Abstract
Objectives
Observational studies have revealed that socioeconomic status is associated with cardiovascular health. However, the potential causal effect remains unclear. Hence, we aimed to investigate the causal relationship between household income status and genetic susceptibility to cardiovascular-related diseases using a bidirectional Mendelian randomization (MR) study.
Methods
An MR study based on a large-sample cohort of the European population from a publicly available genome-wide association study datasets was conducted using a random-effects inverse-variance weighting model as the main standard. Simultaneously, MR-Egger regression, weighted median, and maximum likelihood estimation were used as supplements. Sensitivity analysis, consisting of a heterogeneity test and horizontal pleiotropy test, was performed using Cochran’s Q, MR-Egger intercept, and MR-PRESSO tests to ensure the reliability of the conclusion.
Results
The results suggested that higher household income tended to lower the risk of genetic susceptibility to myocardial infarction (OR: 0.503, 95% CI = 0.405–0.625, P < 0.001), hypertension (OR: 0.667, 95% CI = 0.522–0.851, P = 0.001), coronary artery disease (OR: 0.674, 95% CI = 0.509–0.893, P = 0.005), type 2 diabetes (OR: 0.642, 95% CI = 0.464–0.889, P = 0.007), heart failure (OR: 0.825, 95% CI = 0.709–0.960, P = 0.013), and ischemic stroke (OR: 0.801, 95% CI = 0.662–0.968, P = 0.022). In contrast, no association was evident with atrial fibrillation (OR: 0.970, 95% CI = 0.767–1.226, P = 0.798). The reverse MR study suggested a potentially negative trend between heart failure and household income status. A sensitivity analysis verified the reliability of the results.
Conclusions
The results revealed that the population with higher household income tended to have a lower risk of genetic susceptibility to myocardial infarction and hypertension.
Similar content being viewed by others
Introduction
According to a report by the World Health Organization, ischemic heart disease and stroke were the top two causes of mortality worldwide in 2019, accounting for 16% and 11% of deaths, respectively. Cardiovascular-related diseases (i.e., ischemic heart disease and stroke) are a major health threat to the aging population. In addition, they cause a trend of increasing morbidity in young individuals due to obesity, diabetes, and drug abuse. Over the past two decades, this trend has been reflected by an increasing incidence of ischemic stroke among young people in the United States, Sweden, France, and Denmark. Although cardiovascular-related diseases are highly prevalent, it is gratifying that with the continuous popularization of health education and secondary prevention using medications, the total number of deaths in developed countries declined from 2000 to 2019, especially among high-income populations [1, 2]. Furthermore, multiple observational studies have reported that people with superior socioeconomic status usually have a lower risk of morbidity in cardiovascular diseases or better prognosis [3]. In contrast, low-income populations may be exposed to higher risk or worse prognosis [4, 5]. This social phenomenon requires further research on the potential causal relationship between household income and cardiovascular-related disease morbidity. Unfortunately, reverse causation, measurement error, and potential bias are inherent disadvantages of observational studies that prevent clarification of the potential causal relationship. To the best of our knowledge, limited evidence exists on the causal relationship between household income status and cardiovascular disease-related morbidity, especially the lack of large-sample cohort studies.
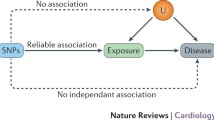
Mendelian randomization (MR) is a method that applies valuable genetic variants, such as single nucleotide polymorphisms (SNPs), as instrumental variables (IVs) to evaluate the causal effects between modifiable, non-genetic exposure factors and genetic susceptibility to diseases. In the absence of randomized controlled trials (RCTs), MR studies represent an alternative strategy for causal inference because genetic variants are randomly assigned during meiosis to simulate the RCT process. Compared with traditional observational studies, the greatest advantage of MR studies is that they are less likely to be influenced by unmeasured confounding factors because genetic variants are identified at the time of conception [6, 7]. MR studies have been successfully applied to various causal relationship analyses between behavior exposure, education, socioeconomic conditions, and various diseases [8, 9]. Hence, this research aims to identify the bidirectional causal relationship between household income status and genetic susceptibility to common cardiovascular-related diseases using an MR study.
Materials and methods
Study design and GWAS datasets information
To achieve impartial results, an MR study depends on three fundamental assumptions: (1) the selected genetic IVs must be significantly associated with the exposure factor, (2) the IVs should be independent of potential confounders associated with exposure factors and outcomes, and (3) the IVs should affect the outcomes only through the exposure factor [6]. This study conducted the MR analysis 14 times to explore the bidirectional association between annual household income status and seven cardiovascular-related diseases.
The research is based on a large-sample cohort of the European population from publicly available genome-wide association study (GWAS) datasets. The variable genetic information involved in this study was extracted from the Integrative Epidemiology Unit (IEU) GWAS database [10] (https://gwas.mrcieu.ac.uk/), which is a publicly available GWAS summary database. Therefore, the requirement for ethical committee approval was waived. The GWAS summary dataset “average total household income before tax” represented the household income status of 397,751 samples originally from the UK biobank database. The annual household income was divided into five intervals: less than 18,000 pounds, 18,000 to 30,999 pounds, 31,000 to 51,999 pounds, 52,000 to 100,000 pounds, and greater than 100,000 pounds. In contrast, cardiovascular-related diseases were represented by coronary artery disease, myocardial infarction, heart failure, atrial fibrillation, hypertension, ischemic stroke, and type 2 diabetes, respectively. Detailed information on all the GWAS datasets is listed in Table 1. The household income GWAS dataset and GWAS datasets of cardiovascular diseases originated from different consortiums to decrease the potential bias caused by sample overlap. In addition, all GWAS datasets involved in this study included populations of European ancestry to mitigate bias from population stratification.
Selection criteria for IVs
The IVs were single nucleotide polymorphisms (SNPs) filtered according to the three afore mentioned pivotal assumptions of the MR study. First, the SNPs were matched with a genome-wide statistical significance threshold (P < 5 × 10− 8). Second, the corresponding linkage disequilibrium was tested to confirm the presence of SNPs in the linkage disequilibrium state and to confirm that these SNPs were independent by trimming SNPs within a 0–10,000 kb window at a threshold of r2 < 0.001. Third, to evaluate the assumption that the IVs affect the outcomes only through the exposure factor, the potential phenotypes that may be relevant to the IVs were investigated by searching the human genotype-phenotype association database (PhenoScanner-V2, http://www.phenoscanner.medschl.cam.ac.uk/) [18]. Fourth, SNPs identified as IVs were further matched with those in the outcome GWAS dataset to establish genetic associations. The summary SNP-phenotype and SNP-outcome statistics were harmonized to ensure effect size alignment, and the palindromic SNPs were excluded. Finally, F-statistics (> 10) were used to evaluate the strength of the IVs to avoid the influence of weak instrumental bias [19].
Mendelian randomization study and sensitivity analysis
The MR study was performed using a random-effects inverse-variance weighting (IVW) model [20] as the primary standard and three other models (MR-Egger regression [21], weighted median [22] and maximum likelihood [23]) as supplements to evaluate the potential causal relationship between household income status and seven common cardiovascular-related diseases. The reverse MR study evaluated the potential causal relationship between seven common cardiovascular-related diseases and household income status using the same methods. In addition, sensitivity analysis was performed to measure the reliability and stability of the conclusion. The sensitivity analysis consisted of (1) Cochran’s Q test (according to the IVW model or MR-Egger regression model), (2) horizontal pleiotropy test using MR-Egger intercept [24] and MR-PRESSO test [25], and (3) “leave-one-out” test (each SNP was abandoned successively to repeat the IVW analysis to identify whether any specific SNP drives the causal relationship estimate). The results are reported as odds ratios (OR) with corresponding 95% confidence intervals (CI) and P-values, illustrated as scatter plots. The evidential threshold in MR analysis was defined as P-value < 0.004(0.05/14) according to the Bonferroni correction method. P-value < 0.05 but above the Bonferroni corrected evidential threshold was regarded as a potential association. Meanwhile, a P-value < 0.05 was also considered significant in the sensitivity analysis. The R 4.0.3 software, with “TwoSampleMR” [26] and “MR-PRESSO” [25] packages were used to process and visualize the study.
Results
Results of the MR study
The sample overlapping of the seven diseases GWAS dataset and UK-biobank database were as follows: coronary artery disease 0%, myocardial infarction: 73.8%, heart failure: 36.96%, atrial fibrillation: 38.4%, hypertension: 0%, stroke: 0%, and type 2 diabetes: 9.8%, respectively. Even though the sample overlapping rate of myocardial infarction is comparatively high, we have followed the sample size and timeliness priority to make the best choice as much as possible.
The numbers of SNPs that ultimately identified as IVs in different outcome datasets were 35 (type 2 diabetes), 43 (coronary artery disease, myocardial infarction, heart failure and hypertension), 44 (ischemic stroke), and 45 (atrial fibrillation) respectively. The F-statistic score of all these selected SNPs were more than 10 (coronary artery disease:57.76, myocardial infarction:57.87, heart failure:57.76, hypertension:57.77, atrial fibrillation:57.52, ischemic stroke:57.76, type 2 diabetes:58.44, respectively), indicating a low risk of weak-instrument bias.
According to the random-effects IVW model results, as the primary standard, higher household income tended to lower the risk of genetic susceptibility to coronary artery disease (OR: 0.674, 95% CI = 0.509–0.893, P = 0.005), myocardial infarction (OR: 0.503, 95% CI = 0.405–0.625, P < 0.001), heart failure (OR: 0.825, 95% CI = 0.709–0.960, P = 0.013), hypertension (OR: 0.667, 95% CI = 0.522–0.851, P = 0.001), type 2 diabetes (OR: 0.642, 95% CI = 0.464–0.889, P = 0.007) and ischemic stroke (OR: 0.801, 95% CI = 0.662–0.968, P = 0.022). However, no evidence was reported on the potential causal relationship between household income status and atrial fibrillation (OR: 0.970, 95% CI = 0.767–1.226, P = 0.798). In addition, the results of the weighted median and maximum likelihood estimation models supported these conclusions. Unfortunately, the MR-Egger regression model results did not show statistically significant differences. In summary, according to the Bonferroni correction standard, the MR study revealed that the higher household income population tended to have a lower risk of genetic susceptibility to myocardial infarction and hypertension. It also suggested a potentially negative relationship between coronary artery disease, heart failure, type 2 diabetes, and ischemic stroke. Detailed information is displayed in the forest map in Fig. 1 and illustrated as a scatter plot (supplement Figure-1).
Results of sensitivity analyses in the MR study
The result of Cochran’s Q test indicated certain heterogeneity among the IVs in coronary artery disease, myocardial infarction, atrial fibrillation, hypertension, and type 2 diabetes (Table 2). Hence, the random effects IVW model was applied to minimize the effect of heterogeneity in the MR study as much as possible. More importantly, no horizontal pleiotropy was detected using the MR-Egger intercept and MR-PRESSO tests (Table 2). In addition, the “leave-one-out” method indicated that no specific SNP among the IVs significantly affected the overall result (supplement Figure-2). In general, the sensitivity analysis verified the robustness of the conclusions.
Results of reverse MR study and sensitivity analyses
The numbers of SNPs that ultimately identified as IVs in different cardiovascular-related diseases were 115 (type 2 diabetes), 24 (coronary artery disease), 74(myocardial infarction), 9 (heart failure), 53 (hypertension), 7 (ischemic stroke), and 111 (atrial fibrillation) respectively in the reverse MR study.
Based on the random-effects IVW model results, there were potential indications of causal association with myocardial infarction (OR: 0.982, 95% CI = 0.967–0.997, P = 0.025), heart failure (OR: 0.964, 95% CI = 0.931–0.998, P = 0.037), type 2 diabetes (OR: 0.986, 95% CI = 0.976–0.997, P = 0.013) and household income status. The results of the maximum likelihood estimation model support these conclusions. However, the results of the MR-Egger regression model and the weighted median model did not show significant statistical differences. The detailed information is displayed in Fig. 2. However, horizontal pleiotropy was detected in SNPs of myocardial infarction (P = 0.027) and type 2 diabetes (P = 0.034) using the MR-Egger intercept test in the sensitivity analysis. This resulted in a lack of stability in the conclusions. Thus, the reverse MR study’s results only suggested a potentially negative association between heart failure and household income status.
Discussion
Epidemiological studies have revealed that socioeconomic status has a non-negligible effect on cardiovascular health. Hence, household income status, as an indispensable part of socioeconomic status, has been consistently considered to be associated with the risk of cardiovascular disease [27]. However, in-depth causality needs further exploration. To the best of our knowledge, this research is the first that focuses on the causal effect between household income status and cardiovascular health using a bidirectional two-sample MR study. The results revealed that the population with higher household income status tended to have a lower risk of genetic susceptibility to myocardial infarction and hypertension, and suggested a potentially negative relationship with coronary artery disease, heart failure, type 2 diabetes, and ischemic stroke. Moreover, a reverse MR study indicated a potential negatively association between heart failure and household income status.
These conclusions were supported by accumulating evidence from cohort studies and meta-analyses. For example, Kucharska-Newton et al. summarized two independent cohorts from the US and Finland with 14 years of follow-up. They demonstrated that low-income status was significantly associated with an increased risk of major adverse cardiac events [28]. Similarly, in America and England, the aging population in low socioeconomic levels has been reported to have nearly double the cardiovascular disease-related mortality rates than that at superior socioeconomic levels [29, 30]. Moreover, Wang et al. conducted a study with 8,989 samples concentrated between income changes and cardiovascular disease risk. They concluded that changes in income might result in negative regulation of cardiovascular health over 17 years [31]. Additionally, it is worth noting that there is a bidirectional negative causal relationship between household income status and heart failure. On the one hand, low-income populations lack advanced medical treatment and quality care [32, 33]. Moreover, they neglect necessary health maintenance behaviors, such as annual medical checkups or adherence to secondary prevention medications. This may result in a worse prognosis of myocardial infarction and likely development of heart failure [34,35,36]. On the other hand, patients with heart failure have limited mobility to various degrees or disabilities in daily work that cause their income and quality of life to decline. Overall, the significant bidirectional negative causal relationship between low household income and heart failure is a complex public health concern. Therefore, policymakers for medical reimbursement should consider household income inequalities and continuously improve the fairness and accessibility to medical services for people [37].
Several relevant mechanisms which may explain the association between household income status and genetic susceptibility to cardiovascular diseases. They include: (1) low-income populations’ likelihood to consume fast foods that are more energy-dense and yield more calories for a given price [38], which creates a long-term tendency to obesity and metabolic syndromes. (2) low-income populations face greater living pressures that may increase depression and anxiety, which are ultimately linked to cardiovascular diseases [39, 40]. (3) low-income populations are more likely to face poor living environments, smoke, and engage in lifestyle behaviors such as drinking, which are already identified as risk factors for cardiovascular health [41, 42].
The biological functions of SNPs as IVs and how they affect cardiovascular health deserve further discussion. Hill et al. reported 30 independent loci associated with individual income, which may involve the biological process of GABAergic and serotonergic neurotransmission [43]. The current research indicated that dysregulation of the GABA signaling pathway was linked to psychiatric disorders, such as depression, autism, and anxiety [44, 45]. Among the 30 reported genetic loci, seven SNPs share common with the selected IVs in our study (rs11588857, rs6699397, rs32940, rs10429582, rs2332719, rs1455350, rs784256). The result enlightens us that household income status may affect the progress of cardiovascular diseases through GABA-mediated mental or psychological-related biological mechanisms. Nevertheless, more direct evidence is needed to support this assumption.
The greatest advantage of this bidirectional MR study is that our findings effectively avoided the influence of reverse causes and minimized residual confounding. However, some limitations of the study should be mentioned. First, the heterogeneity test results suggested certain heterogeneity among the IVs. Although the random effects IVW model has been applied to minimize the effect of heterogeneity in MR study as much as possible. Second, models based on different assumptions involved in MR studies have distinctive advantages and disadvantages that may increase the likelihood of obtaining inconsistent or contradictory results. Thus, this study’s results should be cautiously interpreted. Third, the sample overlapping of the myocardial infarction GWAS dataset and UK-biobank database was comparatively high, which may increase potential bias.
Conclusion
This study explored the causal relationship between household income status and cardiovascular health using a bidirectional MR study based on datasets with million samples. The results revealed that the population with higher household income status tended to have a lower risk of genetic susceptibility to myocardial infarction and hypertension and suggested a potentially negative relationship with coronary artery disease, heart failure, type 2 diabetes, and ischemic stroke. These findings strengthen that medical reimbursement should consider household income inequalities and continuously improve the fairness and accessibility to medical services for the population in low household income status.
Data Availability
The genetic variable information of single nucleotide polymorphisms (SNPs) was obtained from the IEU GWAS database (https://gwas.mrcieu.ac.uk/datasets/), a publicly available GWAS summary database.
Abbreviations
- MR:
-
Mendelian Randomization
- SNP:
-
Single Nucleotide Polymorphism
- GWAS:
-
Genome-Wide Association Study
- IV:
-
Instrumental Variable
- IVW:
-
Inverse Variance Weighting
- OR:
-
Odds Ratio
- CI:
-
Confidence Interval
References
WHO. Global Health estimates 2020: deaths by cause, Age, Sex, by Country and by Region, 2000–2019. World Health Organization Geneva; 2020.
Andersson C, Vasan RS. Epidemiology of cardiovascular disease in young individuals. Nat Reviews Cardiol. 2018;15:230–40.
Jaquet E, Gencer B, Auer R, et al. Association between income and control of cardiovascular risk factors after acute coronary syndromes: an observational study. Swiss Med Wkly. 2019;149:w20049.
Stirbu I, Looman C, Nijhof GJ, Reulings PG, Mackenbach JP. Income inequalities in case death of ischaemic heart disease in the Netherlands: a national record-linked study. J Epidemiol Commun Health. 2012;66:1159–66.
Zang Y, Zhu Z, Shi M, et al. Association between annual household income and adverse outcomes in patients who had ischaemic stroke. J Epidemiol Community Health. 2022;76:293–300.
Davies NM, Holmes MV, Davey Smith G. Reading mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ. 2018;362:k601.
Richmond RC, Davey Smith G. Mendelian Randomization: Concepts and Scope.Cold Spring Harb Perspect Med2022;12.
Tillmann T, Vaucher J, Okbay A, et al. Education and coronary heart disease: mendelian randomisation study. BMJ. 2017;358:j3542.
Harrison S, Davies AR, Dickson M, et al. The causal effects of health conditions and risk factors on social and socioeconomic outcomes: mendelian randomization in UK Biobank. Int J Epidemiol. 2020;49:1661–81.
Elsworth B, Lyon M, Alexander T et al. The MRC IEU OpenGWAS data infrastructure. bioRxiv 2020:2020.08.10.244293.
Bycroft C, Freeman C, Petkova D, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562:203–9.
Kurki MI, Karjalainen J, Palta P et al. FinnGen: Unique genetic insights from combining isolated population and national health register data. medRxiv 2022.
Hartiala JA, Han Y, Jia Q, et al. Genome-wide analysis identifies novel susceptibility loci for myocardial infarction. Eur Heart J. 2021;42:919–33.
Shah S, Henry A, Roselli C, et al. Genome-wide association and mendelian randomisation analysis provide insights into the pathogenesis of heart failure. Nat Commun. 2020;11:163.
Nielsen JB, Thorolfsdottir RB, Fritsche LG, et al. Biobank-driven genomic discovery yields new insight into atrial fibrillation biology. Nat Genet. 2018;50:1234–9.
Malik R, Chauhan G, Traylor M, et al. Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat Genet. 2018;50:524–37.
Xue A, Wu Y, Zhu Z, et al. Genome-wide association analyses identify 143 risk variants and putative regulatory mechanisms for type 2 diabetes. Nat Commun. 2018;9:2941.
Yuan S, Carter P, Bruzelius M, et al. Effects of tumour necrosis factor on cardiovascular disease and cancer: a two-sample mendelian randomization study. EBioMedicine. 2020;59:102956.
Wu F, Huang Y, Hu J, Shao Z. Mendelian randomization study of inflammatory bowel disease and bone mineral density. BMC Med. 2020;18:312.
Burgess S, Dudbridge F, Thompson SG. Combining information on multiple instrumental variables in mendelian randomization: comparison of allele score and summarized data methods. Stat Med. 2016;35:1880–906.
Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44:512–25.
Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in mendelian randomization with some Invalid Instruments using a weighted median estimator. Genet Epidemiol. 2016;40:304–14.
Nguyen LT, Schmidt HA, von Haeseler A, Minh BQ. IQ-TREE: a fast and effective stochastic algorithm for estimating maximum-likelihood phylogenies. Mol Biol Evol. 2015;32:268–74.
Burgess S, Thompson SG. Interpreting findings from mendelian randomization using the MR-Egger method. Eur J Epidemiol. 2017;32:377–89.
Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from mendelian randomization between complex traits and diseases. Nat Genet. 2018;50:693–8.
Hemani G, Zheng J, Elsworth B et al. The MR-Base platform supports systematic causal inference across the human phenome.Elife2018;7.
Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic Status and Cardiovascular Outcomes: Challenges and Interventions. Circulation. 2018;137:2166–78.
Kucharska-Newton AM, Harald K, Rosamond WD, Rose KM, Rea TD, Salomaa V. Socioeconomic indicators and the risk of acute coronary heart disease events: comparison of population-based data from the United States and Finland. Ann Epidemiol. 2011;21:572–9.
Stringhini S, Zaninotto P, Kumari M, Kivimäki M, Lassale C, Batty GD. Socio-economic trajectories and cardiovascular disease mortality in older people: the English Longitudinal Study of Ageing. Int J Epidemiol. 2018;47:36–46.
Faselis C, Safren L, Allman RM, et al. Income disparity and incident cardiovascular disease in older Americans. Prog Cardiovasc Dis. 2022;71:92–9.
Wang SY, Tan ASL, Claggett B, et al. Longitudinal Associations between Income Changes and Incident Cardiovascular Disease: the atherosclerosis risk in Communities Study. JAMA Cardiol. 2019;4:1203–12.
Yong CM, Abnousi F, Asch SM, Heidenreich PA. Socioeconomic inequalities in quality of care and outcomes among patients with acute coronary syndrome in the modern era of drug eluting stents. J Am Heart Assoc. 2014;3:e001029.
Parikh PB, Yang J, Leigh S, et al. The impact of financial barriers on access to care, quality of care and vascular morbidity among patients with diabetes and coronary heart disease. J Gen Intern Med. 2014;29:76–81.
Johnson AE, Swabe GM, Addison D, et al. Relation of Household Income to Access and Adherence to Combination Sacubitril/Valsartan in Heart failure: a retrospective analysis of commercially insured patients. Circulation Cardiovasc Qual outcomes. 2022;15:e009179.
Teng TK, Tay WT, Richards AM, et al. Socioeconomic status and outcomes in heart failure with reduced ejection Fraction from Asia. Circulation Cardiovasc Qual outcomes. 2021;14:e006962.
Eberly LA, Yang L, Eneanya ND, et al. Association of Race/Ethnicity, gender, and socioeconomic status with sodium-glucose cotransporter 2 inhibitor use among patients with diabetes in the US. JAMA Netw open. 2021;4:e216139.
Ma C, Song Z, Zong Q. Urban-Rural Inequality of Opportunity in Health Care: Evidence from China.International journal of environmental research and public health2021;18.
Mellis AM, Athamneh LN, Stein JS, Sze YY, Epstein LH, Bickel WK. Less is more: negative income shock increases immediate preference in cross commodity discounting and food demand. Appetite. 2018;129:155–61.
Freeman A, Tyrovolas S, Koyanagi A, et al. The role of socio-economic status in depression: results from the COURAGE (aging survey in Europe). BMC Public Health. 2016;16:1098.
Ridley M, Rao G, Schilbach F, Patel V. Poverty, depression, and anxiety: Causal evidence and mechanisms.Science2020;370.
Barber S, Hickson DA, Kawachi I, Subramanian SV, Earls F. Neighborhood Disadvantage and Cumulative Biological Risk among a socioeconomically diverse sample of african american adults: an examination in the Jackson Heart Study. J racial ethnic health disparities. 2016;3:444–56.
Maglalang DD, Avila JC, Ahluwalia JS, Murphy CM, Alexander AC, Nollen NL. The role of Financial strain and Educational Attainment on Smoking abstinence of African Americans and Whites who smoke. Ethn Dis. 2022;32:223–30.
Hill WD, Davies NM, Ritchie SJ, et al. Genome-wide analysis identifies molecular systems and 149 genetic loci associated with income. Nat Commun. 2019;10:5741.
Hernández-Vázquez F, Garduño J, Hernández-López S. GABAergic modulation of serotonergic neurons in the dorsal raphe nucleus. Rev Neurosci. 2019;30:289–303.
Padmakumar M, Van Raes E, Van Geet C, Freson K. Blood platelet research in autism spectrum disorders: in search of biomarkers. Res Pract Thromb haemostasis. 2019;3:566–77.
Acknowledgements
We would like to acknowledge the participants and investigators of the IEU OpenGWAS project, the UK Biological Bank and the FinnGen studies for their contributions.
Funding
The research was funded by “Affiliated Hospital of Guangdong Medical University Clinical Research Program, No. LCYJ2020A002”.
Author information
Authors and Affiliations
Contributions
Xifeng Zheng was responsible for conception and article writing, Yu Yang was responsible for data mining, Jianying Chen was involved in literature review and Bing Lu was responsible for scientific supervision. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not Applicable.
Competing interests
The authors declared that they have no conflicts of interests to this work. We declare that we do not have any commercial or associative interests that represents a conflict of interests in connection with the work submitted.
Consent for publication
Not Applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.


Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, X., Yang, Y., Chen, J. et al. Dissecting the causal relationship between household income status and genetic susceptibility to cardiovascular-related diseases: Insights from bidirectional mendelian randomization study. BMC Public Health 23, 749 (2023). https://doi.org/10.1186/s12889-023-15561-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15561-7