Abstract
Housing instability is variably defined but generally encompasses difficulty paying rent, living in poor or overcrowded conditions, moving frequently, or spending the majority of household income on housing costs. While there is strong evidence that people experiencing homelessness (i.e., lack of regular housing) are at increased risk for cardiovascular disease, obesity, and diabetes, less is known about housing instability and health. We synthesized evidence from 42 original research studies conducted in the United States examining the association of housing instability and cardiometabolic health conditions of overweight/obesity, hypertension, diabetes, and cardiovascular disease. The included studies varied widely in their definitions and methods of measuring housing instability, but all exposure variables were related to housing cost burden, frequency of moves, living in poor or overcrowded conditions, or experiencing eviction or foreclosure, measured at either the individual household level or at a population level. We also included studies examining the impact of receipt of government rental assistance, which serves as a marker of housing instability given that its purpose is to provide affordable housing for low-income households. Overall, we found mixed but generally adverse associations between housing instability and cardiometabolic health, including higher prevalence of overweight/obesity, hypertension, diabetes, and cardiovascular disease; worse hypertension and diabetes control; and higher acute health care utilization among those with diabetes and cardiovascular disease. We propose a conceptual framework for pathways linking housing instability and cardiometabolic disease that could be targeted in future research and housing policies or programs.
Similar content being viewed by others
Background
Housing instability is variably defined but generally encompasses difficulty paying rent, living in overcrowded conditions, moving frequently, spending the majority of household income on housing costs [1], or experiencing poor housing quality or unstable neighborhood environments [2, 3]. It has been associated with decreased access to routine healthcare, increased acute care utilization, and poor self-rated and mental health [2, 4,5,6,7], and is widely considered to be a fundamental social determinant of health. Housing instability disproportionately affects racial and ethnic minorities whose housing and economic opportunities have been restricted due to a history of discriminatory housing practices in the United States [8]. Rooted in structural racism, these practices forced minority groups such as Blacks and Hispanics into disadvantaged housing [9] and perpetuate residential racial segregation, which has been associated with poor health outcomes [10]. Housing instability is also a risk factor for homelessness, defined as lacking a regular nighttime residence or having a primary nighttime residence that is a temporary shelter or place not designed for sleeping [11]. While there is strong evidence that people experiencing homelessness have high rates of overweight and obesity [12, 13], barriers to diabetes management and health care access [14], increased risk for uncontrolled diabetes [15], and higher cardiovascular disease morbidity and mortality [16], less is known about the impact of housing instability on cardiometabolic health. Although housing instability represents a less severe housing status compared to homelessness, its implications on both the health of individuals and families, as well as on racial and ethnic health disparities, have increasingly become a focus of public health research and policy efforts [8, 10].
Several mechanisms linking housing affordability and both physical and mental health have been proposed in a recent systematic review by Downing and expanded upon by Rodgers et al. [17, 18]. We draw upon three of these proposed mechanisms to help explain how housing instability in general may impact cardiometabolic health: 1) material budgeting and tradeoffs, 2) displacement and distribution into disadvantaged environments, and 3) psychosocial stress and mental health (Fig. 1). The first mechanism, material budgeting and trade-offs, occurs in response to high housing cost burden, as decreased financial resources lead to lower capacity to purchase or access health-promoting goods and services, such as healthy foods, medications, and healthcare. Financial restraints may also cause individuals to work longer hours or additional jobs, leaving less time for health-promoting behaviors, such as physical activity, sleep, or medical appointments [17, 18]. In the second pathway of displacement and distribution, unaffordable housing costs and evictions or foreclosures can lead to forced moves, displacing households and distributing them into disadvantaged neighborhoods with multiple factors that can harm health, such as poor housing quality, environmental detriments like crime, pollution, and toxins, or decreased availability of healthy foods or safe recreation areas [17,18,19]. Finally, high housing cost burden, forced moves, or the perception of poor housing quality can lead to psychosocial stress, depression, and anxiety [20], which have been linked to obesity [21,22,23,24], cardiovascular disease [25,26,27,28], and diabetes [25, 29, 30].
An emerging body of literature has examined associations between cardiometabolic health outcomes and various dimensions of housing instability. Due to a lack of a singular definition, measures of housing instability vary widely in the literature [2, 20, 31]. Housing stability is often considered to represent one of four core dimensions of housing, along with affordability, quality, and neighborhood environment, each representing a pathway by which housing affects health [32,33,34]. While these pathways are often distinctly delineated in the literature, there is significant overlap of each of these dimensions of the housing construct. In this review, we broadly define the term housing instability, which is often used interchangeably with the term housing insecurity, to include problems with housing stability, affordability, and quality. Table 1 provides a summary of definitions and descriptions of the various components that can be used as measures of housing instability, including degree of difficulty affording housing costs (i.e., housing cost burden), frequency of moves, forced moves due to eviction or foreclosure, living in overcrowded conditions, living with friends or relatives to spilt housing costs (i.e., doubling up [35]), or experiencing poor housing quality. Use of government rental assistance programs may also be considered an indicator of housing instability, given that the goal of these programs is to alleviate housing cost burden for low-income households. Additionally, each of these components can represent exposure variables assessed at the individual household level, or aggregated by populations located within a geographical area, such as a county or census block [17]. Individual-level studies have examined the effects of direct household exposure to housing instability using participant surveys, interviews, or other screening tools. Population-level studies of housing instability have assessed the impacts of overcrowding, housing cost burden, or eviction and foreclosure rates affecting populations located within geographical area, such as census-level foreclosure rates or proportion of total household income spent on housing costs, aggregated to the county level.
The purpose of this narrative review is to summarize the literature on the relationship between housing instability and cardiometabolic health. We synthesized evidence from 42 original research studies conducted in the United States examining the relationship between various individual- or population-level exposures of housing instability, including housing cost burden, frequent moves, overcrowding/doubling up, poor housing quality, rental assistance use, and foreclosures and evictions, and the cardiometabolic conditions of overweight/obesity, hypertension, diabetes, and cardiovascular disease in adult populations.
Methods
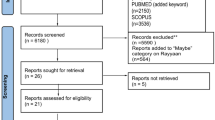
This review includes original research studies examining the relationship between housing instability and cardiometabolic health in US adult populations collected through a search of Pubmed and Scopus databases. Search terms included “cardiometabolic risk,” “overweight and obesity,” “hypertension,” diabetes and prediabetes,” “coronary disease,” “heart failure,” and “stroke,” in combination with “housing instability,” “housing insecurity,” “unstable housing,” “housing affordability,” “housing quality,” “housing conditions,” “foreclosures or mortgage possessions,” “evictions,” “rental assistance,” “housing assistance,” and “public housing.” These search terms yielded 394 English-language abstracts from the databases. We excluded animal studies, review articles, book chapters, editorials, commentaries, studies that focused on children, and literature examining the association between the built or neighborhood environment and cardiometabolic health, which has been comprehensively reviewed in prior literature [47,48,49,50,51,52]. We also excluded studies that focused exclusively on people experiencing homelessness as this area has been widely studied and reviewed and may have different implications for health outcomes and management of disease [35]. One hundred fifty abstracts remained after applying our exclusion criteria.
We reviewed these 150 abstracts to isolate studies examining the association between cardiometabolic health and the exposure variable of housing instability in the form of housing cost burden, frequent moves, overcrowding/doubling up, poor housing quality, or foreclosures or eviction. We also included studies exploring the exposure to government rental assistance programs, such as tenant-based (i.e., vouchers) and unit-based (i.e., public housing or project-based assistance) rent subsidies, as potential markers of current or recent housing instability. Forty articles met our inclusion criteria, with the remaining articles excluded as they did not specifically examine associations between housing instability as the exposure variable and the cardiometabolic conditions or outcomes of interest. While review articles were excluded from the results of our paper, we identified one additional article [53] absent from the database search after reading a pertinent review [43], and one article was identified during the peer review process [54]. We then grouped studies by cardiometabolic condition (overweight and obesity, hypertension, diabetes, and cardiovascular disease), and further categorized them based on whether the housing instability exposure represented an individual or population-level variable. Selected characteristics and key findings of the 42 included studies are provided in Table 2.
Throughout the literature, there was significant variability in the methods used to measure housing instability as well as the terminology used to refer to similar concepts (e.g., “housing instability,” “housing insecurity,” or “unstable housing”). In the results, we include the housing terms used in the original research articles and describe how the housing exposure was measured in the study. A few studies included homelessness in the broader definition of housing instability [56, 57, 78] but most studies reviewed did not explicitly include people experiencing homelessness in their sample populations. Regarding housing quality, we only include studies which assessed the effects of the perception of poor housing quality (e.g., poor housing quality reported on a study survey). The perception of or dissatisfaction with inadequate housing quality has been linked to a feeling of limited control over one’s housing circumstance [20], which may have important implications on health. We exclude the large body of literature demonstrating associations of specific household environmental toxins (e.g., lead, air pollutants) or adverse conditions (e.g., cold indoor temperature) with poor respiratory and cardiometabolic health, as these relationships have been comprehensively reviewed in prior literature [92,93,94,95,96,97].
Results
Overweight/obesity
Individual-level studies
Seven quantitative studies explored the relationship between housing instability on the individual level and weight status. While none examined housing instability alone as a primary exposure variable, two studies assessed housing instability in combination with other measures of social determinants of health to represent a composite exposure of social risk. In a longitudinal cohort study of 11,543 adults in Massachusetts receiving care at a large safety net health system, authors demonstrated that within 3 months of the coronavirus disease-2019 (COVID-19) lockdown, men with food or housing insecurity (collected by an unspecified electronic health record [EHR] screening tool) had higher odds of at least a 5% weight gain (odds ratio [OR] 1.44, 95% confidence interval [CI] 1.05, 1.97) compared to those without food or housing insecurity [73]. In a cross-sectional study of 33,550 adults receiving primary care at an academic medical center in New York, Heller et al. found that having three social needs (measured by a survey which included questions on housing quality and instability, as well as other social determinants of health such as food, utility, and transportation insecurity) was associated with higher prevalence of obesity (prevalence ratio [PR] 1.06, 95% CI 1.00–1.12) compared to having no needs [54].
Five studies explored the effect of government rental assistance on weight. A longitudinal cohort study by Fertig and Reingold using data from the Fragile Families and Child Wellbeing Study found that mothers moving into public housing between baseline and year one of follow-up had increased likelihood of being overweight at three-year follow-up compared to mothers eligible for but not yet living in public housing [62]. Another longitudinal cohort study of 116 adults receiving rental assistance, defined as use of public housing, other project-based housing including low-income housing tax credit, tenant-based housing (mostly vouchers), or state-assisted housing, between baseline and two-year follow-up, found moderate but not significant increases in body mass index (BMI) and obesity at two-year follow-up compared to the 1258 matched adults who were eligible for, but did not receive, rental assistance. In a sensitivity analysis excluding permanently disabled participants, authors found significantly higher obesity at two-year follow-up in the group receiving rental assistance, though this difference did not persist at four- or six-year follow-up [55]. Fertig and Reingold suggested that the increase in obesity associated with public housing residence may be due to factors in the neighborhood environment that promote weight gain, or due to increased financial resources created by housing subsidies that are then diverted to purchase of unhealthy food or excess calories [62].
The Moving to Opportunity (MTO) for Fair Housing Demonstration Program, a large, randomized housing mobility project by the US Department of Housing and Urban Development (HUD) intended to uncover the effects of neighborhood characteristics on social and health outcomes, showed similar associations with obesity. The MTO project randomized 4498 women with children living in public housing located in high-poverty census tracts of five large, urban US cities to one of three groups to receive: 1) housing vouchers usable for private-market housing located in low-poverty census tracts, and counseling to help with their housing search; 2) standard vouchers with no restrictions on where they could reside; and 3) no additional housing assistance (control). In an analysis of the MTO project, Ludwig et al. found that women from families in the low-poverty voucher group, who were given the opportunity to move out of public housing located in high-poverty census tracts into private-market housing located in low-poverty census tracts, had lower prevalence of BMI > 35 kg/m2 (− 4.61%, 95% CI − 8.54%, − 0.69%) and BMI > 40 kg/m2 (− 3.38%, 95% CI − 6.39%, − 0.36%) at a mean follow up of 12.6 years compared to the control group [71]. In contrast to these studies, a study by Kalousova using data from the Michigan Recession and Recovery Study found that there was no difference in BMI between adults receiving any type of rental assistance versus those eligible for but not receiving assistance [53].
In a study using repeated, cross-sectional data from the National Health Interview Survey to examine racial differences in sleep and cardiometabolic health by government-assisted rental housing status, Gaston et al. compared the prevalence of overweight/obesity in Black versus White adults by sleep duration category (i.e., short sleepers, recommended sleepers, and long sleepers). The study found that among government-assisted renters, there were no racial differences in overweight/obesity prevalence in men across sleep duration categories. However, among unassisted renters, Black male short and recommended sleepers had higher prevalence of overweight and obesity compared to White male recommended sleepers. In women, Black short and recommended sleepers had higher prevalence of overweight/obesity regardless of housing status, though racial differences were more pronounced among those living in unassisted housing compared to government-assisted housing. Gaston et al. concluded that government-assisted housing narrowed the weight disparities seen in Black men with worse sleep compared to White men with recommended sleep durations; however, racial disparities persisted in women regardless of housing tenure. The authors noted that since women are often primary caregivers of families, these gender differences highlight an area that deserves future research given its potential implications on maternal and child health [64].
Population-level studies
Nine quantitative studies examined the association between population-level measures of housing instability and weight. Three studies found that housing cost burden was associated with higher obesity prevalence. A study by Rodgers et al. examining the association between housing cost burden (measured as the proportion of total household income spent on housing costs aggregated to the county level) and cardiovascular disease risk factors found that a one percent increase in median county-level household income spent on housing costs was associated with a 37% increase in the odds of obesity. This association was stronger both in renters compared to homeowners, and in men compared to women, when results were stratified by housing tenure and gender, respectively. The authors proposed that the higher obesity risk in men may be due to increased susceptibility to financial stress, or lower healthcare utilization, compared to women [18]. Using geographically weighted regression (GWR) which allows for measurement in spatial variation of regression models, Hohl and Lotfata found that obesity was positively associated with severe rent (defined as percentage of population spending > 50% of income on housing rent) and that the region in Chicago with the worst severe rent problem also had the highest obesity prevalence using a spatiotemporal clustering technique [88]. Similarly Lotfata and Tomal used multiscale geographically weighted regression to find that severe rent and eviction rates are the main housing determinants associated with obesity prevalence in Chicago [90].
Six studies investigating the association between population-level eviction or foreclosure rates and weight produced mixed results. Hazekamp et al. found that the prevalence of obesity, as well as other unhealthy behavior indicators (i.e., binge drinking, current smoking status, lack of leisure-time physical activity, and short sleep), was associated with census-level eviction rates in urban Illinois communities [87]. Another cross-sectional study found that foreclosures in 75 of the top 100 most populous metropolitan areas in the United States were independently associated with obesity prevalence [89]. A longitudinal study followed 2068 adults from the Framingham Offspring Cohort over four examination waves between 1987–2008 to assess the association between area-level foreclosures and blood pressure. Authors found that each additional foreclosed property located within 100 m of a person’s home occurring in the year preceding the study examination was associated with a 0.2 kg/m2 increase in BMI and a 1.77 higher odds of being overweight (95% CI 1.02, 3.05) [80]. A cohort study of 59,854 adults receiving care at a Veterans Health Administration (VA) facility in metropolitan Chicago found no association between neighborhood foreclosures and BMI over six years of follow-up in the overall sample; however when restricting the sample to people who did not move over the study period, authors found that every 20 additional foreclosures was associated with a 0.03 kg/m2 increase in BMI (95% CI 0.01, 0.06) [86]. In contrast, a study of 105,919 continuously insured adults with diabetes in Northern California did not find an association between census-level foreclosure and BMI, though authors noted that the relatively shorter study period of four years may not have been long enough to detect an effect [84]. A longitudinal study by Christine et al. using data from the Multi-ethnic Study of Atherosclerosis (MESA) also found that there was no association between a standard deviation increase in neighborhood foreclosure count (1.9 foreclosures per quarter mile) and mean difference in BMI over a five-year follow-up period [83].
Hypertension
Individual-level studies
Literature regarding the association of hypertension with individual-level housing instability, housing affordability, or foreclosures was limited to five quantitative studies. Results from three studies examining measures of housing instability alone or in combination with other social determinants of health generally showed higher incidence and prevalence of hypertension. One longitudinal study of 4,342 Black and White young adults participating in the Coronary Artery Risk Development In Young Adults (CARDIA) study found no association of housing instability (measured by interview questions regarding overcrowding, frequent moves, or occupying a space without paying rent) and incident hypertension over 15 years of follow-up in the overall sample. When stratified by race and sex, however, authors found that women with housing instability were at higher risk of incident hypertension (incidence rate ratio [IRR] 4.7, 95% CI 2.4, 9.2) compared to stably housed white women. The authors explained these differences could be attributed to uneven distribution of social and environmental risk factors [79]. A cross-sectional study of 10,007 individuals participating in biennial Southeastern Pennsylvania Household Health Survey explored the relationship between hypertension and housing affordability, assessed as the level of difficulty paying rent. Authors found that among homeowners and renters, difficulty paying rent was associated with increased odds of poor self-rated health (adjusted OR 1.75, 95% CI 1.33, 2.29) and hypertension (adjusted OR 1.34, 95% CI 1.07, 1.69). Authors suggested these findings were related to the knowledge that those with housing unaffordability have a higher likelihood of delaying or skipping doctors’ visits or accessing medications, and this was supported by their results demonstrating that high housing costs were associated with cost-related healthcare nonadherence (adjusted OR 2.94, 95% CI 2.04, 4.25) and cost-related prescription medication nonadherence (adjusted OR 2.68, 95% CI 1.95, 3.70) [5]. The previously mentioned cross-sectional study by Heller et al. examining housing instability and quality in combination with other social needs found that having three social needs was associated with higher prevalence of hypertension (PR 1.15, 95% CI 1.09, 1.21) compared to having no needs [54].
One study examined the relationship between hypertension prevalence and individual-level foreclosures, and another investigated the effect of government rental assistance on hypertension prevalence. A case–control study by Pollack et al. found significantly higher rates of hypertension (adjusted OR 1.40, 95% CI 1.08, 1.81) and renal disease (adjusted OR 1.83, 95% CI 1.09, 3.06) among 404 adult homeowners who received a foreclosure notice (cases) compared to the 2020 adults in the control group who received care from the hospital system and lived in the same zone improvement plan (ZIP) code as cases. Authors also found that people experiencing foreclosure were more likely to have an ED visit, outpatient visit, and no-show appointment, but less likely to have a PCP visit in the 6 months prior to foreclosure notice, suggesting that health care utilization patterns shift in the time period leading up to a foreclosure event [74]. In the previously cited study by Gaston et al. examining racial differences in sleep and cardiometabolic health by government-assisted rental housing status, among those in unassisted housing, Black male short and recommended sleepers had higher prevalence of hypertension compared to White recommended sleepers, a difference was not seen among those receiving government-assisted housing. In women, the prevalence of hypertension was higher in Blacks compared to Whites across all sleep categories and rental assistance categories, with larger differences seen among unassisted residents, highlighting the importance of future research on gender differences in racial/ethnic health disparities [64].
Population-level studies
Four quantitative population-based studies on the relationship between housing instability and hypertension produced mixed results. The study by Rodgers et al. cited previously found that each percentage point increase in county-level median percentage of household income spent on housing was associated with a 22% increase in the likelihood of incident hypertension (OR 1.22, 95% CI 1.06, 1.42) among renters and homeowners. When results were stratified by housing tenure and gender, this association was stronger in renters compared to homeowners, and in men compared to women, possibly owing to increased financial stressors and decreased healthcare use in men as previously mentioned. Additionally, among people with incident hypertension, a one unit increase in housing cost burden was associated with lower likelihood of antihypertensive medication use (OR 0.79, 95% CI 0.65, 0.97), suggesting that the financial strain from unaffordable housing may negatively affect access to health resources [18].
Three other studies examined the relationship between hypertension and population-level foreclosures. In a cross-sectional study, Chambers et al. found that renters participating in the Hispanic Community Health Study/Study of Latinos living in a high foreclosure risk area (based on census tract-level data) had a higher prevalence of hypertension (PR 1.25, 95% CI 1.08, 1.46) and hypercholesterolemia (PR 1.12, 95% CI 1.01, 1.24) compared to those in medium or low foreclosure risk areas [82]. In a longitudinal study exploring the relationship between hypertension and proximity to foreclosures in the Framingham Offspring Cohort in Massachusetts, Arcaya et al. found that each additional foreclosure located within 100 m of a participant’s home was associated with an increase in systolic blood pressure (SBP) of 1.71 mmHg (95% CI 0.18, 3.24) [81]. In contrast, the longitudinal study by Christine et al. found that an increase in neighborhood foreclosure count of 1.9 foreclosures per quarter mile was associated with a mean decrease in SBP of 0.27 mmHg (95% CI -0.49, -0.04). The authors of this study noted that the variation in their results compared to Arcaya et al. may have been due to differences in measures of foreclosure, different statistical methods, or true variation in different locations. The authors further hypothesized that the stigma associated with foreclosure changed over time, recognizing that the study by Arcaya et al. overlapped with the housing crisis in the mid-2000s [83]. Ultimately, the mixed associations between foreclosures and hypertension in these studies demonstrate that the relationship is complex and depends on several multi-level factors.
Diabetes
Individual-level studies
A relatively larger body of literature (16 quantitative, 3 qualitative studies) exists on housing instability and diabetes outcomes. These studies examined multiple diabetes-related outcomes, including incidence and prevalence, disease control, healthcare utilization, healthcare quality, and self-care behaviors. Two studies analyzed the relationship between housing instability and diabetes incidence or prevalence. A longitudinal study by Schootman et al. of 998 African American adults living in St. Louis, Missouri, found that those reporting fair or poor housing quality (measured by survey questions regarding cleanliness inside building, physical condition of interior, condition of furnishings, condition of exterior of building, and global rating) had higher risk of incident diabetes compared to those reporting good or excellent conditions (cleanliness inside building, OR 1.78, 95% CI 1.03, 3.07; physical condition inside building, OR 2.53, 95% CI 1.47, 4.34; condition of furnishings inside building, OR 2.20, 95% CI 1.29, 3.75; condition of the outside of the building, OR 2.39, 95% CI 1.40, 4.08; overall condition of the dwelling, OR 1.78, 95% CI 1.02, 3.09) [75]. In a cross-sectional study investigating the association between housing instability and diabetes prevalence among white, Asian, and Native Hawaiian/other Pacific Islanders (NHOPIs) in Hawaii, Stupplebeen found that NHOPIs with housing insecurity, measured using a survey question on housing cost burden, had higher adjusted odds of diabetes (adjusted OR 1.85, 95% CI 1.13, 3.01) than those with housing security [76].
Two studies investigated the association between housing instability and diabetes control. In a study of 411 patients with diabetes from four clinics within a practice-based research network in Massachusetts, Berkowitz et al. found in unadjusted analyses that patients with housing instability (measured using survey questions assessing housing status, including homelessness, evictions, frequent moves, or doubling up) were more likely to have poor diabetes control (defined as a composite measure of hemoglobin A1c (HbA1c) > 9% (74.9 mmol/mol), low-density lipoprotein (LDL) cholesterol > 100 mg/dL (2.6 mmol/L), or blood pressure > 140/90 mmHg), but this difference was no longer statistically significant after adjusting for covariates [35, 56]. Similarly, a study of 274,123 adults with type 2 diabetes receiving care at Kaiser Permanente Northern California found that having at least one address change (a potential indicator of housing instability) was associated with higher chance of uncontrolled diabetes (HbA1c > 9% [74.9 mmol/mol], ARR 1.12, 95% CI 1.09, 1.15) and lower chance of controlled diabetes (HbA1c < 8% [63.9 mmol/mol], ARR 0.95, 95% CI 0.94, 0.96) [77].
Three cross-sectional studies assessed the association of housing instability on healthcare utilization in people with diabetes. In the same study by Berkowitz et al. cited above, housing instability was associated with a higher number of outpatient visits after adjusting for covariates (IRR 1.31, 95% CI 1.14, 1.51) [56]. A separate cross-sectional study by Berkowitz et al. examined 1087 nationally-representative, non-homeless, safety-net clinic patients with self-reported diabetes and found that unstable housing (measured using survey responses regarding housing cost burden, frequent moves, and doubling up) was associated with increased diabetes-related emergency department (ED) visits or hospitalizations (adjusted OR 5.17, 95% CI 2.08, 12.87) [35]. The Thomas et al. study mentioned above also found that having at least one address was associated with higher chance of ED visits (ARR 1.25, 95% CI 1.23, 1.27) [77].
Three cross-sectional studies examined diabetes care quality or self-care behaviors. A cross-sectional study of 16,091 employed adults with type 2 diabetes found that housing insecurity (measured using survey responses related to housing cost burden) was associated with decreased likelihood of having a physician visit (adjusted OR 0.58, 95% CI 0.37, 0.92), HbA1c assessment (adjusted OR 0.45, 95% CI 0.26, 0.78), or eye exam (adjusted OR 0.61, 95% CI 0.44, 0.83) [72]. In contrast, Gold et al. examined diabetes guideline-recommended care quality in a cross-sectional study of 73,484 community health center patients with diabetes and found that overall care quality was similar in those with housing insecurity (measured using an unspecified EHR screening tool), except for being less likely to have an up-to-date LDL screening [65]. Vijayaraghavan et al. found that among 711 low-income participants with diabetes, housing instability (ordered into five categories from most to least stable based on survey responses), was significantly associated with decreased diabetes self-efficacy, measured using the validated Self-Efficacy for Diabetes Scale [78].
Four studies assessed housing instability in combination with other adverse social determinants of health to determine the association between a composite measure of unmet basic needs and diabetes prevalence or diabetes-related outcomes. In Heller et al.’s large cross-sectional study mentioned previously, authors found that among adults receiving primary care at an academic medical center in New York, those with three social needs (measured by a survey which included questions on housing quality and instability) was associated with higher prevalence of diabetes (p-trend < 0.001) compared to no needs [54]. Similarly, a cross-sectional study of 5846 adults with type 2 diabetes receiving care from a hospital system based in Bronx, New York found that compared to having no social needs, having three or more needs (based on the same survey used in Heller et al.’s study) was associated with a higher likelihood (adjusted OR 1.59, 95% CI 1.26, 2.00) of uncontrolled diabetes, defined as HbA1c ≥ 9.0% (74.9 mmol/mol). Authors also found that having housing issues (which included problems with both housing quality and housing instability) was associated with higher likelihood of uncontrolled diabetes (p < 0.05) [59]. A cross-sectional study of 4043 adult patients with diabetes receiving care at Kaiser Permanente Northwest found that having one or more unmet basic needs (based on a survey which included questions about housing stability and affordability) was associated with an increased odds of having a HbA1c > 8% (63.9 mmol/mol), more outpatient and ED visits, and more delayed refills of diabetes medications compared to having no needs [63]. A study examining the cumulative association of various social risk factors including housing, food, financial, and utility insecurity in 579 adults with diabetes found that those with three or four social risk factors had a greater likelihood of cost-related medication non-adherence, diabetes distress, and anxiety or depression compared to those with no social risks [69].
The association of public housing or government rental assistance with diabetes-related measures was examined in four studies. In the same analysis of the MTO project cited previously, Ludwig et al. found that women from families in the low-poverty voucher group, who were given the opportunity to move out of public housing located in high-poverty census tracts into private-market housing located in low-poverty census tracts, had lower prevalence (− 4.31%, 95% CI − 7.82%, − 0.80%) of HbA1c ≥ 6.5% (47.5 mmol/mol) at a mean follow up of 12.6 years compared to those who received no additional housing assistance [71]. A study using the National Health and Nutrition Examination Survey (NHANES) survey data from 1999–2016 comparing 795 adults receiving either project-based housing (n = 450) or housing vouchers (n = 345) to 255 adults not yet receiving assistance but remained on the waitlist, found that those receiving project-based housing had lower HbA1c levels compared to the waitlist group, but the differences were not statistically significant. The authors did find, however, that residence in project-based housing was associated with a lower prevalence (− 3.7%, 95% CI − 7.0, 0.0%) of uncontrolled diabetes, defined as HbA1c ≥ 9.0% (74.9 mmol/mol), compared to the waitlist group [61]. A longitudinal cohort study by Lim et al. found that residence in New York City public housing was associated with higher prevalence of stable housing pattern (PR 1.16, 95% CI 1.07, 1.25), based on number of address changes over the 12-year follow-up period, but not with reduced diabetes risk (relative risk [RR] 1.11, 95% CI 0.83, 1.48). Among those experiencing housing instability, living in public housing was associated with a higher risk of diabetes compared to not living in public housing. The authors proposed that one potential mechanism for this finding could be that relocation from one public housing unit to another may cause stress via disruption of social cohesion and support [70]. In the study by Gaston et al., among those in unassisted housing, Black male short sleepers had higher prevalence of diabetes compared to White recommended sleepers, a difference that was not seen among those in government-assisted housing. In women, compared to White recommended sleepers, Black short sleepers had higher prevalence of diabetes in either rental assistance category [64]. As mentioned previously, this finding suggests that rental assistance appears to attenuate racial disparities in diabetes prevalence for men but not women.
Finally, there were three qualitative studies examining both provider and patient perspectives on housing instability and diabetes management. A study on the perspective of providers practicing in Southeastern Appalachian Ohio found that providers cited patients’ housing insecurity, lack of access to providers, lack of access to transportation, food insecurity and financial insecurity as barriers to diabetes care [57]. Two other qualitative studies found that patients with diabetes viewed housing access as an important influence on their diabetes self-management and ability to afford diabetes-related expenses [67] and that transitions to rent-assisted housing may support diabetes self-management [68].
Population-level studies
Two quantitative studies examined the relationship between neighborhood-level housing foreclosure and diabetes control. The longitudinal study by Christine et al. used data from the MESA cohort to examine fasting glucose levels and found that an increase in neighborhood foreclosure count of 1.9 foreclosures per quarter mile was associated with an increase in mean fasting glucose of 0.26 mg/dL (0.014 mmol/L; 95% CI 0.04, 0.46) [83]. A longitudinal study by Downing et al. found no statistically significant relationship between changes in foreclosure rate per census-block group and change in annual mean HbA1c level among 105,930 adults with diabetes receiving care at a large integrated healthcare system in Northern California, suggesting that increased foreclosure rates did not worsen glycemic control in this population [85].
Cardiovascular disease
Individual-level studies
Literature examining the association between housing instability and cardiovascular disease (i.e., coronary heart disease, heart failure, and stroke) was limited to four quantitative studies. Three studies analyzed the relationship between individual-level housing instability and cardiovascular disease measures, and one examined the association between cardiovascular disease and government rental assistance use. A study of 2,952,605 Medicare beneficiaries hospitalized for acute myocardial infarction (MI) or congestive heart failure (termed the index admission) found that those with housing instability (defined in this study as two or more unique residential addresses on EHR claims data) had higher odds of hospital readmission within 30 days of discharge from index admission [66]. A large cross-sectional study using data from the Behavioral Risk Factor Surveillance System (BRFSS) to evaluate the independent effects of chronic illness on food and housing insecurity, found that having self-reported cardiovascular disease (i.e., MI, angina, or coronary heart disease) was associated with increased odds of having housing insecurity (OR 1.69, 95% CI 1.07, 2.66), measured using a survey question related to housing cost burden. This study found no association between stroke and housing insecurity. The authors posited that patients experiencing stroke may have more functional limitations that require them to move in with or closer to family members, which in turn increases their level of support and potentially decreases their risk of housing insecurity. In contrast, those with cardiac disease may have higher pharmaceutical costs for medications and decreased likelihood of relocating closer to or moving in with family members compared to patients experiencing stroke, leaving them susceptible to adverse social determinants of health like housing insecurity [60]. The study by Stupplebeen found that among NHOPIs, those with housing insecurity had higher adjusted odds of self-reported MI, angina, coronary heart disease, or stroke [76].
Chambers and Rosenbaum compared cardiovascular disease-related outcomes across three government rental assistance groups (public housing residents, housing vouchers recipients, and people eligible for but not receiving housing assistance) in the cross-sectional Affordable Housing as an Obesity Mediating Environment (AHOME) study of 371 Latino adults. This study found lower odds of cardiovascular disease (defined as having at least one cardiovascular disease [CVD]-related outcome of heart attack, stroke, or hypertension) for those not receiving housing assistance (OR 0.394, 95% CI 0.204, 0.761) and those using housing vouchers (OR 0.527, 95% CI 0.280, 0.992), compared to residents of public housing. They also found that the prevalence of CVD was similar for those using housing vouchers and those not receiving housing assistance. Overall, these findings suggested a potential benefit of housing vouchers use over public housing [58].
Population-level studies
Only one study explored the relationship between population-level housing instability and cardiovascular disease. A large cross-sectional study by Segar et al. using data from the American Heart Association’s Get With The Guidelines-Heart Failure registry compared hospital length of stay for heart failure by various social determinants of health and race. This study found that housing instability (measured in this study by ZIP code-level neighborhood/residential characteristics including percentage of housing vacancy, mobile homes, or overcrowding) was associated with longer length of stay for both Black and White adults [91].
Conclusions
Our review of the literature found generally adverse associations between housing instability and cardiometabolic health conditions of overweight/obesity, hypertension, diabetes, and cardiovascular disease. There is moderate evidence to suggest that housing instability is associated with higher prevalence of overweight/obesity, hypertension, diabetes, and cardiovascular disease, worse hypertension and diabetes control, and higher acute health care utilization among those with diabetes and cardiovascular disease. Most studies included in this narrative review were cross-sectional which do not allow for conclusions to be drawn about the causal direction of these associations. The longitudinal cohort studies produced inconsistent results, and only a few studies leveraged natural experiments to assess the impact of governmental rental assistance use on health outcomes. We found no randomized studies that tested interventions to address housing instability and improve cardiometabolic health.
Through the lens of the conceptual framework proposed in Fig. 1, we can categorize some of the evidence from this narrative review to help understand which pathways may be the best targets for housing policies and interventions aimed at improving cardiometabolic health outcomes. Several studies have shown that housing cost burden is associated with cost-related nonadherence, both to prescription medications and health care visits [5, 18, 69], highlighting the importance of the material budgeting and trade-off pathway in which high housing costs lead to increased financial strain, thereby leaving fewer resources to address health-related needs. While qualitative studies in this review are limited, they have demonstrated that transition to a more stable and affordable housing situation such as subsidized housing frees up financial resources to allow patients to afford health-related expenses [67, 68]. Those with housing instability may also work longer hours or take on additional jobs to offset housing cost burden, leading to decreased time to devote to their health [18]. Additional research is needed to further understand whether obtaining affordable housing through subsidized housing programs can improve adherence and increase patient’s capacity to engage in health promoting behaviors by allowing patients to free up financial resources and time for their health needs.
The second pathway of residential displacement and distribution to poor quality housing and disadvantaged environments may also serve as a crucial target for interventions and policies to improve the health of those with housing instability. The studies in this review which examined the health implications associated with specific types of government rental assistance support the idea that displacement and resultant redistribution of families into disadvantaged neighborhoods can have detrimental health effects. While the overarching purpose of government rental assistance is to alleviate housing cost burden and theoretically improve housing stability, a few studies suggest that transition into subsidized housing, and particularly public housing, is associated with worse cardiometabolic health outcomes [55, 58, 62]. Although transition into public housing may provide housing stability [70], the associated adverse health outcomes may be explained by the fact that public housing units tend to be located in racially segregated areas with high socioeconomic deprivation and limited neighborhood resources [62, 98] which have been tied to poor cardiometabolic health [99, 100]. The MTO demonstration project, a landmark housing mobility study leveraging a natural experimental design, further supported this phenomenon by showing that lifting families out of high-poverty neighborhoods through tenant-based vouchers led to less severe obesity and uncontrolled diabetes [71]. Another study included in this review found that adults receiving tenant-based housing assistance had lower odds of cardiovascular disease compared to those living in public housing [58], suggesting that there may be a benefit of housing voucher programs over unit-based subsidies. Tenant-based assistance allows tenants to rent in the private market which may provide families with more flexibility to choose homes located in better neighborhoods and built environments (i.e., physical characteristics of neighborhoods where people live, work, and recreate), compared to subsidies that are tied specific units and may be located in disadvantaged areas. Housing units located in these areas may suffer from poor housing quality due to lack of community resources and investment, as suggested by another MTO analysis by Nguyen et al. which found that those moving out of public housing in high-poverty areas to private-market housing located in low-poverty areas improved housing quality (i.e. fewer problems with housing units such as broken windows, problems with heating, or pests) compared to those who remained in public housing. While it is well-established that the neighborhood and built environment are associated with cardiometabolic health [47,48,49,50,51,52], this group of literature suggests that housing quality and neighborhood environment appear to be intimately linked to rental assistance type and clearly play important roles in cardiometabolic health outcomes [49, 52, 71]. Further research, ideally in the form of additional natural experiments, is needed to test differences in cardiometabolic health outcomes by rental assistance type and neighborhood environment, which in turn will help inform policymakers’ prioritization of housing assistance programs.
The third pathway of psychosocial stress and mental health may also help to explain the adverse associations between housing instability and cardiometabolic health. Stress can increase not only in response to one’s own experience of financial strain or a forced move, but also at the population level through observing neighbors’ experiences of residential displacement in areas with high foreclosure and eviction rates, which can contribute to decreased social cohesion and neighborhood disinvestment. In addition to stress, other mental health conditions such as depression, anxiety, and substance use disorder have been linked to housing instability and other frequently coexisting adverse social determinants of health like food insecurity [18, 54, 69, 77]. Efforts to reduce the psychosocial stress and address mental health diagnoses tied to housing instability therefore may improve overall cardiometabolic health, especially since stress, anxiety, and depression have been associated with increased obesity [21, 23, 24], metabolic syndrome [22], diabetes [25, 29, 30], and cardiovascular disease [25,26,27,28]. Future research should further define this relationship given its role as an important mediator in the pathway towards improved cardiometabolic health.
While a few themes emerged from our review of this body of literature, a major barrier that precludes further definitive conclusions is the heterogeneity in both the measures used to capture housing instability as an exposure, as well as the cardiometabolic measures examined as outcomes. Housing instability as a construct is variably defined in the literature and can encompass many elements including housing cost burden, overcrowding and doubling up, poor housing quality, frequent moves, forced moves due to evictions or foreclosures, and use of government rental assistance, each of which was measured in various ways throughout this body of literature. Furthermore, each element does not exist in isolation, but rather families often experience multiple housing stressors simultaneously, which likely have more detrimental effects on health than one alone [20]. In addition to the myriad of housing instability measures, the cardiometabolic health outcomes examined in this body of literature also varied widely, spanning domains of disease prevalence and control, healthcare utilization, guideline-recommended care quality, self-management behaviors, and qualitative assessments of provider and patient perspectives on housing and health. Overall, the heterogeneity of current research makes it challenging to identify the most effective housing interventions or policies to improve various aspects of cardiometabolic health.
Although our understanding of the mechanisms driving the adverse associations between housing instability and cardiometabolic health has continued to grow, the complexity of this relationship leaves many gaps in our knowledge and makes it difficult to endorse specific housing policies or programs. Instead, we believe these knowledge gaps highlight potential areas for further research. Given that randomized controlled housing interventions may be difficult, costly, and possibly unethical to design and implement, we recommend that researchers leverage natural experiments to examine the potential impact of new or existing housing policies or programs on cardiometabolic health. Specifically, natural experiments can assess whether programs or policies intended to alleviate housing cost burden, prevent displacement of households into disadvantaged neighborhoods, or address the stress and mental health conditions associated with housing instability have positive effects on cardiometabolic health. This future research will help stakeholders and policymakers focus efforts on existing housing programs, or identify opportunities for new policies in these domains, with the collective goal of improving cardiometabolic health equity.
Availability of data and materials
Not applicable.
Abbreviations
- AHOME:
-
Affordable Housing as an Obesity Mediating Environment
- BMI:
-
Body mass index
- BRFSS:
-
Behavioral Risk Factor Surveillance System
- CARDIA:
-
Coronary Artery Risk Development In Young Adults
- CI:
-
Confidence interval
- COVID-19:
-
Coronavirus disease-2019
- CVD:
-
Cardiovascular disease
- ED:
-
Emergency department
- EHR:
-
Electronic health record
- GWR:
-
Geographically weighted regression
- HbA1c:
-
Hemoglobin A1c
- IRR:
-
Incidence rate ratio
- LDL:
-
Low-density lipoprotein
- MESA:
-
Multi-ethnic Study of Atherosclerosis
- MI:
-
Myocardial infarction
- MTO:
-
Moving to Opportunity for Fair Housing Demonstration Program
- NHANES:
-
National Health and Nutrition Examination
- NHOPIs:
-
Native Hawaiian/other Pacific Islanders
- OR:
-
Odds ratio
- PR:
-
Prevalence ratio
- RR:
-
Relative risk
- SBP:
-
Systolic blood pressure
- VA:
-
Veterans Health Administration
- ZIP:
-
Zone improvement plan
References
Office of Disease Prevention and Health Promotion. Housing Instability: Healthy People 2030; [Available from: https://health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/housing-instability.
Sandel M, Sheward R, de Ettinger S, Coleman SM, Frank DA, Chilton M, et al. Unstable Housing and Caregiver and Child Health in Renter Families. Pediatrics. 2018;141(2):e20172199.
Johnson A, Meckstroth A. Ancillary Services to Support Welfare to Work. US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. 1998. https://aspe.hhs.gov/reports/ancillary-services-support-welfare-work. Accessed 17 May 2023.
Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71–7.
Pollack CE, Griffin BA, Lynch J. Housing affordability and health among homeowners and renters. Am J Prev Med. 2010;39(6):515–21.
Burgard SA, Seefeldt KS, Zelner S. Housing instability and health: findings from the Michigan Recession and Recovery Study. Soc Sci Med. 2012;75(12):2215–24.
Kim H, Burgard SA. Housing instability and mental health among renters in the michigan recession and recovery study. Public Health. 2022;209:30–5.
Hilovsky K, Lim K, Williams TT. Creating the Healthiest Nation: Health and Housing Equity. American Public Health Association, May 2020. https://www.apha.org/-/media/files/pdf/topics/equity/health_and_housing_equity.ashx. Accessed 17 May 2023.
Jacobs DE. Environmental health disparities in housing. Am J Public Health. 2011;101(Suppl 1):S115-22.
Kalra GL, Watson KE. Health Consequences of Segregation and Disenfranchisement. J Am Heart Assoc. 2022;11(3):e024772.
US Department of Housing and Urban Development. HUDUser Glossary [Available from: https://archives.huduser.gov/portal/glossary/glossary_all.html.
Huang C, Foster H, Paudyal V, Ward M, Lowrie R. A systematic review of the nutritional status of adults experiencing homelessness. Public Health. 2022;208:59–67.
Tsai J, Rosenheck RA. Obesity among chronically homeless adults: is it a problem? Public Health Rep. 2013;128(1):29–36.
White BM, Logan A, Magwood GS. Access to Diabetes Care for Populations Experiencing Homelessness: an Integrated Review. Curr Diab Rep. 2016;16(11):112.
Axon RN, Gebregziabher M, Dismuke CE, Hunt KJ, Yeager D, Ana EJS, et al. Differential Impact of Homelessness on Glycemic Control in Veterans with Type 2 Diabetes Mellitus. J Gen Intern Med. 2016;31(11):1331–7.
Al-Shakarchi NJ, Evans H, Luchenski SA, Story A, Banerjee A. Cardiovascular disease in homeless versus housed individuals: a systematic review of observational and interventional studies. Heart. 2020;106(19):1483–8.
Downing J. The health effects of the foreclosure crisis and unaffordable housing: A systematic review and explanation of evidence. Soc Sci Med. 2016;162:88–96.
Rodgers J, Briesacher BA, Wallace RB, Kawachi I, Baum CF, Kim D. County-level housing affordability in relation to risk factors for cardiovascular disease among middle-aged adults: The National Longitudinal Survey of Youths 1979. Health Place. 2019;59:102194.
Desmond M, Shollenberger T. Forced Displacement From Rental Housing: Prevalence and Neighborhood Consequences. Demography. 2015;52(5):1751–72.
Suglia SF, Chambers EC, Sandel M. Poor Housing Quality and Housing Instability. The Social Determinants of Mental Health. In: Compton MT, Shim RS, editors. The social determinants of mental health. American Psychiatric Publishing, Inc., a division of the American Psychiatric Association; 2015. p. 171-192.
Tomiyama AJ. Stress and Obesity. Annu Rev Psychol. 2019;70:703–18.
Tenk J, Matrai P, Hegyi P, Rostas I, Garami A, Szabo I, et al. Perceived stress correlates with visceral obesity and lipid parameters of the metabolic syndrome: A systematic review and meta-analysis. Psychoneuroendocrinology. 2018;95:63–73.
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–9.
Amiri S, Behnezhad S. Obesity and anxiety symptoms: a systematic review and meta-analysis. Neuropsychiatr. 2019;33(2):72–89.
Hackett RA, Steptoe A. Psychosocial Factors in Diabetes and Cardiovascular Risk. Curr Cardiol Rep. 2016;18(10):95.
Cohen BE, Edmondson D, Kronish IM. State of the Art Review: Depression, Stress, Anxiety, and Cardiovascular Disease. Am J Hypertens. 2015;28(11):1295–302.
Hare DL, Toukhsati SR, Johansson P, Jaarsma T. Depression and cardiovascular disease: a clinical review. Eur Heart J. 2014;35(21):1365–72.
Steptoe A, Kivimaki M. Stress and cardiovascular disease. Nat Rev Cardiol. 2012;9(6):360–70.
Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord. 2012;142(Suppl):S8-21.
Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24(6):1069–78.
Frederick TJ, Chwalek M, Hughes J, Karabanow J, Kidd S. HOW STABLE IS STABLE? DEFINING AND MEASURING HOUSING STABILITY. J Community Psychol. 2014;42(8):964–79.
Sims M, Kershaw KN, Breathett K, Jackson EA, Lewis LM, Mujahid MS, et al. Importance of Housing and Cardiovascular Health and Well-Being: A Scientific Statement From the American Heart Association. Circ Cardiovasc Qual Outcomes. 2020;13(8):e000089.
Taylor L. Housing and Health: an Overview of the Literature. Health Affairs Health Policy Brief June 7, 2018. https://doi.org/10.1377/hpb20180313.396577.
Swope CB, Hernandez D. Housing as a determinant of health equity: A conceptual model. Soc Sci Med. 2019;243:112571.
Berkowitz SA, Kalkhoran S, Edwards ST, Essien UR, Baggett TP. Unstable Housing and Diabetes-Related Emergency Department Visits and Hospitalization: A Nationally Representative Study of Safety-Net Clinic Patients. Diabetes Care. 2018;41(5):933–9.
Office of Policy Development and Research. Rental Burdens: Rethinking Affordability Measures: US Department of Housing and Urban Development; [Available from: https://www.huduser.gov/portal/pdredge/pdr_edge_featd_article_092214.html.
Blake KS, Kellerson RL, Simic A. Measuring Overcrowding in Housing. Washington (DC): US Department of Housing and Urban Development, Office of Policy Development and Research; 2007. Available at: https://www.huduser.gov/publications/pdf/Measuring_Overcrowding_in_Hsg.pdf. Accessed 17 May 2023.
Office of Policy Development and Research. American Housing Survey Reveals Rise in Doubled-Up Households During Recession: US Department of Housing and Urban Development; Available at: https://www.huduser.gov/portal/pdredge/pdr_edge_research_012714.html. Accessed 17 May 2023.
Office of Disease Prevention and Health Promotion. Quality of Housing: U.S. Department of Health and Human Services; [Available from: https://health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/quality-housing#:~:text=Poor%20housing%20quality%20and%20inadequate,including%20chronic%20disease%20and%20injury.
U.S. Department of the Treasury & the U.S. Department of Housing and Urban Development. Glossary of Key Terms [Available from: https://www.makinghomeaffordable.gov/get-answers/get-answers-learning-glossary#:~:text=Foreclosure%3A%20The%20legal%20process%20by,to%20make%20timely%20mortgage%20payments.
US Department of Housing and Urban Development. Glossary of Terms to Affordable Housing [Available from: https://archives.hud.gov/local/nv/goodstories/2006-04-06glos.cfm.
US Department of Housing and Urban Development. Housing Choice Vouchers Fact Sheet [Available from: https://www.hud.gov/topics/housing_choice_voucher_program_section_8#hcv01.
Chen KL, Miake-Lye IM, Begashaw MM, Zimmerman FJ, Larkin J, McGrath EL, et al. Association of Promoting Housing Affordability and Stability With Improved Health Outcomes: A Systematic Review. JAMA Netw Open. 2022;5(11):e2239860.
National Housing Law Project. Project-Based Rental Assistance [Available from: https://www.nhlp.org/resource-center/project-based-rental-assistance/.
US Department of Housing and Urban Development. HUD's Public Housing Program [Available from: https://www.hud.gov/topics/rental_assistance/phprog.
Cassella J. Understanding Project-Based Rental Assistance. National Housing Law Project, 2018. Available at: https://www.nhlp.org/wp-content/uploads/2018/03/Saving-HUD-Homes-2-FINAL.pdf. Accessed 17 May 2023.
Chandrabose M, Rachele JN, Gunn L, Kavanagh A, Owen N, Turrell G, et al. Built environment and cardio-metabolic health: systematic review and meta-analysis of longitudinal studies. Obes Rev. 2019;20(1):41–54.
Booth KM, Pinkston MM, Poston WS. Obesity and the built environment. J Am Diet Assoc. 2005;105(5 Suppl 1):S110–7.
Amuda AT, Berkowitz SA. Diabetes and the Built Environment: Evidence and Policies. Curr Diab Rep. 2019;19(7):35.
Black JL, Macinko J. Neighborhoods and obesity. Nutr Rev. 2008;66(1):2–20.
Leal C, Chaix B. The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obes Rev. 2011;12(3):217–30.
Malambo P, Kengne AP, De Villiers A, Lambert EV, Puoane T. Built Environment, Selected Risk Factors and Major Cardiovascular Disease Outcomes: A Systematic Review. PLoS ONE. 2016;11(11):e0166846.
Kalousova L, Evangelist M. Rent Assistance and Health: Findings from Detroit. Hous Stud. 2019;34(1):111–41.
Heller CG, Rehm CD, Parsons AH, Chambers EC, Hollingsworth NH, Fiori KP. The association between social needs and chronic conditions in a large, urban primary care population. Prev Med. 2021;153:106752.
Antonakos CL, Colabianchi N. Impact of Rental Assistance on Modifiable Health Risk Factors and Behaviors in Adults. Cityscape. 2018;20(2):133–44.
Berkowitz SA, Meigs JB, DeWalt D, Seligman HK, Barnard LS, Bright OJ, et al. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med. 2015;175(2):257–65.
Beverly EA, Ritholz MD, Cook K, Johnson LK, Ruhil A, Singh RP, et al. Diabetes in Appalachia: providers’ perspectives. Prim Health Care Res Dev. 2020;21:e11.
Chambers EC, Rosenbaum E. Cardiovascular health outcomes of Latinos in the Affordable Housing as an Obesity Mediating Environment (AHOME) study: a study of rental assistance use. J Urban Health. 2014;91(3):489–98.
Chambers EC, McAuliff KE, Heller CG, Fiori K, Hollingsworth N. Toward Understanding Social Needs Among Primary Care Patients With Uncontrolled Diabetes. J Prim Care Community Health. 2021;12:2150132720985044.
Charkhchi P, Fazeli Dehkordy S, Carlos RC. Housing and Food Insecurity, Care Access, and Health Status Among the Chronically Ill: An Analysis of the Behavioral Risk Factor Surveillance System. J Gen Intern Med. 2018;33(5):644–50.
Fenelon A, Lipska KJ, Denary W, Blankenship KM, Schlesinger P, Esserman D, et al. Association Between Rental Assistance Programs and Hemoglobin A1c Levels Among US Adults. JAMA Netw Open. 2022;5(7):e2222385.
Fertig AR, Reingold DA. Public housing, health and health behaviors: is there a connection? J Policy Anal Manage. 2007;26(4):831–59.
Fitzpatrick SL, Banegas MP, Kimes TM, Papajorgji-Taylor D, Fuoco MJ. Prevalence of Unmet Basic Needs and Association with Diabetes Control and Care Utilization Among Insured Persons with Diabetes. Popul Health Manag. 2021;24(4):463–9.
Gaston SA, Jackson WB 2nd, Williams DR, Jackson CL. Sleep and cardiometabolic health by government-assisted rental housing status among Black and White men and women in the United States. Sleep Health. 2018;4(5):420–8.
Gold R, Kaufmann J, Gottlieb LM, Weiner SJ, Hoopes M, Gemelas JC, et al. Cross-Sectional Associations: Social Risks and Diabetes Care Quality, Outcomes. Am J Prev Med. 2022;63(3):392-402.
Joynt Maddox KE, Reidhead M, Hu J, Kind AJH, Zaslavsky AM, Nagasako EM, et al. Adjusting for social risk factors impacts performance and penalties in the hospital readmissions reduction program. Health Serv Res. 2019;54(2):327–36.
Keene DE, Guo M, Murillo S. “That wasn’t really a place to worry about diabetes”: Housing access and diabetes self-management among low-income adults. Soc Sci Med. 2018;197:71–7.
Keene DE, Henry M, Gormley C, Ndumele C. “Then I Found Housing and Everything Changed”: Transitions to Rent-Assisted Housing and Diabetes Self-Management. Cityscape. 2018;20(2):107–18.
Leung CW, Heisler M, Patel MR. Multiple social risk factors are adversely associated with diabetes management and psychosocial outcomes among adults with diabetes. Prev Med Rep. 2022;29:101957.
Lim S, Liu SYS, Jacobson MH, Poirot E, Crossa A, Locke S, et al. Housing stability and diabetes among people living in New York city public housing. SSM Popul Health. 2020;11:100605.
Ludwig J, Sanbonmatsu L, Gennetian L, Adam E, Duncan GJ, Katz LF, et al. Neighborhoods, obesity, and diabetes–a randomized social experiment. N Engl J Med. 2011;365(16):1509–19.
Mosley-Johnson E, Walker RJ, Thakkar M, Campbell JA, Hawks L, Pyzyk S, et al. Relationship between housing insecurity, diabetes processes of care, and self-care behaviors. BMC Health Serv Res. 2022;22(1):61.
Mulugeta W, Desalegn H, Solomon S. Impact of the COVID-19 pandemic lockdown on weight status and factors associated with weight gain among adults in Massachusetts. Clin Obes. 2021;11(4): e12453.
Pollack CE, Kurd SK, Livshits A, Weiner M, Lynch J. A case-control study of home foreclosure, health conditions, and health care utilization. J Urban Health. 2011;88(3):469–78.
Schootman M, Andresen EM, Wolinsky FD, Malmstrom TK, Miller JP, Yan Y, et al. The effect of adverse housing and neighborhood conditions on the development of diabetes mellitus among middle-aged African Americans. Am J Epidemiol. 2007;166(4):379–87.
Stupplebeen DA. Housing and Food Insecurity and Chronic Disease Among Three Racial Groups in Hawai’i. Prev Chronic Dis. 2019;16:E13.
Thomas T, Dyer W, Adams A, Grant R, Schmittdiel J. Address Changes Are Associated With Unmet Glycemic Targets: Opportunities to Improve Processes and Outcomes of Care Among People With Type 2 Diabetes. Perm J. 2022;26(2):1–10.
Vijayaraghavan M, Jacobs EA, Seligman H, Fernandez A. The association between housing instability, food insecurity, and diabetes self-efficacy in low-income adults. J Health Care Poor Underserved. 2011;22(4):1279–91.
Vijayaraghavan M, Kushel MB, Vittinghoff E, Kertesz S, Jacobs D, Lewis CE, et al. Housing instability and incident hypertension in the CARDIA cohort. J Urban Health. 2013;90(3):427–41.
Arcaya M, Glymour MM, Chakrabarti P, Christakis NA, Kawachi I, Subramanian SV. Effects of proximate foreclosed properties on individuals’ weight gain in Massachusetts, 1987–2008. Am J Public Health. 2013;103(9):e50–6.
Arcaya M, Glymour MM, Chakrabarti P, Christakis NA, Kawachi I, Subramanian SV. Effects of proximate foreclosed properties on individuals’ systolic blood pressure in Massachusetts, 1987 to 2008. Circulation. 2014;129(22):2262–8.
Chambers EC, Hanna DB, Hua S, Duncan DT, Camacho-Rivera M, Zenk SN, et al. Relationship between area mortgage foreclosures, homeownership, and cardiovascular disease risk factors: The Hispanic Community Health Study/Study of Latinos. BMC Public Health. 2019;19(1):77.
Christine PJ, Moore K, Crawford ND, Barrientos-Gutierrez T, Sanchez BN, Seeman T, et al. Exposure to Neighborhood Foreclosures and Changes in Cardiometabolic Health: Results From MESA. Am J Epidemiol. 2017;185(2):106–14.
Downing J, Karter A, Rodriguez H, Dow WH, Adler N, Schillinger D, et al. No Spillover Effect of the Foreclosure Crisis on Weight Change: The Diabetes Study of Northern California (DISTANCE). PLoS ONE. 2016;11(3):e0151334.
Downing J, Laraia B, Rodriguez H, Dow WH, Adler N, Schillinger D, et al. Beyond the Great Recession: Was the Foreclosure Crisis Harmful to the Health of Individuals With Diabetes? Am J Epidemiol. 2017;185(6):429–35.
Duran AC, Zenk SN, Tarlov E, Duda S, Smith G, Lee JM, et al. Foreclosures and weight gain: Differential associations by longer neighborhood exposure. Prev Med. 2019;118:23–9.
Hazekamp C, Yousuf S, Khare M, MacDowell M. Unhealthy behaviours in urban Illinois communities affected by eviction: A descriptive analysis. Health Soc Care Community. 2021;29(3):867–75.
Hohl A, Lotfata A. Modeling spatiotemporal associations of obesity prevalence with biking, housing cost and green spaces in Chicago, IL, USA, 2015–2017. J Transp Health. 2022;26: 101412.
Jones A, Mamudu HM, Squires GD. Mortgage possessions, spatial inequality, and obesity in large US metropolitan areas. Public Health. 2020;181:86–93.
Lotfata A, Tomal M. Exploring Housing Determinants of Obesity Prevalence Using Multiscale Geographically Weighted Regression in Chicago, Illinois. The Professional Geographer. 2022. Available at: https://doi.org/10.1080/00330124.2022.2111692. Accessed 17 May 2023.
Segar MW, Keshvani N, Rao S, Fonarow GC, Das SR, Pandey A. Race, Social Determinants of Health, and Length of Stay Among Hospitalized Patients With Heart Failure: An Analysis From the Get With The Guidelines-Heart Failure Registry. Circ Heart Fail. 2022;15(11): e009401.
Raju S, Siddharthan T, McCormack MC. Indoor Air Pollution and Respiratory Health. Clin Chest Med. 2020;41(4):825–43.
Lee KK, Bing R, Kiang J, Bashir S, Spath N, Stelzle D, et al. Adverse health effects associated with household air pollution: a systematic review, meta-analysis, and burden estimation study. Lancet Glob Health. 2020;8(11):e1427–34.
Wang Q, Li C, Guo Y, Barnett AG, Tong S, Phung D, et al. Environmental ambient temperature and blood pressure in adults: A systematic review and meta-analysis. Sci Total Environ. 2017;575:276–86.
Marsh GM, Riordan AS, Keeton KA, Benson SM. Non-occupational exposure to asbestos and risk of pleural mesothelioma: review and meta-analysis. Occup Environ Med. 2017;74(11):838–46.
Pettigrew HD, Selmi CF, Teuber SS, Gershwin ME. Mold and human health: separating the wheat from the chaff. Clin Rev Allergy Immunol. 2010;38(2–3):148–55.
Eguiluz-Gracia I, Mathioudakis AG, Bartel S, Vijverberg SJH, Fuertes E, Comberiati P, et al. The need for clean air: The way air pollution and climate change affect allergic rhinitis and asthma. Allergy. 2020;75(9):2170–84.
Center on Budget and Policy Priorities. Policy Basics: Public Housing: Center on Budget and Policy Priorities; [Available from: https://www.cbpp.org/research/public-housing.
Claudel SE, Adu-Brimpong J, Banks A, Ayers C, Albert MA, Das SR, et al. Association between neighborhood-level socioeconomic deprivation and incident hypertension: A longitudinal analysis of data from the Dallas heart study. Am Heart J. 2018;204:109–18.
Powell-Wiley TM, Cooper-McCann R, Ayers C, Berrigan D, Lian M, McClurkin M, et al. Change in Neighborhood Socioeconomic Status and Weight Gain: Dallas Heart Study. Am J Prev Med. 2015;49(1):72–9.
Acknowledgements
Not applicable.
Funding
KDG receives NIH Training Grant support (T32DK007028). KCF and ANT receive NIH R01 grant support (DK124145). ANT receives NIH K24 grant support (HL163073).
Author information
Authors and Affiliations
Contributions
KDG and ANT contributed to the conception and design of the narrative review. KDG and KCF collected, organized, and interpeted the research articles, and wrote the main manuscript text. ANT performed critical revision of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gu, K.D., Faulkner, K.C. & Thorndike, A.N. Housing instability and cardiometabolic health in the United States: a narrative review of the literature. BMC Public Health 23, 931 (2023). https://doi.org/10.1186/s12889-023-15875-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15875-6