Abstract
Background
Tianjin is one of the cities with the highest prevalence of hypertension in China and one of the first regions to develop community management of hypertension. Our aim was to analyze the characteristics of hypertension in the last 16 years, and estimate the population attributable fraction for cardiovascular mortality in Tianjin, China.
Methods
We compared the epidemiological characteristics of hypertension between 2002 and 2018 by analyzing data from the National Nutrition and Chronic Disease Risk Factor Survey. Subsequently, we obtained the cause-specific mortality in the same year from the Tianjin All Cause of Death Registration System (CDRS), and the population attributable fraction was used to estimate the annual cardiovascular disease (CVD) deaths caused by hypertension.
Results
In 2002 and 2018, the crude prevalence, awareness, treatment rate in diagnosed, control rate in treated, and overall control rate of hypertension were 36.6% and 39.8%, 36.0% and 51.9%, 76.0% and 90.1%, 17.4% and 38.3%, 4.8% and 17.9%, respectively (P < 0.05). The mean SBP for males between the ages of 25 and 50 was significantly higher in 2018 than in 2002. The number of CVD deaths attributed to hypertension was 13.8 thousand in 2002 (account for 59.1% of total CVD deaths), and increased to 21.7 thousand in 2018 (account for 58.8% of total CVD deaths). The population attributable fraction have increased in the age groups of 25–44 and 75 and above, and decreased in the age group of 45–74 from 2002 to 2018.
Conclusions
Compare to 2002, the proportion of CVD deaths attributed to hypertension remains high, particularly among younger and older people, despite a very significant increase in treatment and control rates for hypertension in 2018.
Similar content being viewed by others
Background
High blood pressure (BP) is the leading cause of death globally and a core risk factor for cardiovascular disease (CVD). In 2017, 218 million (95% uncertainty interval [UI], 198–237 million) disability-adjusted life-years (DALYs) were attributed to high systolic blood pressure (SBP). [1] China has the largest population with hypertension and the highest total disease burden of hypertension in the world, characterized by high prevalence, low awareness, and low treatment and control rates. [1] Tianjin, a large city of over 10 million people in northern China, has one of the highest prevalence of hypertension in China, [2] and is also one of the first regions to carry out community management of hypertension. However, there were few reports on the prevalence characteristics, long-term trends of hypertension and its impact on cardiovascular disease mortality in Tianjin. Tianjin participated in the National Nutrition and Chronic Disease Risk Factors Survey [3] in 2002 and 2018 respectively. Using data from these two surveys, we analyzed the prevalence characteristics of hypertension and the trends over the last 16 years, and estimated the risk of cardiovascular mortality following the methodological framework and analytical strategy of the Global Burden of Disease (GBD) Study. [4].
Methods
Data source
Data of BP were obtained from the National Nutrition and Chronic Disease Risk Factors Survey in 2002 and 2018, including 2668 cases in 2002 and 4419 cases in 2018. The response rates were 94.3% in 2002 and 96.8% in 2018. The National Nutrition and Chronic Disease Risk Factors Survey is a nationally representative survey on the nutritional and health status of residents, organized by the National Health Commission using a multistage stratified cluster random sampling method at each point. [3, 5].
Data of cause of death in 2002 and 2018 were both obtained from the Tianjin All Cause of Death Registration System (CDRS), which was established and covered the entire population in 1984. [6] Garbage codes of cause of death were redistributed according to the well-established methods in the GBD study, [7] and all the data mapped age-, sex-, and cause-specific mortality. Based on the Comparative Risk Assessment in the GBD Study, Ischemic heart disease (IHD) (ICD-10 code: I20–I25), Ischemic stroke [ICD-10 code: I63, I65–I67 (except I67.4), I69.3], Hemorrhagic and other nonischemic stroke (ICD-10 code: I60–I62, I69.0–I69.2, I67.4), rheumatic heart disease (ICD-10 code: I01, I02.0, I05–I09), endocarditis, cardiomyopathy and myocarditis (ICD-10 code: I33, I40, I42), aorta aneurysm (ICD-10 code: I71), hypertensive heart disease (ICD-10 code: I11), atrial fibrillation, peripheral vascular disease, and other circulatory diseases [ICD-10 code: I48, I73, I70.2, I00, I02.9, I27–I28 (except I27.1), I30–I32 (except I31.2,I31.3), I34–I39, I47, I70.8, I72, I77–I80, I82–I84, I86–I98, G45] were identified as an etiological health outcomes of CVD associated with elevated BP. [7].
BP measurements and definitions
In 2002, BP was measured with standard mercury sphygmomanometer (scale range 0–300 mmHg, 1 mmHg = 0.133 kPa) with an accuracy of 2 mmHg. Systolic and diastolic blood pressures were measured 3 times by the physician according to the Korotkoff sound, and the average of the last 2 was adopted in the final analysis. In 2018, BP was measured 3 times with a HEM-7071 OMRON (OMRON Corporation, Kyoto, Japan) electronic BP meter, and the average of the last 2 times was used for the final analysis.
The main outcomes were prevalence, awareness, treatment rate in diagnosed, control rate in treated, and overall control rate of hypertension. Hypertension was defined as SBP ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg and who self-reported on antihypertensive medication within 2 weeks and who report having been diagnosed with hypertension by a health professional, according to 2010 Chinese guidelines for the management of hypertension. [8] Awareness of hypertension was defined as the percentage of people with hypertension who self-reported being diagnosed with hypertension by a doctor. Treatment rate was defined as self-reported use of a prescription medication for hypertension within 2 weeks at the time of the interview in hypertension group. Control rate was defined as whose SBP < 140 mmHg and DBP < 90 mmHg in hypertension group.
Treatment rate in diagnosed was defined as the percentage of using antihypertensive medication in the past 2 weeks in patients with diagnosed hypertension.
Control rate in treated was the percentage of control (SBP < 140 mmHg and DBP < 90 mmHg) in treated group.
Statistical analysis
Continuous variables were presented as means and 95% confidence intervals (CIs) and categorical variables were expressed as frequencies, percentages and proportions. The age-standardized rates were calculated by using the age composition of Segi’s world standard population. Pearson Chi-square was used to make between-group comparisons of categorical variables. SPSS 21.0 was used for statistical analyses. All P-values were derived from two-sided tests, and the significance level was set at P < 0.05.
We employed the comparative risk assessment framework to estimate the number of deaths for adults aged over 25 years attributable to hypertension in 2002 and 2018 in Tianjin, China. We first calculated the number of deaths by age and sex for each of the 11 types of cardiovascular diseases. Further, We obtained the relative risk (RR) for each 10 mmHg increase in SBP for each age group (25 years and older) for each health outcome from the GBD study, which used a meta-analysis based on randomized controlled trials and large cohort studies, and confounding factors were consistently adjusted. [7].
Population attributable fractions (PAFs) were calculated to obtain the proportion of CVD deaths attributable to elevated BP by comparing the observed SBP distribution with a theoretical minimum (mean of 115 mmHg with standard deviation (SD) of 6 mmHg) for each disease by sex and age group. The formula with BP treated as a continuous variable was:
where RR(x) is the relative risk at SBP level x; P(x) is the observed population distribution of SBP; P’(x) is the theoretical minimum SBP distribution (mean of 115 mm Hg with SD of 6 mm Hg); and m is the maximum amount of SBP level. [7] CVD mortality attributable to elevated BP for each disease was calculated by multiplying the PAF with the observed deaths of CVD by sex and age group (≥ 25 years).
@RISK software (version 6.1 for Excel; Microsoft Corporation, Redmond, WA) was used to calculate uncertainty ranges. We defined risk-factor exposure levels and RR values as the input variables (RR as a lognormal distribution and others as normal distributions). The attributable fractions, attributable CVD deaths, were treated as the output variables. For each of the output variables, 95% uncertainty intervals were calculated using the 1000 iteration values generated between the 2.5th and 97.5th percentile.
Results
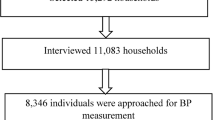
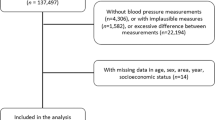
Characteristics of participants in 2002 and 2018
In 2002, there were 2668 participates, of whom 47.7% were male, 53.6% were from urban areas and 98.0% were Han ethnicity. The mean age was 46.54 ± 16.08. In 2018, there were 4419 participates, of whom 49.3% were male, 52.4% were from urban areas and 94.8% were Han ethnicity. The mean age was 48.67 ± 16.85. There were statistical significances of mean age, mean body mass index, percentage of Han ethnicity, and education attainment between 2002 and 2018 (Table 1).
Characteristics of the prevalence of hypertension in 2018
The crude prevalence, awareness rate, treatment rate, and overall control rate of hypertension were 39.8%, 51.9%, 46.8% and 17.9% among Tianjin residents in 2018, respectively. The treatment rate in diagnosed, control rate in treated were 90.1%, 38.3%. The prevalence of hypertension was higher in males (46.5%) than in females (33.2%), especially in the lower age-group, while the awareness was higher in females than in males. The prevalence, awareness rate was increasing by age. (Table 2).
Comparison of characteristics of hypertension between 2018 and 2002
The crude prevalence of hypertension was 39.8% in 2018, higher than in 2002 (36.6%) (2 = 6.5, P = 0.01). The crude awareness rate (51.9% vs 36.0%, 2 = 61.1, P = 0.000), treatment rate in diagnosed (90.1% vs 76.0%, 2 = 39.6, P = 0.000), control rate in treated (38.3% vs 17.4%, 2 = 37.2, P = 0.000)and overall control rate (17.9% vs 4.8%, 2 = 88.4, P = 0.000) all increased significantly in 2018 compared to 2002 (Fig. 1.A). For the age-adjusted rates, the prevalence (33.0% vs 32.0%, 2 = 14.4, P = 0.000), awareness rate (29.7% vs 24.5%, 2 = 469.4, P = 0.000), treatment rate in diagnosed (69.7% vs 58.5%, 2 = 1871.4, P = 0.000), control rate in treated (25.2% vs 21.3%, 2 = 285.9, P = 0.000) and overall control rate (9.6% vs 3.4%, 2 = 2226.5, P = 0.000) also increased significantly in 2018 compared to 2002.
In 2018, the mean SBP was significantly higher in 2018 than in 2002 for males between the ages of 25 and 50, and that was basically the same for males over 50 years (Fig. 1.B). The mean SBP was higher in 2018 than in 2002 for females in the age groups of 25–29, 30–34, 40–44, and 80 and older (Fig. 1.C).
CVD deaths attributed to hypertension in 2002 and 2018
In 2002, 13.8 thousand CVD deaths (account for 59.1% of total CVD deaths) were attributed to hypertension, including 5.7 thousand IHD, 7.7 thousand stroke and 0.4 thousand other CVDs. In 2018, a total of 21.7 thousand CVD deaths were attributed to hypertension, including 11.8 thousand IHD, 9.7 thousand strokes and 0.2 thousand other CVDs, which accounts for 58.8% of total CVD deaths. Both attributing number and ratio of male’s were higher than female’s (12.0 thousand versus 9.8 thousand, 60.1% versus 57.5%) (Table 3).
In 2002 and 2018, the attribution ratios were 51.2% and 61.3%, 66.5% and 66.0%, 62.5% and 59.3%, and 54.7% and 57.7% for the age groups of 25–44, 45–59, 60–74, and 75 years and older, respectively. The attribution ratios have increased in the age groups of 25–44 and 75 and above, and decreased in the age groups of 45–74 from 2002 to 2018 (Fig. 2). The attributing number of 75 and above age group was extremely higher in 2018 than in 2002 (13.7 thousand vs 5.9 thousand).
Discussion
In this study, we found a high prevalence of hypertension and a large attribution to the burden of CVD, although the awareness, treatment, and control rates of hypertension have improved tremendously over the past 16 years in Tianjin, China.
Our results showed that the prevalence of hypertension in Tianjin in 2018 was much higher than the national level (23.2%, from 2012 to 2015). [2] Previous studies have shown that the higher incidence and prevalence of hypertension in northeastern and eastern China compared to western China [2, 9] may be closely associated with higher salt intake, obesity rates and higher body weight. In 2017, high sodium intake was the leading dietary risk for deaths and high DALYs in China. [10] About 98.7% of residents consume more than 6 g/day of salt, which was 3–4 times higher than the average standard in Tianjin in 2015. [11] Besides, Tianjin also has the highest obesity rate in China, with an adult obesity rate of 12.2%, [12] which is also a major risk factor for hypertension.
The study showed that the awareness, treatment and control rates of hypertension among Tianjin residents have improved significantly, although the prevalence of hypertension among Tianjin residents has shown a slight upward trend over the past 16 years, which was consistent with previous studies [2, 13,14,15]. Over the past 20 years, the prevalence of hypertension had declined in some high-income countries, [16,17,18,19] but had increased in low- and middle-income countries, including China, [13,14,15] which largely due to the prevalence of unhealthy lifestyles as a result of rapid economic development and the acceleration of the aging process. [2] Comparing the population characteristics of the two surveys, we found that the mean age, mean BMI and education level were all higher in 2018 than in 2002, which may partly explain the changes in the prevalence characteristics of hypertension. The prevalence of hypertension was higher in the elderly and in people with high BMI, while higher levels of education were usually accompanied by higher levels of awareness.
However, the increase of awareness, treatment, and control rates may be closely related to the improvement of community public health service level. Since 2007, China has gradually incorporated the management of hypertensive patients into community public health services. [20, 21] Community doctors provide free follow-up management for patients four times a year. At present, over 90% of patients with hypertension and diabetes use community public health services. [22] Another reason may be related to the significant improvement of medical insurance coverage rate. [23] The medical insurance coverage rate in China was only 10% in 2003, but it raised to 96.7% by 2019. [24] This could provide more medical insurance for residents to manage their hypertension. However, the awareness and control rates of hypertension among Tianjin residents were still far below that of developed countries, [25] especially among the 18–45 age group, where the awareness rate was only 14.25%, compared to 74.7% in the United States. [26].
Although the treatment rate in diagnosed to be a high level, the control rate is still relatively low. Fixed-dose combination therapy can help to improve the control rate of treated hypertensive patients. [27] However, the proportion of single-drug use in Tianjin was 62.97%, and the proportion of combination drugs was lower, even in patients with grade 2 and 3 hypertension. [28] So, we should promote the “National Clinical Practice Guidelines on the Management of Hypertension”, [29] especially in community public health services.
A new finding in our study was that the mean SBP in males increased most in the 25–50 age-group, but the awareness rate was lower, a phenomenon that needs to be given adequate attention. This may be mainly due to the prevalence of higher BMI, lower physical activity levels, higher red meat intake, [30] smoking, excessive alcohol consumption, and higher dietary sodium intake in males. [10, 31, 32]. A study showed that elevated SBP was a major predictor of CVD events regardless of whether diagnostic criteria for hypertension were met. [33] Previous studies have shown that the incidence of acute myocardial infarction [34] and the mortality of cerebral infarction [35] in males in the lower age group in Tianjin tended to increase, while in females it was relatively stable, which is basically consistent with the trend of BP changes in this study. The risk of death from CVD was also higher in the lower age group than in the higher age group in patients with hypertension. [36, 37] People in the lower age group usually pay little attention to BP, and the current public health policy in China mainly emphasizes in clinical practice that people aged 35 and above should have their BP checked first, which may be one of the important reasons for the low awareness rate. Therefore, more active hypertension prevention and control strategies should be implemented in the lower age group. Health education and BP examination should be carried out for the lower age group and the frequency of BP measurement should be increased through community service or family self-testing.
Another new finding of our study was an increase in the attribution ratio of CVD attributable to high SBP in the 25–44 and 75 and above age groups in Tianjin. CVD is the largest single contributor to global mortality, [38] which accounts for more than 40% of deaths in China [39] and 53.7% in Tianjin city. [40] Our results showed a significant increase in the number and proportion of deaths attributed to hypertension in the age group 75 years and older compared to other age groups from 2002 to 2018. Although there is still controversy over the target of BP control in the elderly, [41, 42] cohort studies from China have shown that all-cause mortality and CVD mortality were significantly increased in elderly when their SBP is ≥ 160 mmHg. [43,44,45] Control of hypertension is the most important measure to reduce the DALYs of CVD. [46].
In 2018, the number of deaths from ischemic heart disease exceeded that of stroke attributable to hypertension. This was associated with an increase in age-standardized mortality from ischemic heart disease and a decrease in age-standardized mortality from stroke. [4, 47] The factors contributing to these declines mainly include improvements in healthcare coverage, upgrades in medical technology and improvements in the public health environment for stroke prevention by the government. [48].
Some limitations cannot be ignored. One of the study’s limitations is that the number of survey samples in 2002 was significantly smaller than that in 2018. Although it could meet the requirement of minimum representative sample size in 2002, the results of stratified analysis may be unstable. Furthermore, the RRs of SBP to CVD were from the GBD study, which was a global meta-result and not the real situation of Tianjin. More cohort studies are needed in the future.
Conclusions
Although the treatment and control rates of hypertension increased a lot, the prevalence of hypertension and the proportion of CVD deaths attributed to hypertension remains high especially in younger and old age groups, suggesting that effective hypertension prevention measures should be targeted to reduce the overall prevalence of hypertension according to different regions and populations. The results of this study provide a scientific basis for the development of relevant hypertension prevention and control policies. In addition, large population-based prospective studies should be implemented to explore effective preventive measures to reduce the incidence and prevalence of hypertension and thereby reduce the risk of cardiovascular mortality in the population.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.Data are however available from the authors upon reasonable request and with permission of the Tianjin Center for Disease Control and Prevention ethics committees.
Abbreviations
- BP:
-
Blood pressure
- CVD:
-
Cardiovascular disease
- UI:
-
Uncertainty interval
- DALYs:
-
Disability-adjusted life-years
- SBP:
-
Systolic blood pressure
- GBD:
-
Global Burden of Disease
- CDRS:
-
Tianjin All Cause of Death Registration System
- ICD-10:
-
International Classification of Diseases 10th Revision
- IHD:
-
Ischemic heart disease
- DBP:
-
Diastolic blood pressure
- PAFs:
-
Population-attributable fractions
- SD:
-
Standard deviation
References
Collaborators GBDRF. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1923–94.
Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of Hypertension in China: Results From the China Hypertension Survey, 2012–2015. Circulation. 2018;137(22):2344–56.
Zhao L, Ma G, Piao J, Zhang J, Yu D, He Y, et al. Scheme of the 2010–2012 Chinese nutrition and health surveillance. Zhonghua Yu Fang Yi Xue Za Zhi. 2016;50(3):204–7.
Liu S, Li Y, Zeng X, Wang H, Yin P, Wang L, et al. Burden of cardiovascular diseases in China, 1990–2016: findings from the 2016 Global Burden of disease study. JAMA Cardiol. 2019;4(4):342–52.
Xu Y, Wang L, He J, Bi Y, Li M, Wang T, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310(9):948–59.
Jiang G, Zhang H, Li W, Wang D, Xu Z, Song G, et al. Study on smoking-attributed mortality by using all causes of death surveillance system in Tianjin. Zhonghua Liu Xing Bing Xue Za Zhi. 2016;37(3):381–3.
Collaborators GBDMM. Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1775–812.
Liu LS. Writing Group of 2010 Chinese Guidelines for the Management of Hypertension [2010 Chinese guidelines for the management of hypertension.]. Zhonghua Xin Xue Guan Bing Za Zhi. 2011;39:579–615.
Luo Y, Xia F, Yu X, Li P, Huang W, Zhang W. Long-term trends and regional variations of hypertension incidence in China: a prospective cohort study from the China Health and Nutrition Survey, 1991–2015. BMJ Open. 2021;11(1):e042053.
Collaborators GBD. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393(10184):1958–72.
Wang ZB, Pan Y, Xin P, Zhang J, Jiang GH. Dietary intake of sodium and potassium among adult inhabitants and evaluation of survey methods in Tianjin in 2015. Zhonghua Yu Fang Yi Xue Za Zhi. 2019;53(11):1141–6.
Zhang L, Wang Z, Wang X, Chen Z, Shao L, Tian Y, et al. Prevalence of overweight and obesity in China: Results from a cross-sectional study of 441 thousand adults, 2012–2015. Obes Res Clin Pract. 2020;14(2):119–26.
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation. 2016;134(6):441–50.
Wang X, Bots ML, Yang F, Hoes AW, Vaartjes I. Prevalence of hypertension in China: a systematic review and meta-regression analysis of trends and regional differences. J Hypertens. 2014;32(10):1919–27 discussion 27.
Qi SF, Zhang B, Wang HJ, Yan J, Mi YJ, Liu DW, et al. Prevalence of hypertension subtypes in 2011 and the trends from 1991 to 2011 among Chinese adults. J Epidemiol Community Health. 2016;70(5):444–51.
Dorans KS, Mills KT, Liu Y, He J. Trends in prevalence and control of hypertension according to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline. J Am Heart Assoc. 2018;7(11):e008888.
Overwyk KJ, Zhao L, Zhang Z, Wiltz JL, Dunford EK, Cogswell ME. Trends in blood pressure and usual dietary sodium intake among children and adolescents, national health and nutrition examination survey 2003 to 2016. Hypertension. 2019;74(2):260–6.
Kim TJ, Lee JW, Kang HT, Cho MC, Lim HJ, Kim JY, et al. Trends in blood pressure and prevalence of hypertension in Korean adults based on the 1998–2014 KNHANES. Yonsei Med J. 2018;59(3):356–65.
Hata J, Ninomiya T, Hirakawa Y, Nagata M, Mukai N, Gotoh S, et al. Secular trends in cardiovascular disease and its risk factors in Japanese: half-century data from the Hisayama Study (1961–2009). Circulation. 2013;128(11):1198–205.
Wang ZW, Wang X, Zhang LF, Wang W, Chen WW, Zhu ML, et al. Hypertension Control in Communities (HCC): evaluation result of blood pressure management among hypertensive. Zhonghua Liu Xing Bing Xue Za Zhi. 2010;31(1):1–4.
Wang Z, Wang X, Chen Z, Wang W, Zhu H, Chen W, et al. Hypertension control in community health centers across China: analysis of antihypertensive drug treatment patterns. Am J Hypertens. 2014;27(2):252–9.
Yang L, You L, Lian Z, Chen X, Liu Y. Survey on utilization and satisfaction of basic public health services for patients with hypertension and diabetes. Chin J Prev Control Chron Dis. 2020;28(04):253–8.
Chen Z. Launch of the health-care reform plan in China. Lancet. 2009;373(9672):1322–4.
Chen Z, Zhang Z, Zhu J. Analysis on Impact of Health Insurance Universal on Medical Expense Containment for Residents. Chin Health Econ. 2021;40(1):49–52.
Collaboration NCDRF. Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet. 2019;394(10199):639–51.
Zhang Y, Moran AE. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension. 2017;70(4):736–42.
Gu Q, Burt VL, Dillon CF, Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health And Nutrition Examination Survey, 2001 to 2010. Circulation. 2012;126(17):2105–14.
Zhang Y, Yang H, Wang R, Zhao F, Liu T, Zhang Y, et al. An Analysis of Medication Prescriptions for Hypertension in Urban and Rural Residents in Tianjin. Adv Ther. 2020;37(10):4414–26.
Management NCoEoPH, Project NBPHS, Center NC. [National Clinical Practice Guidelines on the Management of Hypertension in Primary Health Care in China (2020)]. Chin Circul J. 2021;36(3):209–20.
Wang L, Peng W, Zhao Z, et al. Prevalence and Treatment of Diabetes in China, 2013–2018. JAMA. 2021;326(24):2498–506. https://doi.org/10.1001/jama.2021.22208.Erratum.In:JAMA.2022Mar15;327(11):1093.
Zheng W, Zhang H, Shen C, Trend analysis of lung cancer mortality and years of life lost (YLL) rate from, et al. to 2016 in Tianjin, China: Does the lung cancer burden in rural areas exceed that of urban areas?[J]. Thoracic Cancer. 1999;2020:11.
Chang gai,Wang ping, LI jing,et al.[Investigation of drinking status in residents (≥ 15 years old) of urban and rural areas in Tianjin].2016,24(7):493–497,501. https://doi.org/10.16386/j.cjpccd.issn.
Salazar MR, Espeche WG, Aizpurúa M, et al. Blood pressure response to a community-based program and long-term cardiovascular outcome. Am J Hypertens. 2014;27(8):1061–8. https://doi.org/10.1093/ajh/hpt240.
Wang DZ, Shen CF, Zhang Y, Zhang H, Song GD, Li W, et al. Fifteen-year trend in incidence of acute myocardial infarction in Tianjin of China. Zhonghua Xin Xue Guan Bing Za Zhi. 2017;45(2):154–9.
Wang DZ, Xue XD, Zhang H, Xu ZL, Zhang Y, Song GD, et al. Analysis on trend of cerebral infarction mortality from 1999 to 2015 in Tianjin of China. Zhonghua Xin Xue Guan Bing Za Zhi. 2018;46(2):152–8.
Lewington S, Lacey B, Clarke R, Guo Y, Kong XL, Yang L, et al. The Burden of Hypertension and Associated Risk for Cardiovascular Mortality in China. JAMA Intern Med. 2016;176(4):524–32.
Wang M, Wu T, Yu C, Gao W, Lv J, Wu Y, et al. Association between blood pressure levels and cardiovascular deaths: a 20-year follow-up study in rural China. BMJ Open. 2020;10(2):e035190.
Sacco RL, Roth GA, Reddy KS, Arnett DK, Bonita R, Gaziano TA, et al. The heart of 25 by 25: achieving the goal of reducing global and regional premature deaths from cardiovascular diseases and stroke: a modeling study from the American heart association and world heart federation. Circulation. 2016;133(23):e674–90.
Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387(10015):251–72.
Xu Z, Zhang H, Wang D, Song J, Zhang Y, Shen C, et al. Analysis on causes of death and life expectancy in residents of Tianjin, 2014. Tianjin Med J. 2016;44(12):1510–3.
van Bemmel T, Gussekloo J, Westendorp RG, Blauw GJ. In a population-based prospective study, no association between high blood pressure and mortality after age 85 years. J Hypertens. 2006;24(2):287–92.
Satish S, Freeman DH Jr, Ray L, Goodwin JS. The relationship between blood pressure and mortality in the oldest old. J Am Geriatr Soc. 2001;49(4):367–74.
Guo J, Lv J, Guo Y, Bian Z, Zheng B, Wu M, et al. Association between blood pressure categories and cardiovascular disease mortality in China. PLoS ONE. 2021;16(7):e0255373.
Wu CY, Hu HY, Chou YJ, Huang N, Chou YC, Li CP. High Blood Pressure and All-Cause and Cardiovascular Disease Mortalities in Community-Dwelling Older Adults. Medicine (Baltimore). 2015;94(47):e2160.
Lv YB, Gao X, Yin ZX, Chen HS, Luo JS, Brasher MS, et al. Revisiting the association of blood pressure with mortality in oldest old people in China: community based, longitudinal prospective study. BMJ. 2018;361:k2158.
Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145–58.
Wang W, Wang D, Liu H, Sun H, Jiang B, Ru X, et al. Trend of declining stroke mortality in China: reasons and analysis. Stroke Vasc Neurol. 2017;2(3):132–9.
Wang Z, Hu S, Sang S, Luo L, Yu C. Age-Period-Cohort Analysis of Stroke Mortality in China: Data From the Global Burden of Disease Study 2013. Stroke. 2017;48(2):271–5.
Acknowledgements
The authors thank all staff from local CDCs, hospitals, and community health service centers, who were involved in the national nutrition and chronic disease risk factors survey of Tianjin and Tianjin CDRS.
Funding
This research was supported by Tianjin Medical Key Discipline (Specialty) Construction Project from Tianjin Health Bureau.
Author information
Authors and Affiliations
Contributions
G.J. contributed to the study conception and design; W.Z. contributed to the study design, data analysis, interpretation of results, and manuscript preparation; X.W., X.X., W.L., L.F., S.Z., C.L., Z.W., M.X. and P.X. contributed to the literature search, data collection, data analysis, and manuscript preparation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures were carried out in accordance with the provisions of the World Medical Association Declaration of Helsinki (2013). The Ethics Committee of the Tianjin Center for Disease Control and Prevention approved the study. Informed consent was obtained from all participants in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, W., Wang, X., Xue, X. et al. Characteristics of hypertension in the last 16 years in high prevalence region of China and the attribute ratios for cardiovascular mortality. BMC Public Health 23, 114 (2023). https://doi.org/10.1186/s12889-022-14974-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-14974-0