Abstract
Background
Racial inequities in life expectancy, driven by structural racism, have been documented at the state and county levels; however, less information is available at the city level where local policy change generally happens. Furthermore, an assessment of life expectancy during the decade preceding COVID-19 provides a point of comparison for life expectancy estimates and trends post COVID-19 as cities recover.
Methods
Using National Vital Statistics System mortality data and American Community Survey population estimates, we calculated the average annual city-level life expectancies for the non-Hispanic Black (Black), non-Hispanic White (White), and total populations. We then calculated the absolute difference between the Black and White life expectancies for each of the 30 cities and the U.S. We analyzed trends over four time periods (2008-2010, 2011-2013, 2014-2016, and 2017-2019).
Results
In 2017-2019, life expectancies ranged from 72.75 years in Detroit to 83.15 years in San Francisco (compared to 78.29 years for the U.S.). Black life expectancy ranged from 69.94 years in Houston to 79.04 years in New York, while White life expectancy ranged from 75.18 years in Jacksonville to 86.42 years in Washington, DC. Between 2008-2010 and 2017-2019, 17 of the biggest cities experienced a statistically significant improvement in life expectancy, while 9 cities experienced a significant decrease. Black life expectancy increased significantly in 14 cities and the U.S. but decreased significantly in 4 cities. White life expectancy increased significantly in 17 cities and the U.S. but decreased in 8 cities. In 2017-2019, the U.S. and all but one of the big cities had a significantly longer life expectancy for the White population compared to the Black population. There was more than a 13-year difference between Black and White life expectancies in Washington, DC (compared to 4.18 years at the national level). From 2008-2010 to 2017-2019, the racial gap decreased significantly for the U.S. and eight cities, while it increased in seven cities.
Conclusion
Urban stakeholders and equity advocates need data on mortality inequities that are aligned with city jurisdictions to help guide the allocation of resources and implementation of interventions.
Similar content being viewed by others
Introduction
Life expectancy at birth, perhaps the best single indicator of overall health in a population, summarizes mortality from all diseases and injuries, and across all ages [1, 2]. Racial inequities in this important health metric have consistently been observed at the national level since at least 1850, when a White person could expect to live to age 40, on average, while a Black person could only expect to live to age 23 [3]. Although this gap varied throughout the 1900’s, it generally narrowed through the end of the century and early 2000’s [2, 4]. In the first two decades of the twenty-first century, the Black-White difference in life expectancy shrank by more than two years (from 5.9 to 3.6 years) [5]. However, the racial gap increased by almost two years (to 5.50 years in 2021) due to the COVID-19 pandemic, reflecting continued systemic racism that disproportionately affects communities and individuals of color [6,7,8,9].
Racial inequities in life expectancy have also been documented at the state and county levels; [10, 11] however, less information is available at sub-county levels, including cities. Public health officials and researchers increasingly seek local data to inform place-based initiatives [12,13,14]. This is especially important because data for bigger geographic areas (e.g. county) hides local variation, making it difficult to detect inequities [15]. Even city-level data hides variation across neighborhoods; [16] however, local policy change generally happens at the city (not neighborhood or census tract) level, making it an optimal level for analysis. Moreover, four in five people in the U.S. currently live in urban areas and this number continues to grow [17].
In the past several years, there has been increasing access to city-level health data via open access data platforms [18, 19]. However, life expectancy estimates at the city level are either based upon small area estimates and do not include race-specific estimates, [18] or the race-specific sources do not estimate non-Hispanic Black life expectancy [19]. In addition, they include very limited (or no) historical data and lack an an evaluation of trends. It is critical to add to this work by specifically examining inequities between non-Hispanic Black (NHB) and non-Hispanic White (NHW) populations and assessing how these inequities have changed during the past decade leading up to the COVID-19 pandemic (prior to dramatic shifts in life expectancy). The explicit measurement of racial inequities and city-level comparisons of such inequities provide a more in-depth assessment of our current urban equity landscape [20] In addition, trend analyses can help identify cities that have been making significant progress in improving population health and/or ameliorating inequities [21, 22]. These cities can serve as potential models to others that are striving to be more equitable. Furthermore, an assessment of life expectancy during the decade preceding COVID-19 provides a point of comparison for life expectancy estimates and trends post COVID-19 as cities recover.
This analysis provides data on total and race-specific life expectancy, and inequities found within, for the 30 most populous U.S. cities. We assess trends in inequities across four time periods between 2008 and 2019. These new data provide critical information for urban health leaders and equity advocates to help identify areas and groups of greatest need, motivate partners, and begin exploring ways to address equity challenges through population-level structural interventions [22,23,24].
Methods
This study followed the Strengthening the Reporting of Observational Studies in Epidemiology reporting guideline for observational studies.
Study population
The 30 most populous cities were identified according to the 2019 U.S. Census Bureau data. Our analysis included three cases in which city and county governments representing slightly different geographies have merged to form a consolidated city with one governing body (i.e. Louisville and Jefferson County, KY; Nashville and Davidson County, TN; and Indianapolis and Marion County, IN). In those three cases, mortality data was only available at the county level. Therefore, the results presented for these cases represent county life expectancies. Due to uncertainty about the geographic area included in Las Vegas death records, we excluded Las Vegas from the analysis and included Milwaukee, WI, the 31st largest city, in its place. Collectively, these cities make up 12.1% of the US population. Select demographic data for each city are listed in Supplemental Table 1.
Data sources
Mortality data
Mortality data comes from the Multiple Cause of Death data files from the National Vital Statistics System [25] For the years 2008–2010 (T1), 2011–2013 (T2), 2014–2016 (T3), and 2017–2019 (T4), we extracted race- and ethnicity-specific deaths by age group (0–4, 5–9, 10–14, 15–19, 20–24, 25–29, 30–34, 35–44, 45–54, 55–64, 65–74, 75–84, and 85 years and above) and the recorded city of residence. City of residence (as opposed to city of occurrence) was used to classify the geography for deaths to ensure our numerators and denominators reflected the same population.
Population data
For the U.S. overall and each individual city, total race- and age-specific population-based denominators were obtained from the U.S. Census Bureau. Denominator data for the total and non-Hispanic White populations came from the American Community Survey (ACS) 5-year estimates from the midpoint year of each of the time periods included in the study [26]. This is consistent with previous work and methodology used by others in this field [27,28,29]. One exception was made for Detroit, where ACS estimates for 2009 were inconsistent with estimates for other years. Therefore, for T1 we used the average of the 3-year ACS estimate for 2008 and 5-year ACS estimate for 2010 for the city of Detroit. The process for obtaining non-Hispanic Black denominator data was different as the only source of population data for the non-Hispanic Black population is the Decennial Census. The non-Hispanic Black population was estimated for the U.S. overall and each individual city using the formula:
Where n is age group, NHB Pop is Non-Hispanic Black Population, Black Pop is Total (Hispanic + non-Hispanic) Black Population, US Census refers to the 2010 Decennial and ACS refers to the American Community Survey 5-year estimates for the midpoint year of each study period.
The total overall U.S. and individual city outcomes include all race/ethnic groups (not just Black and White). To calculate life expectancy, we used all 13 age groups available in the ACS.
Statistical analyses
Life expectancy
Life expectancy measures the average number of years from birth a person can expect to live according to the current mortality experience (age-specific death rates) of the population. Life expectancy was calculated for the total population, the NHB (Black) population, and the NHW (White) population. The life expectancy for each city and the U.S. overall were calculated using a modified version of the life expectancy calculation developed by Chiang [30]. Chiang’s original life expectancy formula was calculated using 18 distinct age groups, whereas our life expectancy formula was restricted to the 13 age groups available in the ACS. To assess the accuracy of this method, a test was conducted wherein life expectancy was calculated for the same populations using 13 and 18 age groups, with data from the 2010 U.S. Census. Both methods produced similar results, therefore, the ACS data was used so to have population denominators that reflected the same time periods as the deaths included in this analysis.
Z scores were calculated to assess the significance of changes in life expectancy over time for the total populations, as well as Black and White populations. To assess inequities in life expectancy, we calculated the absolute difference in Black and White life expectancy and its 95% confidence interval for each of the 30 cities and the U.S. overall in each time period. To identify a statistically significant increase or decrease in life expectancy inequities, the t-test was applied.
This study was reviewed by the Mount Sinai Hospital (Chicago, IL) institutional review board (IRB) and deemed to be exempt, in accordance with 45 CFR §46. Mount Sinai Hospital IRB waived written informed consent due to the retrospective and deidentified nature of the data.
Results
A total of 31,686,825 death records were assessed for eligibility, from which 62,671 records of non-U.S. residents and 1,799 records where age was missing were excluded. There were 31,622,355 death records from 2008–2019 included in the analysis.
Overall life expectancy
The life expectancy for a baby born in the U.S. between 2017–2019 (T4) was 78.29 years, as seen in Table 1. Life expectancy at the city level ranged from a low of 72.75 years in Detroit to a high of 83.15 years in San Francisco. Of the 30 cities, 13 had life expectancies higher than the U.S., while 17 had lower life expectancies.
The U.S. experienced a small but significant decrease in life expectancy (from 0.43 years; p < 0.05) between T1 and T4 (see Supplemental Table 2 for all time points). Also, nine cities experienced a statistically significant decrease in life expectancy, ranging from a loss of 0.48 years in Nashville to 1.47 years in Louisville. Conversely, 17 experienced a statistically significant improvement in life expectancy. This increase ranged from 0.25 years (San Diego) to 2.22 years (Washington DC). Life expectancy in the remaining four cities did not change.
Race-specific life expectancy
During the most recent time period (T4), the Black life expectancy for the U.S. was 74.25 years (Table 2). Across the cities, life expectancy for Black individuals ranged from 69.94 years in Houston to 79.04 years in New York. The White life expectancy for the U.S. was 78.44 years. The range across cities (11.24 years) was slightly larger in magnitude to that seen for Black life expectancy (9.10), going from 75.18 years (Jacksonville) to 86.42 years (Washington, DC).
Black life expectancy increased significantly from T1 to T4 in the U.S. (from 73.54 to 74.25 years) and in 14 of the 30 largest cities (see Supplemental Table 2 for all time points). This increase in Black life expectancy ranged from 0.57 years (Dallas) to 3.20 years (Boston). However, life expectancy for the Black population significantly decreased in four cities (Portland, Houston, Milwaukee, and Chicago). The lowest decrease occurred in Chicago (1.05 years) and the highest in Portland (3.38 years). There was no statistically significant change in Black life expectancy in the 12 remaining cities.
White life expectancy in the U.S. showed a small, but statistically significant, increase from 78.38 to 78.44 years between T1 and T4 (see Supplemental Table 2 for all time points). Among the big cities, it increased significantly in 17 cities (ranging from an increase of 0.51 years in San Diego to 4.42 years in Detroit) and decreased in 8 cities (ranging from a decrease of 0.48 years in Indianapolis to 1.51 years in Memphis). There was no statistically significant change in White life expectancy in the remaining five cities (Nashville, Dallas, Phoenix, Houston, and Columbus).
Racial inequities in life expectancy
At the national level, the absolute difference between the Black and White life expectancies was 4.18 years in T4. All but one city (El Paso) had a longer life expectancy for the White population compared to the Black, with most (n = 27) showing a difference of three or more years between the race-specific rates. In 22 of the 30 cities, the racial difference was wider than the one found at the national level. Most strikingly, there was more than a 13-year difference (13.26 years, 95% CI: 12.80, 13.72) between Black and White life expectancies in Washington, DC.
In the U.S., the inequity statistically significantly decreased by 0.67 years for the country from T1 to T4, with inequity declining more sharply between T1 and T2, and then remaining stable from T2 to T4. In Fig. 1, we plotted the change in Black:White life expectancy inequity over time for the cities in which there was a significant change from T1 to T4. There were significant increases in the Black:White difference in seven cities. Of note, Houston, Chicago, Detroit, and Portland all saw increases in the Black:White gap of more than two years between T1 and T4. The cities where inequities increased generally experienced increases over the four time periods, except for Fort Worth, where inequity increased sharply from T1 to T2 then remained flat for the remainder of the study period. In contrast, the inequity decreased significantly between T1 and T4 in ten cities, with decreases of more than two years in Boston, Philadelphia, and Memphis. Among these cities, the data showed a trend of sharp decreases between T1 and T2, followed by modest increases from T2 through T4. Jacksonville was an exception to this trend; it was the only city where inequities decreased at each point during the study period. The racial inequity remained stable in 13 cities.
Comparing cities by outcome and equity
In Fig. 2, we plotted the 30 cities based on both overall life expectancy (y-axis) and the racial gap in life expectancy at T4 (x-axis). The U.S. life expectancy and Black:White difference in life expectancy were used to separate outcomes into quadrants. The upper left quadrant represents the “best-performing cities” that had life expectancies above the U.S. life expectancy and Black:White differences below the national level of inequity. El Paso, Boston, and San Jose are the only cities in this category. The lower right quadrant represents the “worst-performing” cities that had life expectancies lower than the U.S. and levels of racial inequity greater than the U.S. gap. There are 11 cities that performed poorly in both outcomes. Chicago stands out for high inequity, while Detroit, Baltimore, and Memphis stand out for having poor overall life expectancy within this group.
The remaining cities performed well for either life expectancy or equity. Most notably, San Francisco was the top city for longest life expectancy but the second worst city for racial inequity. Conversely, Jacksonville was one of the top cities for racial equity in life expectancy but was well below the national life expectancy.
Discussion
Urban stakeholders and public health professionals have increasingly called for more granular data to identify local health issues, compare outcomes, and assess progress [13, 18, 31]. The present study provides detailed city-level data on racial inequities in life expectancy across four time points, confirming wide variation among the biggest U.S. cities. Across 29 of the biggest cities and all time points (El Paso being the exception), Black life expectancy was consistently shorter than White life expectancy. In the most recent time period (2017–2019), prior to the COVID-19 pandemic, 18 of the 29 cities had a Black-White gap in life expectancy of at least 5 years and the remainder had at least a 2-year gap. The size of the inequities, despite decades of programs and policies designed to eliminate them, is troubling. Even more worrisome is the trend of increasing inequities in seven cities, with another 15 cities showing a consistent racial gap over time. Overall, the data suggest that the U.S. needs a more tailored approach to achieve health equity in our urban areas.
The current data adds to existing sources of city-level data health information. For example, the City Health Dashboard provides life expectancy estimates for the 900 largest U.S. cities, but they do not currently include race-specific data, their numbers are estimated using weighted averages of small area estimations of life expectancy, and they only include a single six-year estimate [29]. A second notable source of data, the Big Cities Health Inventory, provides extensive health data for the 35 largest U.S. cities. However, the mortality data provided there for the Black population includes individuals with either Hispanic or non-Hispanic ethnicity [19]. Race and ethnicity are two separate social constructs and research shows that Black Hispanic and Black non-Hispanic populations have different health experiences [32,33,34]. Within the peer-reviewed literature, a relatively recent paper provided an extensive analysis of trends in (all-cause and cause-specific) mortality and life expectancy at the city level. However, the authors did not include explicit measures of racial inequities and used county-level data for race-specific life expectancy estimates [19].
City departments of public health guide large budgets, set the agenda for local health initiatives, and often lead innovative policy development [35, 36]. However, conducting this type of local-level analysis is time-intensive and requires methodological expertise, which may be beyond the capacity of local public health departments due to funding constraints [37,38,39]. Thus, cities are often compelled to make decisions based on data not specific to their actual population. Furthermore, a growing number of local health departments are specifically focused on increasing racial health equity in their jurisdiction, as indicated by the inclusion of racial health equity within strategic health plans, the establishment of equity-related positions or divisions, the provision of health equity data, and declarations of racism as a public health crisis [40, 41]. An evaluation of these strategic plans and activities must include a regular assessment of racial inequities in health outcome measures, as was done in this study. Cities that increase their focus (and presumably budget) on equity-related outcomes should carefully evaluate trends in their local data to ascertain if the additional resources translate into decreased racial gaps over time. If not, the data could be used to strengthen appeals for increased support, as well as to prompt a critical examination of the strategies used.
More broadly, this type of data offers the opportunity to comparatively assess local policies, programs, and resources that may be supportive of more equitable health outcomes. Our study identified cities that had below average racial inequities, as well as those making strides towards greater equity. In particular, both Jacksonville and Boston had a smaller Black:White gap than the country as a whole and a significant reduction in the size of the gap between T1 and T4. In a recent study covering the local health departments that serve the 30 biggest US cities, these same two cities were recognized for having both a focus on racial health inequities within their strategic plan and having specific goals related to racial health equity [42]. While many other factors, including structural racism (e.g., income inequality), influence population-level outcomes like inequities in life expectancy, the impact of these types of policy-related indicators warrants more investigation [27].
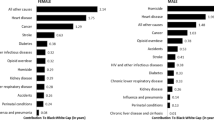
Moving forward, analyses like the current study may also spur analyses at an even more local level to pinpoint the neighborhoods or population subgroups that would benefit the most from targeted interventions or resource allocations [43, 44]. Another potentially useful approach is for cities to decompose life expectancy inequities to determine which causes of death contribute the most to the racial gaps, which could help individuals cities more effectively target potential solutions [45, 46]. For cities with health inequities, evidence-based or -informed interventions and policies that address social determinants of health and are intentionally directed at reducing health inequities are critical for closing the racial gap in health [47,48,49,50] There are several model city-level initiatives that offer insight into how local data and multi-sector approach may be used to tackle and assess initiatives aimed at addressing racial inequities in care and outcome [51,52,53]
This work has several limitations. To begin, the race and ethnicity data provided on death certificates may be inaccurate as it may come from interviews with the decedent’s family or on the reporter’s observations. However, research suggests race reporting for the categories used here (White and Black races and Hispanic ethnicity) is highly accurate [54, 55]. We also recognize the complexity of quantifying inequities and acknowledge that we only include one measure of inequities [56]. Additionally, we limited our analyses to inequities between the Black and White populations. We made this choice because, in the U.S., Black and White populations are frequently used in public health as representative of the extremes of privilege and marginalization [27]. Future work should examine inequities affecting other racial and ethnic groups, as data permit. Finally, the current analyses do not include an examination of ecological factors and, thus, cannot account for demographic or socioeconomic changes that may have occurred within the cities during the study period.
Conclusions
It is critical to measure racial inequities in life expectancy and assess how they are changing over time in order to gauge city-level progress in achieving health equity, a primary goal within the Healthy People initiative [57] and a specific focus of many health departments covering our largest urban areas [41]. Moreover, directly comparing (or even ranking) racial inequities across geographic areas can increase awareness and advocacy for equity; guide resource allocation; and highlight cities that might be implementing effective population health strategies [58,59,60,61,62,63]. The pandemic’s short-, mid-, and long-term impacts on life expectancy in urban cities remains to be seen. A re-assessment of life expectancy trends during and after the COVID-19 pandemic is warranted given that populations in urban centers were amongst the hardest hit [64]. Additionally, local-level variability and inequities in vaccination uptake are likely to forestall improvement and equity in life expectancy in some areas [65]. Structural racism and social conditions facilitate inequities in life expectancy (and many other health outcomes). This is reflected in the persistent racial gaps seen in almost all the cities included in the present analysis. The magnitude and multifaceted nature of these inequities demand broad and immediate economic, social, and political changes that allow everyone equal opportunities to leading healthy lives [6, 66, 67].
Availability of data and materials
The datasets analyzed during the current study are restricted-use vital statistics data obtained from the National Vital Statistics System (NCHS) via a data use agreement. Data are available from the authors upon reasonable request and with permission from NCHS.
References
Kochanek KD, Murphy SL, Xu JQ, Arias E. Deaths: Final data for 2017. National Vital Statistics Reports; vol 68 no 9. Hyattsville: National Center for Health Statistics; 2019.
Kochanek KD, Anderson RN, Arias E. Changes in life expectancy at birth, 2010–2018. National Center for Health Statistics Health E-Stats. 2020.
Haines MR. Ethnic Differences in Demographic Behavior in the United States Has There Been Convergence? Historical Methods: A Journal of Quantitative and Interdisciplinary History. 2003/01/01 2003;36(4):157–195. https://doi.org/10.1080/01615440309604818
Grove RD, Hetzel AM. Vital statistics rates in the United States, 1940–1960. Washington DC: US Government Printing Office; 1968.
Dwyer-Lindgren L, Kendrick P, Kelly YO, et al. Life expectancy by county, race, and ethnicity in the USA, 2000–19: a systematic analysis of health disparities. The Lancet. 2022;400(10345):25–38.
Andrasfay T, Goldman N. Reductions in US life expectancy during the COVID-19 pandemic by race and ethnicity: Is 2021 a repetition of 2020? PLoS One. 2022;17(8):e0272973. https://doi.org/10.1371/journal.pone.0272973.
Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet (London, England). 2017;389(10077):1453–63. https://doi.org/10.1016/s0140-6736(17)30569-x.
Braveman PA, Arkin E, Proctor D, Kauh T, Holm N. Systemic And Structural Racism: Definitions, Examples, Health Damages And Approaches To Dismantling. Health affairs (Project Hope). 2022;41(2):171–8. https://doi.org/10.1377/hlthaff.2021.01394.
Garcia MA, Homan PA, García C, Brown TH. The Color of COVID-19: Structural Racism and the Disproportionate Impact of the Pandemic on Older Black and Latinx Adults. J Gerontol B Psychol Sci Soc Sci. 2021;76(3):e75–80. https://doi.org/10.1093/geronb/gbaa114.
Bharmal N, Tseng CH, Kaplan R, Wong MD. State-level variations in racial disparities in life expectancy. Health Serv Res. 2012;47(1 Pt 2):544–55. https://doi.org/10.1111/j.1475-6773.2011.01345.x.
Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, et al. Inequalities in Life Expectancy Among US Counties, 1980 to 2014: Temporal Trends and Key Drivers. JAMA Intern Med. 2017;177(7):1003–11. https://doi.org/10.1001/jamainternmed.2017.0918.
Kumaresan J, Prasad A, Alwan A, Ishikawa N. Promoting health equity in cities through evidence-based action. J Urban Health. 2010;87(5):727–32. https://doi.org/10.1007/s11524-010-9500-2.
KB DeSalvo, Wang YC, Harris A, Auerbach J, Koo D, O’Carroll P. Public Health 3.0: A Call to Action for Public Health to Meet the Challenges of the 21st Century. Preventing Chronic Disease. 2017;14:78 https://doi.org/10.5888/pcd14.170017.
Nagasako E, Waterman B, Reidhead M, Lian M, Gehlert S. Measuring Subcounty Differences in Population Health Using Hospital and Census-Derived Data Sets: The Missouri ZIP Health Rankings Project. J Public Health Manag Pract. 2018;24(4):340–349. https://doi.org/10.1097/phh.0000000000000578
Spoer B, Feldman J, Gofine M, et al. Health and health determinant metrics for cities: A comparison of county versus city-level data. Prev Chronic Dis. 2020;17:200125.
Hunt BR, Tran G, Whitman S. Life Expectancy Varies in Local Communities in Chicago: Racial and Spatial Disparities and Correlates. J Racial Ethn Health Disparities. 2015;2(4):425–33. https://doi.org/10.1007/s40615-015-0089-8.
United States Census Bureau. Urban Areas Facts. 01/24/23. https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural/ua-facts.html
Gourevitch MN, Athens JK, Levine SE, Kleiman N, Thorpe LE. City-Level Measures of Health, Health Determinants, and Equity to Foster Population Health Improvement: The City Health Dashboard. Am J Public Health. 2019;109(4):585–92. https://doi.org/10.2105/ajph.2018.304903.
Bilal U, McCulley E, Li R, et al. Tracking COVID-19 Inequities Across Jurisdictions Represented in the Big Cities Health Coalition (BCHC): The COVID-19 Health Inequities in BCHC Cities Dashboard. Am J Public Health. 2022;112(6):904–12. https://doi.org/10.2105/ajph.2021.306708.
Fenelon A, Boudreaux M. Life and Death in the American City: Men’s Life Expectancy in 25 Major American Cities From 1990 to 2015. Demography. 2019;56(6):2349–75. https://doi.org/10.1007/s13524-019-00821-2.
Benjamins MR, Silva A, Saiyed NS, De Maio FG. Comparison of All-Cause Mortality Rates and Inequities Between Black and White Populations Across the 30 Most Populous US Cities. JAMA Netw Open. 2021;4(1):e2032086. https://doi.org/10.1001/jamanetworkopen.2020.32086
Sighoko D, Murphy AM, Irizarry B, Rauscher G, Ferrans C, Ansell D. Changes in the racial disparity in breast cancer mortality in the ten US cities with the largest African American populations from 1999 to 2013: The reduction in breast cancer mortality disparity in Chicago. Cancer Causes Control. 2017;28(6):563–8. https://doi.org/10.1007/s10552-017-0878-y.
Brown AF, Ma GX, Miranda J, et al. Structural Interventions to Reduce and Eliminate Health Disparities. Am J Public Health. 2019;109(S1):S72-s78. https://doi.org/10.2105/ajph.2018.304844.
Grubbs SS, Polite BN, Jr JC, et al. Eliminating Racial Disparities in Colorectal Cancer in the Real World: It Took a Village. J Clin Oncol. 2013;31(16):1928-1930https://doi.org/10.1200/jco.2012.47.8412
Detailed Mortality data are compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative; the data set is produced by the U.S. Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS), Division of Vital Statistics (DVS), Mortality Statistics Branch.
Herman E. The American Community Survey: an introduction to the basics. Gov Info Quarterly. 2008;25(3):504–19.
Benjamins MR, De Maio FG, eds. Unequal Cities: Structural Racism and the Death Gap in America's Largest Cities. Johns Hopkins University Press; 2021.
Benjamins MR, Lorenz P, Saiyed NS, et al. Black-White Inequities in Kidney Disease Mortality Across the 30 Most Populous US Cities.J Gen Intern Med. 2022/05// 2022;37(6):1351–1358. https://doi.org/10.1007/s11606-022-07444-1
City Health Dashboard Team. City Health Dashboard Technical Document. 2022. https://www.cityhealthdashboard.com/technical-documentation
Chiang CL. The life table and its construction. In: Introduction to Stochastic Processes in Biostatistics. Wiley; 1968. p. 189–214.
Rothenberg R, Stauber C, Weaver S, Dai D, Prasad A, Kano M. Urban health indicators and indices—current status. BMC Public Health. 2015;15(1):494.
LaVeist-Ramos TA, Galarraga J, Thorpe RJ Jr, Bell CN, Austin CJ. Are black Hispanics black or Hispanic? Exploring disparities at the intersection of race and ethnicity. J Epidemiol Community Health. 2012;66(7): e21. https://doi.org/10.1136/jech.2009.103879.
Ford ME, Kelly PA. Conceptualizing and categorizing race and ethnicity in health services research. Health Serv Res. 2005;40(5 Pt 2):1658–75. https://doi.org/10.1111/j.1475-6773.2005.00449.x.
Flanagin A, Frey T, Christiansen SL, Committee AMoS. Updated Guidance on the Reporting of Race and Ethnicity in Medical and Science Journals. Jama. 2021;326(7):621–627. doi:https://doi.org/10.1001/jama.2021.13304
Freudenberg N, Franzosa E, Chisholm J, Libman K. New approaches for moving upstream: how state and local health departments can transform practice to reduce health inequalities. Health Educ Behav. 2015;42(1 Suppl):46s–56s. https://doi.org/10.1177/1090198114568304.
Sims J, Baird R, Aboelata MJ, Mittermaier S. Cultivating a Healthier Policy Landscape: The Building Healthy Communities Initiative. Health Promot Pract. 2023;24(2):300–9. https://doi.org/10.1177/15248399221114341.
O’Keefe KA, Shafir SC, Shoaf KI. Local health department epidemiologic capacity: a stratified cross-sectional assessment describing the quantity, education, training, and perceived competencies of epidemiologic staff. Front Public Health. 2013;1:64. https://doi.org/10.3389/fpubh.2013.00064.
Newman SJ, Ye J, Leep CJ, Hasbrouck L, Zometa C. Assessment of Staffing, Services, and Partnerships of Local Health Departments - United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65(25):646–9. https://doi.org/10.15585/mmwr.mm6525a2.
Ye J, Leep C, Newman S. Reductions of budgets, staffing, and programs among local health departments: results from NACCHO's economic surveillance surveys, 2009–2013. Journal of public health management and practice : JPHMP. Mar-Apr 2015;21(2):126–33. https://doi.org/10.1097/phh.0000000000000074
American Public Health Association. Racism is a Public Health Crisis. Accessed 01/31/2023, https://www.apha.org/topics-and-issues/health-equity/racism-and-health/racism-declarations
Benjamins MR, Poonsapaya J, Laflamme E, F GDM. Racial Health Equity Plans in the 30 Largest US Cities. J Racial Ethn Health Disparities. 2023;https://doi.org/10.1007/s40615-023-01662-x
Castaneda Y, Jacobs J, Margellos-Anast H, et al. Developing and Implementing Racial Health Equity Plans in 4 Large US Cities: A Qualitative Study.J Public Health Manag Pract. 6 2023;https://doi.org/10.1097/phh.0000000000001756
Kho AN, Cashy JP, Hota B, et al. The Chicago Health Atlas: A Public Resource to Visualize Health Conditions and Resources in Chicago. 2012:
Ansell DA, Fruin K, Holman R, Jaco A, Pham BH, Zuckerman D. The Anchor Strategy - A Place-Based Business Approach for Health Equity. N Engl J Med. 2023;388(2):97–9. https://doi.org/10.1056/NEJMp2213465.
Bishop-Royse J, Saiyed NS, Schober DJ, et al. Cause-Specific Mortality and Racial Differentials in Life Expectancy, Chicago 2018–2019. J Racial Ethn Health Disparities. 27 2023:1–7. https://doi.org/10.1007/s40615-023-01566-w
Roesch PT, Saiyed NS, Laflamme E, De Maio FG, Benjamins MR. Life Expectancy Gaps Among Black and White Persons and Contributing Causes of Death in 3 Large US Cities, 2018–2019. JAMA Netw Open. 2023;6(3):e233146–e233146. https://doi.org/10.1001/jamanetworkopen.2023.3146.
Frolich K, Potvin L. The inequality paradox: the population approach and vulnerable populations. Am J Public Health. 2008;98(2):216–21.
Hall M, Graffunder C, Metzler M. Policy Approaches to Advancing Health Equity. J Public Health Manag Pract. 2016;22 Suppl 1:S50–9. https://doi.org/10.1097/phh.0000000000000365
Eslava-Schmalbach J, Mosquera P, Alzate JP, et al. Considering health equity when moving from evidence-based guideline recommendations to implementation: a case study from an upper-middle income country on the GRADE approach. Health Policy Plan. 2017;32(10):1484–90. https://doi.org/10.1093/heapol/czx126.
Gómez CA, Kleinman DV, Pronk N, et al. Addressing Health Equity and Social Determinants of Health Through Healthy People 2030. J Public Health Manag Pract. 2021;27(Supplement 6):S249–57. https://doi.org/10.1097/phh.0000000000001297.
Ansell D, Grabler P, Whitman S, et al. A community effort to reduce the black/white breast cancer mortality disparity in Chicago. Cancer Causes Control. 2009;20(9):1681–8. https://doi.org/10.1007/s10552-009-9419-7.
Richards CA, Kerker BD, Thorpe L, et al. Increased screening colonoscopy rates and reduced racial disparities in the New York Citywide campaign: an urban model. Am J Gastroenterol. 2011;106(11):1880–6. https://doi.org/10.1038/ajg.2011.191.
Johnson AK, Smith CS, Hunt B, Jacobs J, Roesch P. Chicago's Citywide COVID-19 Vaccine Equity Program: Protect Chicago Plus. Public Health Rep (Washington, DC : 1974). 2023;138(2):218–222. https://doi.org/10.1177/00333549221143093
Arias E, Schauman WS, Eschbach K, Sorlie PD, Backlund E. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital Health Stat 2. 2008;(148):1–23.
Caveney AF, Smith MA, Morgenstern LB, Lisabeth LD. Use of death certificates to study ethnic-specific mortality. Public Health Rep (Washington, DC : 1974). 2006;121(3):275–81. https://doi.org/10.1177/003335490612100309
Harper S, Lynch J. Methods for measuring cancer disparities: using data relevant to healthy people 2010 cancer-related objectives. NCI Cancer Surveillance Monograph Series, Number 6. Bethesda, MD: National Cancer Institute; 2005. NIH Publication No. 05-5777.
Ochiai E, Kigenyi T, Sondik E, et al. Healthy People 2030 Leading Health Indicators and Overall Health and Well-being Measures: Opportunities to Assess and Improve the Health and Well-being of the Nation. J Public Health Manag Pract. 01 2021;27(Suppl 6):S235-s241. https://doi.org/10.1097/phh.0000000000001424
Peppard PE, Kindig DA, Dranger E, Jovaag A, Remington PL. Ranking community health status to stimulate discussion of local public health issues: the Wisconsin County Health Rankings. Am J Public Health. 2008;98(2):209–12. https://doi.org/10.2105/ajph.2006.092981.
Purtle J, Peters R, Kolker J, Diez Roux AV. Uses of Population Health Rankings in Local Policy Contexts: A Multisite Case Study. Med Care Res Rev. 2019;76(4):478–96. https://doi.org/10.1177/1077558717726115.
Woolf SH, Purnell JQ, Simon SM, et al. Translating evidence into population health improvement: strategies and barriers. Annu Rev Public Health. 2015;36:463–82. https://doi.org/10.1146/annurev-publhealth-082214-110901.
Farrer L, Marinetti C, Cavaco YK, Costongs C. Advocacy for health equity: a synthesis review. Milbank Q. 2015;93(2):392–437. https://doi.org/10.1111/1468-0009.12112.
Erwin PC, Myers CR, Myers GM, Daugherty LM. State responses to America's Health Rankings: the search for meaning, utility, and value. J Public Health Manag Pract. 2011;17(5):406–12. https://doi.org/10.1097/PHH.0b013e318211b49f
Corburn J, Cohen AK. Why we need urban health equity indicators: integrating science, policy, and community. PLoS Med. 2012;9(8):e1001285. https://doi.org/10.1371/journal.pmed.1001285.
Curtin SC, Heron MP. COVID-19 Death Rates in Urban and Rural Areas: United States, 2020. US Deparment of Health and Human Services, Centers for Disease Control and …; 2022.
Bor J, Assoumou SA, Lane K, et al. Inequities in COVID-19 vaccine and booster coverage across Massachusetts ZIP codes after the emergence of Omicron: A population-based cross-sectional study. PLoS Med. 2023;20(1):e1004167. https://doi.org/10.1371/journal.pmed.1004167.
Geronimus AT. To mitigate, resist, or undo: addressing structural influences on the health of urban populations. Am J Public Health. 2000;90(6):867–72. https://doi.org/10.2105/ajph.90.6.867.
Mody A, Bradley C, Redkar S, et al. Quantifying inequities in COVID-19 vaccine distribution over time by social vulnerability, race and ethnicity, and location: A population-level analysis in St. Louis and Kansas City, Missouri. PLoS Med. 2022;19(8):e1004048. https://doi.org/10.1371/journal.pmed.1004048
Acknowledgements
This work builds on the research first conducted by Dr. Steve Whitman, the founding director of the Sinai Urban Health Institute.
Funding
None.
Author information
Authors and Affiliations
Contributions
MB conceived the idea for the study. NS acquired the restricted data and conducted the statistical analysis. AS contributed to the statistical analysis. AS, MB, and NS wrote the initial draft of the manuscript. MB, NS, and EC designed the tables and figures. All authors provided edits to the manuscript, read it, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Mount Sinai Hospital Institutional Review Board determined the study to be exempt in accordance with United States Department of Health and Human Services Regulation 45 CFR 46.101(b) and approved a waiver of consent in accordance with 45 CFR 46.117C(2). All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 1.
Selected City-Level Sociodemographic Characteristics for the U.S. and the 30 Most Populous Cities.
Additional file 2: Table 2.
Life Expectancy and 95% Confidence Intervals for the Total Population (Males and Females) by Racial Group at Four Time Points.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Silva, A., Saiyed, N.S., Canty, E. et al. Pre-pandemic trends and Black:White inequities in life expectancy across the 30 most populous U.S. cities: a population-based study. BMC Public Health 23, 2310 (2023). https://doi.org/10.1186/s12889-023-17214-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17214-1