment of severe COVID-19 outcomes using measures of Smoking Status and Smoking Intensity. Int J Environ Res Public Health 2021, 18(17).
Nyman AL, Spears CA, Churchill V, Do VV, Henderson KC, Massey ZB, Reynolds RM, Huang J. Associations between COVID-19 risk perceptions and Smoking and quitting behavior among U.S. adults. Addict Behav Rep. 2021;14:100394.
Joyce AA, Styklunas GM, Rigotti NA, Neil JM, Park ER, Kruse GR. Quit experiences among primary care patients enrolled in a Smoking Cessation Pilot RCT early in the COVID-19 pandemic. Int J Environ Res Public Health 2021, 18(3).
Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, Fenning AS, Vandelanotte C. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, Tobacco and Alcohol Use in Australian adults. Int J Environ Res Public Health 2020, 17(11).
Carreras G, Lugo A, Stival C, Amerio A, Odone A, Pacifici R, Gallus S, Gorini G. Impact of COVID-19 lockdown on smoking consumption in a large representative sample of Italian adults. Tob Control. 2022;31(5):615–22.
Kim TW, Koh DH, Park CY. Decision tree of occupational Lung cancer using classification and regression analysis. Saf Health Work. 2010;1(2):140–8.
Lemon SC, Roy J, Clark MA, Friedmann PD, Rakowski W. Classification and regression tree analysis in public health: methodological review and comparison with logistic regression. Ann Behav Med. 2003;26(3):172–81.
Chester R, Khondoker M, Shepstone L, Lewis JS, Jerosch-Herold C. Self-efficacy and risk of persistent shoulder pain: results of a classification and regression tree (CART) analysis. Br J Sports Med. 2019;53(13):825–34.
Johns H, Bernhardt J, Churilov L. Distance-based classification and regression trees for the analysis of complex predictors in health and medical research. Stat Methods Med Res. 2021;30(9):2085–104.
Zheng H, Fei J, Zhang L, Zhou W, Ding Z, Hu W. Risk factor analysis of insufficient fluid intake among urban adults in Wuxi, China: a classification and regression tree analysis. BMC Public Health. 2020;20(1):286.
Alqahtani HM, Koroukian SM, Stange K, Bissada NF, Schiltz NK. Combinations of chronic conditions, functional limitations and geriatric syndromes associated with periodontal Disease. Fam Med Community Health 2022, 10(3).
Lei Y, Nollen N, Ahluwahlia JS, Yu Q, Mayo MS. An application in identifying high-risk populations in alternative Tobacco product use utilizing logistic regression and CART: a heuristic comparison. BMC Public Health. 2015;15:341.
Higgins ST, Kurti AN, Redner R, White TJ, Keith DR, Gaalema DE, Sprague BL, Stanton CA, Roberts ME, Doogan NJ, et al. Co-occurring risk factors for current cigarette Smoking in a U.S. nationally representative sample. Prev Med. 2016;92:110–7.
Lai CC, Huang WH, Chang BC, Hwang LC. Development of Machine Learning models for Prediction of Smoking Cessation Outcome. Int J Environ Res Public Health 2021, 18(5).
Timeline of number. of COVID-19 daily cases in China [https://coronavirus.jhu.edu/region/china].
Cheshmehzangi A, Zou T, Su Z. Commentary: China’s Zero-COVID Approach depends on Shanghai’s Outbreak Control. Front Public Health. 2022;10:912992.
Tan C, Luo X, Zhou Z, Zeng X, Wan X, Yi L, Liu Q. Dynamic zero-COVID strategy in controlling COVID-19 in Shanghai, China: a cost-effectiveness analysis. J Infect Public Health. 2023;16(6):893–900.
Feng Y, Shao H, Gong X, Song Z, Xie Y, Qi S, Shi L, Hu Y, Liu X, Liu X, et al. Dynamic zero-COVID’ policy and viral clearance during an omicron wave in Tianjin, China: a city-wide retrospective observational study. BMJ Open. 2022;12(12):e066359.
Chen G, Gully SM, Eden D. Validation of a New General Self-Efficacy Scale. Organizational Res Methods. 2001;4(1):62–83.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Freiberg A, Schubert M, Romero Starke K, Hegewald J, Seidler A. A Rapid Review on the influence of COVID-19 Lockdown and Quarantine measures on Modifiable Cardiovascular Risk factors in the General Population. Int J Environ Res Public Health 2021, 18(16).
Kosendiak A, Król M, Ściskalska M, Kepinska M. The changes in stress coping, Alcohol Use, cigarette Smoking and physical activity during COVID-19 related lockdown in medical students in Poland. Int J Environ Res Public Health 2021, 19(1).
Klemperer EM, West JC, Peasley-Miklus C, Villanti AC. Change in Tobacco and electronic cigarette Use and Motivation to quit in response to COVID-19. Nicotine Tob Res. 2020;22(9):1662–3.
Hu Z, Lin X, Chiwanda Kaminga A, Xu H. Impact of the COVID-19 epidemic on Lifestyle behaviors and their Association with Subjective Well-being among the General Population in Mainland China: cross-sectional study. J Med Internet Res. 2020;22(8):e21176.
Hwang J, Chun HR, Cheon E. A qualitative study on the impact of COVID-19 on the behavior and attitudes of smokers and non-smokers in South Korea. BMC Public Health. 2021;21(1):1972.
Alves RF, Precioso J, Becoña E. Smoking behavior and secondhand smoke exposure among university students in northern Portugal: relations with knowledge on Tobacco use and attitudes toward Smoking. Pulmonology. 2022;28(3):193–202.
Okoli CT, Kodet J. A systematic review of secondhand Tobacco smoke exposure and Smoking behaviors: Smoking status, susceptibility, initiation, dependence, and cessation. Addict Behav. 2015;47:22–32.
Tabatabaeizadeh SA. Airborne transmission of COVID-19 and the role of face mask to prevent it: a systematic review and meta-analysis. Eur J Med Res. 2021;26(1):1.
Tan M, Wang Y, Luo L, Hu J. How the public used face masks in China during the coronavirus Disease pandemic: a survey study. Int J Nurs Stud. 2021;115:103853.
Yang Q, Yang S, Jiao Y. Assessing disposable masks consumption and littering in the post COVID-19 pandemic in China. Environ Pollut. 2023;334:122190.
Merkle EC, Shaffer VA. Binary recursive partitioning: background, methods, and application to psychology. Br J Math Stat Psychol. 2011;64(Pt 1):161–81.
Romeo M, Yepes-Baldó M, Soria M, Jayme M. Impact of the COVID-19 pandemic on higher education: characterizing the Psychosocial Context of the positive and negative Affective States using classification and regression trees. Front Psychol. 2021;12:714397.
Bahelah R, DiFranza JR, Ward KD, Eissenberg T, Fouad FM, Taleb ZB, Jaber R, Maziak W. Waterpipe smoking patterns and symptoms of nicotine dependence: the Waterpipe dependence in Lebanese Youth Study. Addict Behav. 2017;74:127–33.
Ng R, Sutradhar R, Yao Z, Wodchis WP, Rosella LC. Smoking, drinking, diet and physical activity-modifiable lifestyle risk factors and their associations with age to first chronic Disease. Int J Epidemiol. 2020;49(1):113–30.
Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, Li X, Wang L, Wang L, Liu Y, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2019;394(10204):1145–58.
Malini H, Lenggogeni DP, Windah A, Qifti F, Thapa DK, West S, Cleary M. #Stressed: Covid-19, chronic Illness and Technostress. Issues Ment Health Nurs. 2022;43(2):189–92.
Higgins V, Sohaei D, Diamandis EP, Prassas I. COVID-19: from an acute to chronic Disease? Potential long-term health consequences. Crit Rev Clin Lab Sci. 2021;58(5):297–310.
Keith DR, Stanton CA, Gaalema DE, Bunn JY, Doogan NJ, Redner R, Kurti AN, Cepeda-Benito A, Lopez AA, Morehead AL, et al. Disparities in US Healthcare Provider Screening and advice for Cessation Across Chronic Medical conditions and Tobacco products. J Gen Intern Med. 2017;32(9):974–80.
Hu Y, Chen Q, Zhang B. Can Chronic Disease diagnosis urge the patients to quit Smoking? - evidence from the China Health and Nutrition Survey. Risk Manag Healthc Policy. 2021;14:3059–77.
Wu L, He Y, Jiang B, Zuo F, Liu Q, Zhang L, Zhou C, Liu M, Chen H, Cheng KK et al. Effectiveness of additional follow-up telephone counseling in a Smoking cessation clinic in Beijing and predictors of quitting among Chinese male smokers. (1471–2458 (Electronic)).
Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2013;2013(5):Cd000165.
Acknowledgements
None
Funding
This work was supported by the National Natural Science Foundation of China (Grant#72204107), Guangzhou Science and Technology Program (Grant#2024A04J02668), the Guangdong Medical Scientific Research Foundation (Grant#A2023125), Science and Technology Program of Guangzhou (Grant#2023A04J2267).
Author information
Authors and Affiliations
Contributions
Conceptualization, CJY, CJH and WYB.; methodology, LSY, ZHZ, YXH., and YJ; validation, LSY, and ZHZ; investigation, WYB; data curation, LSY, ZHZ, LML and YXH; writing—original draft preparation, YJ, CZY; writing—review and editing, YJ, CJY, CJH; supervision, WYB. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Classification and Regression Tree (CART).
New General Self-Efficacy Scale short form-3 (NGSES-SF3).
Patient Health Questionnaire-9 (PHQ-9).
Generalized Anxiety Disorder Questionnaire (GAD).
Perceived Social Support Scale short form (PSSS-SF3).
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki. All experimental protocols were approved by Shaanxi institute of international trade and commerce (No. JKWH-2022-02) and second xiangya hospital of central south university (No.2022-K050). The cover page of the questionnaire will explain the study’s purpose and assure anonymity, confidentiality, and the right to refuse to participate in the study. Informed consent was obtained from all participants involved in the study.
Consent for publication
Not applicable.
Consent to participate
I Informed consent to participate in this study was obtained from the participant (or the parent or legal guardian of a child under 16 years of age).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, J., Yang, J., Liu, S. et al. Risk profiles for smoke behavior in COVID-19: a classification and regression tree analysis approach. BMC Public Health 23, 2302 (2023). https://doi.org/10.1186/s12889-023-17224-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17224-z