Abstract
Background
In low-resource settings, the awareness level of colorectal cancer (CRC) signs and symptoms plays a crucial role in early detection and treatment. This study examined the public awareness level of CRC signs and symptoms in Palestine and investigated the factors associated with good awareness.
Methods
This was a national cross-sectional study conducted at hospitals, primary healthcare centers, and public spaces in 11 governorates across Palestine between July 2019 and March 2020. A translated-into-Arabic version of the validated bowel cancer awareness measure (BoCAM) was utilized to assess the awareness level of CRC signs and symptoms. For each correctly identified CRC sign/symptom, one point was given. The total score (ranging from 0 to 12) was calculated and categorized into three categories based on the number of symptoms recognized: poor (0 to 4), fair (5 to 8), and good awareness (9 to 12).
Results
Of 5254 approached, 4877 participants completed the questionnaire (response rate = 92.3%). A total of 4623 questionnaires were included in the analysis; 1923 were from the Gaza Strip and 2700 from the West Bank and Jerusalem (WBJ). Participants from the Gaza Strip were younger, gained lower monthly income, and had less chronic diseases than participants in the WBJ.
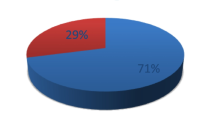
The most frequently identified CRC sign/symptom was ‘lump in the abdomen’ while the least was ‘pain in the back passage’. Only 1849 participants (40.0%, 95% CI: 39.0%-41.0%) had a good awareness level of CRC signs/symptoms. Participants living in the WBJ were more likely to have good awareness than participants living in the Gaza Strip (42.2% vs. 37.0%; p = 0.002). Knowing someone with cancer (OR = 1.37, 95% CI: 1.21–1.55; p < 0.001) and visiting hospitals (OR = 1.46, 95% CI: 1.25–1.70; p < 0.001) were both associated with higher likelihood of having good awareness. However, male gender (OR = 0.80, 95% CI: 0.68–0.94; p = 0.006) and following a vegetarian diet (OR = 0.59, 95% CI: 0.48–0.73; p < 0.001) were both associated with lower likelihood of having good awareness.
Conclusion
Less than half of the study participants had a good awareness level of CRC signs and symptoms. Future education interventions are needed to improve public awareness of CRC in Palestine.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the third most common cancer and the second common cause of cancer-related mortality globally with 1,931,590 new cases and 935,173 deaths in 2020 [1]. In Palestine, CRC is the second most common cancer in both males and females with incidence rates of 15.2 per 100,000 general population in the West Bank and Jerusalem (WBJ) and 11.5 per 100,000 general population in the Gaza Strip [2, 3]. In 2020, cancer was the third most common cause of mortality in Palestine constituting 14.1% of total reported deaths. CRC was the second highest cause of death among all cancers making up 13.9% of all cancer-related deaths in Palestine [4].
The global burden of cancer is predicted to rise by 47.0% in 2040 compared to 2020 [5]. This is anticipated to affect low- and middle-income countries (LMICs), like Palestine, to a significantly greater extent than high-income countries (HICs) with predicted increases of 64.0% to 95.0% and 32.0% to 56.0% respectively [5]. Simultaneously, the associated mortality is predicted to rise in LMICs significantly, while cancer-associated mortality in HICs is predicted to follow its current trend of remaining stable or decreasing [6]. An estimate of 75.0% of the global cancer mortality is predicted to occur in LMICs by 2030 [7]. Factors contributing to these disparate trends are many, including lack of screening programs in LMICs, poorer risk factor control, improved cancer therapies in HICs, lack of educational resources in LMICs and prolonged times to diagnosis in LMICs [8, 9]. In Palestine, too, no screening program exists for CRC, access to treatment is often difficult and cancer-related mortality is high and often judged avoidable [10, 11]. In order to improve outcomes from cancer treatment, the interval from first signs and symptoms to diagnosis has to be shortened.
Signs and symptoms like abdominal and rectal masses, iron deficiency anemia, rectal bleeding, and change in bowel habits could be suggestive of CRC [12]. Good recognition of these signs and symptoms may facilitate early presentation, which increases the chances of patients to be diagnosed in early stages and have higher survival rates [13,14,15].
A previous study conducted in the Gaza Strip showed poor awareness of CRC signs and symptoms; highlighting the need to explore the level of national awareness about CRC in Palestine [16]. This is especially important given that there is no established screening program for CRC in Palestine [17]. High awareness of CRC signs and symptoms may enhance early diagnosis, which could potentially reduce the socioeconomic and health burden of CRC in Palestine.
This national study aimed to: (i) evaluate the Palestinians’ awareness level of CRC signs and symptoms, (ii) compare CRC awareness in the two main areas of Palestine; the Gaza Strip vs. the WBJ, and (iii) explore the factors associated with good awareness of CRC signs and symptoms.
Materials and methods
Study design and population
This was a national cross-sectional study. It was conducted from the 16th of July 2019 to the 31st of March 2020. The target population was adult Palestinians living in the Gaza Strip or the WBJ. Palestine consists of 16 governorates: five located in the Gaza Strip, and 11 in the WBJ. Participants were recruited from 11 governorates from all over Palestine: four in the Gaza Strip, and seven in the WBJ [18].
Sampling methods and data collection
The Palestinian Ministry of Health (MoH) has 11 general hospitals with a bed capacity of ≥ 100: six in the West Bank and five in the Gaza Strip [17]. There is no MoH hospital in Jerusalem. However, there are two hospitals with a bed capacity of ≥ 100 owned by non-governmental organizations. There are 26 MoH PHCs that provide all primary healthcare services (i.e., classified as level four): 17 are in the WBJ and nine in the Gaza Strip [17]. Public spaces at the governorates of the corresponding hospitals and PHCs were also targeted. Those included markets, mosques, churches, public transportations, neighborhoods, malls, gardens, and others. Stratified convenience sampling was used to recruit study participants in concordance with previous studies [16, 19,20,21,22,23,24]. Potential participants could be either visitors in waiting rooms at hospitals and PHCs or visitors to public spaces in 11 out of 16 governorates of Palestine (four in the Gaza Strip and seven in the WBJ). Data were collected on a daily basis by the team of authors who were all working or studying in a health-related field and had been trained on how to approach potential participants, explain the purpose of the study and gain informed consent. Participants were invited to complete the questionnaire in face-to-face interviews at the time of recruitment. Data were collected utilizing ‘Kobo Toolbox’, a secure, user-friendly data collection tool that can be accessed via smartphones [25]. The average time to complete the questionnaire was about seven minutes.
Inclusion and exclusion criteria
Inclusion criteria included being an adult Palestinian (≥ 18 years), being a visitor in one of the data collection sites as well as the ability and willingness to provide an informed consent to participate in the study. Exclusion Criteria included being a visitor to the oncology departments, working or studying in the medical field, holding a nationality other than Palestinian, and being unable to complete the questionnaire.
Questionnaire
Data were collected utilizing a modified and translated-into-Arabic version of the Bowel Cancer Awareness Measure (BoCAM) [26]. The questionnaire was translated from English to Arabic for the purpose of this study and then was back translated into English. Each step was done by two different bilingual healthcare professionals with expertise in clinical research and survey design, some of whom were part of the research team, others were researchers at local universities. To ensure content validity, the questionnaire was then reviewed by five independent experts in the fields of gastroenterology, coloproctology, and public health. This was followed by conducting a pilot study (n = 25) to assess the clarity of the questions in the Arabic BoCAM. The questionnaires of the pilot study were not included in the final analysis. Finally, internal consistency was evaluated using Cronbach’s Alpha, which reached an acceptable value (α = 0.887).
The questionnaire consisted of two sections. The first section included socio-demographic questions including age group, gender, educational level, occupation, monthly income, place of residency, marital status, having a chronic disease, following a vegetarian diet, knowing someone with cancer, and site of data collection. The second section comprised 12 questions that assessed the recognition of CRC signs and symptoms using a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree). The questions in the original BoCAM with yes/no/unknown responses were modified into 5-point Likert scale questions. This was intended to minimize the possibility of participants answering questions randomly [22, 26, 27]. The signs/symptoms of ‘unexplained generalized fatigue’, ‘unexplained loss of appetite’, and ‘feeling persistently full’ were added to the questionnaire since they were mentioned in other forms of the Cancer Awareness Measure [28,29,30], and it was thought that it would be helpful to include them in the context of CRC.
Outcomes
The primary outcome measure was the level of public awareness about CRC signs and symptoms. Secondary outcomes included the proportion of people recognizing each CRC sign and symptom.
Statistical analysis
The latest recommendation of the American Cancer Society for people at average risk of CRC is to start screening at the age of 45 [31]. Therefore, participants’ age was categorized into two categories using this cutoff: 18–44 years and ≥ 45 years. The monthly income was also categorized into two categories: < 1450 NIS and ≥ 1450 NIS. The cutoff of 1450 NIS (about US$450) was used as it is the minimum wage in Palestine [32].
Continuous variables were described using the median and interquartile range (IQR) as they were non-normally distributed. Categorical variables were described using frequencies and percentages. Baseline characteristics of the participants recruited from the WBJ vs. those recruited from the Gaza Strip were compared using Kruskal–Wallis test if the characteristic was continuous or using Pearson's Chi-square test if it was categorical.
The recognition of each CRC sign/symptom was evaluated using a question based on a 5-point Likert scale with ‘strongly agree’ or ‘agree’ as a correct answer, and ‘strongly disagree’, ‘disagree’, or ‘not sure’ as an incorrect answer. CRC signs/symptoms were further categorized into three categories: (i) signs/symptoms with mass or blood, (ii) signs/symptoms of a non-specific nature, and (iii) other gastrointestinal signs/symptoms. Recognition of CRC signs and symptoms was described using frequencies and percentages with comparisons made by Pearson's Chi-Square test. This was followed by running bivariable and multivariable logistic regression analyses. The model of the multivariable analysis included age group, gender, educational level, occupation, monthly income, place of residency, marital status, having a chronic disease, following a vegetarian diet, knowing someone with cancer, and site of data collection. This model was determined a priori based on previous studies [16, 33,34,35,36,37,38,39]. Results of the bivariable analyses are provided in additional file 1.
To assess the participants’ awareness level of CRC signs and symptoms, a scoring system was used. Similar scoring systems were also used in previous studies [19, 21,22,23,24]. For each correctly recognized CRC sign/symptom, one point was given. The total score (ranging from 0 to 12) was calculated and categorized based on the number of CRC signs and symptoms recognized into three categories: poor (0 to 4), fair (5 to 8), and good awareness (9 to 12). The awareness level of participants recruited from the Gaza Strip was compared with the awareness level of participants recruited from the WBJ using Pearson's Chi-Square test. Bivariable and multivariable logistic regression analyses were also performed to test the association between participant characteristics and having good awareness level.
Complete case analysis was used to handle missing data, which occurred completely at random. Data were analyzed using Stata software version 16.0 (StataCorp, College Station, Texas, United States).
Results
Participant characteristics
Of 5254 approached, 4877 participants completed the questionnaire (response rate = 92.3%).
A total of 4623 questionnaires were included in the analysis and 254 were excluded (44 did not meet the inclusion criteria and 210 had missing data). Of those included, 1923 (41.6%) were from the Gaza Strip and 2700 (58.4%) from the WBJ. The median age (IQR) of all participants was 31.0 years (24.0, 43.0) and 1879 (40.6%) were males (Table 1). Participants from the Gaza Strip were younger, gained lower monthly income, had less chronic diseases, and more frequently followed a vegetarian diet than participants from the WBJ.
Good awareness and its associated factors
A total of 1849 participants (40.0%) demonstrated good awareness of CRC signs and symptoms (Table 2). Participants from the WBJ were more likely than participants from the Gaza Strip to have a good awareness level about CRC symptoms (42.2.0% vs. 37.0%).
On the multivariable analysis, knowing someone with cancer (OR = 1.37, 95% CI: 1.21–1.55; p < 0.001) and visiting hospitals (OR = 1.46, 95% CI: 1.25–1.70; p < 0.001) were both associated with higher likelihood of having good awareness of CRC signs and symptoms (Table 3). However, male gender (OR = 0.80, 95% CI: 0.68–0.94; p = 0.006) and following a vegetarian diet (OR = 0.59, 95% CI: 0.48–0.73; p < 0.001) were associated with a lower likelihood of having good awareness.
Recognition of CRC signs and symptoms
Among all participants, the most frequently identified CRC sign/symptom was ‘lump in the abdomen’ (n = 3421, 74.0%) followed by ‘unexplained weight loss’ (n = 3297, 71.3%) (Table 4). These signs/symptoms were also the most identified in both the Gaza Strip and the WBJ. The least identified signs/symptoms were ‘pain in the back passage’ (n = 2222, 42.1%) and ‘bowel does not completely empty after using the lavatory’ (n = 2404, 52.0%). These signs/symptoms were also the least identified in both the Gaza Strip and the WBJ.
Association between recognizing signs/symptoms with mass or blood and participant characteristics
On the multivariable analysis, participants residing in the WBJ were less likely than participants residing in the Gaza Strip to recognize ‘lump in the abdomen’ (OR = 0.64, 95% CI: 0.53–0.77) and ‘bleeding from back passage’ (OR = 0.70, 95% CI: 0.59–0.82) as CRC signs/symptoms (Supplementary table 1). In addition, participants who suffered from a chronic disease were less likely than participants who did not have a chronic disease to recognize ‘lump in the abdomen’ (OR = 0.82, 95% CI: 0.68–0.98). Moreover, male participants were less likely than female participants to recognize ‘bleeding from back passage’ (OR = 0.73, 95% CI: 0.62–0.86).
On the other hand, vegetarian participants were more likely than non-vegetarian participants to identify ‘lump in the abdomen’ (OR = 1.43, 95% CI: 1.13–1.80) and ‘bleeding from back passage’ (OR = 1.47, 95% CI: 1.21–1.80). Additionally, participants who knew someone with cancer had a higher likelihood than participants who did not to identify ‘lump in the abdomen’ (OR = 1.22, 95% CI: 1.07–1.40). Participants recruited from hospitals were more likely than participants recruited from public spaces to identify ‘blood in the stools’ (OR = 1.20, 95% CI: 1.02–1.41) and ‘bleeding from back passage’ (OR = 1.17, 95% CI: 1.01–1.36).
Association between recognizing signs/symptoms of a non-specific nature and participant characteristics
Vegetarians were less likely than non-vegetarians to recognize all CRC signs and symptoms of a non-specific nature (Supplementary table 2). In addition, male participants were less likely than female participants to recognize three out of four CRC signs and symptoms of a non-specific nature. On the contrary, participants who knew someone with cancer and those recruited from hospitals were more likely to recognize all CRC signs and symptoms of a non-specific nature. Participants aged ≥ 45 years had a higher likelihood than younger participants (18–44 years) to recognize ‘anemia’ (OR = 1.34, 95% CI: 1.12–1.61).
Association between recognizing other gastrointestinal signs/symptoms and participant characteristics
Vegetarians were less likely than non-vegetarians to recognize all other gastrointestinal signs/symptoms except ‘persistent pain in the abdomen’ for which no difference was found (Supplementary table 3). Conversely, participants who knew someone with cancer had a higher likelihood than participants who did not to recognize all other gastrointestinal signs/symptoms. In addition, participants recruited from hospitals were more likely than participants recruited from public spaces to recognize all other gastrointestinal signs/symptoms except ‘pain in the back passage’ for which no difference was found.
Discussion
Good awareness was exhibited by 40.0% of the study participants. Participants from the WBJ had a higher likelihood of having good awareness than participants from the Gaza Strip. Knowing someone with cancer and visiting hospitals were associated with higher odds of having good awareness. In contrast, male gender and following a vegetarian diet were both associated with lower odds of having good awareness. The most frequently identified CRC sign/symptom was ‘lump in the abdomen’ while the least was ‘pain in the back passage’.
Poor awareness of CRC signs and symptoms has been found to be associated with delayed presentation, which may lead to diagnosis at advanced stages [40,41,42]. Therefore, raising and sustaining high awareness of CRC signs and symptoms should be prioritized in future public health actions. This is especially important where no screening programs exist, as in Palestine [12].
In concordance with this study, previous studies reported low levels of CRC awareness in other Arab countries including Lebanon (33% displayed good awareness), Jordan (34.5%), Qatar (40.2%), and United Arab Emirates (< 50.0%) [43,44,45,46]. Conversely, studies in non-Arab countries showed better CRC awareness: the United States of America (91.0% showed good awareness), the United Kingdom (88.0%) Malaysia (70.9%), Turkey (69.0%), and Norway (60.0%) [47,48,49,50,51]. This may reflect poor health education about CRC signs and symptoms in Arab countries and underline the need for establishing continuous educational programs. Another contributing factor could be the shared, misleading cultural beliefs in these countries [52]. A living example of this was noticed during the data collection for this study. Some people thought that God protects them from getting CRC, which could lead to more negligence about the recognition of possible CRC signs/symptoms and late diagnosis.
A previous study in Denmark showed that cancer was perceived as a terminal illness that cannot be treated and screening was only relevant for symptomatic patients [53]. The hopelessness and helplessness people feel towards CRC could be the result of their poor insight—healthcare illiteracy—towards the role of early detection in the morbidity and mortality of the disease [52]. Thus, a multidisciplinary approach should be considered to raise the public awareness about the importance of early detection. This may include creating a curriculum that provides the public with a comprehensive understanding of CRC [53]. Improved awareness following an educational intervention has been shown to improve the ability to recognize and recall the signs and symptoms of cancer for six months after the intervention took place [54]. A previous study in Malaysia showed that individuals exposed to a mass media advertisement campaign for CRC awareness via radio, television, or print format, were more likely to recognize CRC signs and symptoms with more confidence than those who had not been exposed [55]. This could be a component of an efficient strategy in countries with low-resource settings, such as Palestine, where the public can be targeted using mass media, but also an individualized approach like integrating CRC signs and symptoms can be employed in school and university curricula [54,55,56].
Differences in the awareness level between the Gaza Strip vs. the WBJ
In this study, the finding that participants from the WBJ were more likely to have good awareness than participants from the Gaza Strip could be related to several factors. Firstly, the lower availability of healthcare resources in the Gaza Strip might make it more challenging for people to access treating facilities, which may reduce their chance to be exposed to health education activities in these facilities [57]. Secondly, digital access to health education sources (e.g., social media) might be different between the two areas. This is primarily due to the regular power cuts experienced by people living in the Gaza Strip [58]. Finally, there could be a variation in the frequency and location of routine health check-ups and follow-ups in the Gaza Strip vs. the WBJ. The Palestinian MoH reported higher numbers and percentages of visitors to its facilities in the WBJ than in the Gaza Strip [32, 57]. The greater exposure to MoH facilities in the WBJ might have helped the participants living there accumulate more knowledge about health topics including CRC [19,20,21,22]. Additionally, with the higher median income in the WBJ [32], people living there may be more able to visit private healthcare centers. This may further support people living in the WBJ to enrich their health literacy.
Factors associated with good awareness of CRC signs and symptoms
In concordance with previous studies [43, 44], in this study, participants who knew someone with cancer or visited hospitals had an increased likelihood of having good awareness of CRC signs and symptoms compared with those who did not. People exposed to sick relatives and patients are personally more concerned and intimidated by the disease and thus are more likely to seek information about health-related topics including CRC [22]. On the contrary, male gender and following a vegetarian diet were found in this study to be associated with a decrease in the likelihood of displaying good awareness of CRC signs and symptoms. This is in line with previous studies which showed that women were more aware about CRC signs and symptoms overall [16, 21, 37]. It could be that females are more frequently exposed to healthcare professionals than males, due to their maternity care experiences. This is supported with the finding that visiting hospitals was associated with a higher likelihood to have good awareness of CRC signs and symptoms. Furthermore, females more frequently take on the care of sick relatives and, thus, become more familiar with health issues. Participants on a vegetarian diet had a lower likelihood to have a good awareness of CRC signs and symptoms. Vegetarians are usually expected to follow a healthier lifestyle [59], which might drive them to read more about health-related topics including CRC. Interestingly, in this study, vegetarians were less likely to recognize most CRC signs and symptoms. This unexpected finding could be potentially explained by the reason for following a vegetarian diet. While this variable was not captured in this study, there was an association between monthly income and following a vegetarian diet, where participants with a lower wage (< 1450 NIS) were about three times more likely to be on a vegetarian diet (OR = 3.22, 95% CI: 2.64–3.93; data not shown). This suggests that inability to afford meat could be the reason for following a vegetarian diet not the intent to have a healthier lifestyle, which might explain the lower likelihood of vegetarians to recognize most CRC signs and symptoms.
Future directions
The findings of this study underline the substantial need to establish sustainable educational programs that should focus on raising the public awareness of CRC signs and symptoms. Awareness campaigns should be tailored to be appropriate for the specific cultural needs. Improving the awareness of CRC may make the public feel more confident and encourage them to discuss their symptoms with healthcare professionals as soon as they recognize them. This may facilitate early detection and diagnosis of CRC and may improve patient prognosis.
Strengths and limitations
The major strengths of this study included the large sample size from different areas in Palestine, the high response rate, and the use of a translated version of the validated BoCAM. In addition, the face-to-face interviews for data collection minimized the possibility that a participant could use the internet to answer questions correctly. On the other hand, limitations of this study included the use of stratified convenience sampling, which does not guarantee creating a representative sample of the pubic in Palestine. Nonetheless, the large sample size, the high response rate, and the data collection from different geographical areas across Palestine and from various locations (i.e., hospitals, PHCs, and public spaces) may mitigate this. Another limitation is the exclusion of visitors to the oncology departments and participants with medical backgrounds, which could possibly reduce the number of participants with a presumably good awareness of CRC signs and symptoms. However, the exclusion of these participants was intended to increase the relevancy of this study as a measure of the public awareness. Finally, the study included participants who did not experience actual CRC symptoms, but looked at their perceived knowledge.
Conclusions
Only 40.0% of the study participants had good awareness of CRC signs and symptoms. Participants living in the WBJ were more likely to have good awareness than participants living in the Gaza Strip. The most frequently identified CRC symptom was ‘lump in the abdomen’ while the least was ‘pain in the back passage’. Knowing someone with cancer and visiting hospitals were both associated with higher likelihoods of having good awareness. However, male gender and following a vegetarian diet were both associated with lower likelihoods of having good awareness. Future education interventions are needed to improve awareness of CRC signs and symptoms and, thus, may improve early diagnosis and survival of CRC patients in Palestine.
Availability of data and materials
The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.
Change history
18 September 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12889-023-16709-1
Abbreviations
- CRC:
-
Colorectal cancer
- WBJ:
-
West Bank and Jerusalem
- LMICs:
-
Low- and middle-income countries
- HICs:
-
High-income countries
- MoH:
-
Ministry of health
- BoCAM:
-
Bowel cancer awareness measure
- CI:
-
Confidence interval
- OR:
-
Odds ratio
References
International Agency for Research on Cancer. Colorectal Cancer. https://bit.ly/2ZgcdJ5. Accessed 21 April 2022.
The Palestinian Health Information Center. Cancer Incidence in the Gaza Strip Facts & Figures 2015–2016. https://bit.ly/2T3i7eb. Accessed 21 April 2022.
Palestinian Ministry of Health. Annexes to the annual health report of Palestine 2020. https://bit.ly/3ueQrB5. Accessed 21 April 2022.
Palestinian Ministry of Health. Palestine Annual Health Report 2020. https://bit.ly/3AHZYD2. Accessed 21 April 2022.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Thun MJ, DeLancey JO, Center MM, Jemal A, Ward EM. The global burden of cancer: priorities for prevention. Carcinogenesis. 2010;31(1):100–10.
The Lancet GLOBOCAN. counting the toll of cancer. Lancet (London, England). 2018;392(10152):985.
Shah SC, Kayamba V, Peek RM Jr, Heimburger D. Cancer Control in Low- and Middle-Income Countries: Is It Time to Consider Screening? J Glob Oncol. 2019;5:1–8.
Forouzanfar MH, Alexander LT, Anderson HR, Bachman VF, Biryukov S, Brauer R, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287–323.
Jubran J SA, Jarrar K, Hammad S. Pathway to Survival - the Story of Breast Cancer in Palestine 2018. https://bit.ly/2GCvdZs. Accessed 21 April 2022.
Halahleh K, Gale RP. Cancer care in the Palestinian territories. Lancet Oncol. 2018;19(7):e359–64.
Thompson MR, O’Leary DP, Flashman K, Asiimwe A, Ellis BG, Senapati A. Clinical assessment to determine the risk of bowel cancer using Symptoms, Age, Mass and Iron deficiency anaemia (SAMI). Br J Surg. 2017;104(10):1393–404.
Smith D, Ballal M, Hodder R, Soin G, Selvachandran SN, Cade D. Symptomatic presentation of early colorectal cancer. Ann R Coll Surg Engl. 2006;88(2):185–90.
Brenner H, Jansen L, Ulrich A, Chang-Claude J, Hoffmeister M. Survival of patients with symptom- and screening-detected colorectal cancer. Oncotarget. 2016;7(28):44695–704.
Barillari P, de Angelis R, Valabrega S, Indinnimeo M, Gozzo P, Ramacciato G, et al. Relationship of symptom duration and survival in patients with colorectal carcinoma. Eur J Surg Oncol. 1989;15(5):441–5.
Elshami M, Alfaqawi M, Abdalghafoor T, Nemer AA, Ghuneim M, Lubbad H, et al. Public Awareness and Barriers to Seeking Medical Advice for Colorectal Cancer in the Gaza Strip: A Cross-Sectional Study. J Glob Oncol. 2019;5:JGO1800252-JGO.
Qumseya BJ, Tayem YI, Dasa OY, Nahhal KW, Abu-Limon IM, Hmidat AM, et al. Barriers to colorectal cancer screening in Palestine: a national study in a medically underserved population. Clin Gastroenterol Hepatol. 2014;12(3):463–9.
European Council on Foreign Relations. Mapping Palestinian Politics. https://bit.ly/3kEmO9c. Accessed 21 April 2022.
Elshami M, Bottcher B, Alkhatib M, Ismail I, Abu-Nemer K, Hana M, et al. Perceived barriers to seeking cancer care in the Gaza Strip: a cross-sectional study. BMC Health Serv Res. 2021;21(1):28.
Elshami M, Abu Kmeil H, Abu-Jazar M, Mahfouz I, Ashour D, Aljamal A, et al. Breast Cancer Awareness and Barriers to Early Presentation in the Gaza-Strip: A Cross-Sectional Study. J Glob Oncol. 2018;4:1–13.
Elshami M, Elshami A, Alshorbassi N, Alkhatib M, Ismail I, Abu-Nemer K, et al. Knowledge level of cancer symptoms and risk factors in the Gaza Strip: a cross-sectional study. BMC Public Health. 2020;20(1):414.
Elshami M, Al-Slaibi I, Abukmail H, Alser M, Radaydeh A, Alfuqaha A, et al. Knowledge of Palestinian women about cervical cancer warning signs: a national cross- sectional study. BMC Public Health. 2021;21(1):1779.
Elshami M, Thalji M, Abukmail H, Al-Slaibi I, Alser M, Radaydeh A, et al. Knowledge of cervical cancer risk factors among Palestinian women: a national cross-sectional study. BMC Womens Health. 2021;21(1):385.
Elshami M, Tuffaha A, Yaseen A, Alser M, Al-Slaibi I, Jabr H, et al. Awareness of ovarian cancer risk and protective factors: A national cross-sectional study from Palestine. PLoS ONE. 2022;17(3):e0265452.
Harvard Humanitarian Initiative. KoBoToolbox. https://bit.ly/3jWdUmi. Accessed 21 April 2022.
Power E, Simon A, Juszczyk D, Hiom S, Wardle J. Assessing awareness of colorectal cancer symptoms: measure development and results from a population survey in the UK. BMC Cancer. 2011;11:366.
Elshami M, Yaseen A, Alser M, Al-Slaibi I, Jabr H, Ubaiat S, et al. Knowledge of ovarian cancer symptoms among women in Palestine: a national cross-sectional study. BMC Public Health. 2021;21(1):1992.
Simon AE, Juszczyk D, Smyth N, Power E, Hiom S, Peake MD, et al. Knowledge of lung cancer symptoms and risk factors in the UK: development of a measure and results from a population-based survey. Thorax. 2012;67(5):426–32.
Simon AE, Wardle J, Grimmett C, Power E, Corker E, Menon U, et al. Ovarian and cervical cancer awareness: development of two validated measurement tools. J Fam Plann Reprod Health Care. 2012;38(3):167–74.
Stubbings S, Robb K, Waller J, Ramirez A, Austoker J, Macleod U, et al. Development of a measurement tool to assess public awareness of cancer. Br J Cancer. 2009;101(Suppl 2):S13-7.
American Cancer Society. American Cancer Society Guideline for Colorectal Cancer Screening. https://bit.ly/3cCl1vY. Accessed 21 April 2022.
Palestinian Central Bureau of Statistics. The current Status of the Palestinian Labor Force. https://bit.ly/3oFRt4O. Accessed 21 April 2022.
Gimeno-García AZ, Quintero E, Nicolás-Pérez D, Jiménez-Sosa A. Public awareness of colorectal cancer and screening in a Spanish population. Public Health. 2011;125(9):609–15.
McVeigh TP, Lowery AJ, Waldron RM, Mahmood A, Barry K. Assessing awareness of colorectal cancer symptoms and screening in a peripheral colorectal surgical unit: a survey based study. BMC Surg. 2013;13:20.
Almutairi KM, Alonazi WB, Alodhayani A, Vinluan JM, Ahmad M, Alhurishi SA, et al. A Cross-Sectional Assessment of Literacy and Awareness, Attitudes, and Beliefs About Colorectal Cancer and Its Screening in Riyadh Region. J Cancer Educ. 2018;33(3):660–7.
Al-Sharbatti S, Muttappallymyalil J, Sreedharan J, Almosawy Y. Predictors of Colorectal Cancer Knowledge among Adults in the United Arab Emirates. Asian Pac J Cancer Prev. 2017;18(9):2355–9.
Nasaif HA, Al Qallaf SM. Knowledge of Colorectal Cancer Symptoms and Risk Factors in the Kingdom of Bahrain: a Cross- Sectional Study. Asian Pac J Cancer Prev. 2018;19(8):2299–304.
Saeed RS, Bakir YY, Alkhalifah KH, Ali LM. Knowledge and Awareness of Colorectal Cancer among General Public of Kuwait. Asian Pac J Cancer Prev. 2018;19(9):2455–60.
Walter FM, Emery JD, Mendonca S, Hall N, Morris HC, Mills K, et al. Symptoms and patient factors associated with longer time to diagnosis for colorectal cancer: results from a prospective cohort study. Br J Cancer. 2016;115(5):533–41.
Simon AE, Waller J, Robb K, Wardle J. Patient delay in presentation of possible cancer symptoms: the contribution of knowledge and attitudes in a population sample from the United kingdom. Cancer Epidemiol Biomarkers Prev. 2010;19(9):2272–7.
Vega P, Valentín F, Cubiella J. Colorectal cancer diagnosis: Pitfalls and opportunities. World J Gastrointest Oncol. 2015;7(12):422–33.
Teng CLJ, Yu JT, Chen YH, Lin CH, Hwang WL. Early Colonoscopy Confers Survival Benefits on Colon Cancer Patients with Pre-Existing Iron Deficiency Anemia: A Nationwide Population-Based Study. PLoS One. 2014;9(1):e86714.
Taha H, Jaghbeer MA, Shteiwi M, AlKhaldi S, Berggren V. Knowledge and Perceptions about Colorectal Cancer in Jordan. Asian Pac J Cancer Prev. 2015;16(18):8479–86.
Tfaily MA, Naamani D, Kassir A, Sleiman S, Ouattara M, Moacdieh MP, et al. Awareness of Colorectal Cancer and Attitudes Towards Its Screening Guidelines in Lebanon. Ann Glob Health. 2019;85(1):75.
Al Abdouli L, Dalmook H, Akram Abdo M, Carrick FR, Abdul RM. Colorectal Cancer Risk Awareness and Screening Uptake among Adults in the United Arab Emirates. Asian Pac J Cancer Prev. 2018;19(8):2343–9.
Al-Dahshan A, Chehab M, Bala M, Omer M, AlMohamed O, Al-Kubaisi N, et al. Colorectal cancer awareness and its predictors among adults aged 50–74 years attending primary healthcare in the State of Qatar: a cross-sectional study. BMJ Open. 2020;10(7):e035651.
Kaya İ, Hoca O, Kulacoglu H. Knowledge and awareness of auxiliary health personnel about colorectal cancer. Turk J Gastroenterol. 2013;24:339–44.
Sindhu CK, Nijar AK, Leong PY, Li ZQ, Hong CY, Malar L, et al. Awareness of Colorectal Cancer among the Urban Population in the Klang Valley. Malays Fam Physician. 2019;14(3):18–27.
Brandt HM, Dolinger HR, Sharpe PA, Hardin JW, Berger FG. Relationship of colorectal cancer awareness and knowledge with colorectal cancer screening. Colorectal Cancer. 2012;1(5):383–96.
Knudsen MD, Hoff G, Tidemann-Andersen I, Bodin GE, Øvervold S, Berstad P. Public Awareness and Perceptions of Colorectal Cancer Prevention: a Cross-Sectional Survey. J Cancer Educ. 2021;36(5):957–64.
Anderson AS, Caswell S, Macleod M, Craigie AM, Stead M, Steele RJC, et al. Awareness of Lifestyle and Colorectal Cancer Risk: Findings from the BeWEL Study. Biomed Res Int. 2015;2015:871613.
Unger-Saldaña K, Saldaña-Tellez M, Potter MB, Van Loon K, Allen-Leigh B, Lajous M. Barriers and facilitators for colorectal cancer screening in a low-income urban community in Mexico City. Implement Sci Commun. 2020;1:64.
Tatari CR, Andersen B, Brogaard T, Badre-Esfahani SK, Jaafar N, Kirkegaard P. Perceptions about cancer and barriers towards cancer screening among ethnic minority women in a deprived area in Denmark – a qualitative study. BMC Public Health. 2020;20(1):921.
Kyle RG, Forbat L, Rauchhaus P, Hubbard G. Increased cancer awareness among British adolescents after a school-based educational intervention: a controlled before-and-after study with 6-month follow-up. BMC Public Health. 2013;13(1):190.
Schliemann D, Paramasivam D, Dahlui M, Cardwell CR, Somasundaram S, Ibrahim Tamin NSB, et al. Change in public awareness of colorectal cancer symptoms following the Be Cancer Alert Campaign in the multi-ethnic population of Malaysia. BMC Cancer. 2020;20(1):252.
Pedersen AF, Forbes L, Brain K, Hvidberg L, Wulff CN, Lagerlund M, et al. Negative cancer beliefs, recognition of cancer symptoms and anticipated time to help-seeking: an international cancer benchmarking partnership (ICBP) study. BMC Cancer. 2018;18(1):363.
World Health Organization. Mapping the Palestinian Heath Workforce: National Human Resources for Health Observatory. https://bit.ly/3AHZIUA. Accessed 21 April 2022.
UN Office for the Coordination of Humanitarian Affairs. Occupied Palestinian Territory: Humanitarian Atlas 2019. https://bit.ly/3LmuWpn. Accessed 21 April 2022.
Bedford JL, Barr SI. Diets and selected lifestyle practices of self-defined adult vegetarians from a population-based sample suggest they are more “health conscious.” Int J Behav Nutr Phys Act. 2005;2(1):4.
Acknowledgements
The authors would like to thank all participants who took part in the survey.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
ME and MA contributed to design of the study, data analysis, data interpretation, and drafting of the manuscript. MA, IA, SAN, BMM, WSI, AS, BY, YAQ, FKH, MFD, RRS, RTJ, KAA, MEA, MMH, IIA, BKA, MNA, ASA, MSA, OAA, RA, CTG, AYA, RMAN, NMA, and SMS contributed to design of the study, data collection, data entry, and data interpretation. NAE and BB contributed to design of the study, data interpretation, drafting of the manuscript, and supervision of the work. All authors have read and approved the final manuscript. Each author has participated sufficiently in the work to take public responsibility for the content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research Ethics Committee at the Islamic University of Gaza prior to starting data collection. In addition, the study was approved by the Human Resources Development department at the Palestinian MoH and the Helsinki Committee in the Gaza Strip on the 24th of June, 2019.
Before interviews, written informed consents were obtained from the participants and also from legal guardians of the illiterate participants. A detailed explanation of the study was given to all study participants with the emphasis that participation was completely voluntary, and the decision would not affect the medical care the participants receive. All study methods were carried out in accordance with relevant guidelines and regulations. Data confidentiality was maintained throughout the study.
Consent for publication
Not applicable.
Competing interests
All authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been updated to correct an author name.
Supplementary Information
Additional file 1:
Table 1. Multivariable logistic regression analyzing the association between the recognition of colorectal cancer signs/symptoms with mass/blood and participant characteristics. Table 2. Multivariable logistic regression analyzing the association between the recognition of colorectal cancer signs/symptoms of a non-specific nature and participant characteristics. Table 3. Multivariable logistic regression analyzing the association between the recognition of other gastrointestinal signs/symptoms and participant characteristics. Table 4. Bivariable logistic regression analyzing the association between recognizing colorectal cancer symptoms with mass/blood and participant characteristics. Table 5. Bivariable logistic regression analyzing the association between recognizing colorectal cancer symptoms of a non-specific nature and participant characteristics. Table 6. Bivariable logistic regression analyzing the association between recognizing other gastrointestinal symptoms and participant characteristics.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Elshami, M., Ayyad, M., Alser, M. et al. Awareness of colorectal cancer signs and symptoms: a national cross-sectional study from Palestine. BMC Public Health 22, 866 (2022). https://doi.org/10.1186/s12889-022-13285-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13285-8