Abstract
Background
In western countries, age at menarche (AAM) is nowadays lower than a century ago, coinciding with increased Body Mass Index (BMI) and prevalence of non-communicable diseases (NCD). This study aimed to determine the time trend in AAM, and its association with BMI and NCD prevalence at later age, in Indonesia.
Methods
We used secondary data of 15,744 women aged 15–65 years from the Indonesian Family Life Survey (IFLS) conducted in the period 1993 to 2015. Multiple linear regression was applied to determine the association of AAM with BMI, and Poisson regression with robust variance for investigating the association of AAM with NCD prevalence ratios. Models were adjusted for age, and effect modification by wealth status, living area, and region was investigated.
Results
AAM has significantly declined from 14.4 (SD:2.1) years of age in the 1940s to 13.4 y (SD:1.5) in the 1990s. AAM was inversely associated with BMI (β: − 0.30 kg/m2, 95%CI: − 0.37, − 0.22) and body weight (β: − 0.67 kg, 95%CI: − 0.75, − 0.54), but was not associated with height. After adjustment for age, AAM was not associated with NCD, i.e. hypertension, type 2 diabetes mellitus, liver diseases, asthma, chronic lung diseases, cardiovascular diseases, stroke, cancer, or arthritis. Including BMI in the models did not change the results.
Conclusions
From the 1940s to 1990s, AAM has declined with 1 year in Indonesia. Women with earlier AAM had higher BMI and body weight at later age, but AAM was not associated with NCD prevalence in later life in the Indonesian population. Further longitudinal research is needed to disentangle the direction of causality of the associations.
Similar content being viewed by others
Introduction
In recent decades, non-communicable diseases (NCD) have emerged as the leading cause of death in both developing and developed countries. In Indonesia, six of the top 10 leading causes of death consisted of NCD in 2017, of which stroke was the number one cause from 2007 to 2017 [1]. Based on Indonesian National Health survey data, the prevalence of NCD increased significantly from 2013 to 2018. For example, the prevalence of stroke among people aged 15 years or older increased from 7.0 to 10.9%, type 2 diabetes mellitus (DM) from 6.9 to 8.5%, and hypertension from 25.8 to 34.1%. The prevalence of cancer, arthritis, and cardiovascular diseases (CVD) also increased, especially among the older age groups (> 55 years).
The etiology of NCD is explained by a multitude of factors such as ethnicity, age, physical activity, dietary patterns, smoking status, as well as early biological maturation [2]. Overweight and obesity, which have globally increased over the past fourty years [3], are known as the most important proximal risk factors for NCD [4]. Any increase in the prevalence of overweight and obesity should therefore be of concern. The prevalence of overweight, obesity and abdominal obesity among people aged 15 years or older in Indonesia increased from 8.6, 10.5 and 18.8% in 2007 to 13.6, 21.8, and 31.0% in 2018, respectively [5]. Overweight and obesity during childhood have been associated with accelerated physical maturation [6]. Obese girls experience their menarche at an earlier age than normal [7], but it is not clear if higher BMI is either a cause or a consequence of earlier maturation, or both. In addition, some studies have reported that earlier age at menarche (AAM) is associated with increased risk of NCDs in later life, such as stroke, cardiovascular diseases [8], and diabetes [9]. Moreover, AAM has shown to be predictive for cardiovascular disease events and mortality [8].
In Indonesia, a previous study showed that higher Body Mass Index (BMI), higher parental income, and living in an urban area were associated with earlier puberty in both girls and boys based on Tanner scale assessment (pubic hair, female breast development, and male external genitalia) [10]. Globally, menarche occurs at an earlier age than in previous decades [11, 12]. For example, in Mexico mean AAM decreased from 13.6 to 12.6 years of age from 1900s to 1980s, while undergoing rapid economic transition, and earlier AAM was associated with diabetes and hypercholesterolaemia [13]. Therefore, early AAM may be an intermediary factor between childhood obesity and the development of NCD.
We aimed to describe the time trend in AAM, and to identify any associations of AAM with obesity and NCD among women from diverse socio-economic groups, living areas, and regions in Indonesia by analysing nationally representative data from the Indonesian Family Life Survey. We expected these associations to be inverse.
Material and methods
Indonesian family life survey
Data collection
The Indonesian Family Life Survey (IFLS) has so far been conducted in 5 waves, namely in 1993, 1997–1998, 2000, 2007–2008, and 2014–2015. IFLS is the only large longitudinal survey in Indonesia and represents 83% of the Indonesian population. Administration of questionnaires and health measurements, such as anthropometry and blood analysis, has been conducted under supervision of the non-profit RAND Corporation (Santa Monica, CA, USA). The aim of the IFLS survey is to provide multi-factorial data on economic and non-economic behavioural variables and outcomes such as food consumption, health status, and insurance utilization.
The first wave of IFLS included 13 out of 27 provinces and included 22,000 individuals living in 7244 households, using a stratified random sampling technique. The sampling method considered the heterogeneity of the population and represents four out of the five largest islands of Indonesia; Sumatra, Java, Kalimantan, and Sulawesi. Data collection areas were adapted from the areas covered by the National Socioeconomic Survey (SUSENAS) in 1993, which was based on the 1990 census. The details of the sampling frame have been described previously in an online IFLS report [14].
IFLS wave 2 collected data from the same individuals as in 1997, covering approximately 94.4% of the first wave. The next IFLS data collection rounds (wave 3–5) mostly interviewed dynasty households, which means that they already participated in any of the previous IFLS data collection rounds. The proportion of dynasty data was 95.3% in 2000 (wave 3), 93.6% in 2007 (wave 4), and 92% in 2014 (wave 5). The proportion of successfully re-contacted households was higher for the IFLS than generally seen in surveys conducted in the United States and Europe. Data collection, comprising self-reported data and direct measurements, was conducted by duly trained data collectors.
Participants
For the aim of the present analysis, data were selected of all women aged 15 years and older with a complete record for AAM, age, anthropometric indicators, and NCD from each IFLS wave. Information on AAM was only collected from married women, while NCD was assessed for all women, albeit only in wave 4 and 5. For the purpose of this study, only data of the most recent survey were included for women participating in multiple survey waves (Suplemental Fig. 1).
Explanatory and outcome variables
AAM was assessed using a questionnaire by asking: “how old were you (in years) at your first menstruation?” We classified early AAM as < 12 years of age, normative AAM as in the range ≥ 12 – < 16 years, and late AAM as ≥16 years. This classification was based on the AAM distribution in our population, defined as plus and minus one standard deviation of the mean (mean: 13.75 and SD: 1.80). Similar age classification of AAM has been used in previous studies [15, 16].
Trained data collectors measured body weight of each participant using a body weight scale up to the nearest tenth of a kilogram or one single decimal, while height was measured using a Seca plastic height board (model 213) up to the nearest millimeter. BMI was calculated as weight (kg)/height (m)2 and classified into categories of normal weight (BMI < 25), overweight (BMI ≥25 - < 30) and obese (BMI ≥30).
Occurrence of NCD was assessed by questionnaire, asking whether or not participants had been diagnosed with any of the following chronic conditions: hypertension, type 2 diabetes mellitus, asthma, chronic lung disease, cardiovascular disease, liver disease, stroke, cancer and arthritis. Because not all waves collected these data, only wave 4 and 5 were included in the part of the analysis relating AAM to NCD.
Other variables that were included in our analysis were household socio-economic status, living area, and region. A variable for socio-economic status (SES) was constructed by assigning weights of eleven household assets (ownership of the house, ownership of another building, posession of farmland, fishpond or poultry, vehicles, electronic devices (e.g. radio, tv, refrigerator or washing machine), savings, jewellery, and other assets) into a five-quintile wealth index by Principle Component Analysis (PCA). For the present analysis, we categorized this index further into three groups; poor for the two bottom quintiles, average for the two middle quintiles, and rich for the highest quintile. The same classification of SES has been used for IFLS data in previous studies [17]. Participants were categorized into rural and urban areas of living using the classification of Indonesia’s Bureau of Statistics [18], which is based on population density, percentage of agricultural households, and presence/access to facilities.
Statistical analysis
Data were analysed using STATA statistical software version 14. Data cleaning was employed at two levels; the first level was the data cleaning for AAM and BMI data which were extracted from all IFLS waves; and the second level was for NCD data, which were additionally extracted only from the last two waves (wave 4 and 5), since these were not available for the earlier waves. (Supplementary Fig. 1). Data on AAM were used to determine the time trend of AAM and its association with BMI, while NCD data were used to assess associations between AAM and NCD. Completeness of variables such as AAM, BMI, age, wealth index, and unplausible AAM and body weight because of input errors were considered in data cleaning. Wealth index, BMI and NCD were taken from the last wave in which the respondent was enrolled since these outcomes are influenced by age. Assumptions of normal data distribution was verified by visual inspection of Q-Q plots. In addition, multicollinearity was insepcted by plotting the correlation matrix of all independent variables and identifying the Variance Inflation Factor (VIF) for each variable. The correlation matrix showed that all correlation coefficientss were < 0.4, and the average VIF was < 2.
AAM, women’s weight, height, and BMI were described using means and standard deviations. We determined the mean AAM per decade, based on the birth year of participants, to investigate the time trend. Determinant variables in each wave were analyzed in relation to AAM by ANOVA and Chi-square test. Furthermore, associations between AAM and nutritional status (BMI, weight, and height) were determined by multiple linear regression and Poisson regression models with robust variance, adjusted for age. The data were stratified by wealth index, living area, and region, since these variables were found to be effect modifiers. Finally, we used Poisson regression models with robust variance to determine the association of AAM with the prevalence of NCD, while adjusting for age as well as for BMI as a potential intermediate.
Results
Characteristics of respondents
Characteristics of respondents are shown in Table 1. The total number of respondents was 15,744 women, and their average age was 36 years (SD:10.1 y). Most respondents were classified in the wealth index categories “poor” and “average”. More than half of respondents lived in urban areas and in the region of the islands Java and Bali.
Time trend of AAM
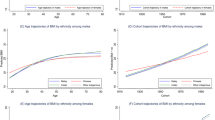
AAM decreased from 14.4 (SD:2.1) years of age for women born in the 1940s to 13.4 (SD:1.5) years of age for women born in the 1990s. Mean AAM over the entire time period was 13.8 years (SD:1.8). Of all respondents, 5.8% were categorized as having early AAM (< 12 years), 81.6% as normative (≥12 – < 16 years), and 12.5% as late (≥16 years). AAM was not significantly different between women who lived in urban (mean:13.7 y, SD:1.7) and rural areas (mean:13.9 y, SD:1.8; p:0.08), who lived on the two main ilsands Java or Bali (mean:13.7 y, SD:1.9) or elsewhere (mean:13.8 y, SD:1.7; p:0.10), or who fell in different wealth status classifications; poor (mean:13.7 y, SD:1.8), average (mean:13.8 y, SD: 1.8), and rich, (mean:13.8 y, SD:1,9; p:0.10) (Fig. 1).
AAM and body weight, height, and BMI
Table 2 shows the results of multiple linear regression models investigating the association between AAM and BMI. In unadjusted as well as in age-adjusted analysis, AAM (in years) was inversely associated with BMI (adjusted β: − 0.30 kg/m2 per year of AAM, 95%CI: − 0.37, − 0.22). When stratifying this analysis, the association appeared to be stronger in the highest wealth category (β: − 0.39 kg/m2 per year, 95%CI: − 0.43, − 0.26), in the urban area (β: − 0.35 kg/m2 per year, 95%CI: − 0.43, − 0.26) and at the two main islands (Java and Bali; β: − 0.33 kg/m2 per year, 95%CI: − 0.40, − 0.24) compared to the other socio-demographic categories. Further analysis using Poisson regression models adjusted for age showed that in later life, overweight and obesity were more prevalent among women with early age at menarche (overweight: PR: 1.11, 95%CI: 1.02–1.22; and obesity: PR: 1.35, 95%CI: 1.35–1.76) as compared to women with normative age at menarche, whereas the prevalence ratio of overweight and obesity among women with late age at menarche was lower (overweight: PR: 0.86, 95%CI: 0.81–0.94; and obesity: PR: 0.77, 95%CI: 0.67–0.87).
AAM was also inversely associated with current body weight (adjusted β: − 0.67 kg per year of AAM, 95%CI: − 0.75, − 0.54) (Table 3). The association was stronger in urban (β: − 0.68 kg per year of AAM, 95%CI: − 0.81, − 0.54) than in rural women (β: − 0.52 kg per year, 95%CI: − 0.67, − 0.38), whereas differences between other sociodemographic categories were small. The association between AAM and height was either small or absent (β: − 0.03 cm per year of AAM, 95%CI: − 0.09, 0.02). (Table 4).
AAM and risk of NCD
Hypertension was the NCD with the highest prevalence (14.7%) while liver disease and stroke were less prevalent (0.8 and 0.6% respectively) in the study population. Although AAM was associated with an increased prevalence of hypertension, cardiovascular diseases and arthritis in crude models, these associations disappeared after adjusting for age and BMI (Table 5).
Discussion
In this study, we found that among Indonesian women AAM declined over birth decades from 14.4 years in the 1940s to 13.4 years in the 1990s. Furthermore, AAM was inversely associated with BMI and body weight in later life, independently of age. AAM was also associated with a higher prevalence of several NCD such as hypertension, CVD, and arthritis, but this depended on age. Additional adjustment for BMI did not alter these results.
A previous study that reviewed published data indicated a similar time trend of AAM in Indonesia, with a decline from 14.4 y to 13.6 y since 1970 [19]. For China, also a decline in AAM has been reported, with an average of 16.2 y for women born before 1950 to 14.7 y for those born after 1959 [20]. Whereas AAM in China is estimated at 15.4 years for the period of 2004–2008, for Taiwan, it was 13.9 years for the same period of time; this disparity may have been influenced by the economic development in Taiwan since the mid-1980s, leading to changes in lifestyle and nutritional status, and thereby to earlier maturation of women [21]. Decline in AAM in both developed and developing countries has been associated with factors such as wealth index, access to health facilities, and intake of food, and it varies within populations based on the local context [22]. Nevertheless, AAM did neither differ between rural and urban areas, nor between different wealth groups in our study.
We observed a significant inverse association of AAM with BMI and body weight, indicating that each year of earlier menarche was associated with an increment in BMI of 0.30 kg m− 2, and of 0.67 kg in adult body weigth after adjustment for age. Previous research, both in western and Asian countries, showed a similar pattern [8, 23]. A systematic review showed that the mean difference in BMI of adult women with menarche < 12 years versus ≥12 years was 0.34 kg m− 2 [23]. This is less than what we found in the current study (1.13 kg m− 2) when using the same classification. In a survey among 12,336 Korean women it was reported that early AAM (defined as ≤11 years) was correlated with a higher BMI [24]. The same trend was also seen in a number of longitudinal studies from the UK that made use of mendelian randomization by genetic traits related to pubertal onset, although in one of these cohorts the association attenuated after adjusting for pre-pubertal BMI [25, 26].
The question arises whether increased body mass predisposes girls to earlier puberty, or that earlier puberty in physical and hormonal changes contributes to increased body (fat) mass in later life. In support of the prior pathway, a longitudinal study showed that girls with a higher percentage of body fat at 5 years of age, and higher BMI and waist circumference at 7 years of age, were more likely to be classified with earlier pubertal development at 9 years of age. Earlier pubertal development was assessed by breast development, level of estradiol, and pubertal developmental scale (PDS) [27]. Also, a higher BMI-for-age z score at 9 and 43 months of age, and rapid increase in BMI during childhood, were associated with having menarche before 12 years of age among 2083 women in Southern Brazil [28]. Furthermore, fast increases in BMI at 4 months, 1 year, and 4 year of age were associated with increased likelihood of having a 4.6-month earlier menarche in the United States [29]. This may be explained by the fact that children with higher BMI are exposed to higher circulating concentrations of leptin, which could stimulate gonadotropin releasing hormone and premature secretion of sex hormones [30]. A 4-year longitudinal study among adolescents showed that AAM indeed declined by approximately 1 month per 1-ng/mL increase in leptin concentration [31]. In contrast, however, cohort data from India, Peru, and Vietnam consistently showed that increases in BMI during childhood (1–8 years of age) were not associated with earlier menarche [32]. The discrepancy between findings might be explained by the lower obesity prevalence in low- and middle-income countries (LMICs) compared to advanced economies such as the United States and some Latin American and European countries [33, 34]. Despite rapid increases in the prevalence of childhood overweight in LMICs, the prevalence of undernutrition also remains high [32].
There is also evidence that early maturation may induce higher BMI in later life [35]. Prospective cohort studies conducted in the UK and in Australia showed that earlier menarche was related to higher BMI in middle age, independent of their BMI at 4–6 years of age, and at 20 years of age, independent of their BMI at 8 years of age, respectively [36, 37]. Furthermore, a systematic review on genetic predisposition of pubertal timing by mendelian randomization found that earlier pubertal timing assessed by several pubertal traits such as age at menarche, age at voice breaking, male genital and female breast development, was related to increased BMI at adult age [38]. Therefore, both pathways may play a role in the relationship between AAM and BMI which cannot be disentangled by our cross-sectional data.
Although we did not find any association with height, a previous large prospective study with data from 286,205 women from nine European countries found that they were 0.31 cm taller for each year of later menarche [39]. A prospective study in South Africa also showed an increase in adult height of 1.15 cm per year of later menarche after adjusting for prepubertal height and BMI [40]. It has been hypothesized that women with early menarche experience premature closure of the epiphyseal growth plate which is responsible for elongation of the bones. Therefore, later menarche would allow further development of the long bones resulting in a greater adult height [39].
Regarding NCD, a number of large studies did find associations between AAM and cardiovascular diseases, hypertension, and stroke, both in developed and developing countries [8, 20, 24], whereas some others, consistent with our findings, did not [13, 41]. Among 118,964 women with breast cancer from 117 epidemiological studies, it was shown that with every year decline in AAM, the risk for breast cancer increased with 5% [42]. Early menarche (< 12 years) was also identified to increase the risk of asthma [43]. Furthermore, a one-year earlier menarche was associated with a higher risk of Non-Alcoholic Fatty Acid Disease (NAFLD) [9, 44]. The effect of AAM on rheumatoid arthritis is still under debate, with some studies showing a protective effect for early AAM [45], as well as for late AAM [46], whereas others reported no association [41]. The longer estrogen exposure among women with earlier AAM may provide a possible mechanism for the related higher risk of NCD [39]. In addition, the higher BMI in middle age seen with earlier AAM may mediate the association with NCD. The prevalence of obesity among Indonesian women has increased while AAM has declined, as shown in this study. Even though the prevalence of NCD has also risen, it may not be at its highest point yet. The incidence of high blood pressure, type 2 diabetes mellitus and stroke is still much lower in Indonesia than for example in the UK [8], China [20], and Korea [24]. This may explain why an association between AAM and NCD for Indonesia could not yet be shown, although an association between AAM and BMI has been clearly demonstrated. More studies with large sample sizes and small confidence intervals are needed in similar populations to clarify the relationship between AAM and NCD.
This is the first study using nationally representative data to explore the trend of AAM and its association with nutritional status and disease outcomes in Indonesia. The longitudinal nature of this study allowed us to assess the trend in AAM over six decades based on the year of birth. This study highlights an inverse association between AAM and BMI, with the latter known to be the most important proximal risk factor for NCD. There are some limitations to our study. For instance, the retrospective recall of NCDs or AAM might not be accurate, although the respondents of IFLS were generally healthy and able to remember their health history. Self-reported AAM collected by personal interview, like we used for this study, was shown to be consistent with AAM recall 30 years earlier in a retrospective follow-up study [47], as well as in a study with repeated interviews of menstrual history in the period of 1985–1993 [48]. To better understand the associations between AAM, BMI and NCD, prospective, longitudinal research with more details on pubertal stage and measurement of sex hormones and other biological factors are needed. Full characterization of body compisition would also be needed instead of relying on BMI alone [35]. In the current study, no data on prepubertal BMI was available from the women included in the first two waves, nor for NCD data in the first three waves of IFLS. Possible selection bias may have occurred since data on AAM was only collected from married women. The analysis may have selectively excluded women due to early mortality or non-response; nevertheless, the number of missing cases was relatively small and therefore we do not expect it would change our conclusion.
Conclusion
In Indonesia, AAM declined over birth decades from 14.4 years in the 1940s to 13.4 years in the 1990s. We found that women from the Indonesian Family Life Survey with earlier AAM had a higher BMI and body weight later in life. Nevertheless, AAM was not independently associated with any of the NCD outcomes. With the prospect of rising overweight and obesity prevalence, future longitudinal cohort studies should include pubertal stage with comprehensive indicators, and including all risk factors related to early AAM, to unravel causal pathways.
Availability of data and materials
The data are available at https://www.rand.org/well-being/social-and-behavioral-policy/data/FLS/IFLS.html
Abbreviations
- AAM:
-
Age At Menarche
- BMI:
-
Boddy Mass Index
- NCD:
-
Non-Communicable Diseases
- SD:
-
Standard Deviation
- IFLS:
-
Indonesian Family Life Survey
- SUSENAS:
-
The Indonesia National Socio-economic Survey
- PCA:
-
Principal Component Analysis
- SES:
-
Socio-economic Status
- LMIC:
-
Low-and-Middle Income Countries
- NAFLD:
-
Non-alcoholic Fatty Acid Disease
References
The Institute for Health Metrics and Evaluation. Indonesia: what cause death the Most? 2019. http://www.healthdata.org/indonesia.
Masana LS, Ros E, Sudano I, Angoulvant D, Ibarretxe Gerediaga D, Murga Eizagaechevarria N, et al. Is there a role for lifestyle changes in cardiovascular prevention? What, when and how? Atheroscler Suppl. 2017;26:2–15. https://doi.org/10.1016/S1567-5688(17)30020-X.
Bentham J, Di Cesare M, Bilano V, Bixby H, Zhou B, Stevens GA, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–42. https://doi.org/10.1016/S0140-6736(17)32129-3.
Nyberg ST, Batty GD, Pentti J, Virtanen M, Alfredsson L, Fransson EI, et al. Obesity and loss of disease-free years owing to major non-communicable diseases: a multicohort study. Lancet Public Health. 2018;3:e490–7. https://doi.org/10.1016/S2468-2667(18)30139-7.
Kementerian Kesehatan Republik Indonesia. Laporan Nasional Riset Kesehatan Dasar 2018 (report of Indonesian basic health survey 2018). 2018.
World Health Organization (WHO). Consideration of the evidence on childhood obesity for the Commission on Ending Childhood Obesity: Report of the Ad hoc Working Group on Science and Evidence for Ending Childhood Obesity. Geneva: World Heal Organ; 2016. p. 219. https://doi.org/ISBN 978 92 4 151006 6.
Kaplowitz P. Pubertal development in girls: secular trends. Curr Opin Obstet Gynecol. 2006;18:487–91. https://doi.org/10.1097/01.gco.0000242949.02373.09.
Lakshman R, Forouhi NG, Sharp SJ, Luben R, Bingham SA, Khaw KT, et al. Early age at menarche associated with cardiovascular disease and mortality. J Clin Endocrinol Metab. 2009;94:4953–60. https://doi.org/10.1210/jc.2009-1789.
Mueller NT, Duncan BB, Barreto SM, Chor D, Bessel M, Aquino EML, et al. Earlier age at menarche is associated with higher diabetes risk and cardiometabolic disease risk factors in Brazilian adults: Brazilian longitudinal study of adult health (ELSA-Brasil). Cardiovasc Diabetol. 2014;13:1–8. https://doi.org/10.1186/1475-2840-13-22.
Hariadi Edi Saputra, Hakimi, Melda Deliana, Siska Mayasari Lubis KSA. Puberty onset in rural and urban children. Paediatr Indones 2011;51:207–212. https://doi.org/10.14238/pi57.1.2017.52-6.
Krieger N, Kiang MV, Kosheleva A, Waterman PD, Chen JT, Beckfield J. Age at menarche: 50-year socioeconomic trends among US-born black and white women. Am J Public Health. 2015;105:388–97. https://doi.org/10.2105/AJPH.2014.301936.
Hosokawa M, Imazeki S, Mizunuma H, Kubota T, Hayashi K. Secular trends in age at menarche and time to establish regular menstrual cycling in Japanese women born between 1930 and 1985. BMC Womens Health. 2012;12:1. https://doi.org/10.1186/1472-6874-12-19.
Petersohn I, Zarate-Ortiz A, Cepeda-Lopez A, Melse-Boonstra A, Petersohn I, Zarate-Ortiz AG, et al. Time trends in age at menarche and related non-communicable disease risk during the 20th century in Mexico. Nutrients. 2019;11:394. https://doi.org/10.3390/nu11020394.
Strauss J, Beegle K, Sikoki B, Dwiyanto A, Herwati Y, Witoelar F, et al. The 5th wave of the Indonesia family life survey (IFLS): overview and field report 2016.
Lee MH, Kim SH, Oh M, Lee KW, Park MJ. Age at menarche in Korean adolescents: trends and influencing factors. Reprod Health. 2016;13:1–7. https://doi.org/10.1186/s12978-016-0240-y.
Lim SW, Ahn JH, Lee JA, Kim DH, Seo JH, Lim JS. Early menarche is associated with metabolic syndrome and insulin resistance in premenopausal Korean women. Eur J Pediatr. 2016;175:97–104. https://doi.org/10.1007/s00431-015-2604-7.
Rachmi CN, Agho KE, Li M, Baur LA. Stunting, underweight and overweight in children aged 2.0-4.9 years in Indonesia: prevalence trends and associated risk factors. PLoS One. 2016;11:1–17. https://doi.org/10.1371/journal.pone.0154756.
Badan Pusat Statistik Indonesia. Regulation of the head of Indonesia’s Bureau of Statistics, number 37 of 2010 concerning urban and rural classification in Indonesia (Peraturan Kepala Badan Pusat Statistik Nomor 37 Tahun 2010 tentang Klasifikasi Perkotaan dan Perdesaan di Indonesia). 2010.
Wahab A, Wilopo SA, Hakimi M, Ismail D. Declining age at menarche in Indonesia: a systematic review and meta-analysis. Int J Adolesc Med Health. 2018:1–9. https://doi.org/10.1515/ijamh-2018-0021.
Yang L, Li L, Millwood IY, Peters SAE, Chen Y, Guo Y, et al. Age at menarche and risk of major cardiovascular diseases: evidence of birth cohort effects from a prospective study of 300,000 Chinese women. Int J Cardiol. 2017;227:497–502. https://doi.org/10.1016/j.ijcard.2016.10.115.
Chang CJ, Lai MM, Lin CC, Liu CS, Li TC, Li CI, et al. Age at menarche and its association with the metabolic syndrome in Taiwan. Obes Res Clin Pract. 2016;10:S26–34. https://doi.org/10.1016/j.orcp.2015.10.003.
McDowell MA, Brody DJ, Hughes JP. Has age at menarche changed? Results from the National Health and nutrition examination survey (NHANES) 1999-2004. J Adolesc Health. 2007;40:227–31. https://doi.org/10.1016/j.jadohealth.2006.10.002.
Prentice P, Viner RM. Pubertal timing and adult obesity and cardiometabolic risk in women and men: a systematic review and meta-analysis. Int J Obes. 2013;37:1036–43. https://doi.org/10.1038/ijo.2012.177.
Won JC, Hong JW, Noh JH, Kim D-J. Association between age at menarche and risk factors for cardiovascular diseases in Korean women. Medicine (Baltimore). 2016;95:e3580. https://doi.org/10.1097/md.0000000000003580.
Bell JA, Carslake D, Wade KH, Richmond RC, Langdon RJ, Vincent EE, et al. Influence of puberty timing on adiposity and cardiometabolic traits: a Mendelian randomisation study. PLoS Med. 2018;15:1–25. https://doi.org/10.1371/journal.pmed.1002641.
Gill D, Brewer CF, Del Greco MF, Sivakumaran P, Bowden J, Sheehan NA, et al. Age at menarche and adult body mass index: a Mendelian randomization study. Int J Obes. 2018;42:1574–81. https://doi.org/10.1038/s41366-018-0048-7.
Davison KK, Susman EJ, Birch LL. Percent body fat at age 5 predicts earlier pubertal development among girls at age 9. Pediatrics. 2003;111:815–21.
Martínez J, Araújo C, Horta BL, Gigante DP. Growth patterns in early childhood and the onset of menarche before age twelve. Rev Saude Publica. 2010;44:249–60. https://doi.org/10.1590/s0034-89102010000200004.
Flom JD, Cohn BA, Tehranifar P, Houghton LC, Wei Y, Protacio A, et al. Earlier age at menarche in girls with rapid early life growth: cohort and within sibling analyses. Ann Epidemiol. 2017;27:187–93.e2. https://doi.org/10.1016/j.annepidem.2017.01.004.
Shalitin S, Phillip M. Role of obesity and leptin in the pubertal process and pubertal growth - a review. Int J Obes. 2003;27:869–74. https://doi.org/10.1038/sj.ijo.0802328.
Matkovic V, Ilich JZ, Skugor M, Badenhop NE, Goel P, Clairmont A, et al. Leptin is inversely related to age at menarche in human females. J Clin Endocrinol Metab. 1997;82:3239–45. https://doi.org/10.1210/jc.82.10.3239.
Aurino E, Schott W, Penny ME, Behrman JR. Birth weight and prepubertal body size predict menarcheal age in India, Peru, and Vietnam. Ann N Y Acad Sci. 2018;1416:107–16. https://doi.org/10.1111/nyas.13445.
Walvoord EC. The timing of puberty: is it changing? Does it matter? J Adolesc Health. 2010;47:433–9. https://doi.org/10.1016/j.jadohealth.2010.05.018.
Currie C, Ahluwalia N, Godeau E, Nic Gabhainn S, Due P, Currie DB. Is obesity at individual and national level associated with lower age at menarche? Evidence from 34 countries in the health behaviour in school-aged children study. J Adolesc Health. 2012;50:621–6. https://doi.org/10.1016/j.jadohealth.2011.10.254.
Kaplowitz PB. Link between body fat and the timing of puberty. Pediatrics. 2008;121:S208–17. https://doi.org/10.1542/peds.2007-1813f.
Pierce MB, Leon DA. Age at menarche and adult BMI in the Aberdeen children of the 1950s cohort study. Am J Clin Nutr. 2005;82:733–9.
Le-Ha C, Beilin LJ, Burrows S, Huang RC, Hickey M, Mori TA, et al. Age at menarche and childhood body mass index as predictors of cardio-metabolic risk in young adulthood: a prospective cohort study. PLoS One. 2018;13:1–12. https://doi.org/10.1371/journal.pone.0209355.
Chan YM, Feld A, Jonsdottir-Lewis E. Effects of the timing of sex-steroid exposure in adolescence on adult health outcomes. J Clin Endocrinol Metab. 2019;104:4758–86. https://doi.org/10.1210/jc.2019-00569.
Onland-Moret NC, Peeters PHM, Van Gils CH, Clavel-Chapelon F, Key T, Tjønneland A, et al. Age at menarche in relation to adult height: the EPIC study. Am J Epidemiol. 2005;162:623–32. https://doi.org/10.1093/aje/kwi260.
Lundeen EA, Norris SA, Martorell R, Suchdev PS, Mehta NK, Richter LM, et al. Early life growth predicts pubertal development in south African adolescents. J Nutr. 2016;146:622–9. https://doi.org/10.3945/jn.115.222000.
Merlino LA, Cerhan JR, Criswell LA, Mikuls TR, Saag KG. Estrogen and other female reproductive risk factors are not strongly associated with the development of rheumatoid arthritis in elderly women. Semin Arthritis Rheum. 2003;33:72–82. https://doi.org/10.1016/S0049-0172(03)00084-2.
Hamajima N, Hirose K, Tajima K, Rohan T, Friedenreich CM, Calle EE, et al. Menarche, menopause, and breast cancer risk: individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol. 2012;13:1141–51. https://doi.org/10.1016/S1470-2045(12)70425-4.
Lieberoth S, Gade EJ, Brok J, Backer V, Thomsen SF. Age at menarche and risk of asthma: systematic review and meta-analysis. J Asthma. 2014;51:559–65. https://doi.org/10.3109/02770903.2014.903966.
Lu J, Zhang J, Du R, Wang T, Xu M, Xu Y, et al. Age at menarche is associated with the prevalence of non-alcoholic fatty liver disease later in life: J. Diabetes. 2017;9:53–60. https://doi.org/10.1111/1753-0407.12379.
Karlson EW, Mandl LA, Hankinson SE, Grodstein F. Do breast-feeding and other reproductive factors influence future risk of rheumatoid arthritis? Results from the nurses’ health study. Arthritis Rheum. 2004;50:3458–67. https://doi.org/10.1002/art.20621.
Pedersen M, Stripp C, Klarlund M, Olsen SF, Tjønneland AM, Frisch M. Diet and risk of rheumatoid arthritis in a prospective cohort. - travel doctor Online; 2005. p. 32.
Must A, Phillips SM, Naumova EN, Blum M, Harris S, Dawson-Hughes B, et al. Recall of early menstrual history and menarcheal body size: after 30 years, how well do women remember? Am J Epidemiol. 2002;155:672–9. https://doi.org/10.1093/aje/155.7.672.
Bosetti C, Tavani A, Negri E, Trichopoulos D, La Vecchia C. Reliability of data on medical conditions, menstrual and reproductive history provided by hospital controls. J Clin Epidemiol. 2001;54:902–6. https://doi.org/10.1016/S0895-4356(01)00362-6.
Acknowledgments
The author would like to thank RAND, who provided the dataset online.
Funding
This study was performed as part of PhD studies for which MA received a scholarship from Lembaga Pengelola Dana Pendidikan (LPDP), Republic of Indonesia. LPDP had no role in the design and writing process of this article.
Author information
Authors and Affiliations
Contributions
All authors had an essential role in formulation of the research questions; MA and AMB wrote the first draft of the paper, MA analysed the data; MA, MLH, AMB, and EJMF were involved in interpretation of the data and revision of the manuscript. All authors have read and approved the final paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The IFLS and the survey protocol were reviewed and approved by Institutional Review Boards in the USA and the Ethics committee of Universitas Indonesia based in Jakarta for the first wave of IFLS, and by Universitas Gadjah Mada in Yogyakarta for IFLS waves two to five. All methods were performed in accordance with the relevant guidelines and regulations by including a statement in the Ethics approval and informed consent paper. Informed consent was obtained from all participants to participate after explanation of the study.
Consent for publication
Not applicable.
Competing interests
All authors stated no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Asrullah, M., L’Hoir, M., Feskens, E.J.M. et al. Trend in age at menarche and its association with body weight, body mass index and non-communicable disease prevalence in Indonesia: evidence from the Indonesian Family Life Survey (IFLS). BMC Public Health 22, 628 (2022). https://doi.org/10.1186/s12889-022-12995-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-12995-3