Abstract
Background
Men who have sex with men and women (MSMW) are the most important bridge population for HIV transmission. Condom use plays an important role for HIV infection. However the predictors for condom ues with females are not well characterized.
Methods
This was a cross-sectional study. Participants were enrolled by four community-based organizations (CBOs) by offline (bathrooms, bars), and online (gay applications, chat room) from April to December 2019. Electronic questionnare was fulfilled after a face-to-face training led by CBOs. We identified predictors of inconsistent condom use with females by creating a risk score based on regression coefficients. We externally validated this score via an independent cross-sectional survey conducted in Zhejiang Province in 2021. A total of 917, 615 MSMW were included in analysis in 2019 and 2021, seperately.
Results
Among 917 MSMW, 73.2% reported heterosexual behavior in the prior 6 months and 38.3% reported inconsistent condom use with females (ICUF) over that time. Compared with heterosexual/unsure MSMW, bisexual MSMW reported more male and female sex partners, higher proportion of inconsistent condom use with males, less commercial sex with males (p < 0.05). Four risky predictors of ICUF were identified: Duration of local residence ≦6 months; more than one male partner in the prior 6 months; inconsistent condom use with males in the prior 6 months; and never heard post-exposure prophylaxis (PEP). The proportions of respondents indicating ICUF in the low- (0), medium- (2–4) and high-risk (6–20) groups (according to our risk scoring system) were 11.7% (14/120), 26.9% (96/357), and 78.1% (125/160), respectively (Ptrend < 0.001). In the validation survey, the respective proportions of those reporting ICUF were 13.4% (15/112), 17.8% (24/185) and 87.3% (96/110) (Ptrend < 0.001).
Conclusions
We developed and validated a predictive risk score for ICUF among MSMW; four factors were identified, of which inconsistent condom use with men was the most important. Risk reduction intervention programs should focus on MSM who report inconsistent condom use with males, never heard PEP, having multiple partners and living in local less than 6 months.
Similar content being viewed by others
Background
Globally, men who have sex with men (MSM) continue to be disproportionately affected by human immunodeficiency virus (HIV) [1, 2]. Homosexual behavior is an important route of HIV transmission in Zhengjiang province, China which reoported an estimated 400,000 MSM [3,4,5]. Although the reported prevalence of HIV among men who have sex with men and women (MSMW) could be lower or higher than that among men who have sex with men only (MSMO), most studies found no difference between the two groups [6, 7]. Compared with MSMO, MSMW has led to another public health crisis regarding HIV transmission among heterosexuals. Resarches showed that the HIV prevalence among women have increased significantly, and is now as high as 28% [8, 9]; The infection of spouses and offspring caused by female infections can have a huge impact on both families and society. Furthermore, the population size of this group was not small. Studies found that 13 ~ 30% of MSM were self-reported men who have sex with men and women (MSMW) in China and the United States [6, 10,11,12]. Therefore, the public health risks brought by the MSMW population should also be taken seriously.
Research on MSMW has increased since 2006, when the HIV prevalence increased sharply worldwide. Recent studies have documented differences in demographic characteristics, risky sexual behavior, material abuse, physical health, HIV testing, and HIV infection among MSMW and MSMO [13,14,15]. The topic of condom use has always been the focus of AIDS related research for high risk population [16, 17]. However, few recent studies have focused on predictors of condom use when MSMW are with females or on interventions that target this hard-to-reach subgroup. Lack of research leads to insufficient policy strategies for promotion of condom use. China also faces the same problem, with almost no prevention and control strategies specifically targeting MSMW.
In this study, we aimed to detecting risky factors for inconsistant condom use with females among MSMW and develop a prediction model for identifying MSMW who transmit HIV to female partners. For prediction model, reference revealed that risk classification models can uncover independent predictors with high efficiency by risk score [18,19,20]. We tested the performance of the model via two independent studies conducted in Zhejiang Province. In addition, we explored the role of sexual orientation in this research. The study will provide recommendations for the identification of MSMW populations at risk of transmission, and provide guidance for the development of intervention strategies.
Methods
Study participants and design
The eligibility criteria for inclusion in this study were: (1) biological male; (2) aged 18 years or older; (3) anal or oral intercourse with a male at least once, and (4) consent to participate in the study. Those with mental retardation or inability to complet informed consent were excluded from the study.
It was a cross-sectional study. The study was complimented in four cities (Ningbo, Taizhou, Jinhua, and Jiaxing) wihich contained 60% of all MSM in Zhejiang province between April and December 2019. Four local community-based organizations (CBOs) in four cities were responsible for subjects recruitment. For convenient sampling, recruitment advertisements were posted in places where MSM gathered both offline( bathrooms, bars, parks) and online (gay applications, online chat rooms) throughout the recruiment period. Enrollment intervies were arranged in CBOs studio. At the enrollment visit, basic information was obtained and eligibility was confirmed.
Participants were asked to scan a two-dimensional code with their cellphone, and were directed to an electronic questionnaire. Electronic informed consent was obtained before the questionnaire could be completed. All participants received a face-to-face training from interviewers and then completed the questionnaire by their own in a separate room. Following the survey, participants received HIV/STI prevention risk-reduction counselling.
The sample size was caculated by PASS software (ver. 11.0; NCSS, LLC. Kaysville, UT, USA). The rate of inconsistent condom use with females, which ranges from 30 to 60%, was considered to caclulate the sample size. The minimum sample size was estimated at 631 people, with an α of 0.1 and β of 0.1.
Cellphone numbers were collected to check for duplicates, and 22 duplicate participants were identified..After removing 34 participants who did not complete the questionnair and the 22 duplicates, we enrolled 2,026 MSM. Of these, 917 were included in analysis; all self-reported that they were bisexual or heterosexual (or unsure) and had ever engaged in sex with both women and men.
Electronic questionnair was designed by National Center for AIDS/STD Control and Prevention. Information on demographic charactoristics, sexal behaivor, health seeking behavior were collected. CBOs were Responsible for conducting investigation in their studios.
Predictor variables
The participants’ demographic characteristics were obtained, including age, registered permanent residence, length of residence in the local area, educational attainment, monthly income, marital status, and sexual orientation. Risky behavior was also assessed based on sex with males, sex with females, commercial sex with males, and condom use. Inconsistent condom use was deemed as “having sexual intercourse with no condom in the prior 6 months”. Regarding health interventions, the questions were as follows: “Have you received a message on MSM mental health via the app Blued in the last 6 months?”; “Have you ever undergone HIV testing?”; and “Have you heard about post-exposure prophylaxis (PEP)?”.
Outcome measure
The outcome measure was inconsistent condom use with females (ICUF) in the prior 6 months, which was determined by the question “How often have you used condoms during sexual intercourse with women in the prior 6 months?”. “Used condom every time” was deemed as “consisitent condom use”. “Used condom some time or never uses” was deemed as inconsistent condom use.
Cross-sectional validation study
External validation was performed in an independent cross-sectional study conducted from January to July 2021. This survey enrolled 1,393 MSM and 615 MSMW who met the criteria mentioned above. Of these, 407 who reported heterosexual behavior in the prior 6 months were identified. The enrollment and investigation methods were the same as in the original study of 917 MSMW conducted in the same area.
Statistical analysis
SPSS software (ver. 20.0; SPSS Inc., Chicago, IL, USA) was used to analyze the data. Descriptive analyses were generated to describe the demographic characteristics of all subjects. The chi-square test was used to examine differences between bisexual MSMW and those who were unsure/heterosexual. A binary logistic regression model was used to evaluate risk factors and calculate odds ratios (ORs) in univariable analyses. All variables in the binary logistic regression model were also included in the multivariate model (backward logistic regression) to identified the independent factors of ICUF. Missing data were not included in the analysis, but are shown in the table and Figure. Confidence intervals (CI) and 2-sided P-values less than 0.05 were considered to indicate statistical significance.
We developed our risk score based on the literature [18, 19]. Points were assigned to each predictor variable based on the regression coefficients in the multivariate analysis. To validate the model, we conducted a validation study in 2021. Risk scores were generated for all subjects, who were categorized into low-, medium-, and high-risk groups accordingly. The chi-square test was used to compare inconsistent condom use among the three groups.
Results
Demographic characteristics of MSMW
Of 917 MSMW, more than one-third were older than 35 years (36.1%) and 27.9% had an educational level of college or above. 51.6% MSMW lived in Zhejiang and 83.9% had lived in the local area for more than 6 months. In total, 61.0% self-reported that they were bisexual, 7.2% (66) heterosexual, and 31.8% (292) unsure.
Table 1 compares the social demographics between bisexual and unsure/heterosexual MSMW. The groups differed significantly in age (χ2 = 39.831; p < 0.001), educational attainment (χ2 = 20.542; p < 0.001), and marital status (χ2 = 51.018; p < 0.001). There was no significant difference in terms of registered permanent residence, duration of local residence, or monthly income.
Status of Risky sexual behaviors
In the prior 6 months, 68.8% reported homosexual and 73.2% heterosexual behavior. Among those reporting sex with both males and females, the inconsistent condom use rates were 32.8% and 38.3%, respectively. Furthermore, 11.7% reported commercial sex with males.
Table 2 compares the risky sexual behaviors in the prior 6 months between bisexual and unsure/heterosexual MSMW. The groups differed significantly in terms of the number of male partners (χ2 = 69.122; p < 0.001), condom use during anal sex with males (χ2 = 13.740; p < 0.001), sex with female partners (χ2 = 10.256; p < 0.001), and commercial sex with males (χ2 = 6.646; p = 0.010).
Develeopment of predictive risk score
Of the 671 MSMW who had sex with females in the prior 6 months, six of 10 variables were associated with ICUF on univariate analyses (Table 3).
On multivariate analysis, four variables predicted ICUF: A duration of local residence ≤ 6 months (adjusted odds ratio [aOR], 1.889; 95% confidence interval [CI], 1.156–3.087), and more than one male partner in the last 6 months (aOR, 2.203; 95% CI, 1.306–3.718). Compared to consistent condom use with males, inconsistent condom use significantly increased the risk of ICUF (aOR, 27.780; 95% CI, 15.582–49.529). Compared to MSMW who had heard of PEP, those who had not were more likely to report ICUF (aOR, 1.968; 95% CI, 1.275–3.038) (Table 4).
Participants with durations of local residence ≤ 6 months, with more than one male partner in the last 6 months, and who were unfamiliar with PEP were awarded 2 points on our risk score, respectively. Participants who reported inconsistent condom use with a male in the last 6 months and no sex with males were awarded 10 and 4 points (Table 4).
Independent validation by cross-sectioanl study
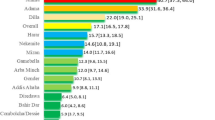
The proportions of respondents indicating ICUF in the low- (0), medium- (2–4) and high-risk (6–20) groups were 11.7% (14/120), 26.9% (96/357), and 78.1% (125/160), respectively (χ2 = 143.15, Ptrend < 0.001). The C-statistic was 0.823 (95% CI, 0.789–0.858) (Fig. 1).
In the 2021 validation study, of the 407 MSMW who reported heterosexual behavior in the last 6 months, 135 (33.2%) reported ICUF. The proportion of ICUF was 13.4% (15/112), 17.8% (24/185) and 87.3% (96/110) in the low-, medium-, and high-risk groups, respectively (χ2 = 135.188, Ptrend < 0.001). The C-statistic was 0.846 (95% CI, 0.798–0.894) (Fig. 1).
Discussion
Study in Tokyo showed that inconsistent condom use was reported by 37% of participants with regular male partners, 18% with casual male partners, and 20% with female partners [21]. Studies in the USA and Africa had found that MSMW are less likely to use condoms with their female than male partners [10, 22]. We found that the proportions of inconsistent condom use with females was higher than that in other reseaches and no difference of condom use was found between with males and females. Culture leads to Chinese people not being good at communicating on condom issues, especially among Chinese women. These risky behaviors need to be considered in surveillance systems to evaluate HIV transmission.
A prediction risk classification model was become popular in these years to predict the. incidence of other chronic disease and motality among HIV patients [23, 24]. In thisstudy, we applied this method to explore the predictor of condom use with females among MSMW. The risk classification model was conducted which contained 4 variables with differente risk score. Then we verified the effectivenss of this model by scoring, grouping, and conducting trend chi square tests of condom use with females on the subjects in 2019 and 2021. The results showed that length of local residence, number of male partner, condom use of annual sex and ever heard PEP were predictors of condom use with females and condom use of annual sex was the highest predictive value.
For sex with women, factors promoting condom use include disclosure of HIV serostatus to female partners, racial pride, stigma, and couple consultations [25,26,27,28]. We hypothesized that the factors affecting condom use when MSMW were with males and females would be both different and independent. However, our study showed that inconsistent condom use with males was the most important risk factor for ICUF with the highest risk score. MSM had special subculture of condom use in these years as the development of HIV prevention and their psychological characteristics [29]. MSMW is more vulnerable to condom culture than heterosexuality men which will also impacted condom use with females. Furthermore, MSMW reported insertions into males, which might be the reason for consistent condom use behavior between males and females [10]. Thus, interventions promoting condom use with males (knowledge of HIV, the attitude to condoms, self-efficacy, intention, and being skilled in the use of condoms) might prevent ICUF [30].
Living in local residence less than 6 months, having more than one male partners and never heard PEP were predictors of ICUF with the same risk score. The Province is economically well-developed in China and a large amount of funds and manpower are invested for MSM intervention. The three “90%” strategy are improved rapidly in these years with 86%, 95% and 97% in the province in 2022 [31]. MSM intervention is prioritized by CBOs online by dating apps and offline in bars, parks et al. MSM in the province can get high quality HIV/AIDS intervention, testing and treatment services. In the province, almost 40% residence are migrant from other economically underdeveloped province for work. Those living in the province less than 6 months have received far less HIV intervention services, and their awareness of safe sex is weak.
PEP, as a biological intervention, plays a very important role in HIV prevention and control [32, 33]. MSM in Chinese reported lower rate of PEP knowlege than in many countries [33]. The relationship between PEP awareness and condom use may be confusing, but it can be interpreted from a health awareness perspective. Those never hearding PEP might be kind of poplulation who are not aware of HIV infection, or have just entered the gay group who have not received enough HIV intervention. This kind of group always report risky sexual behavior, whatever with male or females. We suggest further research to detecte deep reseaon of condom use with females considering more factors.
Notably, we found no relationship between ICUF and interventions on dating app “Blued”. An digital technologies are commonly used based on apps, such as "Wechat", "Tencent", "Blued" in China [34]. App “Blued” is an dating app for finding sexual partners targating MSM and always used by govenment for HIV intervention. In fact, intervention on condom use was complimented in the recent ten years, but not special for MSMW, which could be responsible for the result. So, it should be considered the strategy targeting MSMW should be considered by govenment and make good use of internet.
Bisexual MSM are the principal bridge group for HIV transmission to females [35, 36]. In this study, compared to bisexual MSMW, heterosexual/unsure MSMW were more likely to be younger, less well-educated, and unmarried. Heterosexual/unsure MSMW reported less risky behavior with males and females in the last 6 months, more consistent condom use with males, and more commercial sex. Moreover, MSMW who are unsure of their sexual orientation also need attention; Support from family, relatives, friends, govenment was minimal and risky behavior might be high, given the traditional Chinese family culture [25, 37].
Limitations and strengths: This study had several limitations. First, the participants might not be representative of all MSM and MSMW populations in Zhejiang Province. MSMW were not randomly sampled, instead taking part on a volunteer basis (self-selection); this may have caused selection bias. Second, due to the cross-sectional design, causality could not be inferred; thus, a cohort study is needed to validate our findings. Finally, some predictors of heterosexual behavior and unprotected sex with women may have been missed. Further research should include psychological, sexual, cultural, and additional behavior indicators. As a strength of the study, to minimize bias, the introductory section of the questionnaire emphasized the need for commitment from the participant to ensure high-quality data. Also, all questionnaires were checked and revised if input errors or missing data were identified.
Conclusion
A relatively high rate of heterosexual behavior was observed among MSM in Zhejiang Province. We identified four predictors of ICUF in MSMW, of which inconsistent condom use with men was the most important. In an independent cross-sectional study, the high-risk group had high a rate of ICUF. Risk reduction intervention programs should focus on MSM who report commercial sex with men; these individuals are likely to engage in both heterosexual behavior and unprotected sex.
Availability of data and materials
The data that support the study findings are available from the corresponding author upon reasonable request.
Abbreviations
- MSMW:
-
Men who have sex with men and women
- MSMO:
-
Men who have sex with men only
- ICUF:
-
Inconsistent condom use with a females
- CBOs:
-
Community-based organizations
- MSM:
-
Men who have sex with men
- ORs:
-
Odds ratios
- CI:
-
Confidence intervals
- PEP:
-
Post-exposure prophylaxis
References
Beyrer C, Baral SD, Collins C, Richardson ET, Sullivan PS, Sanchez J, et al. The global response to HIV in men who have sex with men. Lancet. 2016;388(10040):198–206. https://doi.org/10.1016/S0140-6736(16)30781-4.
Raymond HF, Al-Tayyib A, Neaigus A, Reilly KH, Braunstein S, Brady KA, et al. HIV among MSM and heterosexual women in the United States: an ecologic analysis. J Acquir Immune Defic Syndr. 2017;75(3):S276–80. https://doi.org/10.1097/QAI.0000000000001422.
Bai JY, Ning TL, Zhou N, Guo Y, Yu MH. HIV infection status and related factors in men who have sex with men in sentinel surveillance in Tianjin, 2016–2018. Chin J Epidemiol. 2019;40(9):1106–1106. https://doi.org/10.3760/cma.j.issn.0254-6450.2019.09.016.
Yang H, Ye L, Su L, Liu Y, Xiao L, Hu Y, et al. An analysis on incidence of HIV-1 epidemics among men who have sex with men in Sichuan Province during 2011–2015. Chin J Prev Med. 2019;53(3):327–327. https://doi.org/10.3760/cma.j.issn.0253-9624,2019.03.018.
Hu MG, Xu CD, Wang JF. Spatiotemporal analysis of men who have sex with men in mainland China: social app capture-recapture method. JMIR mhealth and uhealth. 2020;8(1):e14800. https://doi.org/10.2196/14800.
Martín-Sánchez M, Case R, Fairley C, Hocking JS, Bradshaw C, Ong J, et al. Trends and differences in sexual practices and sexually transmitted infections in men who have sex with men only (MSMO) and men who have sex with men and women (MSMW): a repeated cross-sectional study in Melbourne, Australia. BMJ Open. 2020;10(11):e037608. https://doi.org/10.1136/bmjopen-2020-037608.
Bowring AL, Veronese V, Doyle JS, Stoove M, Hellard M. HIV and sexual risk among men who have sex with men and women in Asia: A systematic review and meta-analysis. AIDS Behav. 2016;20(10):2243–3226. https://doi.org/10.1007/s10461-015-1281-x.
Chow EP, Wilson DP, Zhang L. What is the potential for bisexual men in China to act as a bridge of HIV transmission to the female population? Behavioural evidence from a systematic review and meta-analysis. BMC Infect Dis. 2022;11(1):242. https://doi.org/10.1186/1471-2334-11-242.
Li X, Zhang B, Wang J, Li Y, Li X, Yu P, et al. Sexual health status of women who have regular sexual relations with men who have sex with men in mainland China. BMC Public Health. 2017;17(1):168. https://doi.org/10.1186/s12889-017-4096-z.
Shadaker S, Magee M, Paz-Bailey G, Hoots BE. Characteristics and risk behaviors of men who have sex with men and women compared with men who have sex with men-20 US cities, 2011 and 2014. J Acquir Immune Defic Syndr. 2017;75(Suppl 3):S281–7. https://doi.org/10.1097/QAI.0000000000001403.
Hu Y, Zhong XN, Peng B, Zhang Y, Liang H. Comparison of depression and anxiety between HIV-negative men who have sex with men and women (MSMW) and men who have sex with men only (MSMO): a cross-sectional study in Western China. BMJ Open. 2019;9(1):e023498. https://doi.org/10.1136/bmjopen-2018-023498.
Lin X, Chi P, Zhang L, Zhang Y, Fang X, Qiao S, et al. Disclosure of HIV serostatus and sexual orientation among HIV-positive men who have sex with men in China. Community Ment Health J. 2016;52(4):457–65. https://doi.org/10.1007/s10597-015-9879-z.
Jeffries WL, Johnson OD. Internalized Homonegativity and Substance Use Among U.S. Men who have sex with men only (MSMO) and men who have sex with men and women (MSMW). Subst Use Misuse. 2018;53(4):559–64. https://doi.org/10.1080/10826084.2017.1347185.
Mirandola M, Gios L, Sherriff N, Pachankis J, Toskin I, Ferrer L, et al. Socio-demographic characteristics, sexual and test-seeking behaviours amongst men Who have sex with both men and women: results from a bio-behavioural survey in 13 european cities. AIDS Behav. 2017;21(10):3013–302. https://doi.org/10.1007/s10461-017-1831-5.
Gaines MT, McCree DH, Gaul Z, Henny KD, Hickson DA, Sutton MY. Comparison of selected sociodemographic characteristics and sexual risk behaviors of black/african american men who have sex with men only and men who have sex with men and women, southeastern United States, 2013–2016. J Racial Ethn Health, Disparities. 2020;7(1):84–9. https://doi.org/10.1007/s40615-019-00636-2.
MohammadiGharehghani MA, Khosravi B, Irandoost SF, Soofizad G, Yoosefi LJ. Barriers to condom use among female sex workers in Tehran, Iran: a qualitative study. Int J Women’s Health. 2020;12:681–9. https://doi.org/10.2147/IJWH.S260481.
Ochonye B, Folayan MO, Fatusi AO, Bello BM, Ajidagba B, Emmanuel G, et al. Sexual practices, sexual behavior and HIV risk profile of key populations in Nigeria. BMC Public Health. 2019;19(1):1210. https://doi.org/10.1186/s12889-019-7553-z.
Sullivan LM, Massaro JM, D’Agostino RB Sr. Presentation of multivariate data for clinical use: the Framingham study risk score functions. Stat Med. 2004;23:1631–60.
Martinez L, Cheng W, Wang XX, Ling F, Mu L, Li C, et al. A risk classification model to predict mortality among laboratory-confirmed avian influenza A H7N9 patients: a population-based observational cohort study. J Infect Dis. 2019;220(11):1780–9. https://doi.org/10.1093/infdis/jiz328.
Rassi A, Little WC, Xavier SS, Rassi SG, Rassi AG, Rassi GG, et al. Development and validation of a risk score for predicting death in Chagas’ heart disease. N Engl J Med. 2006;355(8):799–808.
Hill AO, Bavinton BR, Armstrong G. Prevalence and factors associated with inconsistent condom use among men who have sex with men (MSM) who use mobile geo-social networking applications in Greater Tokyo. Int J Environ Res Public Health. 2018;15(12):1–15. https://doi.org/10.3390/ijerph15122815.
Alcala-Alezones C, Sandfort TGM, Serafino S, Reddy V. South african men who have sex with both men and women and how they differ from men who have sex with men exclusively. J Sex Res. 2018;55(8):1048–55. https://doi.org/10.1080/00224499.2018.1437117.
Laher AE, Paruk F, Venter WDF, Ayeni OA, Motara F, Moolla M, et al. Development and internal validation of the HIV In-hospital Mortality Prediction (HIV-IMP) risk score. HIV Med. 2022;23(1):80–9. https://doi.org/10.1111/hiv.13159.
Schulz CA, Mavarani L, Reinsch N, Albayrak-Rena S, Potthoff A, Brockmeyer N, et al. Prediction of future cardiovascular events by Framingham, SCORE and asCVD risk scores is less accurate in HIV-positive individuals from the HIV-HEART Study compared with the general population. HIV Med. 2021;22(8):732–41. https://doi.org/10.1111/hiv.13124.
Friedman MR, Bukowski L, Eaton LA, Matthews DD, Dyer TV, Siconolfi D, et al. Psychosocial health disparities among black bisexual men in the U.S.: effects of sexuality nondisclosure and gay community support. Arch Sex Behav. 2019;48(1):213–22. https://doi.org/10.1007/s10508-018-1162-2.
Yan HJ, Cao WG, Mo P, Huan X, Wang Z, Lin X, et al. Prevalence and associated factors of HIV serostatus disclosure to regular female sex partners among HIV-positive men who have sex with both men and women in China. AIDS Care. 2019;31(8):1026–34. https://doi.org/10.1080/09540121.2019.1612002.
Perez-Brumer AG, Passaro RC, Oldenburg CE, Garcia J, Sanchez J. Homophobia and heteronormativity as dimensions of stigma that influence sexual risk behaviors among men who have sex with men (MSM) and women (MSMW) in Lima, Peru: a mixed-methods analysis. BMC Public Health. 2019;19(1):1471–2458. https://doi.org/10.1186/s12889-019-6956-1.
Dangerfeld DT, Harawa NT, Smith LR, Jeffries WL, Baezconde-Garbanati L, Bluthenthal R. Latent classes of sexual risk among black men who have sex with men and women. Arch Sex Behav. 2018;47(7):2071–80. https://doi.org/10.1007/s10508-017-1142-y.
Ofreneo MAP, Gamalinda TB, Canoy NA. Culture-embedded drivers and barriers to (non) condom use among Filipino MSM: a critical realist inquiry. AIDS Care. 2020;33(11):1–6. https://doi.org/10.1080/09540121.2020.1801979.
Li MJ, Frank HG, Harawa NT, Williams JK, Chou CP, Bluthenthal RN. Racial pride and condom use in post-incarcerated African-American men who have sex with men and women: test of a conceptual model for the men in life environments intervention. Arch Sex Behav. 2018;47(1):169–81. https://doi.org/10.1007/s10508-016-0734-2.
Chen L, Luo MY, Xu Y, Xia Y, Zhou X, Chen WJ, et al. The first 90: progress in HIV detection in Zhejiang Province, 2008–2018. PLoS ONE. 2021;16(4):1–10. https://doi.org/10.1371/journal.pone.0249517.
Luo Q, Luo Y, Li T, Cui T. An integrated online-to-offline model for HIV post-exposure prophylaxis (O2O-PEP) scale-up among men who have sex with men (MSM): Protocol for developing a pilot randomized controlled trial. Front Public Health. 2022;10:102613. https://doi.org/10.3389/fpubh.2022.1026137.
Wang H, Pan XH, Wang LY, Chen L, Zhou X, Jiang TT, et al. Willingness of post-exposure prophylaxis and possible related factors in men who have sex with men. Zhonghua Liu Xing Bing Xue Za Zhi. 2021;42(6):1071–5. https://doi.org/10.3760/cma.j.cn112338-20200609-00822.
Luo ZZ, Chen WY, Ding Y, Chen JH, Wu QH, Tang WM, et al. Effect of behavioral intervention based on social media to promote HIV/syphilis testing in young men who have sex with me. Zhonghua Liu Xing Bing Xue Za Zhi. 2022;43(6):892–7. https://doi.org/10.3760/cma.j.cn112338-20211101-00840.
Lauby J, Milnamow M, Oseph HA, Hitchcock S, Carson L, Pan Y, et al. Evaluation of project RISE, an HIV prevention intervention for black bisexual men using an ecosystems approach. AIDS Behav. 2018;22(1):164–77. https://doi.org/10.1007/s10461-017-1892-5.
Arnold EA, Kegeles SM, Pollack LM, Neilands TB, Cornwell SM, Stewart WR, et al. A randomized controlled trial to reduce HIV-related risk in African American men who have sex with men and women: the bruthas project. Prev Sci. 2019;20(1):115–25. https://doi.org/10.1007/s11121-018-0965-7.
Painter TM, Song EY, Mullins MM, Mann-Jackson L, Alonzo J, Reboussin BA, et al. Social support and other factors associated with HIV testing by Hispanic/Latino gay, bisexual, and other men who have sex with men in the U.S. South. AIDS Behav. 2019; 23(Suppl 3):251–265. https://doi.org/10.1007/s10461-019-02540-6. The English in this document has been checked by at least two professional editors, both native speakers of English. For a certificate, please see: http://www.textcheck.com/certificate/HLstzW
Acknowledgements
The authors thank the CBOs staff for their assistance with the design of implementation plan, questionnaire and the fieldwork conducted in this study, including the Coastal, Glowworm-light, Love, and Blue-sky public welfare groups.
Funding
This work was supported as a Key Project of the National Science & Technology Pillar Program of the 13th Five-year Plan (grant no. 2018ZX10721102), and supported by Zhejiang Provincial Health Science and Technology Planning Project (2021RC048) and the Natural Science Foundation of Zhejiang Province (grant no. LQ20H260005). These monies supported the study design and implementation, data collection, and manuscript revision.
Author information
Authors and Affiliations
Contributions
LC coordinated the field, conducted quality control, performed the statistical analysis and drafted the manuscript. TT J coordinated the field research and conducted quality control. HW coordinated the field research and conducted quality control. KX conducted quality control. HH conducted quality control. RG conducted quality control. HL T conducted quality control. CL C reviewed the manuscript. QQ M coordinated the field research. JM J reviewed and revised the manuscript. All of the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Research Ethics Committee of the National Center for Disease Control and Prevention, China CDC (approval no. X180629516). Informed consent was obtained from all study participants, who signed electronical consent forms on their cellphones on enrollment.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, L., Jiang, T., Wang, H. et al. Development and validation of a risk score for predicting inconsistent condom use with women among men who have sex with men and women. BMC Public Health 23, 734 (2023). https://doi.org/10.1186/s12889-023-15672-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15672-1