Abstract
Background
Non-pharmaceutical interventions (NPIs), such as travel restrictions, social distancing and isolation policies, aimed at controlling the spread of COVID-19 may have reduced transmission of other endemic communicable diseases, such as measles, mumps and meningitis in England.
Methods
An interrupted time series analysis was conducted to examine whether NPIs was associated with trends in endemic communicable diseases, using weekly reported cases of seven notifiable communicable diseases (food poisoning, measles, meningitis, mumps, scarlet fever and pertussis) between 02/01/2017 to 02/01/2021 for England.
Results
Following the introduction of COVID-19 restrictions, there was an 81.1% (95% CI; 77.2–84.4) adjusted percentage reduction in the total number of notifiable diseases recorded per week in England. The greatest decrease was observed for measles, with a 90.5% percentage reduction (95% CI; 86.8–93.1) from 42 to 5 cases per week. The smallest decrease was observed for food poisoning, with a 56.4% (95%CI; 42.5–54.2) decrease from 191 to 83 cases per week.
Conclusions
A total reduction in the incidence of endemic notifiable diseases was observed in England following the implementation of public health measures aimed at reducing transmission of SARS-COV-2 on March 23, 2020. The greatest reductions were observed in diseases most frequently observed during childhood that are transmitted via close human-to-human contact, such as measles and pertussis. A less substantive reduction was observed in reported cases of food poisoning, likely due to dining services (i.e., home deliveries and takeaways) remaining open and providing a potential route of transmission. This study provides further evidence of the effectiveness of non-pharmaceutical public health interventions in reducing the transmission of both respiratory and food-borne communicable diseases.
Similar content being viewed by others
Background
The World Health Organisation declared severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) a public health emergency on 31st January 2020. Within one year, SARS-CoV-2 had infected more than 100 million people globally, resulting in over 2 million deaths [1]. In response to the public health emergency, countries globally implemented a range of pharmaceutical (e.g., vaccines) and non-pharmaceutical interventions (NPIs) (e.g., national lockdowns, social distancing, isolation policies, contact tracing systems and travel restrictions) to reduce rates of COVID-19 infection [2, 3].
While pharmaceutical interventions are disease specific, NPIs have been shown to suppress transmission of a broad spectrum of endemic notifiable infectious pathogens, such as seasonal influenza [4,5,6] and measles [7], in countries including, but not limited to, Australia, China, Germany and the United States of America [8,9,10,11]. The impact of NPIs on disease spread via respiratory droplets is supported by Bruggemann et al.’s [12] analysis of surveillance data from 26 countries, which demonstrated significant reductions in transmission of bacterial infections from Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis following the introduction of NPIs.
Public health measures to suppress the spread of COVID-19 were first introduced in England on March 23, 2020 [13], with members of the public instructed to stay at home and all non-essential businesses closed. As observed in other countries, it is likely that NPIs implemented in England to suppress transmission of SARS-CoV-2 would have reduced transmission of other endemic notifiable diseases.
To our knowledge, no study to date has utilised national data from Public Health England (now known as UK Health Security Agency following organisational restructure in 2021) to assess the impact of lockdown measures on transmission of communicable diseases in England. This study, therefore, aimed to identify whether the introduction of measures designed to reduce COVID-19 transmission affected the incidence of notifiable communicable diseases in England (Table 1).
Methods
This study examines the impact of NPIs, specifically the introduction of a national ‘lockdown’ (stay at home orders and closure of schools and non-essential business), on cases of notifiable diseases in England. An interrupted time series analysis (ITSA) was considered an appropriate statistical method for evaluating the longitudinal effect of NPIs on reported cases of notifiable diseases, as it enabled comparison before and after intervention.
Outcome and intervention
Due to pre-pandemic widespread prevalence, the outcome of interest for the study was the case frequency per week of: measles, mumps, meningococcal meningitis, pertussis, scarlet fever, and food poisoning (Table 1). The intervention was defined as introduction of a national lockdown, which occurred nationally on March 23, 2020 in England.
Data sources
The data source for the study was weekly reported cases of diseases of interest from Public Health England’s notifications of infectious diseases (NOIDs) dataset for England [14].
Statistical analysis
The ITSAs were conducted using segmented regression with a quasi-Poisson model with weekly cases of notifiable disease as the dependent variable. As the outcome was count of cases, Poisson regression model was considered most appropriate – other regression models such as ordinary least squares (linear) regression for continuous outcomes was considered inappropriate. An assumption of a Poisson distribution is that the variance is equal to the expected count. Initial analyses suggested variance was greater leading to overdispersion of the data, so a quasi-Poisson model was used. A second assumption was that observations are independent and autocorrelation was assessed by examining the plot of residuals and the partial autocorrelation function. It was hypothesised a priori that the intervention would result in a level (step) change in the outcome, given the restrictions that were associated with the NPIs.
The ITSA model included week as a linear variable to model for an underlying linear time trend and NPIs (national ‘lockdown’) as intervention dummy variables, coded ‘0’ for the pre-intervention period and ‘1’ for the post-intervention period. The break point for the model was March 23, 2020 signifying the introduction of national restrictions. The pre-intervention time period therefore was from week of January 02, 2017 to week of March 16, 2020 – and the post-intervention time period was from week of March 23, 2020 to January 02, 2021 for this analysis.
The model was further adjusted for seasonality in the underlying reported cases, using a harmonic term based on the week of the year and using two sine/cosine pairs per 12-month period. We have not considered inclusion of a recovery slope as the focus of the study was on the effect of national restrictions on reported cases of notifiable diseases in the immediate period after the lockdown, and no sensitivity analyses were conducted.
All data were analysed, and all plots generated, using RStudio (version 1.4.1103).
Results
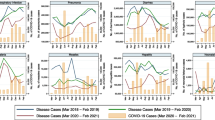
Following the introduction of NPIs in England on March 23, 2020 there was an 81.1% (95% CI; 77.2–84.4) adjusted percentage reduction in the total number of notifiable diseases recorded per week, from an average of 990 cases per week before the introduction of national restrictions to 217 cases per week following the introduction of national restrictions (Table 2 and Fig. 1).
Incidence of notifiable infectious diseases with models adjusted for linear time trend and seasonality. England combined data for food poisoning, measles, meningitis, mumps, scarlet fever and pertussis. (Red line shows the trend based on the seasonally adjusted regression model; green line shows the de-seasonalised trend; grey box represents the time post-lockdown.)
The greatest decrease in England was observed in weekly cases of measles, with a 90.5% percentage reduction (95% CI; 86.8–93.1) from 42 to 5 cases per week, followed by cases of pertussis (90.1% reduction), scarlet fever (88.6% reduction), mumps (88.2% reduction) and meningitis (82.8%). The reduction in the total number of food poisoning incidents was 56.4% (95%CI; 42.5–54.2), from 191 cases per week to 83 cases.
Discussion
A total reduction in the incidence of endemic notifiable diseases was observed in England following the implementation of NPIs aimed at reducing transmission of SARS-COV-2 on March 23, 2020. The greatest reductions were observed in diseases most frequently observed during childhood that are transmitted via close human-to-human contact, such as measles and pertussis. These diseases follow similar routes of transmission as observed for SARS-COV-2 [15]. A less substantive reduction was observed in reported cases of food poisoning, defined by Public Health England as an illness caused by the consumption of food contaminated with bacteria, parasite, virus, chemical or other toxin.
Within England, around one-third of measles cases are international travel related [16], with secondary infection occurring within nursery, school and other educational settings. Travel restrictions [17] and school and nursery closures likely halted initial incursion and subsequent onward transmission of measles, as observed in countries across the European Union [7], including reduced incidence of measles among children in Germany [10]. In addition to measles, COVID-19 travel restrictions and closure of educational settings likely reduced transmission of other vaccine-preventable childhood infections, including mumps and pertussis. This is in line with research predating COVID-19 which highlights the role of educational settings in facilitating transmission of childhood respiratory infections [18, 19], as well as research conducted in Finland during the COVID-19 pandemic showing a decrease in daily emergency department visits for viral respiratory tract infections following nation-wide school closures [20].
In contrast to pathogens transmitted from person-to-person via saliva or respiratory droplets, cases of food-borne pathogens – typically transmitted via the faecal-oral route – displayed a less severe decrease. While enhanced levels of hand-hygiene, closures of educational settings and orders to work from home will have reduced human-to-human transmission of gastro-intestinal infections, many dining services (i.e., home deliveries and takeaways) remained open, providing a potential route of transmission. Findings are consistent with research from Germany and the USA which found a less severe reduction in food-borne pathogens when compared to respiratory infections following introduction of NPIs [7, 10].
Evidence presented here and from other global studies [8,9,10,11, 21, 22] suggest that NPIs to suppress the transmission of SARS-CoV-2, such as international travel restrictions, closures of schools and orders to work from home, led to reduced incidence of respiratory and food-borne pathogens. However, widespread disruption of public health and front-line health services are likely to have also resulted in reduced reporting and recording of notifiable infectious diseases, as observed via a decrease in routine reporting of sexually transmitted diseases within the USA during the pandemic [23].
Our study indicates that NPIs are an effective measure to reduce transmission of communicable diseases, in particular those transmitted via close human to human contact. However, this is balanced against the health, economic and social impacts of COVID-19 restrictions [24]. Findings presented here indicate that the incidence of notifiable diseases, such as measles, may be effective as a proxy to evaluate the effectiveness of restrictions on transmission of COVID-19, particularly in countries with inadequate COVID-19 testing and reporting facilities.
Study limitations include the omission of data on incidence of influenza due to insufficient data availability [14]. There may also have been significant underreporting during the COVID-19 pandemic, as patients may have been less likely to present to hospital, there may have been delays in reporting and there may have been diagnostic uncertainty surrounding the new disease (e.g., scarlet fever has similar symptoms to COVID-19). Furthermore, there were discrepancies between the sum of weekly reported cases reported for each year and the annual total reported. Nevertheless, we found this to be non-random which would reduce the risk of bias. A key assumption made was that without the NPIs (national ‘lockdown’), the pre-intervention trend in reported cases of notifiable infectious diseases would continue unchanged into the post-intervention period. It was not possible to add control group to our study as the intervention was a national lockdown. Finally, as the focus of this study was to determine whether or not the national lockdown in England had an impact on infectious disease notification frequency, and not to develop a prediction model, we did not undertake cross validation. Indeed, the dataset used only had one value for notifications nationally for each week and disease, so it was not possible to create training and validation sets.
In summary, this study provides further evidence of the effectiveness of NPIs in reducing the transmission of both respiratory and food-borne communicable diseases. These findings could be used to inform scientific modelling and decisions regarding NPIs when faced with future outbreaks of disease.
Availability of data and materials
The data sets analysed in this study are publicly available in the UK government Notifications of infectious diseases, available at https://www.gov.uk/government/collections/notifications-of-infectious-diseases-noids.
References
World Health Organisation. Coronavirus disease (COVID-19) Situation Report-202. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed 16 Sept 2022.
Flaxman S, Mishra S, Gandy A, Unwin HJ, Mellan TA, Coupland H, Whittaker C, Zhu H, Berah T, Eaton JW, Monod M. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–61.
Hale T, Angrist N, Hale AJ, Kira B, Majumdar S, Petherick A, Phillips T, Sridhar D, Thompson RN, Webster S, Zhang Y. Government responses and COVID-19 deaths: Global evidence across multiple pandemic waves. PLoS One. 2021;16(7):e0253116.
Kuo SC, Shih SM, Chien LH, Hsiung CA. Collateral benefit of COVID-19 control measures on influenza activity, Taiwan. Emerg Infect Dis. 2020;26(8):1928.
Soo RJ, Chiew CJ, Ma S, Pung R, Lee V. Decreased influenza incidence under COVID-19 control measures, Singapore. Emerg Infect Dis. 2020;26(8):1933.
Sullivan SG, Carlson S, Cheng AC, Chilver MB, Dwyer DE, Irwin M, Kok J, Macartney K, MacLachlan J, Minney-Smith C, Smith D. Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Eurosurveillance. 2020;25(47):2001847.
Nicolay N, Mirinaviciute G, Mollet T, Celentano LP, Bacci S. Epidemiology of measles during the COVID-19 pandemic, a description of the surveillance data, 29 EU/EEA countries and the United Kingdom, January to May 2020. Eurosurveillance. 2020;25(31):2001390.
Adegbija O, Walker J, Smoll N, Khan A, Graham J, Khandaker G. Notifiable diseases after implementation of COVID-19 public health prevention measures in Central Queensland, Australia. Commun Dis Intell. 2018;2021:45. https://doi.org/10.33321/cdi.2021.45.11.
Geng MJ, Zhang HY, Yu LJ, Lv CL, Wang T, Che TL, Xu Q, Jiang BG, Chen JJ, Hay SI, Li ZJ. Changes in notifiable infectious disease incidence in China during the COVID-19 pandemic. Nat Commun. 2021;12(1):1–1.
Ullrich A, Schranz M, Rexroth U, Hamouda O, Schaade L, Diercke M, Boender TS, Robert Koch’s Infectious Disease Surveillance Group. Impact of the COVID-19 pandemic and associated non-pharmaceutical interventions on other notifiable infectious diseases in Germany: An analysis of national surveillance data during week 1–2016–week 32–2020. Lancet Reg Health-Eur. 2021;6:100103.
Crane MA, Popovic A, Panaparambil R, Stolbach AI, Romley JA, Ghanem KG. Reporting of infectious diseases in the United States during the coronavirus disease 2019 (COVID-19) pandemic. Clin Infect Dis. 2022;74(5):901–4.
Brueggemann AB, van Rensburg MJ, Shaw D, McCarthy ND, Jolley KA, Maiden MC, van der Linden MP, Amin-Chowdhury Z, Bennett DE, Borrow R, Brandileone MC. Changes in the incidence of invasive disease due to Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis during the COVID-19 pandemic in 26 countries and territories in the Invasive Respiratory Infection Surveillance Initiative: a prospective analysis of surveillance data. Lancet Digital Health. 2021;3(6):e360–70.
UK Government. Prime Minister's statement on coronavirus (COVID-19): 23 March 2020. Available at: https://www.gov.uk/government/speeches/pm-address-to-the-nation-on-coronavirus-23-march-2020. Accessed 16 Sept 2022.
UK Government. 2022. Notifications of infectious diseases (NOIDs). Available at: https://www.gov.uk/government/collections/notifications-of-infectious-diseases-noids. Accessed 16 Sept 2022. Accessed 16 Sept 2022.
Salian VS, Wright JA, Vedell PT, Nair S, Li C, Kandimalla M, Tang X, Carmona Porquera EM, Kalari KR, Kandimalla KK. COVID-19 transmission, current treatment, and future therapeutic strategies. Mol Pharm. 2021;18(3):754–71.
Public Health England, 2014. Travel associated measles accounts for a third of England cases as numbers continue decline. Available at: https://www.gov.uk/government/news/travel-associated-measles-accounts-for-a-third-of-england-cases-as-numbers-continue-decline. Accessed 16 Sept 2022.
Sokadjo YM, Atchadé MN. The influence of passenger air traffic on the spread of COVID-19 in the world. Transp Res Interdiscip Perspect. 2020;1(8):100213.
Kim S, Kim YW, Ryu S, Kim JW. Norovirus outbreak in a kindergarten: Human to human transmission among children. Infect Chemother. 2019;51(2):171–6.
Lu CY, Huang LM, Fan TY, Cheng AL, Chang LY. Incidence of respiratory viral infections and associated factors among children attending a public kindergarten in Taipei City. J Formos Med Assoc. 2018;117(2):132–40.
Kuitunen I, Artama M, Mäkelä L, Backman K, Heiskanen-Kosma T, Renko M. Effect of social distancing due to the COVID-19 pandemic on the incidence of viral respiratory tract infections in children in Finland during early 2020. Pediatr Infect Dis J. 2020;39(12):e423–7.
Olsen SJ, Azziz-Baumgartner E, Budd AP, Brammer L, Sullivan S, Pineda RF, Cohen C, Fry AM. Decreased influenza activity during the COVID-19 pandemic—United States, Australia, Chile, and South Africa, 2020. Am J Transplant. 2020;20(12):3681–5.
Cowling BJ, Ali ST, Ng TW, Tsang TK, Li JC, Fong MW, Liao Q, Kwan MY, Lee SL, Chiu SS, Wu JT. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5(5):e279–88.
Pagaoa M, Grey J, Torrone E, Kreisel K, Stenger M, Weinstock H. Trends in nationally notifiable sexually transmitted disease case reports during the US COVID-19 pandemic, January to December 2020. Sex Transm Dis. 2021;48(10):798.
Galea S, Merchant R, Lurie N. The Mental Health Consequences of COVID-19 and Physical Distancing. JAMA Intern Med. 2020;180(6):817. https://doi.org/10.1001/jamainternmed.2020.1562.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
KN, JL, and KS extracted the data. FO and SS conducted the statistical analysis of the data. PC, FO, and JSC designed the study. All authors contributed to the final manuscript by either writing the original copy or revising it afterwards.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The data used in this study are freely accessible and fully anonymised. Therefore, no formal ethical approval was required for the study nor the collection of patient consent. Hence, all methods were carried out in accordance with relevant guidance and regulations.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Fatai Ogunlayi and Paul C Coleman Joint senior author.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nash, K., Lai, J., Sandhu, K. et al. Impact of national COVID-19 restrictions on incidence of notifiable communicable diseases in England: an interrupted time series analysis. BMC Public Health 22, 2318 (2022). https://doi.org/10.1186/s12889-022-14796-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-14796-0