Abstract
Objective
Effect of physical exercise on pregnant women currently has become a hot topic in prenatal health care. In this study, A meta-analysis was conducted on account of Randomized Controlled Trial (RCT). It focused on evaluating the effect of physical exercise intervention on blood pressure so that could provide certain evidence for health care during pregnancy.
Methods
Results of relevant studies were retrieved from PubMed, Embase, Web of Science and the Cochrane Library, and all of these included studies were evaluated according to the Cochrane collaboration’s tool for assessing the risk of bias. Stata 15.1 was used for meta-analysis, and mean difference (MD) was used as statistic for pooled analysis. The effect values were combined by conventional meta-analysis and Bayesian meta-analysis respectively, and the consistency of pooled results was considered as well.
Results
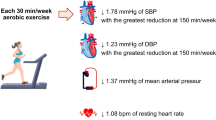
A total of 18 RCT studies were included in the quantitative analysis. The conventional meta-analysis showed differences in blood pressure between intervention group and control group (P < 0.05). Systolic and diastolic blood pressures of intervention group were 3.19 mmHg (95% CI: -5.13, -1.25) and 2.14 mmHg (95% CI: -4.26, -0.03) lower than that of control group, respectively. Bayesian meta-analysis showed that both systolic and diastolic pressure among intervention group decreased by 3.34 mmHg (95% CrI: -5.15, -1.56) and 2.14 mmHg (95% CrI: -3.79, − 0.50), respectively. Subgroup analysis supported that as long as healthy pregnant women participated in exercises, their blood pressure could be slightly regulated, while hypertension susceptible pregnant women significantly lowered blood pressure.
Conclusion
Exercise intervention during pregnancy is beneficial to lower or normalize blood pressure, and this research provides clues for follow-up studies.
Similar content being viewed by others
Background
Physical exercise is a planned, repetitive, purposeful and systematic activity that aims to improve or maintain physical fitness [1]. Physical exercise helps reduce the risk of obesity, diabetes, high blood pressure and mental health problems in adults [2, 3]. The direct and indirect costs of physical inactivity are estimated about €910 million among 10 million people per year globally [3]. Physical inactivity is the fourth largest risk factor for death globally [4]. The American Heart Association (AHA) highlights sedentary behavior and inactivity as major risk factors for cardiovascular disease [2]. A large number of research also confirmed the value of exercise in prevention and treatment of cardiovascular disease. Physical exercise has the positive role on the primary and secondary prevention of coronary heart disease (CHD), and sedentary behavior might lead to metabolic as well as cardiovascular disease [5, 6]. A meta-analysis of 44,370 subjects found that 30 to 40 minutes of moderate physical exercise a day could offset the adverse effects of sitting for 10 hours and reduced all-cause mortality [7]. A meta-analysis based on individual participant data from randomized trials showed that less weight gain occurred in the intervention group than control group (mean difference − 0.70 kg, 95%CI: − 0.92 to − 0.48 kg) [8].
In order to meet the needs of maternal metabolism and fetal development, the state of the pregnant woman’s body will change [9]. The health effect of physical exercise on pregnant women has become a hot topic of pregnancy health care, however, the view is still controversial. Some studies supported that healthy pregnant women should be encouraged to carry out regular physical exercise [6, 10,11,12]. The American College of Obstetricians and Gynecologists encourage pregnant women to get at least 30 minutes of moderate physical exercise a day [13]. Conversely, there is also a view that pregnant women should exercise cautiously, especially at moderate or vigorous levels [14]. Excessive physical exercise during pregnancy can lead to chronic fatigue, hypoglycemia, and an increased risk of injury (i.e., low back pain or musculoskeleal injury). Significant changes in posture and shifts in centre of gravity alter maternal balance and coordination. In the past, Physical exercise is not recommended for women with high blood pressure during pregnancy because of concerns about the safety of the fetus and the pregnant woman, however, recent studies have showed that proper exercise is associated with a significantly reduced risk of gestational hypertensive disorders overall, either structured exercise or yoga have a beneficial effect for preventing the onset of pregnancy-induced hypertension (HDP) [9, 15].
Studies on the relevance between physical exercise and blood pressure during pregnancy are increasing, and the types of study design are diversified gradually [11, 16,17,18,19]. However, none of unanimous conclusions have been drawn. Randomized Controlled Trial (RCT) is generally regarded as the research design with the highest level of evidence. Therefore, a meta-analysis based on RCT studies was conducted to analyse the correlation between physical exercise interventions and blood pressure among pregnancy, with the aim of providing certain evidence for health care during pregnancy
Methods
Search strategy
All the data which was connected with the relationship between physical exercise and blood pressure among pregnancy had been searched from PubMed, Embase, Web of Science and The Cochrane Library since these databases constructed to July 15, 2022 by using a combination of subject and free words. In order to avoid omission, the references which were involved in the study had been further traced. The retrieval strategies are showed as follows (Table 1).
Inclusion and exclusion criteria
The inclusion and exclusion criteria were determined according to the Principles of the Cochrane Systematic Review Manual (PICOS), and the literatures were strictly screened.
Inclusion criteria:
-
(1)
The research objects are pregnant women (Population);
-
(2)
Clearly planned and organized interventions among pregnancy (Interventions);
-
(3)
After certain period of exercise intervention, blood pressure of target population has been measured and reported for comparison (Comparison);
-
(4)
Values of blood pressure in target population after exercise intervention and the standard deviations, or the values of blood pressure in target population before and after interventions and the standard deviations were reported (Outcomes);
-
(5)
The study design was a randomized controlled trial (Study).
Exclusion criteria:
-
(1)
Non-pregnant women from different populations, or pregnant women with HDP (Population);
-
(2)
Short-term studies or acute effects after exercise interventions (Outcome);
-
(3)
Review, conference abstracts, case reports and animal experiments (Study types);
-
(4)
Different studies conducted in the same population (Irrelevant).
Data extraction
Two researchers independently screened literatures, extracted data, and then unified results. Firstly, the literatures that exported from different databases were imported into Endnote X7 (Thomson Reuters, New York, NY, USA), for automatically detecting duplicates and removing duplicates in batches.
After two rounds of screening, we conducted to determine the research which finally match the requirements: To begin with, the title, abstract and literature types of articles were browsed, and the other studies which were irrelevant to the topic were excluded. Secondly, remaining literatures were screened through the full text so that the final studies could be determined for inclusion and analysis.
Bias risk assessment of involved studies
All involved studies were evaluated according to the risk assessment tool for bias in RCT, including seven items as described in the Cochrane Handbook for Systematic Reviews. The risk of bias was assessed by using Review Manager 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration) software.
Statistical analysis
All statistical analyses were performed in Stata/SE 15.1 (Stata Corp, College Station, TX, USA). Since the outcome variables concerned were continuous measured data, mean difference (MD) was used as the effect analysis statistics. Data from the involved studies were collated firstly in order to ensure comparability between studies.
Effect values were analysed by combining classical meta-analysis and Bayesian meta-analysis, respectively. In classic meta-analysis, statistics Q and I2 are assessed heterogeneity if the Q statistic corresponds to P > 0.1 or I2 < 50%, and the heterogeneity of the included studies was considered acceptable in this case, and the effect values were combined using the Inverse Variance method of the fixed effect model. On the contrary, once it comes to significant heterogeneity among studies, the effect values would be combined by random effect model. Egger’s and Begg’s tests were used to estimate publication bias and provide a visual display of funnel plots. The sensitivity analysis has been applied to exclude each study individually and evaluate it for determining the extent to any single study that contributed to overall combined effect.
Compared with classical frequency-school meta-analysis, Bayesian meta-analysis is more advantageous in dealing with complex problems such as random effects, hierarchical structure and data sparseness [20]. Especially when the sample size of the included study is small and the data does not meet normal distribution or cannot be tested for normality. Combined estimates of effects using classical meta-analysis may be biased. However, Bayesian analysis can directly calculate the accurate finite sample distribution without relying on the asymptotic theory, and fully consider the uncertainty of the model, so it can be considered that the Bayesian estimation of meta-analysis is more reliable and reasonable [21]. After improving the model estimation accuracy, the modeling method is more flexible. We used Markov Chain Monte Carlo (MCMC) method to obtain the mean value, and the variation degree between studies (θτ2), whose main command is “BayesMH”, which uses the adjusted Metropolis Hastings (MH) and Inverse gamma methods to compute the Bayesian regression model.
Results
A total of 3179 records were retrieved from PubMed, Embase, Web of Science, and The Cochrane Library. The remaining 81 records were screened based on the title and abstract, and then the full text was read according to the inclusion criteria. Finally, 18 RCT studies that met the criteria were included in the analysis [10, 16, 18, 19, 22,23,24,25,26,27,28,29,30,31,32,33,34,35] (Fig. 1). Seven studies focused on exercise interventions in healthy pregnant women, 10 studies looked at women at high risk for HDP, including overweight or obese women, women with chronic hypertension and family history of hypertension. There is only one study focused on both groups of women (Table 2). The purpose of quality assessment review is to ensure the quality of included studies meets the requirements and to assess the risk of bias in the included studies according to the tools which are provided in the Cochrane Manual. Most studies have reported allocation hiding for sequence generation, including automatic computer generation of random sequences, the use of random number tables, and coin flipping. Although only a few included studies blinded subjects, the outcome variables of concern were not affected by the absence of blinding. Dropouts were reported in all included studies, and no selective reporting bias was found, nor other biases were shown. Therefore, the literature that included in this meta-analysis maintained a high quality (Fig. 2).
Classic meta-analysis
A total of 18 RCTs reported an association between exercise interventions during pregnancy and changes of blood pressure, including 2930 pregnant women, which 1452 are the exercise intervention group and 1478 are in the conventional care control group. The mean and standard deviation of blood pressure of each study intervention and control group were inputted into Stata software for effect value combination. Due to the high heterogeneity among studies (I2 = 81.4%), we accepted the random effect model to combine the effect values. The combined results showed that, comparing with the control group, the systolic pressure of pregnant women in exercise intervention group lowered 3.19 mmHg (95%CI: − 5.13, − 1.25), and the diastolic blood pressure lowered 2.14 mmHg (95%CI: − 4.26, − 0.03), with statistically significant differences (Figs. 3 and 4)
.
Bayesian meta-analysis
According to random MCMC method, the posterior mean difference and variance (δ2) and corresponding 95% CrI. In terms of systolic pressure, the mean difference between exercise intervention group and control group was − 3.34 mmHg (95% CrI: − 5.15, − 1.56). In terms of diastolic pressure, the mean difference between exercise intervention group and control group was-2.14 mmHg (95% CrI: − 3.19, − 0.50), which was similar to the results of above classic meta-analysis and also supported that combined effect values were stable and reliable (Table 3).
In addition, the Bayesian convergence is visualized, including trajectory graph, autocorrelation graph, histogram and kernel density graph. The trajectory diagram shows that when MCMC reaches steady state, the simulated parameter values fluctuate up and down around the mean value (Fig. 5A). The histogram is approximately normally distributed, and consistent with the marginal posterior distribution of the specified conjugate normal (Fig. 5B). The autocorrelation diagram shows a series of lag ranges for the MCMC sample autocorrelation starting with a lag of 0, at which point the value is equal to the MCMC sample variance (Fig. 5C). Kernel density curve is another way to simulate posterior distribution (Fig. 5D). Efficiency analysis indicates that Bayesian analysis has a positive efficiency for statistical inference of unknown parameters, and the prior information has been correctly verified.
Subgroup analysis
A subgroup analysis which applied both classical and Bayesian methods indicated that exercise interventions during pregnancy can lower blood pressure slightly and moderately among ordinary healthy pregnant woman, and the Bayesian analysis did not point out any statistically significant difference. Exercise interventions can significantly reduce blood pressure in high-risk pregnant women. The results of two analysis methods are consistent, so they are considered robust and reliable (Table 4).
Publication bias and sensitivity analysis
According to the publication bias test of the 18 included studies, no significant publication bias has been found on Egger’s test (P = 0.425), and the funnel plot was relatively symmetrical (Fig. 6A). In addition, sensitivity analysis identified that the combined effect value ES and 95%CI were basically stable before and after excluding a single study, and it provided evidence that the analysis results were reliable (Fig. 6B).
Discussion
Regular physical exercise in normal pregnant women might be associate with health effects [36,37,38]. In our study, meta-analysis was conducted for the studies about physical exercise interventions and blood pressure changes during pregnancy, and the effect values were combined by the method of classical meta-analysis as well as Bayesian meta-analysis. The results identified physical exercise during pregnancy can effectively reduce blood pressure. Subgroup analysis presented that physical exercise could slightly regulate blood pressure in healthy pregnant women with normal pregnancy, and physical exercise could significantly reduce blood pressure in pregnant women with high-risk of HDP, and the effect was more obvious.
The result of this meta-analysis indicated that regular physical exercise during pregnancy is beneficial to pregnancy health. After a 12-week exercise intervention among healthy and nonactive pregnant women, the changes in resting blood pressure between intervention and baseline were assessed, and the researchers found that regular, long-term physical exercise significantly reduced resting systolic blood pressure [19]; In a recent meta-analysis, physical exercise interventions during pregnancy reduced the risk of pregnancy-induced hypertension and preeclampsia by 39 and 41%, respectively [17]. The underlying mechanism between prenatal physical exercise and blood pressure control is unclear and may be due to the effect of physical exercise on preventing excessive weight gain, reducing oxidative stress and inflammation, and improving vascular endothelial function [39, 40]. Elevated blood pressure remains a risk factor for maternal, fetus and neonatal mortality, and physical exercise during pregnancy is of particular importance for health [41].
The effect of physical exercise on blood pressure has also been shown in overweight and obese pregnant women who were susceptible to hypertension. In a study conducted in Norway, pregnant women with obesity were randomly divided into physical exercise group and control group. The pregnant women exercised from the middle to the late trimester, and the systolic blood pressure in exercise group was 7.73 mmHg lower than that in the control group at the late trimester [26]. Walking intervention has been found to reduce the incidence of HDP in high-risk pregnant women who contain family history of hypertension, preeclampsia, or chronic hypertension. Therefore, moderate physical exercise is recommended for pregnant women susceptible to hypertension in pregnancy to improve their health status [16]. In a study of hospitalized high-risk pregnant women, participants in intervention group had received lateral and supine structured bed physical exercise, and control group had maintained standard nursing. There were no significant differences in blood pressure, heart rate and fetal heart rate between two groups, but the physical discomfort and anxiety symptoms of pregnant women in structured physical exercise group had been significantly improved. Therefore, structured bed physical exercise for hospitalized high-risk bedridden pregnant women will not increase the health risks of themselves and the fetus, and bed exercise intervention can be considered in the management of high-risk pregnant women during pregnancy [27].
Daily physical exercise is recommended for non-risk or low-risk pregnant women, and regular physical exercise during pregnancy can prevent HDP [42, 43]. In studies of pregnant women with HDP, regular physical exercise during pregnancy has been associated with a reduced risk of adverse outcomes, including preeclampsia, preterm birth and cardiovascular disease [44, 45]. Mild physical exercise during pregnancy, including swimming, walking, yoga and stretching, improves blood vessel perfusion while stimulating major muscle and effectively reducing pregnancy complications [46]. Even in women who do not physical exercise before pregnancy, a moderate physical exercise during pregnancy can improve their health without affecting placental blood flow resistance and fetal growth [47].
The exercise interventions performed in studies included in this meta-analysis can be broadly divided into three types: (1) moderate walking and(or) jogging; (2) pedaling and cycling, and (3) comprehensive exercises designed according to American College of Obstetricians and Gynaecologists (ACOG), which accounts for the majority. This type of exercise program usually consists of four parts: a few minutes of warm-up; followed by aerobic exercises; resistance muscle training including upper and lower limb muscles, joint and pelvic floor muscle exercises; end with stretching and relaxation. One study included land aerobic sessions and aquatic activities session. Purpose of exercise in the water was to avoid a huge impact [29]. At present, regular participation in physical exercise is encouraged during pregnancy for healthy pregnant women [44]. Although there is a wide range of physical exercise that are currently recommended during pregnancy, there is insufficient evidence of superiority among different physical exercise [48]. It is worth noting that, the body at different stages of pregnancy will undergo significant changes, and it is necessary to timely adjust the physical exercise program [47].
This study is the first meta-analysis to explore and evaluate the relationship between physical exercise intervention during pregnancy and blood pressure by using both classical meta-analysis and Bayesian analysis. Through rigorous literature selection and quality assessment, the relevant randomized controlled trial was identified with a high level of evidence, and provided certain clues for blood pressure management during pregnancy. However, there are some certain limitations. First of all, nutritional intervention has not been considered, and its potential relationship with gestational blood pressure changes and pregnancy outcomes has not been examined. Secondly, some studies were limited to specific populations, such as GDM, overweight or obese pregnant women, and that lead to limit generality of the results.
However, we attempted to reduce heterogeneity by introducing subgroup analysis. Furthermore, low compliance in some studies may have affected the true health effects of physical exercise during pregnancy to some extent. Finally, the time of interventions in some studies was not clear, and the intervention effect in different stages of pregnancy was different, which limited the interpretation of the results.
Conclusion
This meta-analysis presented that exercise interventions in pregnant women might reduce systolic and diastolic blood pressure during pregnancy, particularly in pregnant women at high risk for HDP. Therefore, exercise should be promoted as an important way to improve the cardiovascular health of pregnant women.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
World Health Organization. What is physical activity? https://www.who.int/news-room/fact-sheets/detail/physical-activity. Accessed 28 Jan 2021.
Lobelo F, Rohm Young D, Sallis R, Garber MD, Billinger SA, Duperly J, et al. Routine assessment and promotion of physical activity in healthcare settings: a scientific statement from the American Heart Association. Circulation. 2018;137(18):e495–522.
World Health Organisation. Global recommendations on physical activity for health. Geneva: 2010.
World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013–2020 https://www.who.int/publications/i/item/global-action-plan-for-the-prevention-and-control-of-noncommunicable-diseases-2013-2020. Accessed 28 Jan 2021.
Lavie CJ, Ozemek C, Carbone S, Katzmarzyk PT, Blair SN. Sedentary behavior, exercise, and cardiovascular health. Circ Res. 2019;124(5):799–815.
Jeong S-W, Kim S-H, Kang S-H, Kim H-J, Yoon C-H, Youn T-J, et al. Mortality reduction with physical activity in patients with and without cardiovascular disease. Eur Heart J. 2019;40(43):3547–55.
Ekelund U, Tarp J, Fagerland MW, Johannessen JS, Hansen BH, Jefferis BJ, et al. Joint associations of accelero-meter measured physical activity and sedentary time with all-cause mortality: a harmonised meta-analysis in more than 44 000 middle-aged and older individuals. Br J Sports Med. 2020;54(24):1499–506.
Group IWMiPi-WC. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: meta-analysis of individual participant data from randomised trials. BMJ. 2017;358:j3119.
Charlesworth S, Foulds HJA, Burr JF, Bredin SSD. Evidence-based risk assessment and recommendations for physical activity clearance: pregnancy. Appl Physiol Nutr Metab. 2011;36(Suppl 1):S33–48.
Perales M, Valenzuela PL, Barakat R, Cordero Y, Peláez M, López C, et al. Gestational exercise and maternal and child health: effects until delivery and at post-Natal follow-up. J Clin Med. 2020;9(2):379.
Collings PJ, Farrar D, Gibson J, West J, Barber SE, Wright J. Associations of pregnancy physical activity with maternal Cardiometabolic health, neonatal delivery outcomes and body composition in a Biethnic cohort of 7305 mother-child pairs: the born in Bradford study. Sports Med. 2020;50(3):615–28.
Bisson M, Rhéaume C, Bujold E, Tremblay A, Marc I. Modulation of blood pressure response to exercise by physical activity and relationship with resting blood pressure during pregnancy. J Hypertens. 2014;32(7):1450–7.
Committee on Obstetric P. ACOG committee opinion. Exercise during pregnancy and the postpartum period. Number 267, January 2002. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 2002;77(1):79–81.
Wolfe LA, Davies GAL. Canadian guidelines for exercise in pregnancy. Clin Obstet Gynecol. 2003;46(2):488–95.
Danielli M, Gillies C, Thomas RC, Melford SE, Baker PN, Yates T, et al. Effects of supervised exercise on the development of hypertensive disorders of pregnancy: a systematic review and Meta-analysis. J Clin Med. 2022;11(3):793.
Khoram S, Loripoor M, Pirhadi M, Beigi M. The effect of walking on pregnancy blood pressure disorders in women susceptible to pregnancy hypertension: a randomized clinical trial. J Educ Health Promot. 2019;8:95.
Davenport MH, Ruchat S-M, Poitras VJ, Jaramillo Garcia A, Gray CE, Barrowman N, et al. Prenatal exercise for the prevention of gestational diabetes mellitus and hypertensive disorders of pregnancy: a systematic review and meta-analysis. Br J Sports Med. 2018;52(21):1367–75.
Sá JCF, Costa EC, da Silva E, Tamburús NY, Porta A, Medeiros LF, et al. Aerobic exercise improves cardiac autonomic modulation in women with polycystic ovary syndrome. Int J Cardiol. 2016;202:356–61.
Haakstad LAH, Edvardsen E, Bø K. Effect of regular exercise on blood pressure in normotensive pregnant women. A randomized controlled trial. Hypertens Pregnancy. 2016;35(2):170–80.
Turner RM, Jackson D, Wei Y, Thompson SG, Higgins JPT. Predictive distributions for between-study heterogeneity and simple methods for their application in Bayesian meta-analysis. Stat Med. 2015;34(6):984–98.
Friede T, Röver C, Wandel S, Neuenschwander B. Meta-analysis of few small studies in orphan diseases. Res Synth Methods. 2017;8(1):79–91.
Stutzman SS, Brown CA, Hains SMJ, Godwin M, Smith GN, Parlow JL, et al. The effects of exercise conditioning in normal and overweight pregnant women on blood pressure and heart rate variability. Biol Res Nurs. 2010;12(2):137–48.
Barakat R, Perales M, Bacchi M, Coteron J, Refoyo I. A program of exercise throughout pregnancy. Is it safe to mother and newborn? Am J Health Promot. 2014;29(1):2–8.
Fernández-Buhigas I, Brik M, Martin-Arias A, Vargas-Terrones M, Varillas D, Barakat R, et al. Maternal physiological changes at rest induced by exercise during pregnancy: a randomized controlled trial. Physiol Behav. 2020;220:112863.
Petrov Fieril K, Glantz A, Fagevik Olsen M. The efficacy of moderate-to-vigorous resistance exercise during pregnancy: a randomized controlled trial. Acta Obstet Gynecol Scand. 2015;94(1):35–42.
Garnæs KK, Mørkved S, Salvesen Ø, Moholdt T. Exercise training and weight gain in obese pregnant women: a randomized controlled trial (ETIP trial). PLoS Med. 2016;13(7):e1002079.
Kim YJ, Park Y-J. Effect of structured bed exercise on uterine contractions, fetal heart rate patterns, and maternal psychophysical symptoms of hospitalized high-risk pregnant women: a randomized control trial. Asian Nurs Res (Korean Soc Nurs Sci). 2018;12(1):1–8.
Nascimento SL, Surita FG, Parpinelli MÂ, Siani S. Pinto e Silva JL: the effect of an antenatal physical exercise programme on maternal/perinatal outcomes and quality of life in overweight and obese pregnant women: a randomised clinical trial. BJOG. 2011;118(12):1455–63.
Barakat R, Cordero Y, Coteron J, Luaces M, Montejo R. Exercise during pregnancy improves maternal glucose screen at 24-28 weeks: a randomised controlled trial. Br J Sports Med. 2012;46(9):656–61.
Guelfi KJ, Ong MJ, Crisp NA, Fournier PA, Wallman KE, Grove JR, et al. Regular exercise to prevent the recurrence of gestational diabetes mellitus: a randomized controlled trial. Obstet Gynecol. 2016;128(4):819–27.
Halse RE, Wallman KE, Dimmock JA, Newnham JP, Guelfi KJ. Home-based exercise improves fitness and exercise attitude and intention in women with GDM. Med Sci Sports Exerc. 2015;47(8):1698–704.
Seneviratne SN, Jiang Y, Derraik J, McCowan L, Parry GK, Biggs JB, et al. Effects of antenatal exercise in overweight and obese pregnant women on maternal and perinatal outcomes: a randomised controlled trial. BJOG. 2016;123(4):588–97.
Vinter CA, Jensen DM, Ovesen P, Beck-Nielsen H, Jørgensen JS. The LiP (lifestyle in pregnancy) study: a randomized controlled trial of lifestyle intervention in 360 obese pregnant women. Diabetes Care. 2011;34(12):2502–7.
Huifen Z, Yaping X, Meijing Z, Huibin H, Chunhong L, Fengfeng H, Yaping Z. Effects of moderate-intensity resistance exercise on blood glucose and pregnancy outcome in patients with gestational diabetes mellitus: A randomized controlled trial. J Diabetes Complications. 2022;36(5):108186. https://doi.org/10.1016/j.jdiacomp.2022.108186.
Silva-Jose C, Sánchez-Polán M, Diaz-Blanco Á, Coterón J, Barakat R, Refoyo I. Effectiveness of a Virtual Exercise Program During COVID-19 Confinement on Blood Pressure Control in Healthy Pregnant Women. Front Physiol. 2021;12:645136. https://doi.org/10.3389/fphys.2021.645136.
Damm P, Houshmand-Oeregaard A, Kelstrup L, Lauenborg J, Mathiesen ER, Clausen TD. Gestational diabetes mellitus and long-term consequences for mother and offspring: a view from Denmark. Diabetologia. 2016;59(7):1396–9.
Catalano PM, Shankar K. Obesity and pregnancy: mechanisms of short term and long term adverse consequences for mother and child. BMJ. 2017;356:j1.
Neiger R. Long-term effects of pregnancy complications on maternal health: a review. J Clin Med. 2017;6(8):76.
Ruchat S-M, Mottola MF, Skow RJ, Nagpal TS, Meah VL, James M, et al. Effectiveness of exercise interventions in the prevention of excessive gestational weight gain and postpartum weight retention: a systematic review and meta-analysis. Br J Sports Med. 2018;52(21):1347–56.
Genest DS, Falcao S, Gutkowska J, Lavoie JL. Impact of exercise training on preeclampsia: potential preventive mechanisms. Hypertension. 2012;60(5):1104–9.
Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ task force on hypertension in pregnancy. Obstet Gynecol. 2013;122(5):1122–31.
Rudra CB, Williams MA, Lee IM, Miller RS, Sorensen TK. Perceived exertion during prepregnancy physical activity and preeclampsia risk. Med Sci Sports Exerc. 2005;37(11):1836–41.
Saftlas AF, Logsden-Sackett N, Wang W, Woolson R, Bracken MB. Work, leisure-time physical activity, and risk of preeclampsia and gestational hypertension. Am J Epidemiol. 2004;160(8):758–65.
Burgos CSG, Kasawara KT, Costa ML, e Silva JP. PP041. The effect of exercise in pregnant women with chronic hypertension and/or previous preeclampsia on blood pressure and heart rate variability. Pregnancy Hypertens. 2012;2(3):263–4.
Gavard JA, Artal R. Effect of exercise on pregnancy outcome. Clin Obstet Gynecol. 2008;51(2):467–80.
Robledo-Colonia AF, Sandoval-Restrepo N, Mosquera-Valderrama YF, Escobar-Hurtado C, Ramírez-Vélez R. Aerobic exercise training during pregnancy reduces depressive symptoms in nulliparous women: a randomised trial. J Physiother. 2012;58(1):9–15.
de Oliveria Melo AS, Silva JLP, Tavares JS, Barros VO, Leite DFB, Amorim MMR. Effect of a physical exercise program during pregnancy on uteroplacental and fetal blood flow and fetal growth: a randomized controlled trial. Obstet Gynecol. 2012;120(2 Pt 1):302–10.
Mottola MF. Exercise prescription for overweight and obese women: pregnancy and postpartum. Obstet Gynecol Clin N Am. 2009;36(2):301–16.
Acknowledgements
The authors would like to thank all published research that contributed to the data used in this study.
Funding
School-level key project of Jiangsu Vocational Institute of Commerce (JSJM20009), Qing Lan Project of Jiangsu Province, Jiangsu Vocational Institute of Commerce for outstanding youth and Jiangsu Funding Program for Excellent Postdoctoral Talent (2022ZB800).
Author information
Authors and Affiliations
Contributions
Wu Yan, Xu Wang contributed to the study conception and design. Zhu Zhu, Shiping Liu, and Hang Xie contributed to data collection, analysis and interpretation of the data. Zhu Zhu contributed to manuscript drafting. Wu Yan, Zhihua Zhang, Xu Wang, Ruizhe Yang, Juan Yu, Yiping Yan contributed to the review of the manuscript. Zhihua Zhang directed and handled the revise of the manuscript according to reviewer’s comments together with Zhu Zhu, Hang Xie, Wu Yan. All authors read and approved the manuscript for submission.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhu, Z., Xie, H., Liu, S. et al. Effects of physical exercise on blood pressure during pregnancy. BMC Public Health 22, 1733 (2022). https://doi.org/10.1186/s12889-022-14074-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-14074-z