Abstract
Background
Socioeconomic differences in the impact of alcohol consumption on health have been consistently reported in the so-called “alcohol harm paradox” (i.e., individuals from higher socioeconomic backgrounds (SES) drink more alcohol than individuals from lower SES, but the latter accrue more alcohol-related harm). Despite the severe health risks of smoking however, there is a scarcity of studies examining a possible “smoking harm paradox” (SHP). We aim to fill this gap.
Methods
We conducted a prospective cohort study with adolescents from the Norwegian Longitudinal Health Behaviour Study (NLHB). Our study used data from ages 13 to 30 years. To analyse our data, we used the random-intercept cross-lagged panel model (RI-CLPM) with smoking and self-reported health as mutual lagged predictors and outcomes as well as parental income and education as grouping variables. Parental income and education were used as proxies for adolescent socioeconomic status (SES). Smoking was examined through frequency of smoking (every day, every week, less than once a week, not at all). General health compared to others was measured by self-report.
Results
Overall, we found inconclusive evidence of the smoking harm paradox, as not all effects from smoking to self-reported health were moderated by SES. Nevertheless, the findings do suggest that smoking predicted worse subjective health over time among individuals in the lower parental education group compared with those in the higher parental education group. This pattern was not found for parental income.
Conclusions
While our results suggest limited evidence for a smoking harm paradox (SHP), they also suggest that the impact of adolescent smoking on later subjective health is significant for individuals with low parental education but not individuals with high parental education. This effect was not found for parental income, highlighting the potential influence of parental education over income as a determinant of subjective health outcomes in relation to smoking.
Similar content being viewed by others
Background
The harmful effect of social disadvantage on health, in other words social inequities in health, have been reported consistently in previous literature and are long-lasting and significant [1, 2]. Despite being hailed as an equal society, Norway also shows evidence of social inequities in health. For example, men and women with the highest level of attained education live approximately 5–6 years longer than those with the lowest educational attainment [3], and differences in mortality between educational groups in Norway are among some of the largest in Europe [3, 4].
It has been suggested that social inequities in health can be attributed in part to differences in lifestyle behaviours, such as smoking. According to the Norwegian Directorate of Health [5] and Statistics Norway [6], 9% of people in Norway between the ages of 16–74 years smoked daily in 2020, and 6,300 people die of tobacco related diseases each year making smoking an important public health concern. While some studies suggest that daily smoking among youth is decreasing [7], the health effects of smoking earlier in life are likely to still be unfolding today. Smoking has been linked to a wide range of health problems including but not limited to cancer, respiratory and cardiovascular diseases, inflammation, impaired immune function [8], and mental health problems [9]. The Norwegian Directorate of Health [5] reports that individuals with no to low educational attainment have a higher prevalence of smoking than those with higher educational attainment. Similarly, a study conducted among Norwegian adolescents aged 16 to 20 found that those who had no plans to undertake further education versus those who did, had up to 3.8 higher odds of smoking [10]. Furthermore, a systematic review exploring smoking and social inequities concluded that people from disadvantaged backgrounds were both more likely to smoke and experience severe harms from smoking, for example becoming trapped in poverty [11].
Hence, it appears that people from lower socioeconomic backgrounds may incur more severe health harms from certain substances. Alcohol use, for example, has been associated with greater health concerns in lower socioeconomic groups [12]. This has been described in the “alcohol harm paradox” (AHP), which posits that individuals from lower socioeconomic backgrounds experience disproportionately greater alcohol-related health harms than individuals from higher socioeconomic background at the same, or lower, levels of alcohol consumption [13]. The AHP has been reported consistently in previous literature [13,14,15]. This has been shown in studies for both adults and adolescents using cross-sectional and longitudinal designs [16, 17]. Research regarding a “smoking harm paradox” (SHP), on the other hand, is scarce.
A life course perspective suggests that it is necessary to measure the early precursors of diseases to fully grasp their development over time [18]. Onset of smoking commonly occurs during adolescence [19], however, some smoking-related diseases endure a long latency period before manifesting clinically [20, 21]. This suggests that clinical measures of smoking-related harm might not be appropriate at earlier stages of disease development (e.g., adolescence), instead, self-reported health might be more indicative of how adolescent smoking affects health at the subclinical level. The discovery of a SHP as based on self-reported health would corroborate this line of thinking and highlight adolescence as a key developmental period for early interventions aiming to not only reduce smoking but also long-term smoking-related health disparities [19].
Aims
Thus, the purpose of the current study is to investigate a possible SHP in a longitudinal dataset of Norwegian youths (NLHB) that were followed up over 17 years. Though earlier studies using the NLHB have looked at smoking in relation to various health outcomes (e.g., depression) and using different predictors (e.g., sibling smoking, parental smoking etc.), none have specifically considered a smoking-related harm paradox and if this association can be detected at a pre-clinical level as the harmful effects of smoking gradually unfold from adolescence to adulthood [21,22,23,24]. Our research question is whether the relationship between smoking frequency and self-reported health is moderated by parents’ educational attainment and income (as proxies for childhood SES). If the harm paradox holds for smoking, we hypothesise that individuals who smoke from higher socioeconomic backgrounds would report better self-reported health than those with lower socioeconomic backgrounds.
Methods
Study design
We conducted a prospective cohort study using data from the ‘Norwegian Longitudinal Health Behaviour Study’ (NLHB), in which a cluster sample from a cohort of adolescents was followed from age 13 (1990) to 30 (2007). See Table 1 for the sample size of the study between 1990 and 2007. The NLHB study was reviewed by the Data Inspectorate of Norway and received a recommendation from the Regional Committee of Medical Research Ethics (REK). Informed written consent has been obtained from participants at every consecutive time point. More detailed information on data collection is available in previous publications [22, 25]. See Appendix A for a frequency table of variables of interest at each time point. Other studies using the NLHB dataset have also reported on attrition - showing that individuals with higher levels of parental income and education are more likely to participate at later follow-ups [26]. For the present study, we also conducted an attrition analysis for participation in 2007 (age 30) but did not find any associations with degree of smoking and self-reported health at baseline in 1990 (age 13) (See Appendices). For the NLHB total sample, 43% (n = 536) participated in 2007 (age 30) from the original n = 1242 which participated at least once during the study period (See Table 1 for frequencies).
Variables
Outcome
Self-reported health
In line with previous literature, which has used single item measures to suggest that smokers typically report worse self-perceived health than non-smokers [27,28,29,30] and because of the wide range of health problems associated with smoking, we chose to focus on participants’ self-reported health. We measure self-reported health through the item ‘How would you rate your health compared to others your age?’. Response options were: ‘very good’, ‘good’, ‘neither’, ‘bad’ and ‘very bad’.
Predictor
Smoking frequency
Participants’ smoking frequency was measured through the item ‘How often do you smoke?’ with response options: ‘every day’, ‘every week’, ‘less than once a week’ or ‘not at all’. Similar wording has been used to examine smoking frequency in previous studies [27, 31].
Groups
Socioeconomic status
Given that our baseline measurement was taken when participants were aged 13 years, we measured adolescent socioeconomic status (SES) for 1995 through parents’ self-reported salary and educational attainment in 1996. The income variable has the following response categories: “Less than NOK 100.000”, “NOK 100–199.000”, “NOK 200–299.000”, “NOK 300–399.000”, “NOK 400–499.000” and “NOK 500.000 or more” with the annual average wage being 213 000 NOK in 1995 (1 NOK ≈ 0.12 EUR using the 2007 exchange rate). The education variable had the following response categories: “0 years of education after elementary school”, “1–2 years of education after elementary school”, “3 years of education after elementary school”, “Less than 4 years at university/college”, “More than 4 years at university/college” and “Other”. The last category and missing values were replaced with adolescents’ report of parental socioeconomic status following the logic described in Jørgensen and colleagues [26]. Both variables were dichotomised for use in the analyses, resulting in approximately equal distributions for parental education (low = 578, high = 390) and parental income (low = 323, high = 292). The NLHB dataset also contains data on adolescents’ report of parental education and occupation [25], however, using parental SES as a proxy for adolescent SES is a common procedure [32,33,34]. We also chose not to include parental occupation, as salaries and educational attainment are comparable across professions, while occupation can vary greatly in terms of responsibilities and pay.
Control variables
We included gender as a control variable, given the differential educational gradient previously observed between men and women [35].
Statistical analyses
Analyses were performed in Mplus 8 for Windows [36] using maximum likelihood estimation with robust standard errors to account for skewness in the data. Code is available on OSF (DOI https://doi.org/10.17605/OSF.IO/ZCBMS). We conducted a random intercept cross lagged panel model (RI-CLPM) of the relationship between self-reported health and smoking frequency (i.e., every day, every week, less than once a week, not at all) with parental education and income as a moderator. The RI-CLPM was specified following Hamaker [37]. We used standard cut-offs for evaluation of fit for structural equation models: CFI: ≥ 0.90, RMSEA: ≤ 0.08 and SRMR: ≤ 0.08 [38, 39]. Our model evaluation did not rely on the p-value for the chi-square test as studies have shown this is too sensitive to sample size, and thus, not an appropriate criterion for evaluation [40]. We used Full Information Maximum Likelihood (FIML) to manage bias associated with missing data.
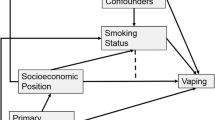
See Fig. 1 for the measurement model. Initially, we created two random intercepts, one for each construct, with factor loadings to all time points constrained to unity. Next, we specified 18 latent within-person variables: one for each measurement occasion in both constructs across nine time points. These latent variables had factor loadings constrained to unity. We constrained the variance in all observed variables to zero to ensure all variance is captured by the intercepts and within-person variables. Next, we added cross-lagged effects from smoking to self-reported health. Notably, we did not include cross-lagged effects from self-reported health to smoking as these effects were not directly relevant to our hypothesis. In addition, we wanted to make our model as parsimonious as possible with as few parameters to estimate as needed.
To investigate whether the model had time-invariant effects from smoking to self-reported health, we constrained similar time intervals of the cross-lagged effects to be equal throughout the study (e.g., 1990 to 1991/1991 to 1992 and 1993 to 1995/1996 to 1998). We compared the model fit of a freely estimated model to the model with cross-lagged constraints using a chi-square difference test. This was examined in all socioeconomic status groups: low parental education, high parental education, low parental income, and high parental income. If the model fit improved or did not significantly deteriorate in the nested model compared to the freely estimated model, the cross-lagged constraints were deemed tenable and kept in place for the multi-group analyses. Lastly, gender was added as a control variable with regression coefficients to the observed variables on each time point.
The socioeconomic moderation analyses were performed using multi-group analyses across parental education and income with 1000 bootstraps. Cross-lagged parameters were compared across groups using the model constraint function in Mplus.
Our analyses were preregistered on the Open Science Framework. The original pre-registration was published on the 7 February 2023 (https://doi.org/10.17605/OSF.IO/U9XVR), and the edited version following changes in analysis due to failed model fit procedures was published on 6 March 2023 (https://doi.org/10.17605/OSF.IO/9Z27A).
Results
Socioeconomic moderation RI-CLPM of smoking and self-reported health
The time-invariant cross-lagged constraints did not significantly deteriorate in the low (ΔX2 = 3.39, Δdf = 5, p = .640) and high (ΔX2 = 1.87, Δdf = 5, p = .867) parental education groups. Similarly, the cross-lagged constraints did not significantly worsen model fit in the low (ΔX2 = 6.21, Δdf = 5, p = .286) and high (ΔX2 = 1.88, Δdf = 5, p = .865) parental income groups. Thus, we kept the time-invariant cross-lagged constraints in the multi-group analyses. For space constraints, we only present the standardised cross-lagged effects of smoking on self-reported health across socioeconomic groups. Please see Appendix B for a comprehensive overview of the results.
Parental education
The parental education multi-group RI-CLPM with smoking and self-reported health achieved acceptable model fit: X2 = 427.065, df = 252, RMSEA (95% CI) = 0.040 (0.033 – 0.047), CFI = 0.962, SRMR = 0.062. The results are presented in Fig. 2 which demonstrate the association from smoking to self-reported health, associations between smoking and self-reported health at the same time-point, an estimate for the association between smoking at one time-point to the next, and the estimate of the association of the random intercepts between smoking and self-reported health (β = − 0.31 and − 0.35). Although there are some cross-lagged differences from smoking to self-reported health across parental education groups, these differences were not significant. The low parental education group had negative and significant cross-lagged effects from smoking to self-reported health from 1990 to 1991 (β = − 0.12, p < .01), 1991 to 1992 (β = − 0.14, p < .01), 1992 to 1993 (β = − 0.13, p < .01), and 1995 to 1996 (β = − 0.13, p < .01). There were no significant cross-lagged effects from smoking to self-reported health in the high parental education group.
Parental income
The parental income multi-group analysis of the RI-CLPM with smoking and self-reported health produced acceptable model fit: X2 = 3.85.816, df = 252, RMSEA (95% CI) = 0.044 (0.035 – 0.052), CFI = 0.957, SRMR = 0.064. The results are presented in Fig. 3, which demonstrate the association from smoking to self-reported health, associations between smoking and self-reported health at the same time-point, an estimate for the association between smoking at one time-point to the next. There were no discernible differences between the parental income groups on the cross-lagged effects from smoking to self-reported health. There were no significant cross-lagged effects from smoking to self-reported health in either of the parental income groups.
Simplified presentation of the parental education moderation of the RI-CLPM with Smoking and self-reported health. Note. Standardised estimates are presented in the figure. The high parental education group is on the top line and the low parental education group is on the lower line. *** p < .001, ** p < .01, * p < .05. SRH = self-reported health
Simplified presentation of the parental income moderation of the RI-CLPM with Smoking and self-reported health. Note. Standardised estimates are presented in the figure. The high parental income group is on the top line and the low parental income group is on the lower line. *** p < .001, ** p < .01, * p < .05. SRH = self-reported health
Discussion
We find inconclusive evidence of a smoking harm paradox in this study. Our findings suggest that young people aged 13–19 years whose parents had lower educational attainment experienced negative effects of smoking on later self-reported health in the period from 1990 to 1996. Based on a simulation study by Orth [41], which categorised the size of effects in RI-CLPM analyses, we can further conclude that the statistically significant effects were large. Contrastingly, the effects of smoking on subsequent self-reported health in the high parental education group were small to moderate [41] and not significant. Smoking did not significantly affect later self-reported health among people in the high or low parental income groups. Furthermore, the difference between the groups in a moderation analysis was not statistically significant.
Our mixed comparative findings imply some similarities to those implied by the alcohol-harm-paradox. While significant associations were identified, they were only captured in relation to parental educational attainment, rather than parental income, suggesting the paradox may be sensitive to specific dimensions of socioeconomic status. Socioeconomic status is a complex social construct, and when measured differently often captures associations of differing size or directions. Educational qualifications offer knowledge assets, and at a parental level offer choice and constraints on how their children’s socioeconomic circumstances can be influenced, including education which is a strong determinant of employment and income opportunities [42,43,44]. Importantly, the predictive power of education has previously been highlighted by Winkleby and colleagues [45], who concluded that higher education may be the strongest SES predictor of good health. Whereas income relates to material assets [43], which can be used to gain access to health promoting environments, such as green-space, safe employment, and commodities such as food, exercise along with a higher relative social-standing [42]. In a study of adolescents, Melotti and colleagues [12] found that a higher socioeconomic position was associated with decreased previous and ever smoking, notably maternal education showed a greater effect size compared to disposable income. In the case of smoking, we find that parental educational attainment is a key construct of socioeconomic status which is likely to capture attitudes, knowledge, and general acceptability of smoking. Hence, further research must explore the smoking harm paradox with a representative sample utilising multiple constructs of socioeconomic status (i.e., education, income, neighbourhood) to examine the differing contributions of social, cultural, and economic advantage.
While our study did not examine underlying mechanisms, it is possible that some mechanisms that have been proposed for the AHP may also be relevant here. For example, populations being exposed to other health challenges that interact creating a ‘multiplicative’ risk to health [46]. It is well known, for instance, that smoking is positively associated with a variety of health behaviours during adolescence, including consumption of alcohol, soft drinks and fast food [47]. In a study of Icelandic adolescents, it was found that some health behaviours had a multiplicative risk, with diet, physical activity and substance use constituting separate constructs using principal component analysis [48]. Similarly, a more recent study of Italian adults found some health behaviours clustered together, although some also had a mixed picture of healthful and unhealthful behaviours [49]. This multiplicative risk may occur at multiple levels including individual, neighbourhood (access to healthful food, or areas to exercise), structural, or political (funding afforded to area, policies to support deprived groups etc.) [50]. Other mechanisms include lifestyle, suggesting that differences in health behaviours observed between socioeconomic groups may be the result of strong socioeconomically patterned environmental influences (e.g., high levels of social and physical stressors) with ramifications for general health consciousness [14]. In essence, it is possible that the paradox represents engagement in wider health behaviours which could extend smoking or alcohol. Further research must confirm this with a longitudinal, representative samples of adolescents.
The results of our study should also be considered in the international context. Norway has consistently been “one step ahead” of the recommendations and regulations of the EU and World Health Organisation Framework Convention on Tobacco Control (WHO FCTC) [51], with a ban on the advertising of tobacco products being in 1973, compared to 1978 in Finland [52, 53], 2002 in the UK, and 2009 in Ireland (despite being signed in 2002) [54]. In Norway, smoking rates have decreased at a faster rate compared to some other EU countries, particularly for men at low and high educational levels [55]; in 2019 only 10% of the population in Norway were considered ‘daily smokers’ compared to the EU average of 18% [56]. Moreover, given Norway has a Gini coefficient of 0.26 [57], the fifth lowest income inequality in the entire index, it is plausible that the paradox could be a larger problem in other, less equal countries, particularly those with limited tobacco control, although it must be noted that there is unclear evidence regarding the equity impact of tobacco control interventions [58]. However, while Norway has progressive tobacco control measures in a global context, we still observed some indication of a paradox in the adolescent years; this association could be due to adolescent-specific symptoms, policy changes, or our sample being underpowered at older ages. We recommend that future research investigate the smoking harm paradox, with specific focus on the effect of parental education, across multiple countries to examine its generalisability beyond the Norwegian context. We further recommend that future research include other measures of sub-clinical health that capture the early effects of smoking.
Strengths and limitations
The study’s strengths include the panel design and follow-up time of 17 years, which allowed us to examine intra-individual changes over time. However, one possible reason for our inconclusive results is the limited variation in SES among our participants. Future studies should examine a smoking harm paradox in more socioeconomically heterogeneous samples across different countries as Norway is known to have a compressed wage structure - with reduced income-gains by additional years of education [56, 59]. Furthermore, we have based our analyses on self-reported measures of smoking. Self-report measures have been criticised for being unreliable and at risk of under-reporting [11]. However, under-reporting of alcohol consumption is said to be similar across socio-economic groups [46] and while a tendency to underreport smoking status has been observed among low international SES women and male blue collar workers, the validity of self-reported smoking status did not differ by SES [60]. Hence, while people may generally under-report smoking, there is little reason to believe that this should differ systematically between socioeconomic groups. It has also been suggested that adolescents from higher SES backgrounds are more likely to participate at later follow-ups [61], a bias that may have affected our findings in that our findings for lower SES individuals may be less valid. In fact, earlier studies using the NLHB data do confirm a bias towards higher SES individuals (i.e., higher parental income and education) being more likely to participate at later time points [26]. Finally, SES is a complex concept and the way in which we chose to measure it, through parental education and salary rather than occupation, may have had impacts on our findings. We present our justification for these choices, but future studies may want to consider different measures of SES as discussed in Cohen [62]. More studies are needed to conclude whether and under what circumstances a smoking harm paradox exists. Finally, we should also note that although the present study uses data dating back to 1990, we believe the longitudinal dimension of the data with multiple time points outweighs the cohort-specific limitations that might be present by adding a novel contribution to the research field.
Conclusions
We found inconclusive evidence of SES affecting participants’ self-reported health over time. However, the findings suggest that the impact of adolescent smoking on later subjective health is significant for individuals in the low parental education group but not individuals in the high parental education group. This pattern was not found for parental income. These findings suggest that the smoking harm paradox might be tentatively comparable to the alcohol harm paradox. Our study lays the groundwork for future studies and indicates that education may play a different role in the impact of smoking on self-reported health compared to income. Nevertheless, this should be further examined in different contexts before clear conclusions can be drawn on the existence of the smoking harm paradox.
Data Availability
Our analyses were preregistered on the Open Science Framework. The original pre-registration was published on the 7 February 2023 (https://doi.org/10.17605/OSF.IO/U9XVR), and the edited version following changes in analysis due to failed model fit procedures was published on 6 March 2023 (https://doi.org/10.17605/OSF.IO/9Z27A). Mplus syntax for the RI-CLPM analyses is available on OSF (DOI https://doi.org/10.17605/OSF.IO/ZCBMS). The data are available upon reasonable request as explicit consent for depository sharing hasn’t been obtained.
Abbreviations
- SES:
-
Socioeconomic status
References
Braveman P, Gottlieb L. The Social determinants of Health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129:19–31.
Truesdale BC, Jencks C. The Health effects of Income Inequality: averages and disparities. Annu Rev Public Health. 2016;37:37:413–30.
Syse A. Social inequalities in health. Norwegian Institute of Public Health; 2018.
Mackenbach JP, Kulhanova I, Artnik B, Bopp M, Borrell C, Clemens T et al. Changes in mortality inequalities over two decades: register based study of European countries. BMJ. 2016;353.
Helsedirektoratet. Tobacco Control in Norway 2021 [Available from: https://www.helsedirektoratet.no/english/tobacco-control-in-norway.
Statistics Norway. Tobacco, alcohol and other drugs 2022 [Available from: https://www.ssb.no/en/helse/helseforhold-og-levevaner/statistikk/royk-alkohol-og-andre-rusmidler.
Tjora T, Skogen JC, Sivertsen B. Increasing similarities between young adults’ smoking and snus use in Norway: a study of the trends and stages of smoking and snus epidemic from 2010 to 2018. BMC Public Health. 2020;20(1).
US Department of Health and Human Services. The health consequences of smoking-50 years of progress A report of the Surgeon General.; 2014.
Luger TM, Suls J, Vander Weg MW. How robust is the association between Smoking and depression in adults? A meta-analysis using linear mixed-effects models. Addict Behav. 2014;39(10):1418–29.
Øverland S, Tjora T, Hetland J, Aaro LE. Associations between adolescent socioeducational status and use of snus and Smoking. Tob Control. 2010;19(4):291–6.
Hiscock R, Bauld L, Amos A, Fidler JA, Munafo M. Socioeconomic status and Smoking: a review. Addict Reviews. 2011;1248:107–23.
Melotti R, Heron J, Hickman M, Macleod J, Araya R, Lewis G. Adolescent Alcohol and Tobacco Use and early socioeconomic position: the ALSPAC Birth Cohort. Pediatrics. 2011;127(4):E948–E55.
Probst C, Kilian C, Sanchez S, Lange S, Rehm J. The role of alcohol use and drinking patterns in socioeconomic inequalities in mortality: a systematic review. Lancet Public Health. 2020;5(6):E324–E32.
Boyd J, Sexton O, Angus C, Meier P, Purshouse RC, Holmes J. Causal mechanisms proposed for the alcohol harm paradox-a systematic review. Addiction. 2022;117(1):33–56.
Bloomfield K. Understanding the alcohol-harm paradox: what next? Lancet Public Health. 2020;5(6):E300–E1.
Patrick ME, Wightman P, Schoeni RF, Schulenberg JE. Socioeconomic status and substance use among young adults: a comparison across constructs and Drugs. J Stud Alcohol Drug. 2012;73(5):772–82.
Collins SE. Associations between socioeconomic factors and alcohol outcomes. Alcohol Research-Current Reviews. 2016;38(1):83–94.
Hetlevik O, Vie TL, Meland E, Breidablik HJ, Jahanlu D. Adolescent self-rated health predicts general practice attendance in adulthood: results from the Young-HUNT1 survey. Scand J Public Health. 2019;47(1):37–44.
Nuyts PAW, Kuipers MAG, Willemsen MC, Kunst AE. Trends in age of Smoking initiation in the Netherlands: a shift towards older ages? Addiction. 2018;113(3):524–32.
Bhatt SP, Kim Y-i, Harrington KF, Hokanson JE, Lutz SM, Cho MH, et al. Smoking duration alone provides stronger risk estimates of Chronic Obstructive Pulmonary Disease than pack-years. Thorax. 2018;73(5):414–21.
Lipfert FW, Wyzga RE. Longitudinal relationships between Lung cancer mortality rates, Smoking, and ambient air quality: a comprehensive review and analysis. Crit Rev Toxicol. 2019;49(9):790–818.
Birkeland MS, Torsheim T, Wold B. A longitudinal study of the relationship between leisure-time physical activity and depressed mood among adolescents. Psychol Sport Exerc. 2009;10(1):25–34.
Tjora T, Hetland J, Aarø LE, Øverland S. Distal and proximal family predictors of adolescents’ smoking initiation and development: a longitudinal latent curve model analysis. BMC Public Health. 2011;11(1):911.
Tjora T, Hetland J, Aarø LE, Wold B, Wiium N, Øverland S. The association between Smoking and depression from adolescence to adulthood. Addiction. 2014;109(6):1022–30.
Holsen I, Kraft P, Vitterso J. Stability in depressed mood in adolescence: results from a 6-year longitudinal panel study. J Youth Adolesc. 2000;29(1):61–78.
Jorgensen M, Smith ORF, Wold B, Boe T, Haug E. Tracking of depressed mood from adolescence into adulthood and the role of peer and parental support: a partial test of the adolescent pathway model. Ssm-Population Health. 2023;23.
Sakala K, Kasearu K, Katus U, Veidebaum T, Harro J. Association between platelet MAO activity and lifetime drug use in a longitudinal birth cohort study. Psychopharmacology. 2022;239(1):327–37.
Larsson D, Hemmingsson T, Allebeck P, Lundberg I. Self-rated health and mortality among young men: what is the relation and how may it be explained? Scand J Public Health. 2002;30(4):259–66.
Prokhorov AV, Warneke C, de Moor C, Emmons KM, Jones MM, Rosenblum C, et al. Self-reported health status, health vulnerability, and smoking behavior in college students: implications for intervention. Nicotine Tob Res. 2003;5(4):545–52.
Cott CA, Gignac MAM, Badley EM. Determinants of self rated health for canadians with chronic Disease and disability. J Epidemiol Commun Health. 1999;53(11):731–6.
de Vries H, Candel M, Engels R, Mercken L. Challenges to the peer influence paradigm: results for 12–13 year olds from six European countries from the European Smoking Prevention Framework Approach study. Tob Control. 2006;15(2):83–9.
Lawlor DA, Sterne JAC, Tynelius P, Smith GD, Rasmussen F. Association of childhood socioeconomic position with cause-specific mortality in a prospective record linkage study of 1,839,384 individuals. Am J Epidemiol. 2006;164(9):907–15.
Kittleson MM, Meoni LA, Wang N-Y, Chu AY, Ford DE, Klag MJ. Association of childhood socioeconomic status with subsequent coronary Heart Disease in physicians. Arch Intern Med. 2006;166(21):2356–61.
Poulton R, Caspi A, Milne BJ, Thomson WM, Taylor A, Sears MR, et al. Association between children’s experience of socioeconomic disadvantage and adult health: a life-course study. Lancet. 2002;360(9346):1640–5.
van Hedel K, van Lenthe FJ, Groeniger JO, Mackenbach JP. What’s the difference? A gender perspective on understanding educational inequalities in all-cause and cause-specific mortality. BMC Public Health. 2018;18.
Muthén LK, Muthén BO. Mplus user’s guide. Los Angeles, CA: Muthén & Muthén; 1998–2017.
Hamaker E. How to run a multiple indicator RI-CLPM with Mplus. 2018.
Hu LT, Bentler PM. Cutoff criteria for fit indexes in Covariance structure analysis: conventional criteria Versus New Alternatives. Structural equation Modeling-a. Multidisciplinary J. 1999;6(1):1–55.
Kline RB. Principles and practice of structural equation modeling. 4 ed. New York: Guilford Press; 2016.
Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equation Modeling-a Multidisciplinary J. 2007;14(3):464–504.
Orth U, Meier LL, Buhler JL, Dapp LC, Krauss S, Messerli D et al. Effect size guidelines for Cross-lagged effects. Psychol Methods. 2022.
Galobardes B, Lynch J, Smith GD. Measuring socioeconomic position in health research. Br Med Bull. 2007;81–82:21–37.
Lynch J, Kaplan G, Socioeconomic L, Kawachi I, editors. Oxford University Press; 2000.
Smith GD, Hart C, Hole D, MacKinnon P, Gillis C, Watt G, et al. Education and occupational social class: which is the more important indicator of mortality risk? J Epidemiol Commun Health. 1998;52(3):153–60.
Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health - how education, income, and occupation contribute to risk-factors for Cardiovascular Disease. Am J Public Health. 1992;82(6):816–20.
Bellis MA, Hughes K, Nicholls J, Sheron N, Gilmore I, Jones L. The alcohol harm paradox: using a national survey to explore how alcohol may disproportionately impact health in deprived individuals. BMC Public Health. 2016;16.
Wang M, Wang H, Fei F-R, Xu C-X, Du X-F, Zhong J-M. The associations between cigarette Smoking and health-related behaviors among Chinese school-aged adolescents. Tob Induc Dis. 2017;15.
Stefansdottir IK, Vilhjalmsson R. Dimensions of health-related lifestyle in young adulthood: results from a national population survey. Scand J Caring Sci. 2007;21(3):321–8.
Glorioso V, Pisati M. Socioeconomic inequality in health-related behaviors: a lifestyle approach. Qual Quant. 2014;48(5):2859–79.
Bronfenbrenner U. The ecology of human development - experiments by nature and design. Harvard University Press; 1979.
Reitan T, Callinan S. Changes in Smoking rates among pregnant women and the General Female Population in Australia, Finland, Norway, and Sweden. Nicotine Tob Res. 2017;19(3):282–9.
ASH. [Internet] Tobacco Act [Cited 2023 Oct 5]: Available from: https://savutonsuomi.fi/en/towards-tobacco-free-finland/tobacco-act/; 2023 [.
Tobacco Advertising and Promotion Act. 2002, Pub. L. No. 7th June 2023.
WHO Framework Convention on Tobacco Control. Best Practices on implementation of the tobacco advertising and display ban at point of sale (No. 5). 2014.
Giskes K, Kunst AE, Benach J, Borrell C, Costa G, Dahl E, et al. Trends in smoking behaviour between 1985 and 2000 in nine European countries by education. J Epidemiol Commun Health. 2005;59(5):395–401.
Eurostat. Tobacco consumption statistics 2019 [Available from: //WOS:000370327400001.
OECD. Income inequality (indicator) 2023 [Available from: https://data.oecd.org/inequality/income-inequality.htm.
Smith CE, Hill SE, Amos A. Impact of population Tobacco control interventions on socioeconomic inequalities in Smoking: a systematic review and appraisal of future research directions. Tob Control. 2021;30(E2):E87–E95.
Lazear EP, Shaw K, National Bureau of Economic R. The structure of wages: an international comparison. Chicago: University of Chicago Press; 2008.
Hovanec J, Weiss T, Koch H, Pesch B, Behrens T, Kendzia B et al. Smoking intensity and urinary nicotine metabolites by socioeconomic status in the Heinz Nixdorf Recall study. BMC Public Health. 2022;22(1).
Jørgensen M, Smith ORF, Wold B, Bøe T, Haug E. Tracking of depressed mood from adolescence into adulthood and the role of peer and parental support: a partial test of the adolescent pathway model. SSM - Population Health. 2023;23.
Cohen S, Janicki-Deverts D, Chen E, Matthews KA. Childhood socioeconomic status and adult health. In: Adler NE, Stewart J, editors. Biology of Disadvantage: Socioeconomic Status and Health. Annals of the New York Academy of Sciences. 11862010. p. 37–55.
Acknowledgements
We thank the participants of the NLHB study for their contribution. Thank you also to Ozden Merve Mollaahmetoglu for providing the inspiration that ultimately led to the idea for this paper.
Funding
This project is funded by Norges Forskningsråd (Grant number 302225).
Open access funding provided by University of Bergen.
Author information
Authors and Affiliations
Contributions
Samantha Marie Harris: Conceptualisation (lead); formal analysis (supporting); project administration (equal); writing – original draft (equal); review and editing (equal). Magnus Jørgensen: Conceptualisation (supporting); formal analysis (equal); Software (equal); project administration (equal); writing – original draft (equal); writing – review and editing (equal). Emily Lowthian: Conceptualisation (supporting); formal Analysis (supporting), writing – original draft (equal); writing – review and editing (equal). Sara Madeleine Kristensen: Conceptualisation (supporting); software (equal); formal analysis (equal); writing – original draft (equal); review and editing (equal).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study used data from the Norwegian Longitudinal Health Behaviour (NLHB) study which has been approved by the Data Inspectorate of Norway and received a recommendation from the Regional Committee of Medical Research Ethics (REK). The study was also done in accordance with the principles of the Declaration of Helsinki. Informed written consent has been obtained from participants at every consecutive time point in the study.
Consent for publication
Not applicable.
Competing interests
Dr Lowthian’s partner works as a Marketing Manager for a Gambling Company in Wales. The remaining authors report no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Harris, S.M., Jørgensen, M., Lowthian, E. et al. Up in smoke? Limited evidence of a smoking harm paradox in 17-year cohort study. BMC Public Health 23, 2022 (2023). https://doi.org/10.1186/s12889-023-16952-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-16952-6