Abstract
Background
Vaccination efforts are a vital part of controlling the spread of diseases, however, lack of vaccine acceptance undermines the efficacy of this public health effort. Current evidence suggests that the most effective interventions to support vaccination uptake and positive vaccination beliefs are multicomponent, and dialogue based. Peer-based education interventions are such a strategy that involves an individual within the same group to act as the vaccine educator.
Objective
This review aims to consolidate the quantitative evidence surrounding the effectiveness and experience of peer-based education initiatives to improve vaccination beliefs and behaviors.
Methods
We conducted a systematic search of PubMed, Web of Science, and a hand reference search. The search was conducted between April and June 2022. The inclusion criteria encompassed using peers, being education based, and being an intervention that addresses vaccination beliefs and behaviors (e.g. vaccination uptake).
Results
Systematic screening revealed 16 articles in the final review. Half of the studies focused on students as their study population. The human papillomavirus vaccine was the most common vaccine assessed in the studies, followed by COVID and influenza vaccines. 11 out of 16 of the articles reported a positive impact of the peer intervention and two studies had mixed results. Six studies suggest a mixed peer- healthcare expert approach.
Conclusions
Despite reported positive effects of using peer-education based initiatives to improve vaccine uptake and beliefs, this systematic review reveals that there is limited existing research in support of this strategy. The strategies that initially appear the most effect are those with a combined peer and health-expert approach, and those that have more group specific and long-term peer interventions. More research is needed to confirm these results and to assess the effectiveness of a peer-based education intervention in a wider variety of settings and for other vaccine types.
Similar content being viewed by others
Introduction
Vaccines are indispensable for reducing disease morbidity and mortality. Low vaccine uptake and limited confidence in vaccines harms this endeavor [1]. The COVID-19 pandemic illustrated this problem. Based on surveys of general public opinions, rates of COVID-19 vaccine acceptance vary from 97.0% in Ecuador to as low as 23.6% in Kuwait [2]. While the rates of COVID-19 vaccine uptake have been making headlines, limited confidence in vaccines is a well-established phenomenon that applies to almost all vaccines [1]. This topic has been widely discussed within the vaccine hesitancy literature.
Vaccine hesitancy is a complex phenomenon that MacDonald (2015) described as the delay in acceptance or refusal of vaccines despite availability of vaccination services [3]. This definition has been challenged by H Larson (2022), M Goldberg (2021), and Bussink-Voorend et al. (2022) who propose that vaccine hesitancy should be defined as “a state of indecisiveness regarding a vaccination decision” [4,5,6]. Whilst MacDonald defines vaccine hesitancy as a behavior, the latter highlight it as a process of decision making [3]. Much research focuses on vaccine confidence or vaccine acceptance as more tangible and positive approaches [7]. Scholars have formulated a vaccine hesitancy determinants matrix that includes contextual influences, individual and group influences, and vaccine specific issues [3]. Overcoming these complex, historical, political and socio-cultural factors is not a simple task, and addressing them requires various interventions [8]. This systematic review includes studies that focus on vaccine hesitancy, vaccine acceptance, vaccine knowledge and beliefs, vaccine confidence and vaccination uptake. We recognize the diversity within these definitions and concepts, and the limits of them to fully capture vaccine knowledge, beliefs, and behavior. For the purpose of this review, we refer to vaccine beliefs and uptake to capture a broad range of widely discussed definitions.
Peer-based education interventions are refined and population specific interventions with the potential to increase vaccine uptake [9,10,11]. This strategy allows for improved cultural competencies taking into account many sociocultural and population characteristic factors [10, 11]. Prior studies have shown the benefits of peer-based interventions for improving other health behaviors [12, 13]. However, despite the mention of peer-based education in several reviews of vaccine beliefs and uptake[9, 10] to our knowledge, there is no comprehensive review of the effectiveness of and experience with peer-based education interventions for vaccination. Jama et al. postulate that peer-to-peer interventions could be a strategy for overcoming some of the barriers to vaccine uptake as the peers can lead by example and act as vaccine ambassadors [14]. There is also some evidence to show that peers in community-based intervention can improve vaccine coverage [15, 16]. This review aims to summarize the quantitative evidence surrounding the effectiveness and experience of peer-education initiatives that have been implemented.
Methods
Search strategy
For the systematic review, we conducted searches of Web of Science and PubMed. The review search was conducted between April and June 2022, then again in June 2023. We ran the searches with all of the combined search terms using the Boolean Operators. For Web of Science, all terms were searched with the ALL category, and for PubMed the advanced search setting was used with All fields. The search terms used for both databases were (Vaccine), (Vaccin*), (Vaccine hesitancy), (vaccine confidence), (vaccine coverage), (vaccination refusal), (vaccine-preventable diseases), (immunization), (peer education initiatives), (peer group*), (peer education), (Peer-to-peer), (peer-to-peer support), (peer), (health education), (vaccin* education), (education*), (Health knowledge, attitudes, practices), (patient education), (intervention). In addition, to the database searching, a hand search of article references was conducted. In relevant systematic reviews and pertinent articles, a researcher did an initial screening of the references to find other articles for inclusion. From the results of the database search, we first did a duplicate deletion using the EndNote software [17]. Then two members of the research team determined inclusion for the screening process. Two members of the team screened the articles that were sought for retrieval.
In the literature there is no single definition of a peer-based education intervention. For the purpose of this study, we define a peer as individuals with key shared characteristics, circumstance or experiences, and who do not have professional training [18]. Simoni et al. (2011) make a distinction between a peer intervener who acts to improve health behavior and has shared characteristics, rather than the colloquial peer as someone with equal standing [18]. For the purpose of this paper, “peer” will mean a “peer intervener.” In the case of a peer-based health intervention, they frequently collaborate with more qualified service providers [18]. Peer’s roles might include advocating, connecting people to resources, conveying information, and offering assistance [18]. Further, the majority of peer-based interventions include some kind of educational delivery. The core idea is that peer education is responsive to the values and objectives of the target group [18]. Peer-based education interventions allow for an individual affected by the same disease or among the same social group to provide vaccine and health information to peers in a more culturally or socially relevant manner than a health educator or provider [19, 20].
The guiding criteria for inclusion was that the articles need to have a peer-based education intervention on vaccination uptake and beliefs. Articles included had the term peer described above [18]. We defined an education intervention as an effort to improve knowledge or awareness on vaccination by providing some type of education via lecture, paper or digital information, tabling event, group meetings, or other means [18, 21]. We included articles that assessed an intervention that focused on addressing vaccination uptake and beliefs as their outcomes. This includes articles that addressed vaccine uptake, willingness-to-vaccine, vaccine hesitancy, and measuring knowledge and beliefs of vaccines.
Each screener assigned the article with a level; definitely fits, probably fits, most likely does not fit, and most likely excluded. This was a self-developed screening tool to guide the screening process. The articles screened as definitely fits and most likely excluded by both screeners were then directly included or excluded. Then based on discussion and input from a third member of the team, articles in probably fits or most likely does not fit were determined for inclusion [17, 21]. Having two options in the middle allowed for the researchers to have more nuance in identifying the article’s likelihood of inclusion and assisted with the conversations with the third team member.
In June 2023, the search was rerun on both PubMed and Web of Science to check for articles published in the year since the initial search. The same search terms and inclusion/exclusion criteria were utilized. On PubMed, the filter of article published last year was used to assess for new articles, and for Web of Science the filter for articles published in 2022 or 2023 was used.
Data extraction and data analysis
For the data extraction, we modified a standardized systematic review extraction form [22]. One researcher conducted the extraction, and a second researcher double-checked the extraction results. Any discrepancies in data extraction were discussed among the authors and adjustments were made based on agreed upon reading or interpretation of the articles.
Quality assessment
We utilized the Effective Public Health Practice Project quality assessment tool for quantitative studies to assess all included articles for their quality [23]. Articles were scored as 1 – Strong, 2 – Moderate, 3 – Weak based on assessment of study design, methods used, biases, and more (Additional file 1)[23]. Two researchers conducted the quality assessment and then matched the two scores. Our average quality score was 1.63 (Table 1) [22]. This indicates that there was a a moderate quality of research papers presented in this review. Overall, the many aspects of the study designs and testing were of high quality, but due to the nature of the interventions often participant randomization or blinding were not conducted [23].
Results
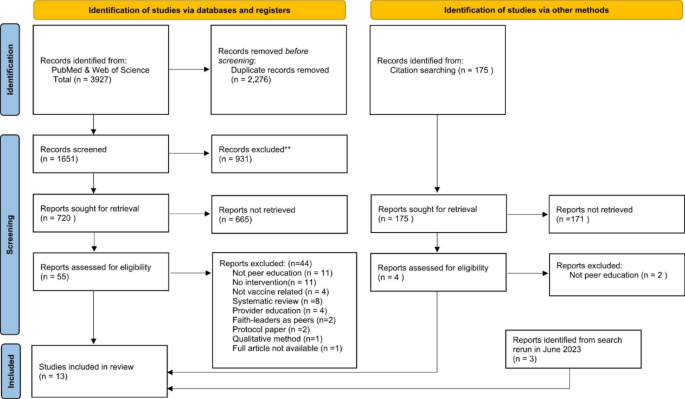
The systematic review revealed 3927 articles from PubMed and Web of Science, and 175 from citation searching (Fig. 1). After removing duplicates, and screening for eligibility, 11 articles were included from database searching. In addition, two eligible articles from citation searching and three articles from the June 2023 search rerun were identified making a total of 16 eligible articles included in this review. One article was excluded due to inability to access the full article.
PRISMA flow diagram of systematic review. Strategy PRISMA 2020 flow diagram for new systematic reviews which included searches of databases, registers and other sources From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: https://doi.org/10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/
Table 1 summarizes all of the results. For the study populations, eight articles studied students, four of which focused on women, two studied senior citizens, and six studied other populations (parents, Japanese general population, gay men, essential workers, and the Diné/Navajo). Studies took place in five different countries with 11 in the United States, two in Poland, and one study in Japan, Scotland, and Nigeria. The vaccines assessed were COVID-19 (six), followed by HPV (human papilloma virus) (five), influenza (three), then childhood vaccination (one), and hepatis B virus (one). The various study methods utilized in the articles were surveys (seven), randomized control trials (six), population vaccination rate (two), and mixed methods with surveys and interviews (one).
The studies covered a variety of primary outcome measures as a strategy to assess a peer education-based intervention for vaccine beliefs and outcomes. Five of them measured a change in vaccination rate [24,25,26,27,28], four collected vaccination uptake rates [29,30,31,32], three gathered willingness to vaccinate [33,34,35], another three surveyed the knowledge and beliefs of participants [36,37,38], and one study assessed the satisfaction with the intervention [39]. Overall, 13 of 16 studies reported a positive impact of the peer intervention, in the studies’ outcome measure [24,25,26,27,28, 31, 33,34,35,36,37,38,39]. A positive impact could mean improved knowledge or intention to vaccine or improved vaccination rates or uptake of vaccines. Three studies had mixed results with some results showing improvement, but some outcomes not being statistically significant [30, 32, 40]. Six out of the 16 studies utilized or suggest a mixed peer and healthcare expert approach [25, 28, 31, 33, 36, 38,39,40].
The different intervention strategies used were grouped into a quick chat with a peer [6], a workshop/lecture approach [5], a narrative- onetime approach [3], and repeated contact with a peer [2]. The interventions utilizing a quick chat with a peer strategy involved peer education tables or promotions [26, 30], having peers provide information and support during an immunization clinic [27, 28, 31], and peer phone-calls to unvaccinated individuals [24]. Even though this was the least intensive intervention strategy, five studies had a positive impact on vaccination with increased vaccination rates compared with baselines [24, 26,27,28, 31]. Several other studies used a one-time workshop or lecture by peers to provide information on vaccination[34, 36,37,38, 40]. These mostly involved a peer training by public health professionals and then an educational session. All studies, except one [40], had positive impact on either knowledge and beliefs or willingness to vaccinate. The Fenick, et al. study had a mixed impact, but utilized a slightly different intervention strategy with group wellness visits with parents to encourage peer support for childhood vaccination [40]. Three studies used a narrative-onetime approach that had peer-based messaging provided online and assessed the impact on willingness to vaccinate, all of which had a positive impact [33, 35, 39]. Lastly, two studies used more intensives strategy with repeated peer contact. One was via a two-month long programing among seniors [25], and one had a peer led Facebook group among essential workers [32]. Both studies had an increase in vaccination uptake or interest in vaccination information.
Several studies (nine) showed improvements in the uptake of vaccines [24,25,26,27,28, 31, 33, 34, 38] [33]. In an intervention at a senior living center the immunization rates for influenza and pneumococcal rose by a greater percentage for those in the intervention building than the control over the two years [24]. Similarly, in a population of low income and minority adults with a repeated peer multilevel participatory intervention there was a 40.6% increase in the intervention group compared with only an 18% increase in the control group [25]. A narrative intervention to improve HPV knowledge and vaccination in college aged women, found that the combined peer and health expert intervention had a nearly double rate of HPV vaccination at two months compared with the control [39]. In a study that utilized peer ambassadors at same-day COVID-19 vaccination clinics, 197 more individuals were vaccinated at centers with peers compared with those without peers [31].
Peer intervention also appears to improve knowledge and intention to vaccinate. In a study of students regarding COVID-19, the intervention had a slight increased willingness to vaccinate from 31.8 to 35.2% [34]. After receiving messaging on HPV by trained students, female adolescence in Nigeria mean knowledge score increased from 12.94 to 53.74 [37]. Unlike the other studies, these two focused on vaccine knowledge and beliefs, rather than changes in vaccination uptake.
Some studies found a mixed result. In a study with a group-based general wellness checkup visit, compared with regular individual visits, they found that there was no difference between the two groups in terms of vaccination timeliness at 2 and 4 months. However, the infants were more likely to be immunized on schedule at 6 months and 12 months, and to attend all 6 visits [40]. A study conducted at a university among Chinese international students found limited knowledge levels on HPV, but 94.9% were interested in receiving the vaccine [28]. However, of the first 400 students educated only 80 actually visited the health center for vaccination [28]. Therefore, whilst the education was arguably successful, it did not lead to significant uptake of the HPV vaccine.
Discussion
This systematic review of peer-education based interventions to improve vaccine uptake and beliefs revealed several benefits of peer-based interventions. Thirteen studies illustrated some positive effect of the peer-based education intervention on the intended outcomes [24,25,26,27,28, 33,34,35,36,37, 39]. This shows that the peer-education based interventions could be a useful tool for improving vaccine uptake and beliefs. Of the 13 studies reporting a positive effect, six combined the peer-based education intervention with a health expert intervention. The studies that were using mixed approaches demonstrated a stronger impact on their outcomes, than studies that only used one intervention type [25, 28, 33, 36, 39, 40]. Thus, future studies or interventions should consider using the potential benefits of utilizing a combination health expert and peers’ approach to encourage vaccination.
Furthermore, the different specific intervention strategies appear to affect the efficacy of the intervention. Although unable to directly compare results, there are some trends that can be seen in the review. Studies that only provided a quick chat with a peer intervener through tabling or a bar intervention seem to have the weakest impact on vaccination and vaccine knowledge [26,27,28, 30, 31, 35]. However, those at universities are more successful than others [27, 28]. The one-time workshop interventions seem to have some limited success in improving vaccine knowledge [34, 36]. The one-time narrative approaches seem be even a bit more effective in improving knowledge [37,38,39], and one even reported doubling the HPV vaccination rate among students receiving the intervention [33]. The two studies with repeated peer interventions had statistically significant increases in vaccination rates, indicating the strength of this strategy [25, 32]. This indicates that a more targeted and repeated approach, appear to have more potential than more generic, one-time interventions.
It is important to note that the peer education interventions presented in these studies were mostly used to encourage vaccination rather than to address vaccinate hesitancy or refusal. Seven of the studies focused on improving vaccine uptake or a change in vaccination rates among groups that were not yet vaccinated such as international students, children, or seniors [24,25,26,27,28, 32, 40]. Thus, the peer-based interventions show a generally positive effect on vaccine uptake and beliefs, but apart from one paper, - on the Diné (Navajo) population which is known to be vaccinate hesitant rooted in governmental mistrust [34] - there was no research on the effectiveness of peer-based educational interventions in communities that present low levels of vaccine confidence. This suggests that there is limited evidence for the use of peer- based interventions to address vaccine hesitancy, which is rooted in specific communities for example, migrant communities, anthroposophic or religious communities, or online communities.
Limitations
There are limitations to the generalizability of these results to diverse range of population groups and vaccine types. The scope of the results is also restricted as only one study took place in a middle-income country [37], none in a low-income country, and the majority were set in the United States [24, 25, 27, 28, 30,31,32,33, 38,39,40]. Several United States-based studies (ten) demonstrated a positive impact, pointing to encouraging benefits of a peer intervention in a high-income setting amongst adults [24, 25, 27, 28, 31,32,33, 38,39,40]. However, the limited geographic scope curtails the generalizability of the evidence found in the systematic review. One study in Nigeria showed promising results with an illustrated improvement in awareness and knowledge regarding the HPV vaccine and cervical cancer. The study did not explore the impact on HPV uptake; thus, the effect remains poorly understood [37]. To understand the potential of peer-based education initiatives for different areas it is necessary to conduct more research in economically and geographically diverse regions.
Additionally, more long-term studies may be required to assess the sustainability of effects of peer-based education intervention. For example, two studies demonstrate the effects of a peer-education on either knowledge or vaccination rates for up to one year [24, 40]. For some vaccines that require a repeated yearly dosage, such as influenza, it may be pertinent to assess the effects of peer-based education interventions for more long-term sustainability.
There are several limitations to this systematic review. Publication bias could be a limitation of the results. We found no articles with a negative outcome. Research with less favorable results could have been conducted but not published. Some studies also could have been missed due to the utilization of different terminology other than peer. The quality of the studies found was mixed. One consistent issue throughout the studies was the inability to blind the participants due to the nature of the interventions. We also had to exclude one article due to an inability to access the full article.
Recommendations
Based on the limitations of the results, we recommend further research to examine the full benefits of a peer-based education approach, particularly for different population groups (not only adults), vaccination types (particularly childhood vaccines), and geographical regions (particularly in low-income settings). Given that we found that the benefits of peer-based education intervention to address vaccine beliefs and uptake are inconclusive, we recommend further studies that apply strong methods such as randomized controlled trial. This would provide greater generalizability of the results and provide clearer guidance for policy making for public health promotion. A peer-based intervention may work better in certain setting than in others, but the positive nature of the results implies that the strategy should be proliferated more in research and interventions [8]. More studies into peer-based interventions with known vaccine hesitant populations would be useful to determine if they are useful for addressing specific vaccine fears or rumors and not just for encouraging vaccination. Also, conducting a randomized controlled trial comparing the effects of a single peer-based and a combined (health expert and peer) would be beneficial for strengthening the findings.
Conclusion
In conclusion, there is limited existing research on peer-based education interventions to improve vaccine beliefs and uptake. The research that exists illustrates the promise of this approach for certain vaccines and populations. To fully assess the effectiveness of peer-based education further research into this strategy for different peer groups, in different parts of the world, and using different methodological approaches is required. Importantly, further research must examine peer-based education interventions in vaccine hesitant communities [8]. Implementing vaccine education by peers could help to address socio-cultural barriers through a culturally competent addition to traditional vaccine interventions. Whilst the claim of the value of peer-based education system continues to be made in the literature, more solid evidence on best approaches is needed.
Data Availability
The datasets used and/or analysed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- HPV:
-
Human Papillomavirus
References
Ali KA, Celentano LP, ADDRESSING VACCINE HESITANCY, IN THE “POST-TRUTH” ERA. Eurohealth Int Eurohealth. 2017;23(4).
Sallam M. COVID-19 Vaccine Hesitancy Worldwide: a concise systematic review of Vaccine Acceptance Rates. Vaccines (Basel). 2021 Feb 16;9(2):160.
MacDonald NE, SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015 Aug;33(34):4161–4.
Larson HJ, Schulz WS, Tucker JD, Smith DMD. Measuring Vaccine Confidence: Introducing a Global Vaccine Confidence Index. PLoS Curr [Internet]. 2015 Feb 25 [cited 2023 Jul 4];7(OUTBREAKS). Available from: /pmc/articles/PMC4353663/.
Bussink-Voorend D, Hautvast JLA, Vandeberg L, Visser O, Hulscher MEJL. A systematic literature review to clarify the concept of vaccine hesitancy. Nat Hum Behav [Internet]. 2022 Dec 1 [cited 2023 Jul 4];6(12):1634–48. Available from: https://pubmed.ncbi.nlm.nih.gov/35995837/.
Goldenberg MJ. Vaccine hesitancy - Public Trust, Expertise and the War on Scince. Universty of Pittsburgh Press; 2021.
Dubé È, Ward JK, Verger P, Macdonald NE. Vaccine Hesitancy, Acceptance, and Anti-Vaccination: Trends and Future Prospects for Public Health. Annu Rev Public Health [Internet]. 2021 [cited 2023 Jul 4];42:175–91. Available from: https://doi.org/10.1146/annurev-publhealth.
Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy. http://dx.doi.org/104161/hv24657 [Internet]. 2013 Aug [cited 2023 Mar 5];9(8):1763–73. Available from: https://www.tandfonline.com/doi/abs/10.4161/hv.24657.
Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ, Eskola J, et al. Strategies for addressing vaccine hesitancy - A systematic review. Volume 33. Vaccine: Elsevier Ltd; 2015. pp. 4180–90.
Shon EJ, Choe S, Lee L, Ki Y, Influenza Vaccination Among US. College or University students: a systematic review. Am J Health Promotion 2021 Jun 3;35(5):708–19.
Abahussin AA, Albarrak AI. Vaccination adherence: review and proposed model. J Infect Public Health 2016 Nov 1;9(6):781–9.
Posavac EJ, Kattapong KR, Dew DE. Peer-Based Interventions to Influence Health-Related Behaviors and Attitudes: A Meta-Analysis. http://dx.doi.org/102466/pr01999853f1179 [Internet]. 2016 Sep 1 [cited 2023 Mar 5];85(3 PART 2):1179–94. Available from: https://journals.sagepub.com/doi/10.2466/pr0.1999.85.3 f.1179?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub++0pubmed.
Webel AR, Okonsky J, Trompeta J, Holzerner WL. A systematic review of the effectiveness of peer-based interventions on health-related behaviors in adults. Am J Public Health [Internet]. 2010 Feb 1 [cited 2023 Mar 5];100(2):247–53. Available from: https://doi.org/10.2105/AJPH.2008.149419.
Jama A, Appelqvist E, Kulane A, Karregård S, Rubin J, Nejat S et al. Design and implementation of tailored intervention to increase vaccine acceptance in a Somali community in Stockholm, Sweden - based on the Tailoring Immunization Programmes approach. Public Health in Practice. 2022 Dec 1;4:100305.
Findley SE, Irigoyen M, Sanchez M, Stockwell MS, Mejia M, Guzman L et al. Effectiveness of a Community Coalition for Improving Child Vaccination Rates in New York City. Am J Public Health [Internet]. 2008 Nov 1 [cited 2023 Mar 13];98(11):1959. Available from: /pmc/articles/PMC2636428/.
Findley SE, Irigoyen M, Sanchez M, Guzman L, Mejia M, Sajous M et al. Community-based strategies to reduce childhood immunization disparities. Health Promot Pract. 2006 Jul;7(3 Suppl).
EndNote. EndNote [Internet]. [cited 2023 Mar 13]. Available from: https://www.myendnoteweb.com/EndNoteWeb.html.
Simoni JM, Franks JC, Lehavot K, Yard SS. Peer interventions to promote health: conceptual considerations. Am J Orthopsychiatry. 2011;81(3):351–9.
Ramchand R, Ahluwalia SC, Xenakis L, Apaydin E, Raaen L, Grimm G. A systematic review of peer-supported interventions for health promotion and disease prevention. Prev Med (Baltim). 2017 Aug;1:101:156–70.
Nelson KM, Yang JP, Molina Y, Simoni JM. Peer-Based Intervention Approaches. Encyclopedia of AIDS [Internet]. 2014 [cited 2023 Mar 5];1–4. Available from: https://link.springer.com/referenceworkentry/10.1007/978-1-4614-9610-6_94-1.
Abdi F, Simbar M. The Peer Education Approach in Adolescents- Narrative Review Article. Iran J Public Health [Internet]. 2013 [cited 2023 Mar 8];42(11):1200. Available from: /pmc/articles/PMC4499060/.
Emily Jones MA, UNC Health Science Library. 2023 [cited 2023 Mar 8]. LibGuides: Systematic Reviews: Step 7: Extract Data from Included Studies. Available from: https://guides.lib.unc.edu/systematic-reviews/extract-data.
Effective Public Healthcare Panacea Project. EPHPP. 2023 [cited 2023 Mar 6]. Quality Assessment Tool for Quantitative Studies. Available from: https://www.ephpp.ca/quality-assessment-tool-for-quantitative-studies/.
Krieger JW, Castorina JS, Walls ML, Weaver MR, Ciske S. Increasing Influenza and Pneumococcal Immunization Rates: a randomized controlled study of a senior Center-Based intervention. Am J Prev Med. 2000.
Schensul JJ, Radda K, Coman E, Vazquez E. Multi-level intervention to prevent influenza infections in older low income and minority adults. In: Am J Community Psychol. 2009. p. 313–29.
Flowers P, Hart GJ, Williamson LM, Ba F, Der Bsc GJ. Does bar-based, peer-led sexual health promotion have a community-level effect amongst gay men in Scotland? Int J STD AIDS. 2002;13:102–8.
Huang JJ, Francesconi M, Cooper MH, Covello A, Guo M, Gharib SD. Community health workers on a college campus: Effects on influenza vaccination. J Am Coll Health. 2018 May;19(4):317–23.
Long AG, Roberts CM, Hayney MS. Pharmacy student involvement with increasing human papillomavirus (HPV) vaccination among international college students. J Am Pharmacists Association. 2017 Jan;57(1):127–8.
Fenick AM, Leventhal JM, Gilliam W, Rosenthal MS. A randomized controlled trial of Group Well-Child Care: Improved Attendance and Vaccination Timeliness. Clin Pediatr (Phila). 2020 Jun 1;59(7):686–91.
Esagoff A, Cohen S, Chang G, Equils O, Sarah ;, Orman V et al. 2531. Using peer-to-peer education to increase awareness and uptake of HPV Vaccine among Chinese International Students. Open Forum Infectious Disease. 2022.
Shover CL, Rosen A, Mata J, Robie B, Alvarado J, Frederes A et al. Engaging Same-Day Peer Ambassadors to Increase Coronavirus Disease 2019 Vaccination Among People Experiencing Unsheltered Homelessness in Los Angeles County: A Hybrid Feasibility-Evaluation Study. 2019 [cited 2023 Jun 27]; Available from: https://doi.org/10.1093/infdis/jiac291.
Ugarte DA, Young S. Effects of an Online Community Peer-support Intervention on COVID-19 Vaccine Misinformation Among Essential Workers: Mixed-methods Analysis. Western Journal of Emergency Medicine [Internet]. 2023 [cited 2023 Jun 27];264(2). Available from: http://escholarship.org/uc/uciem_westjem.
Hopfer S. Effects of a narrative HPV vaccination intervention aimed at reaching College Women: a Randomized Controlled Trial. Prev Sci. 2012 Apr;13(2):173–82.
Pasek O, Michalska J, Piechowicz M, Stoliński M, Ganczak M. Effect of peer-education on willingness to vaccinate against COVID-19 among high school students. European Public Health Conference. 2021.
Sasaki S, Saito T, Ohtake F. Nudges for COVID-19 voluntary vaccination: how to explain peer information? Soc Sci Med. 2022 Jan 1;292.
Ganczak M, Pasek O, Duda-Duma Ł, Komorzycka J, Nowak K, Korzeń M. A peer-based educational intervention effects on SARS-CoV-2 knowledge and attitudes among polish high-school students. Int J Environ Res Public Health. 2021 Nov 1;18(22).
Sadoh AE, Okonkwo C, Nwaneri DU, Ogboghodo BC, Eregie C, Oviawe O, et al. Effect of peer education on knowledge of human papilloma virus and cervical cancer among female adolescent students in Benin city, Nigeria. Ann Glob Health. 2018;84(1):121–8.
Tutt M, Begay C, George S, Dickerson C, Kahn C, Bauer M et al. Diné teachings and public health students informing peers and relatives about vaccine education: providing Diné (Navajo)-centered COVID-19 education materials using student health messengers. Front Public Health. 2022 Dec 14.
Kim M, Lee H, Kiang P, Allison J. Development and acceptability of a peer-paired, cross-cultural and cross-generational storytelling HPV intervention for korean american college women. Health Educ Res. 2019 Oct;34(1):483–94.
Fenick AM, Leventhal JM, Gilliam W, Rosenthal MS. A Randomized Controlled Trial of Group Well-Child Care: Improved Attendance and Vaccination Timeliness. https://doi.org/101177/0009922820908582 [Internet]. 2020 Feb 28 [cited 2023 Mar 8];59(7):686–91. Available from: https://journals.sagepub.com/doi/https://doi.org/10.1177/0009922820908582.
Acknowledgements
none needed.
Funding
Sibylle Herzig van Wees is funded by Forte - Forskningsrådet för hälsa, arbetsliv och välfärd (2021 − 01299) to work on vaccine confidence in Sweden.
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Contributions
E.G. and S.H.vW conceptualized the project and wrote the manuscript. C.H. contributed to the writing of the article. E.G. and K.A. conducted the systematic review under supervision of SHvW, EG and KA conducted the screening and the quality assessment. All authors reviewed the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gobbo, E.L.S., Hanson, C., Abunnaja, K.S.S. et al. Do peer-based education interventions effectively improve vaccination acceptance? a systematic review. BMC Public Health 23, 1354 (2023). https://doi.org/10.1186/s12889-023-16294-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-16294-3