Abstract
Background
Excess body weight (EBW), herein defined as body mass index (BMI) ≥25 kg/m2, is a well-known modifiable risk factor for cancer and a pivotal vector for growing healthcare costs. We estimated the future (2030) federal direct healthcare costs of cancer in the Brazilian Unified Health System (SUS) attributable to EBW. We also projected direct healthcare costs of cancer that could be potentially saved in 2040, considering counterfactual (alternative) scenarios of population-wide reductions in the BMI to be achievedin 2030.
Methods
We developed a macrosimulation model by sex using self-reported BMI data in adults ≥ 20 years who relied exclusively on the public health system from the Brazilian National Health Survey (PNS) 2019; relative risks for 12 types of cancer from the World Cancer Research Fund/American Institute Cancer Research (WCRF/AICR) meta-analysis; and nationwide registries of federal direct healthcare costs of inpatient and outpatient procedures in adults ≥30 years with cancer from 2008-2019. We calculated the attributable costs of cancer via comparative risk assessment, assuming a 10-year lag between exposure and outcome. We used the potential impact fraction (PIF) equation and the Monte Carlo simulation method to estimate the attributable costs and 95% uncertainty intervals, considering the theoretical-minimum-risk exposure and other counterfactual (alternative) scenarios of the EBW prevalence. We assessed the cancer costs attributable to EBW, multiplying PIF by the direct healthcare costs of cancer.
Results
In 2030, 2.4% or US$ 62.8 million in direct healthcare costs of cancer may be attributable to EBW. We projected potential savings of approximately US$ 10.3 to 26.6 million in 2040 by reducing the prevalence of EBW in 2030.
Conclusions
We estimated high future costs of cancer attributable to EBW in Brazil. Our findings may support interventions and policies focused on the primary prevention of EBW and cancer.
Similar content being viewed by others
Background
The prevalence of overweight and obesity has increased over the last decades in Brazil, as in other countries. Between 2008/09 and 2019, the prevalence of excess body weight (EBW, herein defined as body mass index - BMI ≥25 Kg/m2) increased by 20% (from 50.1 to 60.3%), whereas the prevalence of obesity (BMI ≥30 Kg/m2) more than doubled in the same period (from 12.5 to 25.9%) [1]. The increase in the prevalence of EBW will lead to further increases in the burden of non-communicable diseases, such as diabetes, cardiovascular diseases, and cancers [2].
The WCRF/AICR considers the evidence strong that EBW increases the risk of several types of cancer, namely breast (postmenopausal); colorectal; endometrium; gallbladder; kidney; liver; mouth, pharynx, and larynx; esophagus (adenocarcinoma); ovary; pancreas; prostate (advanced stage), and stomach (cardia) [3]. In Brazil, there were an estimated 556,995 new cancer cases in 2020 (excluding non-melanoma skin cancer), of which 64% (n = 357,468) were EBW-related cancers (breast (any): n = 88,492; colorectal: n = 55,102; endometrium: n = 11,791; gallbladder: n = 2,027; kidney: n = 11,971; liver: n = 12,674; mouth, pharynx, and larynx: n = 27,026; esophagus (any): n = 10,363; ovary: n = 7,298; pancreas: n = 13,307; prostate (any): n = 97,278; and stomach (any): n = 20,139) [4]. Additionally, EBW was estimated to account for more than 15 thousand (4%) new cancer cases in Brazil in 2012 and could cause over 29 thousand cancers per year (5%) in 2025 [5].
Primary cancer prevention is imperative to cope with the increasing burden of cancer, particularly in settings with limited access to affordable and effective cancer treatment, such as low- and middle-income countries. It is important to note that the prohibitive’ increase in cancer treatment costs is a concern. We previously estimated the current (2018) federal direct healthcare cost of cancer in the SUS attributable to EBW [6]. In 2018, the Brazilian federal direct healthcare costs of cancer were Int $1.7 billion, of which EBW was estimated to account for 1.8% or Int$ 30 million [6]. In addition to the current cost-of-illness attributable to EBW, quantifying the projected future economic burden of cancer attributable to EBW may inform the potential impact of policies and public health interventions.
Herein, we estimated the future (2030) federal direct healthcare costs of cancer in the SUS attributable to EBW. In addition, we estimated potential savings in federal direct healthcare costs of cancer in 2040 by considering different counterfactual (alternative) scenarios of reduction in the prevalence of EBW to be achieved in 2030.
Methods
Data and study design
This study applied a top-down costing methodology and performed a macrosimulation model to estimate the future costs of cancer attributable to EBW, using the Brazilian population as a case study. We used the following data: 1. Relative risks from WCRF/AICR meta-analyses (Supplementary Material A); 2. Prevalence data (%) of BMI categories in adults aged 20 years or older who relied exclusively on the public health system from the PNS carried out in 2019; 3. Nationwide registries of federal direct healthcare costs of inpatient and outpatient procedures in the SUS in adults aged 30 years or older with cancer. Parameters used in the model are available in Supplementary Material B.
We estimated the impact of EBW on federal direct healthcare costs of cancer, assuming a 10-year time lag between exposure and outcome via comparative risk assessment. We used the potential impact fraction (PIF) equation and the Monte Carlo simulation method to estimate the attributable costs and their 95% uncertainty intervals, considering the theoretical-minimum-risk exposure and other counterfactual (alternative) scenarios of the EBW prevalence. We assessed the cancer costs attributable to EBW, multiplying PIF by the direct healthcare costs of cancer.
Relative risk estimates and cancer sites
We included cancer sites with strong evidence of association (convincing or probable) with EBW according to the WCRF/AICR [3]. We detailed the list of the 10th Revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) codes in Supplementary Material C.
We obtained the relative risks (\({RR}_{x}\)) for EBW-associated cancers incidence by sex from the WCRF/AICR dose-response meta-analysis (Supplementary Material A), considering the increment of \(x\) kg/m2 of BMI (\(x\) = 5)). For prostate (advanced) cancer and ovary cancer, the summary \({RR}_{x}\) included studies with mortality and incidence outcomes. For this reason, we reperformed the WCRF/AICR meta-analysis using random-effects models considering only the incidence as the outcome (Supplementary Material D and E).
We converted these measures per increment of 1 kg/m2 of BMI (\({RR}_{1}\)) using the following equation [7]:
To obtain the RR for each BMI category (RRc) (Supplementary Material F), we used the following equation [8]:
where Mc represents the median value in each category, and ref represents the reference category value (< 25 kg/m2). The reference category reflected the theoretical minimum risk exposure level [3] and the Brazilian National Cancer Institute recommendations [9].
Assessment of EBW prevalence in 2019
We obtained self-reported height and weight from the adult population aged ≥20 years from the PNS 2019 [1], a nationally representative health survey conducted in Brazil. The PNS 2019 microdata are available in the public domain via the Brazilian Institute of Geography and Statistics (IBGE) in partnership with the Ministry of Health at http://www.ibge.gov.br (Supplementary Material G). We considered only adults aged 20 years or older who reported not having health insurance to obtain the prevalence per BMI categories by sex and their corresponding 95% confidence intervals. For postmenopausal breast cancer, we considered women aged 50 years or older. We incorporated the complex sample design into all estimates using RStudio version 1.4.1103.
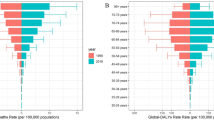
We displayed BMI categories in Fig. 1 and Supplementary Material F. The reference category (BMI < 25 kg/m2) aimed to reflect the theoretical minimum risk exposure level regarding cancer risk [3] and the recommendations of the Brazilian National Cancer Institute (INCA) [9].
Counterfactual (alternative) scenarios for BMI reductions
We proposed four counterfactual (alternative) scenarios of BMI population-wide reductions in 2019 to be achieved in Brazil in 2030 to save direct healthcare costs with cancer in 2040 (Fig. 1). The scenarios considered the following: 1) reduction of BMI distribution to levels observed in the National Household Budget Survey (POF) carried out in 2008/09 [10] (Supplementary Material G); 2) halting the rise in excess body weight prevalence, reaching the BMI distribution to levels observed in 2019; 3) eliminating obesity class II and III (BMI≥35 kg/m2); 4) 1 kg/m2 reduction of BMI’ mean observed in 2019 among participants with BMI ≥ 25 kg/m2 [2]. We based the counterfactual (alternative) scenarios on policy targets [11] and theoretical discussion in the literature [2, 5].
Federal direct healthcare costs of cancer in the Brazilian Unified Health System in 2030 and 2040
We retrieved registries of federal direct healthcare costs of inpatient and outpatient procedures related to cancer between 2008 and 2019 from the Hospital Information System (SIH) and Ambulatory Information System (SIA) of the Brazilian Public Health System (SUS) (Supplementary Material G). We used the 10th Revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) codes for recovering cancer procedures from information systems (Supplementary Material C). We stratified the direct healthcare costs by sex and cancer type. Assuming a 10-year time lag between exposure and outcome, we considered the procedures approved for payment in adults with cancer aged 30 years or older in 2030 and 2040. For postmenopausal breast cancer, we considered women aged 60 years or older.
We performed a simple linear regression to predict the future costs of each cancer type evaluated (dependent variable) as a function of time (independent variable) up to 2030 and 2040 based on the values practiced over time between 2008 and 2019. It is crucial to control for potential confounders while examining the possible determinants of cost. Once our outcome was the direct healthcare costs over time, it was unnecessary to control for confounders because we observed their effect in the observed costs used to fit the regression model [12]. We transformed the monetary values in Brazilian Real (R$) to United States Dollar (US$), considering the purchasing power parity (PPP) of 2019 (conversion factor 2.281) [13].
Cancer cost attributable to EBW
Based on the abovementioned intermediate outputs of the models, we calculated the potential impact fraction (PIF) for EBW-cancers subtypes (Table 1) by sex and counterfactual (alternative) scenario using the following equation [14]:
where \({P}_{i}\) is the proportion of the population at the level \(i\) of BMI category in a given year, \(P^{\prime}_{i}\) is the proportion of the population at the level \(i\) of BMI category in a given counterfactual (alternative) scenario, and \({RR}_{i}\) is the relative risk of cancer subtype (whenever appropriated) at the level \(i\) of BMI. We displayed the levels \(i\) for the BMI category in Supplementary Information B. Of note, the PIF equals the Population Attributable Fraction (PAF) when the counterfactual (alternative) scenario represents the theoretical minimum risk exposure level.
Decision-makers may be more interested in cost by topography (Tables 2 and 3) rather than cancer subtype. Therefore, for esophagus (adenocarcinoma), prostate (advanced), stomach (cardia), and postmenopausal breast cancer, we recalculated the PIF by the topographic site: esophagus, prostate, stomach, and breast (women aged 30 years or older), using the following equation:
We assessed the cancer costs attributable to EBW, multiplying PIF by the cancer costs. We considered the prevalence in 2019 and the costs of cancer in 2030, assuming at least a 10-year time lag between exposure and outcome (i.e., based on the average follow-up time of prospective cohort studies [3]. Finally, we calculated the potential savings in cancer costs in 2040 if reductions in BMI occurred in Brazil to levels fixed in the counterfactual (alternative) scenarios in 2030.
We quantified the uncertainty in all modeled estimates using the Monte Carlo simulation approach [15, 16] with 10,000 iterations. The simulation works thorough producing a draw from the distributions of a) baseline prevalence per BMI category considering a binomial distribution; b) the log of the relative risks per exposition category for the association between EBW and cancer incidence considering a normal distribution. We calculated PIF by sex for the 50th, 2.5th, and 97.5th percentiles as the central estimate and 95% uncertainty intervals across all simulations. Negative values of PIF derived from the Monte Carlo simulation were rounded to 0, assuming that reducing BMI values may not increase the risk of cancer and consequently the attributable costs. We used R Studio version 1.3.1093 for analysis.
Results
Projected federal direct healthcare costs of cancer in Brazil in 2030 attributable to EBW in 2019
In 2030, we projected approximately US$ 2.6 billion federal direct healthcare costs of cancer in Brazil, of which US$ 1.8 billion were estimated to be EBW-related cancers. We estimated that 2.4% (US$ 62.8 million) of federal direct healthcare costs of cancer might be attributable to EBW. Cancers with the highest PIF were estimated to be endometrium (24.6%), followed by liver (19.0%) and kidney (13.8%). Cancers with the highest attributable costs were estimated to be breast (US$ 16.8 million), followed by colorectal (US$ 14.4 million) and endometrium (US$ 9.0 million) (Tables 1 and 2).
The potential impact of the reduction in the prevalence of EBW on projected direct healthcare costs of cancer in Brazil in 2040
We displayed in Fig. 1 the potential reductions (counterfactual/ alternative scenarios) in the prevalence of EBW in Brazil to be achieved in 2030. We projected potential savings of approximately US$ 10.3 to 26.6 million in 2040 by reducing the prevalence of EBW (Table 3). The counterfactual (alternative) scenario with the highest potential impact on cancer costs was the reduction of BMI distribution to levels observed in 2008/09 (US$ 26.55 million), followed for the halting the rise in EBW prevalence, reaching the BMI distribution to levels observed in 2019 (US$ 24.24 million), eliminating obesity class II and III (US$ 12.71 million) and 1 kg/m2 reduction of BMI’ mean observed in 2019 among participants with BMI ≥ 25 kg/m2 (US$ 10.33 million).
Discussion
Our study showed that overweight and obesity may be responsible for US$ 62.8 million federal direct healthcare costs of cancer in 2030, considering the increasing prevalence of overweight and obesity in the last decade, as well as the rising economic burden of cancers in Brazil. Population-wide reductions of BMI to levels fixed in the counterfactual (alternative) scenarios in 2030 could save US$ 10.3 to 24.2 million direct healthcare costs of cancer in 2040.
The detrimental health effects of EBW have been extensively reported. Globally, over 4 million deaths and 140 million disability-adjusted life years (DALYs) are attributable to EBW [17]. Cancer is among the leading causes of EBW-related deaths and DALYs [17]. Globally, approximately 481 thousand new cancer cases or 3.6% of all new cancer cases in adults are attributable to EBW [18]. Attributable cases were higher in countries with high and very high human development indices than low- and middle-income countries [18]. In Brazil, EBW was estimated to account for 15 thousand (4%) new cancer cases in 2012 and may cause over 29 thousand cancers (5%) in 2025 [5].
Several country-wide comparative risk assessment studies have quantified the potential impact of EBW on cancer outcomes [2, 5, 6, 18,19,20], including the economic burden of cancer [6, 21,22,23,24,25,26,27]. In the last decade, costs of cancer attributable to EBW were US$ 43 million in Thailand [25] and US$ 47 million in Ireland [24]. More recently, an Italian cost-of-illness study estimated that EBW was responsible for €13.3 billion in 2020, of which €0.33 were due to direct and indirect costs of cancer [21]. In Brazil, a few studies have quantified the costs of cancer attributable to EBW in Brazil [6, 22, 23]. Direct costs of cancer attributable to EBW in Brazil have ranged from US$ 30 million [6] to US$ 83 million [23]. Variability of results across studies reflects parameters used in the models, such as EBW prevalence, RR, time-lag, and cancer-related costs. Studies have used different methodological approaches to estimate PIF/PAF and included different types of cancers, currencies, and years of reference, which generate difficulties in comparing results.
Our study adds knowledge to the body of evidence by quantifying the future economic burden of cancer attributable to the increasing prevalence of EBW (US$ 62.8 million in 2030). We also projected potential savings in the federal direct healthcare costs of cancer in 2040 (US$ 10.3 to 26.6 million), considering counterfactual (alternative) scenarios of population-wide reductions in the BMI to be achieved in 2030. These results are relevant considering the increasing EBW epidemic worldwide and in Brazil.
Worldwide, the age-adjusted prevalence of obesity tripled between 1975 and 2016 [28]. In 2016, approximately 16% or 650 million adults had obesity [28]. In Brazil, the prevalence of obesity more than doubled in the last decade, increasing from 12.5% in 2008/09 to 25.9% in 2019 [1]. The projected prevalence of obesity in Brazil in 2030 suggest that three out of ten adults will be living with obesity. In addition, the prevalence of obesity classes II and III (≥35 kg/m2) should reach 10% in 2030 [Estivaleti JM, Guzman-Habinger J, Lobos J, Azeredo CM, Claro R, Ferrari G, Adami F, Rezende LFM, unpublished observations].
Hypotheses about the causes of the rising obesity epidemic globally are abundant. More than 30 years ago, Geoffrey Rose noted that etiology confronts two distinct issues: the determinants of individual cases and the determinants of incidence rate [29]. Notably, the determinants of incidence may not be the same as the determinants of individual cases [29]. Genetic predisposition, for instance, could explain where individuals are placed on the distribution of individual weights. However, they do not explain why the body mass has shifted towards heavier weights so rapidly in many populations [30]. The EBW determinants also incorporate several economic, social, and behavioral factors present in modern societies, including social and economic inequalities, an increased offer of high energy density foods, and sedentary behavior [31].
However, the rising share of ultra-processed foods in the food supply has been proposed as the most crucial cause of the obesity epidemic (determinant of incidence rate) [32, 33]. Changes in the food systems during the 70s have led to a rapid increase in food energy availability, particularly towards increased consumption of ultra-processed foods [30, 32, 33]. A recent systematic review of dietary surveys showed that the contribution of ultra-processed foods to total energy intake ranged from 16% in Colombia to 58% in the USA [34]. In Brazil, the contribution of ultra-processed foods to total energy intake increased from 14.3% in 2002 to 19.7% in 2017-18 [35]. Since these changes in the food system, the contribution of ultra-processed food in the population dietary patterns, as the whole population distribution of BMI, has shifted to the right, independent of age group and sex [30, 32]. These observations of period effect are strong signals that changes in the food systems are likely the primary determinant of the obesity epidemic [30]. Policies and public health interventions to reduce the consumption of ultra-processed foods are imperative to reverse the obesity epidemic. Examples include taxation, marketing restrictions, adequate labeling, environmental changes, and public health campaigns. These actions may have benefits for preventing diseases as well as economic benefits.
Our results showed that reductions in the prevalence of EBW through these actions might have economic benefits, mainly to cope with the increasing economic burden of cancer. For instance, we estimated that the highest potential impact on cancer costs was the reduction of BMI distribution to levels observed in 2008/09 (US$ 26.55 million), followed for the halting the rise in EBW prevalence, reaching the BMI distribution to levels observed in 2019 (US$ 24.24 million), eliminating obesity class II and III (US$ 12.71 million) and 1 kg/m2 reduction of BMI’ mean observed in 2019 among participants with BMI ≥ 25 kg/m2 (US$ 10.33 million). To achieve these (bold) scenarios, we need a comprehensive set of integrated actions, including health-promoting environments (e.g., healthy urban planning, community action, improving food and beverage supply, marketing restrictions, fiscal policies, creating and healthy and packaging and labeling improvements), communication for behavior change (e.g., health education actions, advice in health services, information campaigns) and change in the food system (e.g., intersectoral integrated actions).
To our knowledge, this is the first study aimed at quantifying the future economic burden of cancer attributable to EBW and the potential savings in federal direct healthcare costs of cancer by reducing population-wide BMI. We used an extensive, nationally representative survey of Brazilian adults, relative risks from meta-analysis, and nationwide registries of direct healthcare costs of cancers in the Brazilian Unified Health System. However, our study has some limitations. To estimate the PIF/PAF, we used information on self-reported weight and height, which may have led to misclassification bias of BMI categories. We assumed the pooled relative risks from meta-analysis, which did not include Brazilian cohort studies. Nevertheless, we performed the Monte Carlo simulation approach to incorporate the uncertainty of PIF/PAF estimates. We assumed at least a 10-year time lag between BMI and cancers and did not consider recurring events. Our counterfactual (alternative) scenarios considered the potential effect of the BMI reduction on increased cancer risk and its associated costs. We did not consider the adverse effects of the increase in the proportion of the adults in the BMI category < 25kg/m2, such as the increased risk of premenopausal breast cancer. On the other hand, in Brazil, only about 30% of new cases [4] and costs of breast cancer occur in premenopausal women, and this phenomenon (lower BMI increasing the cancer risk) has not been observed for other cancer types. Finally, our risk assessment model did not consider different lifetime BMI trajectories (e.g., cancer risk in people who lived overweight in childhood and young adulthood vs. those who gained weight in adulthood).Future studies may use other modeling approaches (e.g., multistate lifetable modeling of preventive interventions) to incorporate disease status and time dimension more appropriately [36].
Conclusions
EBW may be responsible for 2.4% or US$ 62.8 million federal direct healthcare costs of cancer in 2030. We projected potential savings of approximately US$ 10.3 to 24.2 million in 2040 via population-wide reductions of BMI. Our findings may be helpful to support policies aimed at EBW and cancer prevention strategies in Brazil.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- BMI:
-
Body mass index
- DALY:
-
Disability-adjusted life years
- EBW:
-
Excess body weight
- IBGE:
-
Brazilian Institute of Geography and Statistics
- INCA:
-
Brazilian National Cancer Institute
- ICD-10:
-
10th Revision of the International Statistical Classification of Diseases and Related Health Problems
- PAF:
-
Population Attributable Fraction
- PIF:
-
Potential Impact Fraction
- POF:
-
Brazilian National Household Budget Survey
- PNS:
-
Brazilian National Health Survey
- PPP:
-
Purchasing power parity
- RR:
-
Relative risk
- SIA-SUS:
-
Ambulatory Information System of the Brazilian Unified Health System
- SIH-SUS:
-
Hospital Information System of the Brazilian Unified Health System
- SUS:
-
Brazilian Unified Health System
- WCRF/AICR:
-
World Cancer Research Fund/American Institute Cancer Research
References
Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde: 2019: Atenção Primária à Saúde e Informações Antropométricas. Microdados. 2020. https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html?=&t=microdados. Accessed 15 Mar 2021.
Rabacow FM, Azeredo CM, Rezende LFM. Deaths attributable to high body mass in Brazil. Prev Chronic Dis. 2019;16:E141. https://doi.org/10.5888/pcd16.190143. PMID: 31625870; PMCID: PMC6824148.
World Cancer Research Fund, American Institute for Cancer Research. Continous update project expert report 2018. Body fatness and weight gain and the risk of cancer. 2018. https://www.wcrf.org/diet-and-cancer/. Accessed 15 Jan 2021.
Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F. Global cancer observatory: cancer today. https://gco.iarc.fr/today/home. Accessed 4 May 2022.
Rezende LFM, Arnold M, Rabacow FM, Levy RB, Claro RM, Giovannucci E, Eluf-Neto J. The increasing burden of cancer attributable to high body mass index in Brazil. Cancer Epidemiol. 2018;54:63–70. https://doi.org/10.1016/j.canep.2018.03.006. Epub 2018 Mar 28. PMID: 29604601.
Corrêa Ferreira da Silva R, Bahia LR, Machado da Rosa MQ, Malhão TA, Mendonça EP, Rosa RDS, Araújo DV, Maya Moreira LG, Schilithz AOC, Diogenes Melo MEL. Costs of cancer attributable to excess body weight in the Brazilian public health system in 2018. PLoS One. 2021;16(3):e0247983. https://doi.org/10.1371/journal.pone.0247983. PMID: 33705455; PMCID: PMC7951921.
Islami F, Goding Sauer A, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, McCullough ML, Patel AV, Ma J, Soerjomataram I, Flanders WD, Brawley OW, Gapstur SM, Jemal A. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018;68(1):31–54. https://doi.org/10.3322/caac.21440. Epub 2017 Nov 21. PMID: 29160902.
Brenner DR, Poirier AE, Ruan Y, Hebert LA, Grevers X, Walter SD, Villeneuve PJ, Friedenreich CM, ComPARe Study Team. Estimates of the current and future burden of cancer attributable to excess body weight and abdominal adiposity in Canada. Prev Med. 2019;122:49–64. https://doi.org/10.1016/j.ypmed.2019.03.014. PMID: 31078173.
Instituto Nacional de Câncer José Alencar Gomes da Silva. Dieta, nutrição, atividade física e câncer: uma perspectiva global: um resumo do terceiro relatório de especialistas com uma perspectiva brasileira. 2020. https://www.inca.gov.br/sites/ufu.sti.inca.local/files/media/document/dieta_nutricao_atividade_fisica_e_cancer_resumo_do_terceiro_relatorio_de_especialistas_com_uma_perspectiva_brasileira.pdf. Accessed 15 Mar 2021.
Instituto Brasileiro de Geografia e Estatística. Pesquisa de orçamentos familiares 2008-2009: Análise do consumo alimentar pessoal no Brasil. Microdados. 2011. https://www.ibge.gov.br/estatisticas/sociais/rendimento-despesa-e-consumo/9050-pesquisa-de-orcamentos-?=&t=microdados. Accessed 15 Mar 2021.
Brasil. Ministério da Saúde. Plano de ações estratégicas para o enfrentamento das doenças crônicas e agravos não transmissíveis no Brasil 2021-2030. 2021. https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/publicacoes-svs/doencas-cronicas-nao-transmissiveis-dcnt/09-plano-de-dant-2022_2030.pdf. Accessed 15 Dec 2021.
Ward ZJ, Bleich SN, Cradock AL, Barrett JL, Giles CM, Flax C, Long MW, Gortmaker SL. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381(25):2440–50. https://doi.org/10.1056/NEJMsa1909301. PMID: 31851800.
Organisation for Economic Cooperation and Development. Purchasing power parities (PPP) (indicator). Total, national currency units/US dollar, 2000–2019. 2021. https://data.oecd.org/conversion/purchasing-power-parities-ppp.htm. Accessed 15 Oct 2021.
Vander Hoorn S, Ezzati M, Rodgers A, Lopez AD, Murray CJL. Estimating attributable burden of disease from exposure and hazard data. In: Ezzati M, Rodgers A, Lopez AD, Rodgers A, Murray CJL, editors. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. Geneva: World Health Organization; 2004. p. 2129–40. https://www.who.int/publications/cra/chapters/volume2/2129-2140.pdf. Accessed 15 Jan 2021.
Steenland K, Greenland S. Monte Carlo sensitivity analysis and Bayesian analysis of smoking as an unmeasured confounder in a study of silica and lung cancer. Am J Epidemiol. 2004;160:384–92. https://doi.org/10.1093/aje/kwh211. PMID: 15286024.
Greenland S. Interval estimation by simulation as an alternative to and extension of confidence intervals. Int J Epidemiol. 2004;33(6):1389–97. https://doi.org/10.1093/ije/dyh276. Epub 2004 Aug 19. PMID: 15319402.
Dai H, Alsalhe TA, Chalghaf N, Riccò M, Bragazzi NL, Wu J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: an analysis of the Global Burden of Disease Study. PLoS Med. 2020;17(7):e1003198. https://doi.org/10.1371/journal.pmed.1003198. PMID: 32722671; PMCID: PMC7386577.
Arnold M, Pandeya N, Byrnes G, Renehan PAG, Stevens GA, Ezzati PM, Ferlay J, Miranda JJ, Romieu I, Dikshit R, Forman D, Soerjomataram I. Global burden of cancer attributable to high body-mass index in 2012: a population-based study. Lancet Oncol. 2015;16(1):36–46. https://doi.org/10.1016/S1470-2045(14)71123-4. Epub 2014 Nov 26. PMID: 25467404; PMCID: PMC4314462.
Rezende LFM, Murata E, Giannichi B, Tomita LY, Wagner GA, Sanchez ZM, Celis-Morales C, Ferrari G. Cancer cases and deaths attributable to lifestyle risk factors in Chile. BMC Cancer. 2020;20(1):693. https://doi.org/10.1186/s12885-020-07187-4. PMID: 32711508; PMCID: PMC7382839.
Rezende LFM, Lee DH, Louzada MLDC, Song M, Giovannucci E, Eluf-Neto J. Proportion of cancer cases and deaths attributable to lifestyle risk factors in Brazil. Cancer Epidemiol. 2019;59:148–57. https://doi.org/10.1016/j.canep.2019.01.021. Epub 2019 Feb 14. PMID: 30772701.
d’Errico M, Pavlova M, Spandonaro F. The economic burden of obesity in Italy: a cost-of-illness study. Eur J Health Econ. 2022;23(2):177–92. https://doi.org/10.1007/s10198-021-01358-1. Epub 2021 Aug 4. PMID: 34347176; PMCID: PMC8882110.
Bahia L, Coutinho ES, Barufaldi LA, Abreu Gde A, Malhão TA, de Souza CP, Araujo DV. The costs of overweight and obesity-related diseases in the Brazilian public health system: cross-sectional study. BMC Public Health. 2012;12:440. https://doi.org/10.1186/1471-2458-12-440. PMID: 22713624; PMCID: PMC3416687.
de Oliveira ML, Santos LM, da Silva EN. Direct healthcare cost of obesity in brazil: an application of the cost-of-illness method from the perspective of the public health system in 2011. PLoS One. 2015;10(4):e0121160. https://doi.org/10.1371/journal.pone.0121160. PMID: 25830909; PMCID: PMC4382114.
Dee A, Callnan A, Doherty E. Correction. Overweight and obesity on the island of Ireland: an estimation of costs. BMJ Open. 2015;5(3):e006189corr1. https://doi.org/10.1136/bmjopen-2014-006189corr1. Erratum for: BMJ Open. 2015;5(3):e006189. PMID: 25829368; PMCID: PMC4386213.
Pitayatienanan P, Butchon R, Yothasamut J, Aekplakorn W, Teerawattananon Y, Suksomboon N, Thavorncharoensap M. Economic costs of obesity in Thailand: a retrospective cost-of-illness study. BMC Health Serv Res. 2014;14:146. https://doi.org/10.1186/1472-6963-14-146. PMID: 24690106; PMCID: PMC4109797.
Lehnert T, Streltchenia P, Konnopka A, Riedel-Heller SG, König HH. Health burden and costs of obesity and overweight in Germany: an update. Eur J Health Econ. 2015;16(9):957–67. https://doi.org/10.1007/s10198-014-0645-x. Epub 2014 Nov 8. PMID: 25381038.
Hong YR, Huo J, Desai R, Cardel M, Deshmukh AA. Excess costs and economic burden of obesity-related cancers in the United States. Value Health. 2019;22(12):1378–86. https://doi.org/10.1016/j.jval.2019.07.004. Epub 2019 Aug 20. PMID: 31806194; PMCID: PMC7313233.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–42. https://doi.org/10.1016/S0140-6736(17)32129-3. Epub 2017 Oct 10. PMID: 29029897; PMCID: PMC5735219.
Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30(3):427–32. https://doi.org/10.1093/ije/30.3.427 discussion 433-4. PMID: 11416056.
Rodgers A, Woodward A, Swinburn B, Dietz WH. Prevalence trends tell us what did not precipitate the US obesity epidemic. Lancet Public Health. 2018;3(4):e162–3. https://doi.org/10.1016/S2468-2667(18)30021-5. Epub 2018 Mar 1. PMID: 29501260.
The Lancet Public Health. Tackling obesity seriously: the time has come. Lancet Public Health. 2018;3(4):e153. https://doi.org/10.1016/S2468-2667(18)30053-7. PMID: 29627076.
Vandevijvere S, Jaacks LM, Monteiro CA, Moubarac JC, Girling-Butcher M, Lee AC, Pan A, Bentham J, Swinburn B. Global trends in ultraprocessed food and drink product sales and their association with adult body mass index trajectories. Obes Rev. 2019;20(Suppl 2):10–9. https://doi.org/10.1111/obr.12860. Epub 2019 May 17. PMID: 31099480.
Bleich S, Cutler D, Murray C, Adams A. Why is the developed world obese? Annu Rev Public Health. 2008;29:273–95. https://doi.org/10.1146/annurev.publhealth.29.020907.090954. PMID: 18173389.
Pagliai G, Dinu M, Madarena MP, Bonaccio M, Iacoviello L, Sofi F. Consumption of ultra-processed foods and health status: a systematic review and meta-analysis. Br J Nutr. 2021;125(3):308–18. https://doi.org/10.1017/S0007114520002688. Epub 2020 Aug 14. PMID: 32792031; PMCID: PMC7844609.
Instituto Brasileiro de Geografia e Estatística. Pesquisa de orçamentos familiares: POF 2017-2018: avaliação nutricional da disponibilidade domiciliar de alimentos no Brasil. 2020. https://biblioteca.ibge.gov.br/visualizacao/livros/liv101704.pdf. Accessed 15 Nov 2021.
Blakely T, Moss R, Collins J, Mizdrak A, Singh A, Carvalho N, Wilson N, Geard N, Flaxman A. Proportional multistate lifetable modelling of preventive interventions: concepts, code and worked examples. Int J Epidemiol. 2020;49(5):1624–36. https://doi.org/10.1093/ije/dyaa132. PMID: 33038892.
Acknowledgments
To Fabio Fortunato Brasil de Carvalho for reviewing the article.
Funding
This research received financial support from Climate and Land Use Alliance (CLUA) (Grant Number G-2007-56990). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript and does not necessarily share the positions expressed in the Grantee’s publication.
Author information
Authors and Affiliations
Contributions
LFMR, RSB, and TAM conducted the data acquisition and analysis. LFMR prepared the first draft of the manuscript and TAM prepared tables and figures. All authors substantially contributed to the conception and design of the work and participated in the interpretation of data. All authors substantively revised the work, approved the submitted version, and agreed both to be personally accountable for the author’s contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. Although datasets were publicly available and contain deidentified participants data, ethics approval was obtained from the Institutional Review Board of the Brazilian National Cancer Institute José Alencar Gomes da Silva (INCA) at the Brazilian Ministry of Health (MS) (CAAE 12008119.8.0000.5274).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Material A.
World Cancer Research Fund/ American Institute for Cancer Research meta-analysis references. Supplementary Material B. Parameters considered in the macrosimulation model. Supplementary Material C. 10th revision of the International Statistical Classification of Diseases and Related Health Problems codes. Supplementary Material D. Meta-analysis of prostate (advanced) cancer by incidence as outcome. Supplementary Material E. Meta-analysis of ovary cancer by incidence as outcome. Supplementary Material F. Relative risk of excess body weight-associated cancers per exposition category and sex. Supplementary Material G. Hyperlinks to publicly archived datasets.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rezende, L.F.M., Malhão, T.A., da Silva Barbosa, R. et al. The future costs of cancer attributable to excess body weight in Brazil, 2030-2040. BMC Public Health 22, 1236 (2022). https://doi.org/10.1186/s12889-022-13645-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13645-4