Abstract
Background
While the use of self-management apps has considerable promise to efficiently reduce the diabetes burden that disproportionally affects low- and middle-income countries (LMICs), and the multisectoral and multidisciplinary approaches have been encouraged to be used in diabetes management, little is known about the status of the integration of these approaches in the existing diabetes self-management apps. This review examines the diabetes apps in China as an indication of the current status of integrating multisectoral and multidisciplinary approaches in diabetes mHealth care in LMICs.
Methods
Eligible diabetes apps were searched on major Chinese app stores up to December 23, 2022. The app comprehensiveness index (ranging 0–80) regarding the app functions and diabetes management domains was created. The multisectoral and multidisciplinary features were summarized using indices derived from current guidance.
Results
Sixty-six apps were reviewed, all developed by private companies. The average comprehensiveness score was 16, with many major self-management domains and functions not represented among the reviewed apps. Forty apps (61%) involved multiple sectoral entities, with public/private and private/private collaborations being the most common collaborative combinations. Thirty-seven apps (56%) involved multiple disciplines, among which endocrinology/metabolism, nutrition, and cardiovascular medicine were the top three most common disciplines. Compared to non-multidisciplinary apps, multidisciplinary apps tended to provide more comprehensive services in apps (6.14 vs. 5.18, p = 0.0345). Different sectors and disciplines tended to work independently, without robust interactions, in providing diabetes management services in the reviewed apps.
Conclusion
Multisectoral and multidisciplinary features has presented in the current diabetes self-management apps in China; however, it is still in its infancy and significant limitations existed. More engagement of civil society organizations and community groups and innovative collaborations between sectors and disciplines are needed to provide comprehensive, continuous, and patient-centered mHealth care for patients with diabetes in LMICs like China. Clear guidance for integrating and evaluating the multisectoral and multidisciplinary efforts in self-management apps is necessary to ensure the effective use of mHealth solutions for diabetes management in LMICs.
Similar content being viewed by others
Background
Diabetes disproportionally affects low- and middle-income countries (LMICs), with 80% of adults diagnoses with diabetes in 2021– and an estimated additional 210 million undiagnosed adults – living in LMICs [1]. Its impact is significant, with 31.2 per 100,000 people dying of diabetes-related causes, and a DALY burden of 1108.3 per 100,000 persons per year in LMICs in 2019, each about twice the corresponding rate in HICs [2]. This makes diabetes management a critical concern for LMICs.
Due to the complex interaction of diabetes and its effects with factors spanning a wide range of social systems (e.g., food systems, education, health care, etc.), the WHO Global Action Plan for Prevention and Control NCDs 2013–2030 emphasizes the importance of applying the multisectoral approach to addressing non-communicable diseases (NCDs) like diabetes [3]. Multisectoral approaches recruit public sectors, private sectors and civil society organizations to provide the necessary support to prevent and treat diabetes [4]. Moreover, the Global Partnership for Effective Diabetes Management has recommended the implementation of an interdisciplinary team (IDT) approach, which integrates expertise from multiple medical disciplines, to help people manage and control their diabetes conditions [5].
Integrating multisectoral and multidisciplinary approaches can be demanding, especially given the resource and health system limitations of LMICs. Mobile technologies, which have been demonstrated to provide effective and efficient means for overcoming health system limitations in LMICs, provide a promising place for such integration to occur [6, 7]. Diabetes management mHealth efforts, chiefly in the form of self-management apps, are able to improve communication with health providers, build peer supportive social network, increase medication adherence, facilitate healthy lifestyle modification, and yield a significant reduction in hemoglobin A1C and complications [4, 8,9,10].
A natural hope is that the multisectoral and multidisciplinary collaboration necessary for effective diabetes management in LMICs might be efficiently accomplished through mobile systems. However, while studies have reviewed current diabetes self-management apps and their impact on diabetes-related outcomes among patients, little is known about the integration of multidisciplinary and multisectoral approaches within those apps available in LMICs. This study aims to begin exploring these issues by reviewing diabetes self-management apps in China, which serves as a particularly informative case for several reasons:
-
1)
China has – and likely will continue to have—the world’s largest diabetes epidemic, and the incidence of diabetes has increased more rapidly in China than in the world as a whole [11,12,13,14,15]. This suggests that the demand for effective apps should be comparatively high.
-
2)
China faces health workforce challenges similar to those faced by other LMICs, which makes developing effective systems of self-management for diabetes management essential [16, 17].
-
3)
Mobile penetration in China is high, and Chinese app marketplaces are well-developed, suggesting that there are few supply-side barriers for the development of diabetes management apps and providing a good ‘best-case’ perspective for mobile system and app development in other LMICs [18].
This study reviews the multisectoral and multidisciplinary integration in diabetes self-management apps available in the Chinese market. The findings from this study will 1) extend our current knowledge about the development stage of integrating multisectoral and multidisciplinary approaches in diabetes management mHealth applications in China, and 2) highlight the gap between the diabetes self-management guidance and the mHealth application practices, and provide useful information for future app improvement, in terms of engaging different sectors and disciplines and facilitating effective multisectoral and multidisciplinary collaborations.
Methods
Search strategies and selection criteria
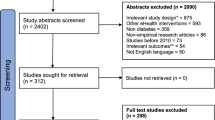
Diabetes self-management apps were identified by searching terms relating to diabetes (e.g., “diabetes/糖尿病,” “glucose/血糖,” “insulin/胰岛素, “diet/饮食,” “exercise/锻炼,” etc.) in the app stores of the four major smartphone brands in China – Xiaomi, Vivo, Apple, and Honor, representing 67% of the Chinese smartphone market as of December 23, 2022 [19]. Apps were deemed eligible for inclusion according to the following criteria: 1) they were designed for diabetes management, and 2) their interface was Chinese. Apps were excluded if: 1) were not designed for diabetes management or exclusively for lifestyle management (e.g., general wellbeing, diet management); 2) were not designed for patient use; 3) had not been updated in the past five years; or 4) could not be downloaded.
App review and data extraction
First, app name, developer, purpose, number of downloads, user rating, release date, date of most recent update, cost, and guidance/evidence basis was extracted from the description page and the actual app content. Second, the usability of the apps were assessed using the frameworks adopted from Arnhold et al. study (Additional file 1: Appendix A) [20].
Third, a comprehensiveness index was created to summarize the app functions in terms of covering the four major diabetes management domains laid out in the Chinese National Guidelines for the Prevention and Control of Diabetes in Primary Care (2022) [21]. The major app functions for diabetes management were adapted from Arnhold et al. study and summarized as 1) documentation (e.g., glucose logging, meal logging, exercise tracking, etc.), 2) education (e.g., providing information on the importance and ways to perform foot care, etc.), 3) sharing (e.g., exporting data, sharing data with healthcare providers, etc.), 4) analysis (e.g., calculating nutrition intakes, predicting the weight change trends, etc.), 5) reminding (e.g., reminding the patient of taking medications, etc.), 6) advising (e.g., using the recorded data or professionals’ experience to provide medication advice to app users, etc.), 7) shopping (e.g., creating in-app stores or providing links for diabetes medicines and care devices purchase, etc.), and 8) interfacing (e.g., connectivity to an external sensor/device to data entry or export) [20]. An ideal, comprehensive app will have all the eight abovementioned functions and cover all the four major diabetes management domains: 1) measures monitoring, 2) lifestyle modification (including 7 subdomains: weight control, nutrition, physical activity, smoking cessation, alcohol cessation, psychosocial care, and salt restriction), 3) medicine management, and 4) diabetic complication prevention and management. Reviewers assgined 0 (if the app did not have the function in the relevant diabetes management domain) or 1 (if the app had the function in the relevant diabetes management domain) to each function-domain pair (a total of 80 pairs) in the comprehensiveness matrix, treating each subdomain of lifestyle modification domain separately. Each app received a comprehensiveness score ranging from 0 to 80, with higher score indicating more comprehensive is the app for diabetes management (Additional file 1: Appendix B).
Finally, the multisectoral and multidisciplinary features of the reviewed apps were assessed. Sectors were divided into ‘public’, ‘private’, and ‘civil society organizations’, as per the WHO Toolkit for Developing a Multisectoral Action for Noncommunicable Diseases [4]. The role of each sector was assessed for each diabetes management function and domain. Multidisciplinarity was assessed by reviewing in-app education and consultation sections for the name of different disciplines, using the Chinese ‘List of Medical Institutions’ Diagnosis and Treatment Subjects’ to standardize the discipline names [22]. The number and name of disciplines and their collaborations in the apps were summarized and reported.
Data synthesis and analysis
Content and descriptive analyses were used to report on the apps’ specific characteristics. Chi-square and ANOVA test, whichever was appropriate, were used to compare the apps in subgroups. Excel for Microsoft 365 was used for analysis.
Results
Basic characteristics
Sixty-six eligible apps released between 2011 and 2022 were identified. The basic information of the reviewed apps is summarized in Table 1. Thirteen of the reviewed apps (20%) were designed for multi-chronic conditions (including diabetes) and their risk management, while the rest 53 reviewed apps were solely developed for diabetes and its risk management. The top three most popular apps (assessed by app downloads) were Huawei Sports Health (华为运动健康) (224 million), Peppermint Nutritionist (薄荷营养师) (12.68 million), and Excellent Health (优健康) (8.69 million). The average usability score among the 66 reviewed apps was 36 (ranging from 26 to 41). The usability scores did not significantly differ by the app release years, with or without within-app-fee-charge services, or download platforms. Apps developed by health/medical technology companies tended to receive higher usability scores than those developed by information technology companies or health management companies or individuals (37.2 vs. 35.5, p = 0.0644). Only one app, MMC Butler, received highest scores (41 out of 41) for its easy-to-use structures, understandable content, clear image and text presentation, and instant and understandable feedback. The average app rating score was 4.41 (on a scale of 0–5), with no significant difference between the average rating score of the Android apps and the IOS apps (4.60 vs. 4.36, p = 0.1285). Among the apps available from both platforms, the average rating scores on the Android platform was significantly higher than that on the IOS platform (4.71 vs. 4.34, p = 0.0270). Twelve apps—including 1 app only available on the Android platform, 6 apps only available on the IOS platform, and 5 app available on both platforms—were rated 5 out of 5 by users for reasons like “user-friendly”, “providing diabetes management-tailored functions and knowledge”, and “providing personalized feedback and advice for patients.” Several findings deserve special mention. First, private firms play a significant role in app development, and all reviewed apps included at least one private firm as the app developer or a partner. Second, many apps included some form of monetization or profit-seeking. Thirty-nine apps (59%) had in-app charges for membership and/or upgrading services (e.g., access to VIP education packages), twenty-seven apps (41%) included in-app markets (e.g., for medicines, books, nutritional supplements, insurance purchasing, etc.) and two apps (3%) cost an average of 12 RMB (1.75 USD at a rate of 6.87 RMB to 1 USD) to download. Third, most apps were focused on diabetes as a general condition without specifying diabetes types. Only three apps (4.5%) specifically targeted one kind of diabetes, with one each targeted for the management of type I, type II, and gestational diabetes. Fourth, explicit reference to scientific evidence or management guidelines was comparatively rare. Only eighteen apps (27%) referred to scientific evidenced and/or national/international guidelines for diabetes management in their app or content development.
Most apps were not comprehensive, and many domains and functions were not represented. The average comprehensiveness score of the reviewed apps was 16 (ranging from 3 to 44) (Table 2). Domains covered in more than 20% of reviewed apps included: measures monitoring (61.9%), weight control (29.5%), and medication management (26.9%), nutrition (22.9%), and physical activity (22%). Domains covered by less than 5% of apps included: salt restriction (2.8%), alcohol cessation (4.4%), smoking cessation (4.4%). Functions found in more than 20% of apps included: documentation (34.1%), education (32.9%), and analysis (20.5%). Major limitations observed in the reviewed apps included a tendency for measures monitoring which failed to include more than glucose and bodyweight, educational materials that lacked information about medication, complication and other lifestyle risks (e.g., smoking, alcohol, salt intake) beyond nutrition/weight control/measures monitoring management, analysis that focused on ad hoc data visualization and failed to make predictions of risks for future health events (like vision and kidney issues), lack of robust tools for the effective use of shared data, and advising that failed to address lifestyle modification and complication management.
Multisectoral collaboration endeavor
Forty reviewed apps (61%) involved more than one sector in their development and/or diabetes self-management service provision (Table 3). Among the multisectoral apps, 14 apps involved two sectoral entities, eight apps involved three entities, eight involved four entities, eight involved five entities, and two involved six entities. Public/private (n = 28) and private/private (n = 26) collaborations were the most common collaborative combinations, and eighteen reviewed apps included both public/private and private/private sector cooperations. Hospitals were the most common public sector entity, which appeared in 27 multisectoral apps, followed by community health centers (n = 3). Health/medical technology companies were the most common private sector entities, appeared in 34 multisectoral apps, followed by healthcare management companies (n = 24), and nutrition and food companies (n = 17), pharmaceutical companies (n = 10), and information technology companies (n = 8). There was only one civil society sector entity (Health Times (健康时报), a media agency, in the Renmin Health app) involved in the reviewed apps.
Different sectors tended to provide different diabetes service functions via the reviewed apps. Public sectors like hospitals were mainly involved in advising and education functions in the reviewed apps. The engagement of private sectors seemed to predict the inclusion of interface, data analysis, data sharing, and shopping functions of the reviewed apps. The participation of medical device companies, in particular, tended to result in an interface function, while the involvement of pharmaceutical companies, food producers, and insurance companies were more likely to include shopping functions. Civil society organization involvement contributed to spreading health education information and empowering the app users.
Even while there was significant multisector presence in the reviewed apps, different organizations tended to take charge of specific parts of the app, but rarely collaborate with each other in an integrated, multisectoral approach to any particular function. For instance, several apps contracted with health professionals from different hospitals and medical companies and allowed the health professionals to provide consulting and advising services to the app users; however, there was lack of obvious communication and collaboration between hospitals (public sector) and medical companies (private sector) in terms of providing holistic, comprehensive diabetes management care services to the app users. Similar patterns have been observed among the same type of sector agencies. For instance, Caring Church (关心堂) app partnered with hospitals and local community health centers, both of which were public sector entities. Although both the agencies provided various services via the app, there was no direct collaboration between the hospitals and the community health centers (like referring patients and providing continuous care to the users).
Multidisciplinary collaboration endeavor
Thirty-seven of the reviewed apps (56%) involve more than one discipline. Four apps – People’s Health, Zhiyun Health, Caring Church, and Master Fang – included over 20 disciplines in their apps. The most common disciplines were endocrinology (n = 34) and nutrition (n = 34), followed by cardiovascular medicine (n = 28), ophthalmology (n = 22), gastroenterology (n = 18), general surgery (n = 18), stomatology (n = 18), nephrology (n = 17), psychiatry (n = 11), rheumatology (n = 11), dermatology (n = 10), orthopedics (n = 10), respiratory medicine (n = 10), obstetrics and gynecology (n = 10), traditional Chinese medicine (n = 9), otorhinolaryngology (n = 8), oncology (n = 6), neurology (n = 5), urology (n = 5), infectious diseases (n = 7), pediatrics (n = 5), andrology (n = 4), anorectal (n = 4), neurosurgery (n = 3), internal medicine (n = 3), thoracic surgery (n = 3), emergency medicine (n = 2), hematology (n = 2), plastic surgery (n = 2), rehabilitation (n = 2), sexually transmitted diseases (n = 2), burns (n = 1), tuberculosis (n = 1), and critical care medicine (n = 1), among which some disciplines that seemed not directly related to diabetes were also presented.
Multidisciplinarity was most often reflected in the education and advising functions of the apps. Regarding the education function, 36 multidisciplinary apps (97%) provided various articles and videos generated by different disciplinary professionals to introduce diabetes and its risk factor and complication management knowledge and skills. Fifteen of the multidisciplinary apps (41%) provided advisory/therapy support that included professionals from multiple disciplinary backgrounds, among which 13 apps (87%) required payment for multidisciplinary consulting services. Multidisciplinary apps tended to have a higher comprehensiveness score than others (6.14 vs. 5.18, p = 0.0345).
Even for multidisciplinary apps, only a few apps (n = 4; 11%) involved multiple disciplines in the provision of any specific service, with most interdisciplinary apps having different disciplines work separately – resulting in a failure to integrate interdisciplinary perspectives. In providing educational information to empower the app users, many of the materials were generated by professionals from a single discipline or only contained information relevant to a single discipline. Regarding health data monitoring and analysis, although many apps allowed multidisciplinary data entering and sharing, the analysis and presentation of the analysis results were independent and not integrated. Similarly, when some apps contracted with professionals from different disciplines to provide consultation services to the app users, the professionals were usually working independently and providing recommendations without consulting professionals from other disciplines.
Discussion
This study reviews diabetes self-management apps in China, with a particular focus on describing the multisectoral and multidisciplinary efforts that had been made in mHealth care to provide effective, comprehensive, continuous care to patients with diabetes. Most of the 66 reviewed apps were solely designed for diabetes self-management, but only 3 apps were developed for specific types of diabetes management. Different types of diabetes require different prevention and treatment measures to fulfill the patients’ needs and improve the prognosis. The lack of specification of the diabetes types may lead to compromise in service quality, which is a significant shortage reflected among the reviewed apps.
The comprehensiveness of the reviewed apps is relatively low. Many key diabetes management functions (e.g., advising, reminding, interfacing, data sharing and analysis) and domains (e.g., lifestyle modification, medication, and complication management) are poorly addressed in existing app solutions. Future apps need to provide more comprehensive services, particularly covering lifestyle risks (especially smoking, alcohol use, psychosocial status, and salt intake), medication and complication management domains.
About 61% of the reviewed diabetes self-management apps were multisectoral, but the nature of this collaboration was limited by an overrepresentation of private sector partners, the underrepresentation of community -based public sector, a failure to engage civil society organizations (CSOs), and a lack of integration in collaboration. All reviewed apps were developed at least in part by private sector entities, the majority of which were medical device companies. While the private sector is a critical part of multisectoral collaboration, their overrepresentation risks an excessively profit-driven approach to diabetes management. For instance, apps developed by medical device companies usually restrict their apps to interface with their own devices and have built-in-app market that only sell devices from their own companies. Moreover, as observed, many companies failed to prioritize comprehensive, high-quality diabetes management by inadequately referring to scientific evidence and/or appropriate guidelines for diabetes management in their app and content development process.
Conversely, community stakeholders were only included by three apps—“Caring Church (关心堂)”, “Hui Health (慧健康)”, and “Shared Care (共同照护)”, which included community health centers as partners in app development or service provision. Primary health care, as the first contact with target population, provides the foundations of health equity and guarantee health service delivery. The involvement and collaboration of community-based healthcare entities with other sector entities via mobile health technologies is necessary and important in strengthening diabetes self-management. Future apps need to engage more community-level health sectors and provide them with a convenient platform for effectively collaborating with other sectors, in order to provide continuous, high-quality diabetes services to app users.
Likewise, the reviewed apps failed to engage civil society organizations (CSOs) in the apps. Increasing evidence has shown that CSOs could play important roles in NCDs prevention and control [23, 24]. In this review, only one app engaged a CSO, while almost all the identified sectors in the apps were public or private sector entities. More CSOs (e.g., academic institutions, non-profits, voluntary organizations, etc.) should be engaged in diabetes self-management apps to support evidence-based development, training and providing personnel, and other functions. Finally, the contributions of different sectors tend to be poorly integrated in the reviewed apps. Partners from different sectors tended to each contribute to specific app functions, while they did not meaningfully interact with each other to optimize the diabetes management functions and services in the apps. This reflects ongoing intersectoral fragmentation represented in the health care system. Robust collaboration mechanisms are needed to tackle this issue on the mobile platform.
Slightly more than half of the reviewed apps (n = 37, 56%) made use of a multidisciplinary approach, meaning that many apps on the Chinese market still failed to follow through the national guidelines and include tools essential for a comprehensive, holistic, and integrated approach to diabetes management. Beyond this general limitation, there are at least three limitations in the way that multidisciplinarity is handled in the existing apps: lack of comprehensive disciplinary coverage, limited applications, and lack of interaction. First, many of the existing apps excluding relevant expertise. Diabetes multidisciplinary care professionals could include general practitioners, endocrinologist, pediatrician, credentialled diabetes educator, dietitian, podiatrist, practice nurse, exercise physiologist, medical practitioners such as ophthalmologist and obstetrician, optometrist, psychologist, and/or social worker specialist [25]. In this review, disciplines that related to diabetes prevention and complications management were seldom presented in the apps. Moreover, there was lack of certified diabetes educator and social worker specialists engaged in mHealth care, which also reflected the significant shortage of the trained specialists in these fields in China. These may significantly comprise the capacity of the apps to provide comprehensive care for patients with diabetes. Second, multidisciplinary features were only presented in a few app functions like education and advising. More functioning potentials need to be explored in future to maximize the benefits of multidiscipline involvement in mHealth care. Third, similarly to the issue observed in multisectoral collaborations, there was a lack of close, robust collaborations between different disciplines in the apps. Increasing evidence has suggested the patients cared by multidisciplinary diabetes team containing physicians, pharmacists, nurses, and dieticians were more likely to result in better diabetes control (e.g., improved HbA1c, glucose, reduced complications) and reduction of diabetes-related expenditures [26,27,28,29]. Innovative collaboration mechanisms are needed to improve effective, robust interactions and collaborations between different disciplines in mHealth care for patients with diabetes.
Among the reviewed apps, one app named ‘Sugar Mama’ (糖妈妈) stood out in terms of its multisectoral and multidisciplinary endeavors. This app was designed and developed under the guidance of Anhui Provincial Health Commission and Anhui Provincial Obstetrics and Gynecology Quality Control Center, collaborating with local hospitals and private companies, to provide diabetes management education content and diagnosis and treatment services to gestational DM patients by an interdisciplinary care team comprised of obstetrician and gynecologist, endocrinologist, dietitian, exercise coach, insulin pump specialist, psychological counselor, and health manager. The involvement of the provincial government agencies as a public sector, which was rare among the existing diabetes apps, seemed to play an important role in coordinating the different sectors and establishing the standardized management platform for the target population. The robust collaborations between sectors and disciplines resulted in several significant advantages of the system, including the provision of one-on-one comprehensive assessment and consultation services, the development of evidence-based individualized gestational diabetes management plan, and the effective integration of the in- and out-of-hospital gestational DM management by linking the app system to the provincial standardized diabetes patient management service platform and allowing sharing information and resources between different sectors and disciplines. More apps like this are needed in future to deliver innovative, high- quality services to the large number of patients with diabetes in China. Meanwhile, future research are needed to evaluate the user experience and their diabetes management outcomes using this kind of multisectoral and multidisciplinary apps.
This review study, to the authors’ knowledge, is among the first few to examine the multisectoral and multidisciplinary features in diabetes self-management apps in China. Moreover, international and national guidance were referred for sector, discipline and domain analysis, which could make the findings of this study more comparable to other studies. There are several limitations of the current study. First, only Xiaomi, Vivo, iPhone, and Honor smartphone app stores were searched for eligible apps in this study, which could introduce potential bias to the study by excluding other apps sources in Chinese market. Second, many apps provided in-app payment opportunities to provide more advanced services. The findings from this study were based on the review of the basic services of the apps, which may result in missing certain features of the apps. Third, when reviewing the multisectoral and multidisciplinary features of the apps, it was challenging to clearly define the features and determine the collaborations and the roles of different sectors and disciplines. This is because there has not existed a clear criterion as a reference, which may create space for reviewers’ subjective judgement and lead to potential bias.
Conclusions
This study revealed that the integration of multidisciplinary and multisectoral features in diabetes-self management apps on the Chinese market has notable limitations. The presence of these limitations indicates an important guidance for LMICs hoping to develop mHealth tools for effective diabetes management. First, relying on private entities to lead the development results in predominantly market-oriented apps, in which business development goals may compete with medical ones, and result in narrow set of stakeholders, which may reduce the ability of such applications to coordinate care at the scale required for effective diabetes management in LMICs. Moreover, CSOs and community groups were often excluded, which may result in a ‘top-down’ design which fails to engage patient interests. Diabetes self-management app development should better engage public sector and civil society entities, like research institutions and professional associations, to reduce bias introduced by the private sector entities and improve the app quality for diabetes management. Second, the available diabetes self-management apps reproduce ongoing intersectoral fragmentation of the health care system. Careful effort will be needed to overcome these obstacles and create innovative ways to engage and integrate different sectors and disciplines at different levels in mHealth care. Third, there is lack of well-developed guidance and framework to evaluate the multisectoral and multidisciplinary features, especially for collaborative mechanisms, in diabetes management mHealth apps. Future studies are needed to develop such evaluation frameworks and evaluate the effectiveness of the multisectoral and multidisciplinary apps on diabetes control in LMICs.
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
- LMICs:
-
Low- and middle-income countries
- DALYs:
-
Disability-adjusted life years
- WHO:
-
World Health Organization
- IDT:
-
Interdisciplinary team
- HbA1c:
-
Hemoglobin A1C
- CSOs:
-
Civil society organizations
- NCDs:
-
Non-communicable diseases
References
IDF Diabetes Atlas. 10th ed. https://diabetesatlas.org/atlas/tenth-edition/.
Liu J, Bai R, Chai Z, Cooper ME, Zimmet PZ, Zhang L. Low- and middle-income countries demonstrate rapid growth of type 2 diabetes: an analysis based on Global Burden of Disease 1990–2019 data. Diabetologia. 2022;65(8):1339–52.
Organization WH. Global action plan for the prevention and con-trol of NCDs 2013–2020. 2014.
World Health Organization. Toolkit for developing a multisectoral action plan for noncommunicable diseases: overview. Geneva: World Health Organization; 2022.
Bailey CJ, Aschner P, Del Prato S, LaSalle J, Ji L, Matthaei S, Management GPfED. Individualized glycaemic targets and pharmacotherapy in type 2 diabetes. Diab Vasc Dis Res. 2013;10(5):397–409.
El-Khatib Z, Shah M, Zallappa SN, Nabeth P, Guerra J, Manengu CT, Yao M, Philibert A, Massina L, Staiger CP, et al. SMS-based smartphone application for disease surveillance has doubled completeness and timeliness in a limited-resource setting - evaluation of a 15-week pilot program in Central African Republic (CAR) 11 medical and health sciences 1117 public health and. Confl Health. 2018;12:1–11.
Agarwal S, Perry HB, Long LA, Labrique AB. Evidence on feasibility and effective use of mHealth strategies by frontline health workers in developing countries: systematic review. Trop Med Int Health. 2015;20(8):1003–14.
Yang Y, Lee EY, Kim H-S, Lee SH, Yoon KH, Cho JH. Effect of a mobile phone-based glucose-monitoring and feedback system for type 2 diabetes management in multiple primary care clinic settings: cluster randomized controlled trial. JMIR Mhealth Uhealth. 2020;8(2):e16266.
Kebede MM, Pischke CR. Popular diabetes apps and the impact of diabetes app use on self-care behaviour: a survey among the digital community of persons with diabetes on social media. Front Endocrinol (Lausanne). 2019;10:135.
Brew-Sam N, Chib A, Rossmann C. Differential influences of social support on app use for diabetes self-management - a mixed methods approach. BMC Med Inform Decis Mak. 2020;20(1):151–151.
Wang L, Peng W, Zhao Z, Zhang M, Shi Z, Song Z, Zhang X, Li C, Huang Z, Sun X. Prevalence and treatment of diabetes in China, 2013–2018. JAMA. 2021;326(24):2498–506.
Zhou B, Lu Y, Hajifathalian K, Bentham J, Di Cesare M, Danaei G, Bixby H, Cowan MJ, Ali MK, Taddei C. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4· 4 million participants. Lancet. 2016;387(10027):1513–30.
Group NDR. A mass survey of diabetes mellitus in a population of 300,000 in 14 provinces and municipalities in China. Zhonghua Nei Ke Za Zhi. 1981;20(11):678–83.
Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, Malanda B. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81.
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, Stein C, Basit A, Chan JC, Mbanya JC. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119.
Yao M, Zhang DY, Fan JT, Lin K, Haroon S, Jackson D, Li H, Chen W, Lehman R, Cheng KK. The experiences of Chinese general practitioners in communicating with people with type 2 diabetes—a focus group study. BMC Fam Pract. 2021;22(1):156.
Sun M, Rasooly A, Fan X, Jian W. Assessing the quality of primary healthcare for diabetes in China: multivariate analysis using the China Health and Retirement Longitudinal Study (CHARLS) Database. BMJ Open. 2020;10(12):e035192.
Huang J. Insights into: Asia’s top mobile markets (China, Korea, Japan). Amsterdam: Newzoo International B.V.; 2019.
China Smartphone Shipments Market Data (Q3 2021 – Q4 2022). https://www.counterpointresearch.com/china-smartphone-share/.
Arnhold M, Quade M, Kirch W. Mobile Applications for diabetics: a systematic review and expert-based usability evaluation considering the special requirements of diabetes patients age 50 years or older. J Med Internet Res. 2014;16(4):e104.
中华医学会糖尿病学分会 国: 国家基层糖尿病防治管理指南 (2022). 中华内科杂志 2022;61(3):249–262.
Chinese Ministry of Health. Directory of diagnostic and treatment subjects in medical institutions. Regulatory Department; 2018. Available at http://www.nhc.gov.cn/fzs/s3576/201808/345269bd570b47e7aef9a60f5d17db97.shtml.
Allen N, Cherlin E, Wong R, Mantopoulos J, de la Peza L. Evaluating leadership, management, and governance capacity building in Rwanda in role of universities in strengthening health systems in low-income settings. Ann Glob Health. 235.
Organization WH. Report of the South-East Asia Regional Meeting on Strengthening NCD Civil Society Organizations. Amsterdam: WHO Regional Office for South-East Asia; 2015.
Multidisciplinary diabetes care. https://www.adea.com.au/for-health-professionals/the-diabetes-team/multidisciplinary-diabetes-care/#:~:text=Multidisciplinary%20diabetes%20care%20is%20a,for%20the%20person%20with%20diabetes.
Joret MO, Osman K, Dean A, Cao C, van der Werf B, Bhamidipaty V. Multidisciplinary clinics reduce treatment costs and improve patient outcomes in diabetic foot disease. J Vasc Surg. 2019;70(3):806–14.
Jiao F, Fung CSC, Wan YF, McGhee SM, Wong CKH, Dai D, Kwok R, Lam CLK. Long-term effects of the multidisciplinary risk assessment and management program for patients with diabetes mellitus (RAMP-DM): a population-based cohort study. Cardiovasc Diabetol. 2015;14:1–11.
Foster D, Sanchez-Collins S, Cheskin LJ. Multidisciplinary team–based obesity treatment in patients with diabetes: current practices and the state of the science. Diabetes Spectrum. 2017;30(4):244–9.
McGill M, Blonde L, Chan JC, Khunti K, Lavalle FJ, Bailey CJ. The interdisciplinary team in type 2 diabetes management: challenges and best practice solutions from real-world scenarios. J Clin Transl Endocrinol. 2017;7:21–7.
Acknowledgements
Thanks to the DKU Global Health Research Center for support the project.
Funding
The research results of this article (or publication) are sponsored by the Kunshan Municipal Government research funding. The funder played no other role in the production of this research.
Author information
Authors and Affiliations
Contributions
MC conceptualized and designed the study, acquired funding, conducted the investigation, analyzed and validated the data, drafted and edited the manuscript, and supervised the project; DEW interpreted the results, and drafted and edited the manuscript. CL, DL, and ZW conducted data curation and analysis, and drafted the manuscript. LZ edited the manuscript and acquired funding for the project. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix A.
Usability Scores of the Reviewed Diabetes Self-Management Apps (N=66). Appendix B. Comprehensiveness of the Reviewed Diabetes Self-Managed Apps (N=66).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, M., Weissglass, D., Li, C. et al. A multisectoral and multidisciplinary endeavor: a review of diabetes self-management apps in China. BMC Public Health 23, 1859 (2023). https://doi.org/10.1186/s12889-023-16735-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-16735-z