Abstract
Background
COVID-19 has resulted in substantial global upheaval. Resilience is important in protecting wellbeing, however few studies have investigated changes in resilience over time, and associations between resilience with depression, anxiety, stress, and physical activity during the COVID-19 pandemic.
Methods
Online surveys were conducted to collect both longitudinal and cross-sectional data at three time points during 2020. Australian adults aged 18 years and over were invited to complete the online surveys. Measures include the six-item Brief Resilience Scale, the 21-item Depression, Anxiety and Stress Scale, and the Active Australia Survey which have eight items identifying the duration and frequency of walking, and moderate and vigorous physical activities (MVPA), over the past 7 days. General linear mixed models and general linear models were used in the analysis.
Results
In the longitudinal sample, adjusted differences (aDif) in resilience scores did not significantly change over time (time 2 vs. time 1 [aDif = − 0.02, 95% CI = − 0.08, 0.03], and time 3 vs. time 1 [aDif = < 0.01, 95% CI = − 0.07, 0.06]). On average, those engaging in at least 150 min of MVPA per week (aDif = 0.10, 95% CI = 0.04, 0.16), and having depression (aDif = 0.40, 95% CI = 0.33), anxiety (aDif = 0.34, 95% CI = 0.26, 0.41), and stress scores (aDif = 0.30, 95% CI = 0.23, 0.37) within the normal range had significantly higher resilience scores. The association between resilience and physical activity was independent of depression, anxiety, and stress levels. All results were similar for the cross-sectional sample.
Conclusions
Resilience scores did not change significantly during the COVID-19 pandemic. However, there were significant associations between resilience with physical activity and psychological distress. This research helps inform future interventions to enhance or nurture resilience, particularly targeted at people identified as at risk of psychological distress.
Similar content being viewed by others
Background
Initially reported in November 2019, the novel coronavirus (COVID-19) has infected more than 244 million people worldwide, with more than 4.9 million deaths (25 October 2021) [1]. In addition to causing a global health emergency, there has been subsequent social and economic repercussions on the world’s population due to government-imposed restrictions to protect public health [2]. How people respond to a persistent stressor, such as the COVID-19 pandemic, may vary based on individual resilience levels [3], which can be defined as “the process involving an ability to withstand and cope with ongoing or repeated demands and maintain healthy functioning in different domains of life such as work and family”(p.637) [4]. Understanding resilience and how it changes across time may help in designing interventions that aim to minimise psychological distress.
Few studies have examined changes in resilience during the COVID-19 pandemic. Sturman (2020) compared levels of resilience in the United States prior to the declaration of a global pandemic (November and December 2019), to levels in the early stages of the pandemic (mid-April 2020), and found no significant change over time [5]. Similarly, Kim et al. (2020) found no significant differences in resilience of Israeli adults between the peak of the COVID-19 pandemic, when Government-enforced restrictions were imposed, and 2 months later when the restrictions had been lifted [6]. However, a USA study found that resilience in the third week of COVID-19 stay-at-home restrictions (April 2020) were lower compared to normative data collected before the pandemic [7]. Additionally, we could not identify any studies examining longitudinal changes in resilience in Australian adults.
Resilience is an important protective factor against psychological distress. A systematic review and meta-analysis found that older adults with higher resilience were less likely to have depressive symptoms [8]; however, no Australian studies were included. To our knowledge, only two studies of resilience and depression have been undertaken in Australia. One study among Iranian immigrants living in Australia found lower levels of resilience associated with higher levels of depression [9]. In contrast, another study found no significant associations between resilience and depression among homeless people in regional Australia [10]. The association between resilience and anxiety was also investigated in another study that found higher levels of resilience was associated with less anxiety among Australians aged 55–90 years [11]. Additionally, several pilot interventions that aimed to improve participants’ resilience through education workshops appeared to have positive effects in mitigating workplace stress among Australian nurses [12,13,14]. However, these previous studies are limited by their cross-sectional design or were not conducted among the general population. A more recent study of Australian parents reported loneliness as a significant contributor to stress during the pandemic, however high levels of social support were associated with both lower stress and anxiety [15]. Healthcare professionals are also predisposed to significant distress and anxiety, despite high levels of resilience, suggesting resilience alone is insufficient as a protective toll against poor mental health [16].
Physical activity is an important health behaviour that benefits both physical and mental health [17]. Studies conducted during the COVID-19 pandemic consistently show strong positive associations between resilience and physical activity levels [7, 18, 19]. One possible underlying mechanism for this association could be due to the positive effect of physical activity on mental health [20]. However, whether physical activity is associated with resilience, independent of mental health status, has not been investigated in these cross-sectional studies. Furthermore, to our knowledge, no Australian study of these relationships has been found.
Therefore, this study aims to investigate: 1) changes in the resilience level of Australian adults over time during the pandemic; and 2) associations between resilience with depression, anxiety, stress, and physical activity. Findings from this study contribute important insights into the role of resilience for physical activity behaviour and psychological distress among Australian adults during the pandemic.
Methods
Study design and participants
Online surveys were conducted to collect both longitudinal and cross-sectional data at three time points. The first survey was conducted early on during the COVID-19 pandemic from 9th to 19th April 2020; the second from 30th July to 16th August 2020; and the third between 1st and 25th December 2020. During the first time point, Australian state governments had adopted extraordinary measures to reduce the rates of infection including social distancing, lockdowns, and travel restrictions. During the second time point, all Australian states except Victoria had relaxed restrictions due to low case numbers of the infection. At the time of the third survey, most COVID-19 restrictions were lifted in all States and Territories as the rates of infection were largely under control [21, 22].
At each survey, participants (including new participants recruited for survey 2) were asked if they would like to participate in future data collection opportunities. Those completing at least two surveys became part of a longitudinal cohort while those who elected to complete only one survey formed the cross-sectional cohort. The surveys were anonymous and hosted on the Qualtrics survey platform. Australian adults aged 18 years and over were invited to complete the surveys using paid Facebook advertising, social media (e.g., Twitter) and institutional sources including email lists. Online informed consent was provided by all participants after they had read the information sheet that outlined the nature of their participation, the risks and benefits of participation, and how the data would be used. Ethical approval was granted by Central Queensland University’s Human Research Ethics Committee (Approval number 22332).
Measures
Demographic characteristics included age (years), gender, years of schooling, weekly household income (< 1000 AUD, 1000 - < 2000 AUD, or ≥ 2000 AUD), and marital status (in a relationship or not). Chronic disease status (Yes/No) was identified using the question; “Have you ever been told by a doctor that you have any chronic health problems?”. These included one or a combination of heart disease, high blood pressure, stroke, cancer, depressive disorder, anxiety disorder, psychotic illness, bipolar disorder, diabetes, arthritis, chronic back/neck pain, asthma, COPD, and chronic kidney/renal diseases [23].
Resilience was assessed using the six-item Brief Resilience Scale (BRS). The BRS measures an individuals’ ability to bounce back from an adverse event and focuses on the ability to recover [24]. The BRS is a reliable measure of resilience, with Cronbach’s alpha ranging from 0.80 to 0.91 and a 1 month test-retest reliability (ICC) of 0.69 [24]. The BRS is comprised of six items with three positively worded items (1, 3, and 5) and negatively worded items (2, 4, and 6). For example, a positive item states “I tend to bounce back quickly after hard times” while a negative item states “I have a hard time making it through stressful events”. Responses were provided on a 5-point Likert scale with anchors at 1 (strongly disagree) and 5 (strongly agree). The scale was scored by reverse coding the negative items and then averaging the total score for the six items. Final scores range from 1.0–5.0 with a score of 3.0–4.3 considered a normal level of resilience [25].
Psychological distress was measured using the 21-item Depression, Anxiety and Stress Scale (DASS-21) [26]. The DASS-21 has shown acceptable construct validity and high reliability (Cronbach’s alphas were 0.88, 0.82 and 0.90 for depression, anxiety and stress respectively) in a non-clinical adult population [27]. Each domain has seven items scored on a 4-point Likert scale between 0 (did not apply to me at all) and 3 (applied to me very much, or most of the time). Example items were “I was aware of dryness of my mouth” or “I found myself getting agitated”. A score was calculated for each domain by adding the scores for the relevant items and multiplying by two. Standard cut-points were used to determine whether participants had symptom severity above normal for depression (≥10 points), anxiety (≥8 points), and stress (≥15 points) [26].
Physical activity was assessed using the Active Australia Survey (AAS), which comprises eight items identifying the duration and frequency of walking, and moderate and vigorous (MVPA) physical activities, over the past 7 days. For example, questions about walking are “In the last week, how many times have you walked continuously, for at least 10 minutes, for recreation, exercise or to get to or from places?” and “What do you estimate was the total time that you spent walking in this way in the last week?”. The AAS guidelines were used to calculate total physical activity by summing minutes of walking, minutes of moderate activity, and minutes of vigorous activity (multiplied by 2). Participants were then categorised as meeting the physical activity guidelines (≥150 min of moderate – vigorous (MVPA) per week) or not (< 150 min MVPA per week) [28]. The AAS criterion validity has been found to be acceptable for use in self-administered format, with correlations between self-reported physical activity and weekly pedometer steps, and accelerometry being 0.43 and 0.52 respectively [29].
Analyses
Statistical analysis was undertaken using SAS software v9.4. Two datasets, longitudinal and repeated cross-sectional, were analysed separately. Participants completing at least two surveys were included in the longitudinal dataset. The repeated cross-sectional dataset excluded those in the longitudinal dataset and therefore included only those completing one survey. Descriptive statistics (mean, standard deviation, and percentages) were calculated and are presented for each time point. Changes in resilience scores were examined using general linear mixed models for the longitudinal data, and general linear models for cross-sectional data. In addition to bivariate analyses, estimated changes in resilience scores were also adjusted for age, gender, years of education, weekly household income, relationship status, and chronic disease status. Multiple comparison correction was applied using the simulation option in PROC GLIMMIX.
Associations between resilience scores with physical activity and depression, anxiety, and stress were also examined using general linear mixed models for the longitudinal data and general linear models for the cross-sectional data. Three models were run for both datasets. Model 1 included resilience scores, time and either physical activity, depression, anxiety, or stress. Model 2 included the additional covariates: age, gender, years of education, weekly household income, relationship status, and chronic disease status. To examine whether the observed associations were independent, physical activity, depression, anxiety, and stress were also included in Model 3 together with time and all other covariates.
Due to missing values for the household income variable being higher than 10%, analyses were conducted with and without household income as a covariate. As the results between these two analyses did not change the findings, only models including household income are presented. Crude and adjusted differences in resilience scores with 95% confidence intervals are reported. All p-values were two sided and considered significant if < 0.05.
Results
Table 1 shows characteristics of the longitudinal sample. At baseline, the majority of respondents were women (68.7%) and in a relationship (64.6%), with almost half reporting a chronic disease (47.5%). On average, participants were 52.5 (SD = 14.3) years old and had about 16 (SD = 4.7) years of education. Most had scores within the normal range for depression (64.0%), anxiety (80.7%), and stress (72.9%). More than half met the physical activity guidelines (56.4%). Average resilience score was about 3.4 out of 5.0 and within the normal range (3.0–4.3). The characteristics of those in the cross-sectional sample were very similar (Table 2).
Table 3 shows changes in resilience scores over time. In the longitudinal sample, crude (Model 1) and adjusted differences (aDif) (Model 2) in resilience scores were not significant between time 2 vs. time 1 (aDif = − 0.02, 95% CI = − 0.08, 0.03), and time 3 vs. time 1 (aDif = < 0.01, 95% CI = − 0.07, 0.06). Similarly, in the cross-sectional sample, crude and adjusted differences in resilience scores were not significant between time 2 vs. time 1 (aDif = − 0.04, 95% CI = − 0.14, 0.07), and time 3 vs. time 1 (aDif = − 0.02, 95% CI = − 0.15, 0.11).
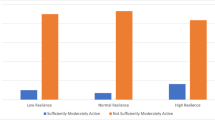
Table 4 shows associations between resilience scores with physical activity, depression, anxiety, and stress. On average, those engaging in at least 150 min of MVPA per week had a significantly higher resilience score (Model 2) in the longitudinal (aDif = 0.10, 95% CI = 0.04, 0.16) and cross-sectional samples (aDif = 0.19, 95% CI = 0.11, 0.27). Resilience scores were also significantly higher for those with depression scores in the normal range (longitudinal sample: aDif = 0.40, 95% CI = 0.33, 0.46; cross-sectional sample: aDif = 0.72, 95% CI = 0.64, 0.79), anxiety scores in the normal range (longitudinal sample: aDif = 0.34, 95% CI = 0.26, 0.41; cross-sectional sample: aDif = 0.68, 95% CI = 0.60, 0.77), and stress scores in the normal range (longitudinal sample: aDif = 0.30, 95% CI = 0.23, 0.37; cross-sectional sample: aDif = 0.71, 95% CI = 0.63, 0.80). Additionally, model 3 shows significant associations between resilience with physical activity, depression, anxiety, and stress, independently from one another. Specifically, resilience scores were, on average, higher for those engaging in at least 150 min MVPA per week (longitudinal sample: aDif = 0.07, 95% CI = 0.01, 0.13; cross-sectional sample: aDif = 0.15, 95% CI = 0.08, 0.21), having depression scores in the normal range (longitudinal sample: aDif = 0.30, 95% CI = 0.22, 0.37; cross-sectional sample: aDif = 0.45, 95% CI = 0.37, 0.53), anxiety scores in the normal range (longitudinal sample: aDif = 0.19, 95% CI = 0.11, 0.27; cross-sectional sample: aDif = 0.20, 95% CI = 0.10, 0.30), and stress scores in the normal range (longitudinal sample: aDif = 0.12, 95% CI = 0.04, 0.19; cross-sectional sample: aDif = 0.30, 95% CI = 0.20, 0.40).
Discussion
This study aimed to investigate changes in resilience of Australian adults across three time points in 2020 during the COVID-19 pandemic, and the associations between resilience and physical activity, depression, anxiety, and stress. The findings show that resilience scores did not change significantly during the pandemic and that participants who engaged in at least 150 MVPA minutes per week, and with depression, anxiety, and stress scores within the normal range, had higher resilience scores. The findings were consistent between the longitudinal and cross-sectional datasets; however, the effects were larger in the cross-sectional data.
Given the extraordinary social circumstances brought about by Australian state governments to enforce movement restrictions in response to the COVID-19 pandemic, and the uncertainty as a result of the health and economic impact of the pandemic, resilience levels may have changed. However, the results from this study suggest that resilience levels largely remained stable during the pandemic, which is consistent with the results from a study in Israel [6]. This is likely due to the samples (both longitudinal and cross-sectional) including mostly Australian adults (about three quarters) with high or normal levels of resilience. Therefore, they may manage and adapt well to the impacts caused by the pandemic. Another factor may be that the Australian government was effective in responding to the pandemic (ranking 3rd among OECD countries) and providing Australians with financial support and mental health consultation via telehealth [30], and therefore helping to alleviate the impacts. It is less likely, but also possible, that levels of resilience may have decreased between pre-COVID-19 and our first survey. Unfortunately, pre-COVID-19 data are not available for comparison. However, one study comparing two cross-sectional samples in small towns in upstate New York found no significant difference in resilience between pre-COVID-19 (November and December 2019) and peak-COVID-19 (mid-April 2020) [5].
Our findings are consistent with previous studies that have found inverse associations between levels of resilience and psychological distress among patients with chronic diseases [31,32,33], and medical students [34, 35]. This finding is also consistent with those from other studies conducted during the COVID-19 pandemic in the U.S [36, 37] and Italy [38]. These associations were expected, as resilience reflects an individual’s ability to cope with life’s adversity, trauma, and threats; and therefore, plays a role as an adaptive defence system against psychological distress such as depression, anxiety, and stress [39]. Given their significant effects on resilience, depression, anxiety, and stress are important factors that should be considered in interventions to improve resilience level in adult populations.
Resilience was also found to be positively associated with physical activity levels in studies conducted during the COVID-19 pandemic, which is consistent with findings in the present study [7, 18, 19]. The positive effects of physical activity on resilience may occur through improving mental health and possible underlying mechanisms for this were discussed by Silverman et al. (2014) [20]. For example, physical activity could serve as a buffer against stress and stress-related disorders. Physical activity also has benefits on brain and hormonal stress-responsive systems that could improve mood and cognition [20, 40]. In this study, we found that physical activity was associated with resilience, independent of depression, anxiety, and stress levels. Although the effect size of physical activity (adjusted difference of 0.07 points) was small compared to that of depression (0.30 points), anxiety (0.19 points), and stress (0.12 points). Given that physical activity has other benefits on both physical and mental health [17], it is still an important factor for consideration in interventions targeting resilience levels.
There are a number of strengths in this study. First, the sample size is large with participants from all states and territories in Australia. Second, to the best of our knowledge, this is the first longitudinal study to explore levels of resilience during the COVID-19 pandemic in Australia. However, the study has limitations. Participation in this study was voluntary with nearly half of the sample having at least one chronic health condition and therefore, the findings may not be generalisable to populations with different characteristics. The self-reported questionnaires are also subject to recall bias, despite being validated instruments. In addition, the first survey started when the pandemic had already begun; and no pre-COVID-19 data was available. Therefore, it is not possible to know whether (and how) resilience scores changed between the pre-COVID-19 period and the first survey.
For the future, the findings from this study helps inform interventions that aim to enhance or nurture resilience. In particular, health promotion strategies that screen for, then target people identified as being at risk of psychological distress, those with low levels of resilience, or those not meeting the physical activity guidelines may maximize the effects of the interventions. Primary health care providers, Government websites, not-for-profit, or other mental health services could provide rapid screening then direct people to appropriate care.
Conclusions
Resilience scores did not change significantly during the COVID-19 pandemic. Participants who met the physical activity guidelines, had depression, anxiety, and stress scores within the normal range, had higher resilience scores compared to those who were less active and those with more psychological distress. Maintaining healthy behaviours such as regular physical activity may buffer the adverse psychological effect of the pandemic and maintain mental health and wellbeing.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AAS:
-
the Active Australia Survey
- BRS:
-
The Brief Resilience Scale
- DASS-21:
-
the Depression, Anxiety, and Stress Scale
- MVPA:
-
Moderate and Vigorous Physical Activity
- OECD:
-
Organisation for Economic Cooperation and Development
References
Countries where COVID-19 has spread [https://www.worldometers.info/coronavirus/countries-where-coronavirus-has-spread/]. Accessed 26 Jan 2022.
Fitzgerald DA, Nunn K, Isaacs D. Consequences of physical distancing emanating from the COVID-19 pandemic: an Australian perspective. Paediatr Respir Rev. 2020;35:25–30.
Vinkers CH, van Amelsvoort T, Bisson JI, Branchi I, Cryan JF, Domschke K, et al. Stress resilience during the coronavirus pandemic. Eur Neuropsychopharmacol. 2020;35:12–6.
Schetter CD, Dolbier C. Resilience in the context of chronic stress and health in adults. Soc Personal Psychol Compass. 2011;5(9):634–52.
Sturman ED. Coping with Covid-19: resilience and psychological well-being in the midst of a pandemic. J Soc Clin Psychol. 2020;39(7):561–70.
Kimhi S, Marciano H, Eshel Y, Adini B. Recovery from the COVID-19 pandemic: distress and resilience. Int J Disast Risk Reduct. 2020;50:101843.
Killgore WDS, Taylor EC, Cloonan SA, Dailey NS. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 2020;291:113216.
Wermelinger Ávila MP, Lucchetti ALG, Lucchetti G. Association between depression and resilience in older adults: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2017;32(3):237–46.
Hosseini A, Kakuma R, Ghazinour M, Davern M, Evans WP, Minas H. Migration experience, resilience and depression: a study of Iranian immigrants living in Australia. Int J Cult Ment Health. 2017;10(1):108–20.
Sharpley CF, Murcell N, Anderson M, Bitsika V, Fourie PJ, Agnew LL. An exploration of recent life stress, psychological resilience, purpose in life, and optimism as correlates of depression in social housing residents in rural Australia. Int J Ment Health. 2021;50(3):1–16.
Li WW, Miller DJ. The impact of coping and resilience on anxiety among older Australians. Aust J Psychol. 2017;69(4):263–72.
Craigie M, Slatyer S, Hegney D, Osseiran-Moisson R, Gentry E, Davis S, et al. A pilot evaluation of a mindful self-care and resiliency (MSCR) intervention for nurses. Mindfulness. 2016;7(3):764–74.
Slatyer S, Craigie M, Heritage B, Davis S, Rees C. Evaluating the effectiveness of a brief mindful self-care and resiliency (MSCR) intervention for nurses: a controlled trial. Mindfulness. 2018;9(2):534–46.
Foster K, Shochet I, Wurfl A, Roche M, Maybery D, Shakespeare-Finch J, et al. On PAR: a feasibility study of the promoting adult resilience programme with mental health nurses. Int J Ment Health Nurs. 2018;27(5):1470–80.
Mikocka-Walus A, Stokes M, Evans S, Olive L, Westrupp E. Finding the power within and without: how can we strengthen resilience against symptoms of stress, anxiety, and depression in Australian parents during the COVID-19 pandemic? J Psychosom Res. 2021;145:110433.
Smallwood N, Karimi L, Bismark M, Putland M, Johnson D, Dharmage SC, et al. High levels of psychosocial distress among Australian frontline healthcare workers during the COVID-19 pandemic: a cross-sectional survey. Gen Psychiatr. 2021;34(5):e100577.
Physical activity guidelines advisory committee: 2018 physical activity guidelines advisory committee scientific report. In. Washington, DC: U.S. Department of Health and Human Services; 2018.
Carriedo A, Cecchini JA, Fernández-Río J, Méndez-Giménez A. Resilience and physical activity in people under home isolation due to COVID-19: a preliminary evaluation. Ment Health Phys Act. 2020;19:100361.
Zach S, Zeev A, Ophir M, Eilat-Adar S. Physical activity, resilience, emotions, moods, and weight control of older adults during the COVID-19 global crisis. Eur Rev Aging Phys Act. 2021;18(1):5.
Silverman MN, Deuster PA. Biological mechanisms underlying the role of physical fitness in health and resilience. Interface Focus. 2014;4(5):20140040.
Coronavirus (COVID-19) Restrictions [https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/coronavirus-covid-19-restrictions]. Accessed 22 Mar 2021.
Victoria’s Restriction Levels [https://www.dhhs.vic.gov.au/victorias-restriction-levels-covid-19]. Accessed 22 Mar 2021.
Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020;17(11):4065.
Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200.
Smith BW, Epstein EM, Ortiz JA, Christopher PJ, Tooley EM. The foundations of resilience: what are the critical resources for bouncing Back from stress? In: Prince-Embury S, Saklofske DH, editors. Resilience in children, adolescents, and adults: translating research into practice. New York: Springer New York; 2013. p. 167–87.
Lovibond S, Lovibond P. Manual for the depression anxiety stress scales. Sydney: Psychology Foundation; 1995. ISBN 7334–1423-0; 1995
Henry JD, Crawford JR. The short-form version of the depression anxiety stress scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44(2):227–39.
Australian Institute of Health and Welfare. The active Australia survey: a guide and manual for implementation, analysis and reportingvol. Cat. no. CVD 22. Canberra: AIHW; 2003.
Brown WJ, Burton NW, Marshall AL, Miller YD. Reliability and validity of a modified self-administered version of the active Australia physical activity survey in a sample of mid-age women. Aust N Z J Public Health. 2008;32(6):535–41.
Global report gives Australia an A for coronavirus response but a D on climate [https://theconversation.com/global-report-gives-australia-an-a-for-coronavirus-response-but-a-d-on-climate-141982]. Accessed 26 Jan 2022.
Tian X, Gao Q, Li G, Zou G, Liu C, Kong L, et al. Resilience is associated with low psychological distress in renal transplant recipients. Gen Hosp Psychiatry. 2016;39:86–90.
Min JA, Yoon S, Lee CU, Chae JH, Lee C, Song KY, et al. Psychological resilience contributes to low emotional distress in cancer patients. Support Care Cancer. 2013;21(9):2469–76.
Shin J-I, Chae J-H, Min J-A, Lee C-U, Hwang S-I, Lee B-S, et al. Resilience as a possible predictor for psychological distress in chronic spinal cord injured patients living in the community. Ann Rehabil Med. 2012;36(6):815–20.
Bacchi S, Licinio J. Resilience and psychological distress in psychology and medical students. Acad Psychiatry. 2017;41(2):185–8.
Rahimi B, Baetz M, Bowen R, Balbuena L. Resilience, stress, and coping among Canadian medical students. Can Med Educ J. 2014;5(1):e5–e12.
Barzilay R, Moore TM, Greenberg DM, DiDomenico GE, Brown LA, White LK, et al. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl Psychiatry. 2020;10(1):291.
Riehm KE, Brenneke SG, Adams LB, Gilan D, Lieb K, Kunzler AM, et al. Association between psychological resilience and changes in mental distress during the COVID-19 pandemic. J Affect Disord. 2021;282:381–5.
Lenzo V, Quattropani MC, Musetti A, Zenesini C, Freda MF, Lemmo D, et al. Resilience contributes to low emotional impact of the COVID-19 outbreak among the general population in Italy. Front Psychol. 2020;11(3062).
Rutter M. Resilience in the face of adversity: protective factors and resistance to psychiatric disorder. Br J Psychiatry. 2018;147(6):598–611.
Matta Mello Portugal E, Cevada T, Sobral Monteiro-Junior R, Teixeira Guimarães T, da Cruz RE, Lattari E, et al. Neuroscience of exercise: from neurobiology mechanisms to mental health. Neuropsychobiology. 2013;68(1):1–14.
Acknowledgements
Not applicable.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization (C.V, K. C, R.S), Data curation (T.L.T), Analysis (Q.G.T, K.C), Original draft (Q.G.T, K.C), Review and Edit (C.V, S.K, S.L.W, S.J.A, T.L.T, A.S.F, R.S). All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was granted by Central Queensland University’s Human Research Ethics Committee (Approval number 22332). Online informed consent was provided by all participants. All methods were carried out in accordance with the Helsinki declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
To, Q.G., Vandelanotte, C., Cope, K. et al. The association of resilience with depression, anxiety, stress and physical activity during the COVID-19 pandemic. BMC Public Health 22, 491 (2022). https://doi.org/10.1186/s12889-022-12911-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-12911-9