Abstract
Background
Cigarette smoking, secondhand cigarette smoke (SHS) exposure, and e-cigarette use (“vaping”) are each associated with increased rates of depressive symptoms and other internalizing mental health disorders. The prevalence of vaping has increased greatly, yet the mental health correlates of secondhand exposure to e-cigarette emissions are as yet to be investigated. This study examined the potential adverse mental health outcomes associated with different tobacco exposures (direct and passive), with a particular focus on the mental health correlates of secondhand exposure to e-cigarette emissions.
Methods
The Population Assessment of Tobacco and Health Study data collected from a sample of 16,173 Wave 4 adults were used to test the hypothesis that secondhand e-cigarette emissions exposure is associated with increased odds of internalizing mental health disorders. Individuals were categorized as exclusive cigarette smokers, exclusive e-cigarette users, cigarette and e-cigarette dual users, exclusive noncombustible tobacco users, secondhand smoke exposed non-users, secondhand e-cigarette emissions exposed non-users, and non-users with no current SHS/secondhand e-cigarette aerosol exposure. Adjusted weighted logistic regression analysis was used to investigate the association between exposure type and internalizing problems as assessed by scores on the Global Appraisal of Individual Needs-Short Screener (GAIN-SS), a widely used instrument for assessing mental health problems.
Results
Cigarette smokers (AOR = 2.53, 95% CI: 2.19–2.92), e-cigarette users (AOR = 3.14, 2.41–4.09), dual users (AOR = 3.37, 2.85–4.00), noncombustible tobacco users (AOR = 1.48, 1.01–2.17), SHS exposed non-users (AOR = 1.63, 1.37–1.94), and secondhand e-cigarette emissions exposed non-users (AOR = 1.43, 1.03–1.99) were each associated with increased odds of moderate to severe internalizing mental health problems as compared to unexposed non-users. Odds of internalizing problems among SHS and secondhand e-cigarette emissions exposed non-users did not differ (p = 0.46).
Conclusions
This is the first study, to our knowledge, to identify an association between recent secondhand exposure to e-cigarette emissions and mental health problems, and the risk is comparable to that of SHS. Corroboration of this relationship needs further research to explicate directionality and mechanisms underlying this association.
Similar content being viewed by others
Background
Tobacco use, principally as cigarette smoking, continues to be the leading preventable cause of premature death globally [1]. While cigarette use in the US continues to decline, there has been a remarkably rapid uptake of electronic cigarette (e-cigarette) use, called “vaping” [2], since their introduction to the US market in 2007 [3]. Despite a decline in overall e-cigarette use in 2020, it remains exceedingly popular among tobacco-naive middle and high school aged adolescents, and the Centers for Disease Control and Prevention notes that “youth e-cigarette use remains an epidemic” [4]. The widespread adoption of vaping by adolescents has led to a great concern that e-cigarettes may foster a new wave of nicotine dependence, thereby endangering the successes of more than a half century of tobacco control efforts [3].
The risks associated with e-cigarette use remains controversial within the scientific and public health communities [5]. Debate has largely centered on their potential to aid in harm reduction (i.e., whether they are a safer alternative to cigarette smoking and whether their use will abate cigarette use) [6, 7], as well as their potential to enlist tobacco-naïve adolescents and young adults to become dependent on nicotine via new nicotine delivery devices [8]. In addition, there remains a paucity of evidence regarding the potential for e-cigarette use in causing adverse acute and long-term physical and mental health consequences. Even less currently is known about the potential adverse health effects of exposure to secondhand e-cigarette emissions. This is particularly troubling given the wide ranging and pervasive nature of adverse effects associated with secondhand smoke (SHS) exposure and the prevailing perception by the general public that passive exposure to e-cigarette emissions is safe—a premise that has been reinforced by e-cigarette advertising campaigns and media coverage [9,10,11].
Mental health problems, well recognized to be among the most pervasive and pernicious of public health problems, can dramatically impair quality of life and overall health. “Internalizing disorders” is a term commonly used by mental health professionals—and referenced in the Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5)—to denote a major category of emotional and behavioral problems characterized by symptoms and feelings of depression, anxiety, and/or social withdrawal [12, 13]. Externalizing problems, in contrast, are characterized by aggressive, oppositional defiant and anti-social emotional states and behaviors [13]. Internalizing problems present a significant disease burden worldwide: depressive disorders and anxiety disorders, which are highly interrelated and often co-occur [14], are very common psychiatric problems [15]. It is estimated that 20% of the US population will suffer a depressive disorder at some point during their lifetime [14]. In 2019, the global burden of depressive disorders impacted 279 million people, leading to 46.8 million Disability-Adjusted Life Years (DALYs) [16]; similarly, anxiety disorders affected 301 million people worldwide, leading to 28.7 million DALYs [16].
It is well established that cigarette smokers are at increased risk for mental health disorders [17,18,19]. Similarly, those exposed to SHS have increased depressive and other internalizing problems. It has been shown that non-smokers reporting substantial SHS exposure are nearly 50% more likely to experience psychological distress [20]. The relationship between SHS exposure and increased rates of internalizing problems such as depression, anxiety, and panic attacks has been found in the US [21, 22], Korea [23,24,25,26,27,28], Canada [29], Germany [30], Japan [31, 32], and China [33, 34], with some demonstrating dose-response relationships [34]. A growing literature suggests that vaping e-cigarettes is independently associated with increased rates of depressive symptoms specifically [35,36,37,38,39], and internalizing disorders broadly [40,41,42,43,44,45]. To our knowledge, no research has: 1) examined the relationship between internalizing mental health disorders among persons with no history of tobacco product use but who are passively exposed to e-cigarette emissions, or 2) directly compared the odds of internalizing problems among consumers of different tobacco products. Improved understanding of the association between different tobacco exposures (via consumption or passive inhalation) and potential adverse mental health outcomes may have substantial implications both for mental health interventions and for tobacco control efforts.
The aim of the current study is to use a nationally representative dataset to investigate potential adverse mental health outcomes associated with different tobacco exposures (direct and passive), with a particular focus on secondhand exposure to e-cigarette emissions. We hypothesized that passive exposure to e-cigarette emissions, as well as e-cigarette consumption (i.e., vaping) is associated with an increased risk of internalizing mental health disorders.
Methods
The Population Assessment of Tobacco and Health (PATH) Study is a nationally representative, cohort study of tobacco products and associated health outcomes. Secondary analyses of adult data (≥ 18 years old) from Wave 4 (December 2016–January 2018) of the PATH study (n = 16,173) were conducted. The fourth wave was used as it was the most recently available data for public use at the time of analysis. Details regarding the PATH study design are available online [46].
Tobacco use/exposure status
Two types of tobacco product exposure were evaluated: that resulting from direct tobacco product consumption, and that resulting from passive exposure to tobacco product emissions. Tobacco product status was determined based on use or exposure at least once within the past 30 days.
Subjects were assigned to a binary tobacco use/exposure category based on responses to queries about former and current tobacco product use or passive exposure. Former smoking status was determined using the PATH derived variable indicating former established cigarette smokers who have smoked at least 100 cigarettes in their lifetime, but had not smoked within the past 12 months. Current tobacco product use was determined based on responses to questions regarding cigarette smoking (“In the past 30 days, have you smoked a cigarette, even one or two puffs?”), e-cigarette use (“In the past 30 days, have you used an electronic nicotine product, even one or two times?”), and noncombustible tobacco use (“Have used smokeless tobacco/snus pouches/dissolvable tobacco within the past 30 days”). The exclusive e-cigarette use and non-combustible tobacco use groups were further categorized by former smoking status, as previously defined, to differentiate between those with and without a history of smoking.
SHS exposure (either residential or occupational) was determined based on self-reports of recent exposure (“Today”, “In the past week,” “In the past two weeks,” or “In the past month”) to the question “How recently did someone smoke around you while you were at work?” or the selection of a combustible tobacco product (‘smoke cigarettes, cigars, cigarillos or filtered cigars and pipe tobacco’) in response to the question: “Does anyone who lives with you now do any of the following…?”). Passive residential or occupational e-cigarette exposure was determined based on self-reports of recent exposure (“Today”, “In the past week,” “In the past 2 weeks,” or “In the past month”) to the question “How recently did someone use e-cigarettes or other electronic nicotine products around you while you were at work?” or the selection of exclusive e-product use when asked: “Does anyone who lives with you now do any of the following…?”
Non-users were defined as individuals who reported no current tobacco product use, no exposure to tobacco product emissions (residential or occupational), and no history of cigarette smoking.
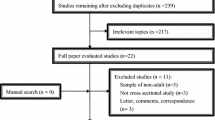
Therefore, nine categories were identified (Fig. 1): (1) Exclusive cigarette smoker (n = 7005), (2) exclusive e-cigarette user with no history of smoking (n = 487), (3) exclusive e-cigarette user with a history of smoking (n = 465), (4) dual user of combustible cigarettes and e-cigarettes (n = 1327), (5) exclusive noncombustible tobacco user with no history of smoking (n = 332), (6) exclusive noncombustible tobacco user with a history of smoking (n = 323), (7) non-user exposed to passive SHS (n = 2673), (8) non-user exposed to passive e-cigarette emissions (n = 337), and (9) non-user with no passive exposure to tobacco product emissions (n = 3224).
Internalizing mental health disorders
Internalizing mental health problems were assessed using the Global Appraisal of Individual Needs-Short Screener (GAIN-SS), a diagnostic tool that screens for internalizing and externalizing problems that has been validated for clinical decision-making cut-points with great sensitivity and for disorder identification with great specificity [47, 48]. The GAIN-SS probes four items associated with internalizing disorders: 1) feeling very trapped, lonely, sad, blue, depressed, or hopeless about the future; 2) sleep trouble such as bad dreams, sleeping restlessly, or falling asleep during the day; 3) feeling very anxious, nervous, tense, scared, panicked, or like something bad was going to happen; and 4) becoming very distressed and upset when something reminded you of the past [49]. The number of items endorsed over the past 12 months are summed to yield an internalizing problem score between 0 and 4, which is used to determine severity: low (0–1 symptom), moderate (2–3 symptoms), or high (4 symptoms) [47, 49,50,51,52]. Individuals with a score = 4 were characterized as having severe internalizing problems. For the purposes of our analyses, individuals with an internalizing GAIN-SS score ≥ 2 were characterized as having moderate to severe internalizing problems.
Covariates
Participants reported socio-demographic characteristics including sex (male / female), age group (18–34 years / 35–55 years / ≥55 years), race/ethnicity (non-Hispanic white / non-Hispanic black / Hispanic / non-Hispanic other), and annual household income (<$49,999 / $50,000 - $99,999/ above $100,000). Body mass index (BMI) was derived via questionnaire data and categorized as underweight (below 18.5), normal or healthy weight (18.5–24.9), overweight (25.0–29.9), and obese (30.0 and above) [53]. Chronic condition was categorized by self-report of a professional diagnosis for any chronic conditions (i.e. heart disease, diabetes, cancer, chronic obstructive pulmonary disease, and stroke) in the past 12 months [54]. We excluded 59 participants with missing data on covariates.
Statistical analyses
Univariate data analyses were conducted to examine the frequency and proportion of study variables. Bivariate data analyses were performed to assess the association between internalizing problems and potential covariates. Logistic regression analyses were conducted to assess the association between tobacco product use status/secondhand exposure type and moderate to severe internalizing problems (GAIN-SS scores ≥2), adjusted for covariates. To study how sensitive the association between tobacco product use/exposure type and internalizing problems was to the cut-point of GAIN-SS score, we conducted two additional logistic regression analyses using the cut-points ≥ 3 and = 4. Adjusted odds ratios (AORs) and the 95% confidence intervals (95% CI; estimated using balanced repeated replication method) are reported [55]. Sampling weights were implemented in all analyses unless indicated otherwise. Weighting procedures were used to correct for differential probability of survey selection, nonresponse, and sampling frame bias; therefore, the weighted sample represents the US adult population at the time of data collection. All data analyses were performed using SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Univariate and bivariate analyses
Descriptive statistics for characteristics of the study sample and the results of bivariate analyses are presented in Table 1. Most participants were younger than 55 years of age (77.1%) and were non-Hispanic White (62.4%). Approximately half of the sample were women (49.9%). One third of participants scored moderate-to-severe (≥2) on the GAIN-SS (34.8%). Fewer than half of these individuals had a GAIN-SS = 4 (15.4%). Moderate to severe internalizing GAIN-SS scores were associated with each category of tobacco use and exposure status, age, race/ethnicity, sex, annual family income, BMI, and chronic disease conditions in the past 12 months. Crude odds ratios for moderate to severe internalizing problems are presented in Table S1.
Logistic regression analyses
Weighted logistic regression models were conducted to examine the associations between tobacco product use or exposure status (nine categories in Fig. 1) and internalizing problems, adjusting for covariates (Fig. 2). Compared to non-users with no passive exposure to tobacco product emissions, dual tobacco product users (i.e., persons who use both cigarettes and e-cigarettes) had the highest odds of moderate to severe internalizing problems (AOR = 3.37, 95% CI: 2.85, 4.00). Exclusive e-cigarette users with no history of smoking were at greater risk for a GAIN-SS ≥2 than were exclusive cigarette smokers (AOR = 3.14; 95% CI: 2.41, 4.09 and AOR = 2.53; 95% CI: 2.19, 2.93, respectively), although these odds were not statistically different (p = 0.09). However, exclusive e-cigarette users that reported a smoking history were lower still (AOR = 2.30, 95% CI: 1.78, 2.99). Risk of moderate to severe internalizing problems (GAIN-SS ≥2) among noncombustible tobacco users were lower than that of individuals who currently use an inhalable tobacco product, regardless of whether they had a history of cigarette smoking (AOR = 1.65, 95% CI: 1.2, 2.26) or not (AOR = 1.48, 95% CI: 1.01, 2.17).
Among non-users, the odds of moderate to severe internalizing problems (GAIN-SS ≥2) were higher for those passively exposed to tobacco product emissions, regardless of the tobacco product source, as compared with non-users with no passive exposure to tobacco product emissions (SHS exposure AOR = 1.63, 95% CI: 1.37, 1.94; e-cigarette aerosol exposure AOR = 1.43, 95% CI: 1.03, 1.99) (Fig. 2).
Results also indicate that moderate to severe internalizing problems were associated with younger age, female sex, non-Hispanic White race/ethnicity, lower annual household income, and diagnosis of chronic disease in the past 12 months, but not BMI (see Table S1).
After assessing the additional cut-points for internalizing problems, we found consistent results that any category of tobacco product use or exposure is associated with an increased likelihood of internalizing problems (Table 2). At the two most severe cut-points for internalizing problems, however, the differences between non-users passively exposed to e-cigarette emissions and the non-user reference group do not reach statistical significance. Regardless of cut-point, dual use always had the highest AOR, and there was no difference in AORs between those exposed to secondhand smoke or e-cigarette emissions. In addition, the relative elevated risk for internalizing problems for each tobacco product use/exposure category followed a similar rank order.
Discussion
This is the first study that we are aware of to identify an association between recent exposure to secondhand e-cigarette emissions and moderate to severe internalizing problems, and the risk was found to be comparable to that of SHS exposure in this large, nationally representative sample of the US adult population. Consistent with the literature on combustible cigarette smoking [56,57,58,59,60], SHS exposure [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34], and more recently e-cigarette use [35, 39, 61, 62], the data in the current study indicate that every category of tobacco product use or exposure assessed was associated with an increased likelihood of mental health problems. Of all categories of tobacco use/exposure, dual users of combustible and e-cigarettes had the highest risk. These associations remained significant even after controlling for multiple other characteristics that are known to be highly associated with internalizing problems such as sex, race/ethnicity, age, chronic health conditions, annual income, and BMI [63,64,65,66,67].
Similar to the results presented here, earlier population-based cross-sectional studies have found that smoking is associated with internalizing disorders, such as depression [68] and anxiety [58,59,60, 69], and that the prevalence of cigarette smoking is higher among those with psychiatric diagnoses when compared to the general population [17,18,19]. Previous research has attempted to interpret such findings by proposing that users with emotional dysfunctions depend on cigarettes to self-medicate [70,71,72], as depressed individuals have been found to smoke at increased rates and with greater intensity due to low positive affect, high negative affect and cognitive impairment [56]. Currently, there is a lack of consensus on the directionality of this relationship, i.e. some longitudinal studies have found that tobacco use precedes depressive and anxiety disorders [73,74,75,76,77]; whereas others have found evidence that depression is associated with future tobacco use [78]. Still other studies have found evidence of a bidirectional relationship, where both tobacco use and internalizing mental health disorders are independent risk factors for one another [79, 80]. Well-designed, longitudinal research is needed to further investigate the critical issue of directionality, with a particular focus on e-cigarette use.
A more recent and limited literature has found that similar to smoking, e-cigarette use appears to be associated with increased levels of psychological distress, possibly in a dose-response fashion [81]. Increasing evidence is accumulating that illustrates a relationship between e-cigarette use and internalizing disorders [40,41,42,43,44,45], and more specifically e-cigarette use and depression among adults [35,36,37,38,39] and children/adolescents [82,83,84,85]. Whether e-cigarette use is associated with anxiety disorders is less well characterized [86, 87]. Dual use of combustible and electronic cigarettes has been consistently linked to depressive/internalizing disorders [36, 43, 61, 83, 88, 89]. Findings from the current study provide further evidence in support of an independent link between e-cigarette use and internalizing disorders, as well as evidence that dual users have the greatest risk. These data add to the growing body of literature that e-cigarette use may not be a harm-free alternative to smoking.
Another concern of great public health importance associated with cigarette smoking is the increased risk of mental health problems among those with SHS exposure [90]. SHS contains over 4000 chemicals, including toxic compounds like hydrogen cyanide, heavy metals such as lead and chromium, as well as a wide range of organic compounds [91], each entailing a unique profile and mechanism of potential health consequences. SHS exposure has been found to be associated with psychological distress [20], depressive conditions [24, 25, 27, 29,30,31,32,33,34, 92, 93], and panic attacks [22] in studies conducted in the US and around the world. The findings of the current study confirm those of these earlier studies.
No study to date that we are aware of has investigated the relationship between exposure to passive e-cigarette aerosols and adverse mental health outcomes. Akin to cigarette smoke, e-cigarette emissions have been found to include harmful substances like heavy metals (e.g. lead, chromium and nickel) [94,95,96], ultrafine particles [97], and inorganic [98] and volatile organic compounds [97]. Although the concentrations of chemical compounds in e-cigarette emissions have been found to be lower than concentrations of toxicants in SHS, some constituents of e-cigarette emissions are known carcinogens [99, 100]. Furthermore, some e-cigarette devices have even been found to emit metals and nicotine quantities that exceed those of combustible cigarettes [101, 102]. Despite the identification of such toxic constituents, the general public is not well informed of potential acute or long-term risks of secondhand exposure, and the information about untoward exposures and outcomes from secondhand e-cigarette exposure is still under active investigation. In the US, 40% of adults believe secondhand e-cigarette exposure causes “little harm” or only “some harm” and 33% are unsure of the potential dangers [11]. This can be compared to the fact that 64.5% of US adults perceive SHS as “very harmful,” and the fact that dual users report a preference for vaping rather than smoking in the presence of loved ones [103, 104]. Misconceptions about the risks associated with e-cigarette emissions put exposed non-users, including children, at risk. The fact that adult non-users passively exposed to e-cigarette emissions at home or in the workplace were almost 1.5 times more likely to have moderate to severe internalizing problems, warrants further study to determine if in fact this relationship is causal in nature, i.e. that exposure to these emissions actually causes or contributes to an increased burden of mental health problems. Of particular note, these data suggest that the risk of moderate to severe internalizing problems among those passively exposed to e-cigarette emissions is no different from that of those exposed to SHS.
Previous PATH studies demonstrated that internalizing and externalizing problems were associated with the use of cigarettes, e-cigarettes, or their dual use, in both adults and youth [49, 51, 105]. Some of these other studies used different cut-points for internalizing problems and focused on different groups of tobacco product use. We were particularly interested in moderate to severe internalizing problems (GAIN-SS ≥2) as opposed to just those with severe internalizing problems (GAIN-SS =4) based on clinical evidence that even those with moderate internalizing problems benefit from mental health intervention/treatments [47, 48, 50]. Furthermore, consistent with extensive earlier literature, the findings of this study corroborate the independent association of younger age [66], female sex [63], non-Hispanic White race/ethnicity [67], lower annual household income [64], and diagnosis of chronic disease in the past 12 months [106] with internalizing problems.
Limitations of this study should be noted. All analyses were cross-sectional; thus it is impossible to determine the directionality of the association between tobacco product use and exposure and internalizing problems. While it may seem improbable that internalizing disorders lead to secondhand tobacco product exposure, it is possible that people with poor mental health have a higher likelihood of working or living with other individuals who are tobacco product users, and as a result be more likely to experience secondhand emissions themselves. Moreover, non-smoking/non-vaping participants who live and/or work with smokers and/or e-cigarette users may feel a sense of isolation within their homes or the workplace that may ultimately contribute negatively to their mental health. Without knowing the length of time that subjects smoked, vaped, or experienced secondhand exposure; the intensity and frequency or the exact nature of the product used or exposed to; or the length or frequency with which subjects experienced symptoms of mental health problems, it is not possible to know how such differences might have influenced the observed associations. Very limited exposure (i.e., being exposed to a coworker vaping once over a 30 day period), likely did not impact internalizing problems. Moreover, it is possible nicotine specifically plays a critical role in the exacerbation of internalizing problems among those who use and are exposed to tobacco products. However, nicotine content can vary greatly by e-cigarette device type and this was not addressed in the present study [102, 107]. Also, the scale used to assess internalizing mental health problems, GAINS-SS, did not allow us to distinguish among the various internalizing disorders (e.g., depression, anxiety disorder, post-traumatic stress disorder, etc). Additionally, the PATH dataset lacks important information regarding social context, such as the mental health of family members, something known to be associated with an individual’s mental health [108,109,110,111]. Also, secondhand exposure is only defined in the context of occupational and residential exposure and not social settings, which likely contribute to SHS and passive e-cigarette aerosol exposure for many individuals. Furthermore, the utilization of self-reported data for the categorization of tobacco product use/exposure may have been influenced by recall bias. Lastly, this study does not address the mechanisms underlying passive exposure to e-cigarette emissions and increased rates of internalizing mental health problems.
Conclusions
Identifying and understanding potential associations between secondhand e-cigarette emissions and adverse health effects is of vital importance to the health of the public. These findings point to one such potential category of major health difficulties, namely an increased risk of mental health problems. In the case of SHS, smoking ban policies significantly reduce major depression risk among those who have never been smokers [112]. The findings reported in this paper indicate the marked need for further investigation of the safety profile of e-cigarette emission exposure, and whether smoking ban policies should extend to cover e-cigarettes, particularly in environments where vulnerable populations, including children, pregnant women, and those with chronic health conditions are likely to be exposed.
Availability of data and materials
The dataset supporting the conclusions of this article is available in the Population Assessment of Tobacco and Health (PATH) study public-use files (ICPSR 36498), https://doi.org/10.3886/ICPSR36231.v28.
Abbreviations
- SHS:
-
Secondhand smoke
- PATH:
-
The Population Assessment of Tobacco and Health Study
- GAIN-SS:
-
Global Appraisal of Individual Needs-Short Screener
- AORs:
-
Adjusted odds ratios
- CI:
-
Confidence intervals
- BMI:
-
Body mass index
References
National Center for chronic disease prevention, health promotion office on smoking and health. The health consequences of smoking—50 years of Progress: a report of the surgeon general. Atlanta: Centers for Disease Control and Prevention (US); 2014.
Levy DT, Warner KE, Cummings KM, et al. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tob Control. 2019;28(6):629. https://doi.org/10.1136/tobaccocontrol-2018-054446.
National Center for Chronic Disease Prevention, Health Promotion Office on Smoking and Health. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US). 2016. https://e-cigarettes.surgeongeneral.gov/documents/2016_sgr_full_report_non-508.pdf. Accessed 17 July 2021.
Centers for Disease Control and Prevention. Youth e-cigarette use is down, but 3.6 million still use e-cigarettes. U.S. Department of Health & Human Services. 2020. https://www.cdc.gov/media/releases/2020/p0909-youth-e-cigarette-use-down.html. Accessed 27 October 2021.
National Institute on Drug Abuse. What are electronic cigarettes? 2020. https://www.drugabuse.gov/publications/research-reports/tobacco-nicotine-e-cigarettes/what-are-electronic-cigarettes. Accessed 17 July 2021.
Richardson S, McNeill A, Brose LS. Smoking and quitting behaviours by mental health conditions in Great Britain (1993-2014). Addict Behav. 2019;90:14–9. https://doi.org/10.1016/j.addbeh.2018.10.011.
Grabovac I, Oberndorfer M, Fischer J, et al. Effectiveness of electronic cigarettes in smoking cessation: a systematic review and Meta-analysis. Nicotine Tob Res. 2021;23(4):625–34. https://doi.org/10.1093/ntr/ntaa181.
Cornelius ME, Wang TW, Jamal A, et al. Tobacco product use among adults - United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(46):1736–42. https://doi.org/10.15585/mmwr.mm6946a4.
Unger JB, Escobedo P, Allem J-P, Soto DW, Chu K-H, Cruz T. Perceptions of secondhand E-cigarette aerosol among twitter users. Tob Regul Sci. 2016;2(2):146–52. https://doi.org/10.18001/TRS.2.2.5.
McCausland K, Maycock B, Leaver T, et al. E-cigarette promotion on twitter in Australia: content analysis of tweets. JMIR Public Health Surveill. 2020;6(4):e15577. https://doi.org/10.2196/15577.
Nguyen KH, Tong VT, Marynak K, et al. Perceptions of harm to children exposed to secondhand aerosol from electronic vapor products, styles survey, 2015. Prev Chronic Dis. 2017;14:E41. https://doi.org/10.5888/pcd14.160567.
Kovacs M, Devlin B. Internalizing disorders in childhood. J Child Psychol Psychiatry Allied Discip. 1998;39(1):47–63. https://doi.org/10.1111/1469-7610.00303.
Regier DA, Kuhl EA, Kupfer DJ. The DSM-5: classification and criteria changes. World Psychiatry. 2013;12(2):92–8. https://doi.org/10.1002/wps.20050.
Hasin DS, Sarvet AL, Meyers JL, et al. Epidemiology of adult DSM-5 major depressive disorder and its Specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–46. https://doi.org/10.1001/jamapsychiatry.2017.4602.
Yu B, Zhang X, Wang C, et al. Trends in depression among adults in the United States, NHANES 2005-2016. J Affect Disord. 2020;263:609–20. https://doi.org/10.1016/j.jad.2019.11.036.
Institute for Health Metrics and Evaluation (IHME). Global burden of disease study (GBD) results tool. Seattle: IHME, University of Washington; 2015. http://ghdx.healthdata.org/gbd-results-tool. Accessed 26 October 2021
Smith PH, Chhipa M, Bystrik J, et al. Cigarette smoking among those with mental disorders in the US population: 2012-2013 update. Tob Control. 2020;29(1):29–35. https://doi.org/10.1136/tobaccocontrol-2018-054268.
Smith PH, Mazure CM, McKee SA. Smoking and mental illness in the U.S. population. Tob Control. 2014;23(e2):e147–53. https://doi.org/10.1136/tobaccocontrol-2013-051466.
Lasser K, Boyd JW, Woolhandler S, et al. Smoking and mental IllnessA population-based prevalence study. JAMA. 2000;284(20):2606–10. https://doi.org/10.1001/jama.284.20.2606.
Hamer M, Stamatakis E, Batty GD. Objectively assessed secondhand smoke exposure and mental health in adults: cross-sectional and prospective evidence from the Scottish health survey. Arch Gen Psychiatry. 2010;67(8):850–5.
Bandiera FC, Richardson AK, Lee DJ, He JP, Merikangas KR. Secondhand smoke exposure and mental health among children and adolescents. Arch Pediatr Adolesc Med. 2011;165(4):332–8. https://doi.org/10.1001/archpediatrics.2011.30.
Taha F, Goodwin RD. Secondhand smoke exposure across the life course and the risk of adult-onset depression and anxiety disorder. J Affect Disord. 2014;168:367–72. https://doi.org/10.1016/j.jad.2014.07.014.
Kim SY. Secondhand smoke exposure, depression symptoms, and suicidal ideation in adults. Korean J Fam Med. 2016;37(2):77. https://doi.org/10.4082/kjfm.2016.37.2.77.
Kim SJ, Lamichhane DK, Park SG, et al. Association between second-hand smoke and psychological well-being amongst non-smoking wageworkers in Republic of Korea. Ann Occup Environ Med. 2016;28:49. https://doi.org/10.1186/s40557-016-0130-3.
Kim NH, Park JH, Choi DP, et al. Secondhand smoke exposure and depressive symptoms among Korean adolescents: JS high school study. PLoS One. 2016;11(12):e0168754. https://doi.org/10.1371/journal.pone.0168754.
Kim NH, Choi H, Kim NR, et al. Secondhand smoke exposure and mental health problems in Korean adults. Epidemiol Health. 2016;38:e2016009. https://doi.org/10.4178/epih.e2016009.
Gim W, Yoo JH, Shin JY, et al. Relationship between secondhand smoking with depressive symptom and suicidal ideation in Korean non-smoker adults: the Korean National Health and nutrition examination survey 2010-2012. Korean J Fam Med. 2016;37(2):97–104. https://doi.org/10.4082/kjfm.2016.37.2.97 10.1001/archpediatrics.2010.243.
Kim B, Kim HR. Associations between secondhand smoke and mental health in Korean adolescents. Asia Pac J Public Health. 2020;32(8):406–13. https://doi.org/10.1177/1010539520957846.
Asbridge M, Ralph K, Stewart S. Private space second-hand smoke exposure and the mental health of non-smokers: a cross-sectional analysis of Canadian adults. Addict Behav. 2013;38(3):1679–86. https://doi.org/10.1016/j.addbeh.2012.10.008.
Erdsiek F, Brzoska P. Is exposure to secondhand smoke associated with current depression (PHQ-8) among never-smokers? Results from a survey among German adults. BMC Public Health. 2020;20(1):1880. https://doi.org/10.1186/s12889-020-09970-1.
Noguchi T, Nakagawa-Senda H, Tamai Y, et al. Association between second-hand smoke exposure and depressive symptoms among Japanese adults: a cross-sectional study. J Epidemiol. 2020;30(12):566–73. https://doi.org/10.2188/jea.JE20190146.
Nakata A, Takahashi M, Ikeda T, et al. Active and passive smoking and depression among Japanese workers. Prev Med. 2008;46(5):451–6. https://doi.org/10.1016/j.ypmed.2008.01.024.
Ye X, Li L, Gao Y, et al. Dose-response relations between second-hand smoke exposure and depressive symptoms among middle-aged women. Psychiatry Res. 2015;229(1–2):533–8. https://doi.org/10.1016/j.psychres.2015.06.008.
Ye X, Huang J, Xia L, et al. Setting-specific and symptom-specific association between secondhand smoke exposure and depressive symptoms. Int J Environ Res Public Health. 2019;16(7). https://doi.org/10.3390/ijerph16071249.
Saeed OB, Chavan B, Haile ZT. Association between E-cigarette use and depression in US adults. J Addict Med. 2020;14(5):393–400. https://doi.org/10.1097/ADM.0000000000000604.
Pergadia ML, Newcomer JW, Gilbert DG. Depression and nicotine withdrawal associations with combustible and electronic cigarette use. Int J Environ Res Public Health. 2020;17(24). https://doi.org/10.3390/ijerph17249334.
Lee S, Oh Y, Kim H, et al. Implications of electronic cigarette use for depressive mood: a nationwide cross-sectional study. Medicine (Baltimore). 2020;99(40):e22514. https://doi.org/10.1097/MD.0000000000022514.
Wiernik E, Airagnes G, Lequy E, et al. Electronic cigarette use is associated with depressive symptoms among smokers and former smokers: cross-sectional and longitudinal findings from the Constances cohort. Addict Behav. 2019;90:85–91. https://doi.org/10.1016/j.addbeh.2018.10.021.
Obisesan OH, Mirbolouk M, Osei AD, et al. Association between e-cigarette use and depression in the behavioral risk factor surveillance system, 2016-2017. JAMA Netw Open. 2019;2(12):e1916800. https://doi.org/10.1001/jamanetworkopen.2019.16800.
Spears CA, Jones DM, Weaver SR, et al. Use of electronic nicotine delivery systems among adults with mental health conditions, 2015. Int J Environ Res Public Health. 2016;14(1):23. https://doi.org/10.3390/ijerph14010010.
King JL, Reboussin BA, Spangler J, et al. Tobacco product use and mental health status among young adults. Addict Behav. 2018;77:67–72. https://doi.org/10.1016/j.addbeh.2017.09.012.
Bianco CL. Rates of electronic cigarette use among adults with a chronic mental illness. Addict Behav. 2019;89:1–4. https://doi.org/10.1016/j.addbeh.2018.08.033.
Versella MV, Borges AM, Lin C, et al. Co-use of electronic nicotine delivery systems and combustible cigarettes, and their association with internalizing pathology and vulnerabilities. Cognit Ther Res. 2019;43(1):114–20. https://doi.org/10.1007/s10608-018-9971-0.
Pham T, Williams JVA, Bhattarai A, et al. Electronic cigarette use and mental health: a Canadian population-based study. J Affect Disord. 2020;260:646–52. https://doi.org/10.1016/j.jad.2019.09.026.
Wamamili B, Wallace-Bell M, Richardson A, Grace RC, Coope P. Associations of history of mental illness with smoking and vaping among university students aged 18-24 years in New Zealand: results of a 2018 national cross-sectional survey. Addict Behav. 2021;112:106635. https://doi.org/10.1016/j.addbeh.2020.106635.
United States Department of Health Human Services, National Institutes of Health, National Institute on Drug Abuse, food drug Administration Center for Tobacco Products. Population assessment of tobacco and health (PATH) study [United States] public-use files. Inter-university consortium for political and social Research. 2020. https://doi.org/10.3886/ICPSR36231.v28.
Dennis ML, Chan YF, Funk RR. Development and validation of the GAIN short screener (GSS) for internalizing, externalizing and substance use disorders and crime/violence problems among adolescents and adults. Am J Addict. 2006;15(Suppl 1):80–91. https://doi.org/10.1080/10550490601006055.
Dennis ML, Feeney T, Stevens LH, et al. Global Appraisal of Individual Needs–Short Screener (GAIN-SS): Administration and Scoring Manual for the GAIN-SS Version 2.0.1. Bloomington: Chestnut Health Systems; 2006. https://portal.ct.gov/-/media/dcf/GAIN/pdf/GAINSSManual122006pdf.pdf?la=en
Conway KP, Green VR, Kasza KA, et al. Co-occurrence of tobacco product use, substance use, and mental health problems among youth: findings from wave 1 (2013-2014) of the population assessment of tobacco and health (PATH) study. Addict Behav. 2018;76:208–17. https://doi.org/10.1016/j.addbeh.2017.08.009.
Da Silva MA, Gonzalez JC, Person GL, et al. Bidirectional association between bullying perpetration and internalizing problems among youth. J Adolesc Health. 2020;66(3):315–22. https://doi.org/10.1016/j.jadohealth.2019.09.022.
Conway KP, Green VR, Kasza KA, et al. Co-occurrence of tobacco product use, substance use, and mental health problems among adults: findings from wave 1 (2013-2014) of the population assessment of tobacco and health (PATH) study. Drug Alcohol Depend. 2017;177:104–11. https://doi.org/10.1016/j.drugalcdep.2017.03.032.
Riehm KE, Young AS, Feder KA, et al. Mental health problems and initiation of E-cigarette and combustible cigarette use. Pediatrics. 2019;144(1). https://doi.org/10.1542/peds.2018-2935.
World Health Organization Consultation on Obesity (1999: Geneva, Switzerland) & World Health Organization. Obesity: preventing and managing the global epidemic. Geneva: Report of a WHO consultation; 2000. p. 894:i-253. https://pubmed.ncbi.nlm.nih.gov/11234459/.
Li H, Ge S, Greene B, et al. Depression in the context of chronic diseases in the United States and China. Int J Nurs Sci. 2019;6(1):117–22. https://doi.org/10.1016/j.ijnss.2018.11.007.
McCarthy PJ. Pseudoreplication: Further evaluation and applications of the balanced half-sample technique. Vital Health Stat 2. 1969;31:1–24 PMID: 5306564.
Mathew AR, Hogarth L, Leventhal AM, et al. Cigarette smoking and depression comorbidity: systematic review and proposed theoretical model. Addiction. 2017;112(3):401–12. https://doi.org/10.1111/add.13604.
Farrell M, Howes S, Taylor C, et al. Substance misuse and psychiatric comorbidity: an overview of the opcs national psychiatric morbidity survey. Addict Behav. 1998;23(6):909–18. https://doi.org/10.1016/s0306-4603(98)00075-6.
Grant BF, Hasin DS, Chou SP, et al. Nicotine dependence and psychiatric disorders in the United States: results from the National Epidemiologic Survey on alcohol and RelatedConditions. Arch Gen Psychiatry. 2004;61(11):1107–15. https://doi.org/10.1001/archpsyc.61.11.1107.
Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on alcohol and RelatedConditions. Arch Gen Psychiatry. 2004;61(8):807–16. https://doi.org/10.1001/archpsyc.61.8.807.
Morrell HER, Cohen LM. Cigarette smoking, anxiety, and depression. J Psychopathol Behav Assess. 2006;28(4):281–95. https://doi.org/10.1037/bul0000003.
Leventhal AM, Strong DR, Sussman S, et al. Psychiatric comorbidity in adolescent electronic and conventional cigarette use. J Psychiatr Res. 2016;73:71–8. https://doi.org/10.1016/j.jpsychires.2015.11.008.
Cummins SE, Zhu SH, Tedeschi GJ, et al. Use of e-cigarettes by individuals with mental health conditions. Tob Control. 2014;23 Suppl 3(Suppl 3):iii48–53. https://doi.org/10.1136/tobaccocontrol-2013-051511.
Cyranowski JM, Frank E, Young E, et al. Adolescent onset of the gender difference in lifetime rates of major depression: a theoretical model. Arch Gen Psychiatry. 2000;57(1):21–7. https://doi.org/10.1001/archpsyc.57.1.21.
Ridley M, Rao G, Schilbach F, et al. Poverty, depression, and anxiety: causal evidence and mechanisms. Science. 2020;370(6522). https://doi.org/10.1126/science.aay0214.
de Wit LM, van Straten A, van Herten M, et al. Depression and body mass index, a u-shaped association. BMC Public Health. 2009;9(1):14. https://doi.org/10.1186/1471-2458-9-14.
van Loo HM, Beijers L, Wieling M, et al. Prevalence of internalizing disorders, symptoms, and traits across age using advanced nonlinear models. Psychol Med. 2021;1-10. https://doi.org/10.1017/S0033291721001148.
Breslau J, Aguilar-Gaxiola S, Kendler KS, et al. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychol Med. 2006;36(1):57–68. https://doi.org/10.1017/S0033291705006161.
Luger TM, Suls J, Vander Weg MW. How robust is the association between smoking and depression in adults? A meta-analysis using linear mixed-effects models. Addict Behav. 2014;39(10):1418–29. https://doi.org/10.1016/j.addbeh.2014.05.011.
Morissette SB, Tull MT, Gulliver SB, et al. Anxiety, anxiety disorders, tobacco use, and nicotine: a critical review of interrelationships. Psychol Bull. 2007;133(2):245–72. https://doi.org/10.1037/0033-2909.133.2.245.
Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harvard Rev Psychiatry. 1997;4(5):231–44. https://doi.org/10.3109/10673229709030550.
Gehricke JG, Loughlin SE, Whalen CK, et al. Smoking to self-medicate attentional and emotional dysfunctions. Nicotine Tob Res. 2007;9(Suppl 4):S523–36. https://doi.org/10.1080/14622200701685039.
Cosci F, Knuts IJ, Abrams K, et al. Cigarette smoking and panic: a critical review of the literature. J Clin Psychiatry. 2010;71(5):606–15. https://doi.org/10.4088/JCP.08r04523blu.
Hockenberry JM, Timmons EJ, Weg MW. Adolescent mental health as a risk factor for adolescent smoking onset. Adolesc Health Med Ther. 2011;2:27–35. https://doi.org/10.2147/AHMT.S11573.
Breslau N, Novak SP, Kessler RC. Daily smoking and the subsequent onset of psychiatric disorders. Psychol Med. 2004;34(2):323–33. https://doi.org/10.1017/s0033291703008869.
Goodman E, Capitman J. Depressive symptoms and cigarette smoking among teens. Pediatrics. 2000;106(4):748–55. https://doi.org/10.1542/peds.106.4.748.
Steuber TL, Danner F. Adolescent smoking and depression: which comes first? Addict Behav. 2006;31(1):133–6. https://doi.org/10.1016/j.addbeh.2005.04.010.
Zimmermann M, Chong AK, Vechiu C, et al. Modifiable risk and protective factors for anxiety disorders among adults: a systematic review. Psychiatry Res. 2020;285:112705. https://doi.org/10.1016/j.psychres.2019.112705.
Breslau N, Peterson EL, Schultz LR, et al. Major depression and stages of smoking: a longitudinal investigation. Arch Gen Psychiatry. 1998;55(2):161–6. https://doi.org/10.1001/archpsyc.55.2.161.
Windle M, Windle RC. Depressive symptoms and cigarette smoking among middle adolescents: prospective associations and intrapersonal and interpersonal influences. J Consult Clin Psychol. 2001;69(2):215–26 PMID: 11393599.
Moylan S, Jacka FN, Pasco JA, et al. Cigarette smoking, nicotine dependence and anxiety disorders: a systematic review of population-based, epidemiological studies. BMC Med. 2012;10:123. https://doi.org/10.1186/1741-7015-10-123.
Park SH, Lee L, Shearston JA, et al. Patterns of electronic cigarette use and level of psychological distress. PLoS One. 2017;12(3):e0173625. https://doi.org/10.1371/journal.pone.0173625.
Marsden DG, Loukas A, Chen B, et al. Associations between frequency of cigarette and alternative tobacco product use and depressive symptoms: a longitudinal study of young adults. Addict Behav. 2019;99:106078. https://doi.org/10.1016/j.addbeh.2019.106078.
Lee Y, Lee KS. Association of depression and Suicidality with electronic and conventional cigarette use in south Korean adolescents. Subst Use Misuse. 2019;54(6):934–43. https://doi.org/10.1080/10826084.2018.1552301.
Chadi N, Li G, Cerda N, et al. Depressive symptoms and Suicidality in adolescents using e-cigarettes and marijuana: a secondary data analysis from the youth risk behavior survey. J Addict Med. 2019;13(5):362–5. https://doi.org/10.1097/ADM.0000000000000506.
Bandiera FC, Loukas A, Wilkinson AV, et al. Associations between tobacco and nicotine product use and depressive symptoms among college students in Texas. Addict Behav. 2016;63:19–22. https://doi.org/10.1016/j.addbeh.2016.06.024.
Chou SP, Saha TD, Zhang H, et al. Prevalence, correlates, comorbidity and treatment of electronic nicotine delivery system use in the United States. Drug Alcohol Depend. 2017;178:296–301. https://doi.org/10.1016/j.drugalcdep.2017.05.026.
Becker TD, Arnold MK, Ro V, et al. Systematic review of electronic cigarette use (Vaping) and mental health comorbidity among adolescents and Young adults. Nicotine Tob Res. 2021;23(3):415–25. https://doi.org/10.1093/ntr/ntaa171.
Okunna N. A comparison of mental and behavioral health risks factors associated with current dual use of electronic cigarette and conventional tobacco cigarettes with exclusive tobacco cigarette use and nonuse among adults in the United States. Am J Addict. 2021;30(2):138–46. https://doi.org/10.1111/ajad.13110.
Chen YL, Wu SC, Chen YT, et al. E-cigarette use in a country with prevalent tobacco smoking: a population-based study in Taiwan. J Epidemiol. 2019;29(4):155–63. https://doi.org/10.2188/jea.JE20170300.
National Center for chronic disease prevention, health promotion office on smoking and health. The health consequences of involuntary exposure to tobacco smoke: a report of the surgeon general. Atlanta: Centers for Disease Control and Prevention (US); 2006. PMID: 20669524
Zhou S, Rosenthal DG, Sherman S, et al. Physical, behavioral, and cognitive effects of prenatal tobacco and postnatal secondhand smoke exposure. Curr Probl Pediatr Adolesc Health Care. 2014;44(8):219–41. https://doi.org/10.1016/j.cppeds.2014.03.007.
Jung SJ, Shin A, Kang D. Active smoking and exposure to secondhand smoke and their relationship to depressive symptoms in the Korea national health and nutrition examination survey (KNHANES). BMC Public Health. 2015;15:1053. https://doi.org/10.1186/s12889-015-2402-1.
Kim NH, Kim HC, Lee JY, et al. Association between environmental tobacco smoke and depression among Korean women. BMJ Open. 2015;5(6):e007131. https://doi.org/10.1136/bmjopen-2014-007131.
Pappas RS, Gray N, Halstead M, et al. Toxic metal-containing particles in aerosols from pod-type electronic cigarettes. J Anal Toxicol. 2021;45(4):337–47. https://doi.org/10.1093/jat/bkaa088.
Ting CY, Ahmad Sabri NA, Tiong LL, et al. Heavy metals (Cr, Pb, cd, Ni) in aerosols emitted from electronic cigarettes sold in Malaysia. J Environ Sci Health Part A Tox Hazard Subst Environ Eng. 2020;55(1):55–62. https://doi.org/10.1080/10934529.2019.1665950.
Halstead M, Gray N, Gonzalez-Jimenez N, et al. Analysis of toxic metals in electronic cigarette aerosols using a novel trap design. J Anal Toxicol. 2020;44(2):149–55. https://doi.org/10.1093/jat/bkz078.
Talih S, Salman R, Soule E, et al. Electrical features, liquid composition and toxicant emissions from ‘pod-mod’-like disposable electronic cigarettes. Tob Control. 2021. https://doi.org/10.1136/tobaccocontrol-2020-056362.
Liu Q, Huang C, Chris LX. Arsenic species in electronic cigarettes: determination and potential health risk. J Environ Sci (China). 2020;91:168–76. https://doi.org/10.1016/j.jes.2020.01.023.
Li L, Yan L, Tian X, et al. Effects of electronic cigarettes on indoor air quality and health. Annu Rev Public Health. 2020;40(1):363–80. https://doi.org/10.1146/annurev-publhealth-040119-094043.
National Academies of Sciences, Engineering, and Medicine. Public health consequences of E-cigarettes. Washington, DC: The National Academies Press; 2018. https://doi.org/10.17226/24952.
EL-Hellani A, Salman R, El-Hage R, et al. Nicotine and carbonyl emissions from popular electronic cigarette products: correlation to liquid composition and design characteristics. Nicotine Tob Res. 2018;20(2):215–23. https://doi.org/10.1093/ntr/ntw280.
Williams M, Villarreal A, Bozhilov K, Lin S, Talbot P. Metal and silicate particles including nanoparticles are present in electronic cigarette cartomizer fluid and aerosol. PLoS One. 2013. https://doi.org/10.1371/journal.pone.0057987.
Kruger J, Patel R, Kegler M, Babb SD, King BA. Perceptions of harm from secondhand smoke exposure among U.S. adults, 2009-2010. Tob Induc Dis. 2016;14:3 Published 2016 Feb 2. https://doi.org/10.1186/s12971-016-0069-8.
Adriaens K, Van Gucht D, Baeyens F. Differences between dual users and switchers center around Vaping behavior and its experiences rather than beliefs and attitudes. Int J Environ Res Public Health. 2018;15(1):12. https://doi.org/10.3390/ijerph15010012.
Kaplan B, Thrul J, Cohen JE. Association of cigarette and electronic nicotine delivery systems use with internalizing and externalizing problems among US adults: findings from wave 3 (2015–2016) of the PATH study. PLoS One. 2021;16(6):e0253061. https://doi.org/10.1371/journal.pone.0253061.
Li H, Ge S, Greene B, Dunbar-Jacob J. Depression in the context of chronic diseases in the United States and China. Int J Nurs Sci. 2018;6(1):117–22. Published 2018 Nov 29. https://doi.org/10.1016/j.ijnss.2018.11.007.
Taylor A, Dunn K, Turfus S. A review of nicotine-containing electronic cigarettes—trends in use, effects, contents, labelling accuracy and detection methods. Drug Test Anal. 2021;13:242–60. https://doi.org/10.1002/dta.2998.
Gotlib IH, Joormann J, Foland-Ross LC. Understanding familial risk for depression: a 25-year perspective. Perspect Psychol Sci. 2014;9(1):94–108. https://doi.org/10.1177/1745691613513469.
Weitzman M, Rosenthal DG, Liu YH. Paternal depressive symptoms and child behavioral or emotional problems in the United States. Pediatrics. 2011;128(6):1126–34. https://doi.org/10.1542/peds.2010-3034.
Tseng KK, Park SH, Shearston JA, Lee L, Weitzman M. Parental psychological distress and family food insecurity: sad dads in hungry homes. J Dev Behav Pediatr. 2017. https://doi.org/10.1097/DBP.0000000000000481.
Amrock S, Weitzman M. Parental psychological distress and Children’s mental health: results of a National Survey. Acad Pediatr. 2014;14:375–81.
Bandiera FC, Caban-Martinez AJ, Arheart KL, et al. Secondhand smoke policy and the risk of depression. Ann Behav Med. 2010;39(2):198–203. https://doi.org/10.1007/s12160-010-9174-8.
Funding
This work was supported, in part, by NIH/NIEHS 1R21ES026996-01A1, NIH/NIEHS 1R01HL139239–01, and NIEHS T32ES007324.
Author information
Authors and Affiliations
Contributions
Authors KRF, MW, EK, TG, and SX conceptualized the project. Author TL conducted literature searches and provided summaries of previous research studies and contributed to the Introduction and Discussion sections. Author SX conducted the statistical analyses and validated results. Author KRF prepared tables and figures. Authors MW, TG, and SX supervised this project. Author KRF wrote the first draft of the manuscript and all authors (KRF, MW, EK, TL, TG, and SX) contributed to and have approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The NYU School of Medicine Office of Science and Research Institutional Review Board determined this secondary analysis of PATH data did not involve human subjects and therefore no IRB review and approval was required.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Crude and Adjusted† Odds Ratios for Moderate to Severe Internalizing Problems.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Farrell, K.R., Weitzman, M., Karey, E. et al. Passive exposure to e-cigarette emissions is associated with worsened mental health. BMC Public Health 22, 1138 (2022). https://doi.org/10.1186/s12889-022-13470-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13470-9