Abstract
Background
Intimate partner violence (IPV) is defined as acts of physical aggression, sexual coercion, psychological/emotional abuse, or controlling behaviors by a current or former partner or spouse. IPV has a special concern for pregnant women since it leads to higher rates of miscarriage, several complications including adverse birth outcomes. So far, the effect of contextual factors on IPV was largely overlooked. Therefore, this study aimed to assess the magnitude and factors associated with IPV among pregnant women in Ethiopia.
Method
Data from the 2016 Ethiopian Demographic and Health Survey was used for this study. A total of 4167 (weighted sample) pregnant women were included in the analysis. The multi-level logistic regression model was fitted to identify factors associated with IPV. Finally, the adjusted odds ratio (AOR) with 95% CI and random effects for the multilevel logistic regression model was reported.
Results
In this study, the overall magnitude of IPV among pregnant women was 28.74 (95% CI 27.38, 30.13) with emotional violence being the most common (24.09%) type. In the multi-level analysis, women with no education (AOR = 2.07; 95%CI 1.23, 3.48), primary education (AOR = 2.04; 95%CI:1.24, 3.38), and secondary education (AOR = 1.53; 95%CI:1.29.2.62), women from households with poorest (AOR = 1.72; 95%CI: 1.16, 2.56), poorer (AOR = 1.62;95% CI:1.09, 2.41), middle (AOR = 1.74;95%CI:1.17, 2.56), and richer (AOR = 1.58;95%CI: 1.08, 2.33) wealth index, women aged 35–39 years (AOR = 1.28;95%CI:1.01, 1.63) and 40–49 years (AOR = 1.78;95%CI:1.28, 2.45) and those from pastoral (AOR = 1.47;95%CI:1.04, 1.93) and agrarian regions (AOR = 1.32;95%CI 1.02, 1.88) had a higher likelihood of having IPV. Of the partner-related factors, women with husbands who drink alcohol (AOR = 2.94; 95%CI: 2.36, 3.42) and secondary educational level (AOR = 1.47; 95%CI 1.02, 2.12) had higher odds of experiencing IPV during pregnancy.
Conclusion
Intimate partner violence during pregnancy is a public health problem in Ethiopia. Therefore, improving the educational status of women and their husbands, improving the economic capacity of women, and promoting the healthy behavior of husbands by reducing the alcohol consumption in those agrarian and pastoral regions of Ethiopia is vital to reduce the magnitude of IPV.
Similar content being viewed by others
Background
Intimate partner violence (IPV) which is defined as acts of physical aggression, sexual coercion, emotional abuse by a current or former partner or spouse [1] against women is the commonest source of violence directed to women [2]. It has three forms such as physical, sexual, and emotional violence [3].
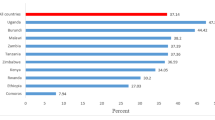
In low-income countries, reported intimate partner violence (IPV) varied widely from less than 5% in Armenia and Comoros to more than 40% in Afghanistan with richer and more empowered women having less IPV [4]. Studies conducted in sub-Saharan African and Asian countries showed an IPV rate ranging from 28% in Madagascar, 74% in Ethiopia, and 57% in India to 87% in Jordan [5]. The evidence from a multi-country study indicated an IPV rate ranging from 18.5 to 75.8%. In sub-Saharan Africa, it is verified that the magnitude of intimate partner violence is higher than non-intimate partner violence [6, 7].
The magnitude of IPV among pregnant women was 33 and 37% in Nigeria [8] and Kenya [9] respectively. In Ethiopia, it varies across different parts of the country ranging from 24.5% in the northwest and southeast [10, 11], 37.5% in the north [12], to 39.81% in the eastern [13] part of Ethiopia.
Intimate partner violence is considered a global problem with serious public health and human rights implications. It affects all the spheres of women’s lives such as self-esteem, productivity, autonomy, capacity to care for themselves and their children, and ability to participate in social activities. Besides, it directly or indirectly leads to serious injury, disability mental disorders, substance use, and even death [6, 14].
Especially for pregnant women, IPV has special concern due to the potential negative impacts for both themselves and their fetuses. It may lead to higher rates of miscarriage, many complications (such as abruption placenta, placenta previa, preeclampsia, gestational diabetes antepartum hemorrhage e.t.c), sexually transmitted infections, and a higher prevalence of mental disorders (such as depression, anxiety, sleep disorders, and eating disorders) [15,16,17,18].
Furthermore, IPV during pregnancy is related with high perinatal and neonatal mortality [19]. Intrauterine growth retardation, preterm delivery, and low birth weight are common neonatal complications which happen as result of pregnancy related violence [20,21,22,23]. Moreover, increased intensity and frequency of pregnancy related violence was reported among women who were victims of violence just before and during pregnancy [24]. Another study found that pregnant abused women had more severe injuries than did nonpregnant abused women [25].
In the previous studies, partner alcohol consumption [9, 26, 27] husband education [9, 27,28,29], women education [27, 28, 30], age of women [31, 32], women decision-making capacity [33], history of IPV [32], place of residence [27] and household resources [34] are significantly associated with intimate partner violence.
Though different studies [10,11,12,13] were conducted in Ethiopia, all of them focus on the specific part of Ethiopia and assess the effect of individual-level factors without considering the context of the community where the women are dwelling and others focus on IPV among reproductive-age women [35, 36].
Although the effect of IPV is superior among pregnant women, there is limited evidence on the magnitude and associated factors of IPV among pregnant women in Ethiopia. Knowing the prevalence of intimate partner violence during pregnancy is the first step for the development and implementation of interventions to prevent and treat sequelae. Therefore, the current study aimed to assess the magnitude and factors associated with IPV among pregnant women in Ethiopia.
Method
Data source and setting
This study used Demographic and Health Survey (DHS) data which were collected using a cross-sectional study design. The DHS collects a wide range of objective and self-reported data with a strong focus on indicators of fertility, reproductive health, maternal and child health, mortality, nutrition, and self-reported health behaviors among adults. Data from DHS facilitate epidemiological research focused on monitoring prevalence, trends, and inequalities. It drew nationally representative samples for the country’s population. A detailed description of the nature of demographic and health survey datasets was published elsewhere [37]. The Ethiopian demographic and health survey is part of the worldwide DHS project. Therefore, the current study was based on data from the fourth Ethiopian demographic and health survey which was conducted in 2016.
Sample size and sampling procedure
To assure national representativeness, the 2016 Ethiopian demographic and health survey (EDHS) employs a stratified two-stage cluster sampling technique. In the first stage, a total of 645 enumeration areas (EAs) that represent the entire country were randomly selected from the sampling frame (i.e. developed from the 2007 census). The second stage is the systematic sampling of households listed in each cluster or EA and interviews are conducted in selected households with target populations (women aged 15–49 and men aged 15–64). A full description of EDHS is published elsewhere [38]. A total of 15,683 reproductive-age women were included in EDHS 2016. Of these, only pregnant women (pregnant at the time of data collection, give birth within the last five years, or had a history of terminated pregnancy) were included in the current study to assess whether they have experienced intimate partner violence during any of their pregnancy. So, the study participants were women aged 15–49 who were selected and interviewed for the domestic violence module and who have ever been pregnant. The sample is extracted as (v044 = 1; selected for domestic violence module) and (v201 > 0: woman had given live birth) or v213 = 1; pregnant at the time of interview) or v228 = 1(woman had history of terminated pregnancy). Therefore, after excluding the missing values the final weighted sample size was 4167 with 640 clusters (EA) (Fig. 1).
Dependent variable
The modified Conflict Tactic Scales of Straus [39] was used to measure intimate partner violence (IPV). Women were asked whether or not they had experienced the acts forwarded by their husband/partner for currently married women and recent husband/partner for previously married women during any of her pregnancies. Then, the women’s self-reported responses to questions were used to decide the women’s IPV experience (Table 1). Thus, respondents were categorized as having experienced IPV if they reported experiencing at least one act of IPV during pregnancy.
Independent variables
Educational status of women (no formal education, primary, secondary, higher education), age of women [4, 15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49], maternal occupation (working, not working), husband education (no formal education, primary, secondary, higher education), husband occupation (not working, working), husband drinking alcohol (yes, no), wealth status (poorest, poorer, middle, richer and richest), media exposure (yes, no), sex of household head (male, female) were considered as individual-level variables.
Of the community level variables, place of residence (urban, rural), and region (city dwellers, pastoral, agrarian), were directly accessible from EDHS dataset. However, community poverty level (low, high), community illiteracy level (low, high), and community media exposure (low, high) were aggregated from individual-level characteristics at the cluster level. The distribution of the proportion values computed for each community was checked by using the histogram. Therefore, for dichotomization, mean and median values were used for normaly distributed and skewed proportions respectively.
Multilevel binary logistic regression analysis
In large surveys, the clustering sampling approach commonly leads to correlation among the observations. This dependence among observations often comes from several levels of the hierarchy due to the multi-stage sampling scheme employed. In this case, applying traditional single-level statistical models leads to biased parameter estimation [40]. Therefore, to draw appropriate inferences and conclusions from hierarchical large survey data, we applied multilevel modeling techniques. Since the outcome variable is dichotomous, multilevel binary logistic regression analysis is employed for the current study.
Thus, the Intraclass Correlation Coefficient (ICC), and Proportional Change in Variance (PCV), were conducted to assess the significance of variability in experiencing IPV across the communities [41]. The proportional change in variance is calculated as;
Where; where VA = variance of the initial model, and VB = variance of the model with more terms.
A total of four models were fitted; the null model (with no predictors), model II (adjusted for individual-level variables only), model III (adjusted for community-level variables only), and model IV (model adjustment for both individual and community-level variables simultaneously) were fitted. The deviance was used for model comparison. Finally adjusted odds ratio (AOR) with a 95% confidence interval (CI) was reported for the best-fitted model.
Results
Sociodemographic characteristics of study participants
This study included a total of 4167 (weighted) married pregnant women. Nearly two-thirds (65.46%) of study participants had no occupation. About 64 and 42% of pregnant women and their husbands had no formal education respectively. The majority (21.37) of the participants were from households with the richest wealth quantile. Nearly 31% of women had a husband who drinks alcohol and about 47% of study participants were exposed to media. Looking at the community-level characteristics, the majority of participants (82.74%) were rural dwellers and more than half (52%) of them were from agrarian regions. Above three- fourth (80.64%) of the study participants were from communities with high poverty level. About 45% of pregnant women were from communities with high illiteracy level (Table 2).
The magnitude of different types of IPV directed to pregnant women
Table 3 presented the weighted magnitude of different forms of intimate partner violence inflicted on pregnant women with 95%CI. Of the variants of IPV, pregnant women were exposed to emotional violence (24%) most frequently. The least prevalent form of IPV was sexual violence. The overall (sexual, physical, or emotional) magnitude of IPV among pregnant women was 28.74 (95% CI 27.38, 30.13).
Factors associated with intimate partner violence
In the null model the community-level variance [country variance = 0.73; standard error (SE) = 0.10; P-value = 0.001], was statistically significant which indicates that there is significant variation in experiencing IPV during pregnancy across communities. This was further supported by the intracluster correlation coefficient which showed that 18.70% of the variation of IPV against pregnant women was attributed to community-level factors.
Moreover, the final model (model IV) indicates that about 45.20% of the variation of IPV directed towards pregnant women is explained by both the individual and community-level factors. The model fitness was assessed by using deviance. Consequently, Model IV was found to be the best-fitted model since it has the lowest deviance value (Table 4).
Regarding the fixed effects, maternal education, maternal age, wealth index, husband education, husband drinking alcohol, and region were significantly associated with intimate partner violence.
The odds of experiencing intimate partner violence among pregnant women with no education, primary education, and secondary education was 2.07 (AOR = 2.07; 95%CI:1.23, 3.48), 2.04 (AOR = 2.04; 95%CI:1.24, 3.38), and 1.53 (AOR = 1.53; 95%CI:1.29.2.62) respectively times higher as compared to those who had higher education. Besides, pregnant women whose husband has primary education has 47% (AOR = 1.47; 95%CI 1.02, 2.12) increased odds of experiencing IPV as compared to women who had a husband with higher education. The likelihood of experiencing IPV among women whose husband drinks alcohol was nearly three folds (AOR = 2.94;95%CI:2.36, 3.42) higher as compared to their counterparts. Regarding wealth index, the odds of experiencing IPV among pregnant women from the poorest, poorer, middle, and richer households was 1.72 (AOR = 1.72; 95%CI: 1.16, 2.56), 1.62 (AOR = 1.62;95% CI:1.09, 2.41), 1.74 (AOR = 1.74;95%CI:1.17, 2.56), and 1.58 (AOR = 1.58;95%CI: 1.08, 2.33) respectively times higher as compared to those from households with richest wealth quantile. The likelihood of experiencing IPV among pregnant women with age category 35–39 and 40–49 was 1.28 (AOR = 1.28;95%CI:1.01, 1.63) and 1.78(AOR = 1.78;95%CI:1.28, 2.45) respectively times higher as compared to women under 15–24 age category. Looking at the region, women from pastoral and agrarian regions had 47% (AOR = 1.47;95%CI:1.04, 1.93) and 32% (AOR = 1.32;95%CI 1.02, 1.88) increased odds of experiencing intimate partner violence respectively as compared to city dwellers (Table 4).
Discussion
The overall magnitude of intimate partner violence among pregnant women was 28.74 (95% CI 27.38, 30.13) with emotional violence at the higher occurrence. Educational status of women and husband, alcohol consumption of husband, age of women, wealth index, and region were significantly associated with experiencing IPV during pregnancy.
The overall magnitude of IPV in the current study was lower than the findings in Nigeria [8], Jordan [42], Kenya [9], Egypt [43], and Portugal [44] and previous Ethiopian studies that were done in Jimma [45] and Tigray [46]. But, it was higher than that of previous studies from Ethiopia that were conducted in the northwest [10] and southern [47] Ethiopia. The lower magnitude of IPV in the current study may be attributed to the differences in culture, social norms, and implementation of laws that prevent violence against women [48]. For example, Ethiopian society is highly patriarchal thus women often feel humiliated and ashamed to disclose violence (most commonly sexual violence) due to fear of negative responses from others within their society because of cultural consequences [49, 50]. Besides, the questions used to assess IPV are culturally sensitive. So, the respondents may not answer such questions honestly. This might lead to underreporting and then low IPV [51, 52]. Furthermore, the difference in gender equality might also contribute to the difference in magnitude of experiencing [53].
This study revealed the higher odds of IPV among women from economically poor households as compared to women from richer households which is supported by the finding in Bangladesh [54]. This might be because women in Ethiopia especially with poor economic status may have minimal access and freedom to utilize the financial resources without consulting their partners which may in turn lead to conflict [55]. In countries like Ethiopia, social responsibility for raising children is vested on women. Therefore, women may be forced to admit the violence from their partner in order not to be separated to minimize the suffering of their children [56].
The odds of experiencing IPV among women with low educational status was higher as compared to those women with secondary and higher education. This finding is consistent with the study in Rwanda [29] and other developing countries [27, 28]. This might be since uneducated pregnant women may have less power to discuss with their partners to minimize any household disputes. It is documented that the likelihood of experiencing violence during pregnancy is negatively affected by low levels of education and lack of decision-making power [57].
Similarly,husband education was also significantly associated with IPV during pregnancy. Women who had a husband with a secondary education level had nearly 50% increased odds of experiencing IPV as compared to those with a husband with higher education. This result is in line with previous studies [9, 27]. It is known fact that education is a source of information and it is a tool to shape a positive behavioral changes. So, uneducated partners may not give freedom to their wives which is commonly driven by cultural beliefs. This study also highlighted another partner-related factor, alcohol consumption. Consistent with the previous findings [9, 26, 29], the likelihood of IPV among women who had a partner that drink alcohol was nearly three folds higher as compared to their counter parts. This might be due to the fact that alcohol facilitates to have violent behaviors [58]. Besides, alcohol use has been associated with having multiple sexual partners, an issue that may also lead to conflict [59].
Age is a significant predictor of IPV during pregnancy. Aged women have higher odds of experiencing IPV as compared to younger ones. This finding is also supported by previous studies in Nigeria [31] and South Africa [32]. This could be because older women might be more likely to report IPV. After all, younger women in Ethiopia are often expected to be submissive, quiet, disciplined, and loyal to their husbands and hence may have a lower probability of reporting IPV.
Similarly, the region was an important predictor of IPV. Women from agrarian and pastoral regions had higher odds of experiencing IPV as compared to city dwellers. The women in urban areas are more autonomous, educated, and well-informed about gender equality. Consequently, they could have confidence in decision-making in the household [60].
The strengths of this study were; first, it was conducted using data from a large national survey which provides adequate power to detect the true effect of the independent variables. Second, the sampling weight was applied during the analysis to get reliable estimates and standard errors. As a limitation, since the study used cross-sectional data, a causal relationship between IPV and the identified independent variables cannot be established.
Conclusion
Intimate partner violence during pregnancy is a public health problem in Ethiopia. The educational status of women and their husbands, wealth index, age of women, alcohol consumption of husband, and region were significantly associated with intimate partner violence during pregnancy. Therefore, improving the educational status of women and their husbands, improving the economic capacity of women, and promoting the healthy behavior of husbands by reducing alcohol consumption is vital to reduce the magnitude of IPV and its consequences in Ethiopia. Besides, minimizing dominant patriarchal ideologies which privilege heterosexual marriage through cultural and religious connections could also play a central role in reducing IPV. In general, the gender issue is prioritized as an essential aspect in accelerating the united nation’s 2030 global agenda [61]. Ethiopia had also considered gender equality as a transformative policy [62] Therefore, the findings in this study could have a positive effect towards achieving the SDG goals in Ethiopia as it provides a piece of evidence for policymakers and program designers to make an informed decision.
Availability of data and materials
The datasets we used for this study were publicly available at http://www.dhsprogram.com. Website.
Abbreviations
- CSA:
-
Central Statistical Agency
- DHS:
-
Demographic and health survey
- EAs:
-
Enumeration Areas
- EDHS:
-
Ethiopian Demographic and Health Survey
- IPV:
-
Intimate partner violence
- WHO:
-
World Health Organization
References
Heise L, Garcia-Moreno C. Violence by intimate partners. In: Krug EG, Dahlberg LL, Mercy JA, Lozano ABZR, editors. World report on violence and health, İçinde. Geneva: World Health Organization (WHO); 2002. p. 87–113.
García-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts C. WHO multi-country study on women’s health and domestic violence against women: World Health Organization; 2005.
Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. 2002;360(9339):1083–8.
Coll CV, Ewerling F, García-Moreno C, Hellwig F, Barros AJ. Intimate partner violence in 46 low-income and middle-income countries: an appraisal of the most vulnerable groups of women using national health surveys. BMJ Glob Health. 2020;5(1):e002208.
Uthman OA, Lawoko S, Moradi T. Factors associated with attitudes towards intimate partner violence against women: a comparative analysis of 17 sub-Saharan countries. BMC Int Health Hum Rights. 2009;9(1):1–15.
Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women's health and domestic violence. Lancet. 2006;368(9543):1260–9.
Muluneh MD, Stulz V, Francis L, Agho K. Gender based violence against women in sub-Saharan Africa: a systematic review and meta-analysis of cross-sectional studies. Int J Environ Res Public Health. 2020;17(3):903.
Oche OM, Adamu H, Abubakar A, Aliyu MS, Dogondaji AS. Intimate partner violence in pregnancy: knowledge and experiences of pregnant women and controlling behavior of male partners in Sokoto, Northwest Nigeria. Int J Reprod Med. 2020;2020.
Makayoto LA, Omolo J, Kamweya AM, Harder VS, Mutai J. Prevalence and associated factors of intimate partner violence among pregnant women attending Kisumu District hospital, Kenya. Matern Child Health J. 2013;17(3):441–7.
Bifftu BB, Dachew BA, Tadesse Tiruneh B, Zewoldie AZ. Domestic violence among pregnant mothers in Northwest Ethiopia: prevalence and associated factors. Adv Publ Health. 2017;2017.
Tulu C, Kiflu E, Hirkisa D, Kedir Z, Abdurahim L, Ganfure G. Prevalence of domestic violence and associated factors among antenatal care attending women at robe hospital, Southeast Ethiopia. Clin Mother Child Health. 2019;16:337.
Alebel A, Kibret GD, Wagnew F, Tesema C, Ferede A, Petrucka P, et al. Intimate partner violence and associated factors among pregnant women in Ethiopia: a systematic review and meta-analysis. Reprod Health. 2018;15(1):1–12.
Musa A, Chojenta C, Loxton D. High rate of partner violence during pregnancy in eastern Ethiopia: findings from a facility-based study. PLoS One. 2020;15(6):e0233907.
Pourasadi M, Hashemi M. Phenomenon of divorce and custody of children after separation; 2012.
Ahmed S, Koenig MA, Stephenson R. Effects of domestic violence on perinatal and early-childhood mortality: evidence from North India. Am J Public Health. 2006;96(8):1423–8.
Boy A, Salihu HM. Intimate partner violence and birth outcomes: a systematic review. Int J Fertil Women's Med. 2004;49(4):159–64.
Campbell JC, Baty M, Ghandour RM, Stockman JK, Francisco L, Wagman J. The intersection of intimate partner violence against women and HIV/AIDS: a review. Int J Inj Control Saf Promot. 2008;15(4):221–31.
Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet. 2004;363(9419):1415–21.
Mbadugha E. Intimate partner violence and sexual violence against women: any end in sight? Int J Med Biomed Res. 2016;5(1):9–18.
Linos N, Slopen N, Subramanian S, Berkman L, Kawachi I. Influence of community social norms on spousal violence: a population-based multilevel study of Nigerian women. Am J Public Health. 2013;103(1):148–55.
Nunes MAA, Camey S, Ferri CP, Manzolli P, Manenti CN, Schmidt MI. Violence during pregnancy and newborn outcomes: a cohort study in a disadvantaged population in Brazil. Eur J Pub Health. 2011;21(1):92–7.
Vo TM, Tran VT, Cuu TN, Do TT, Le TM. Domestic violence and its association with pre-term or low birthweight delivery in Vietnam. Int J Women's Health. 2019;11:501.
Kaye DK, Mirembe FM, Bantebya G, Johansson A, Ekstrom AM. Domestic violence during pregnancy and risk of low birthweight and maternal complications: a prospective cohort study at Mulago hospital, Uganda. Tropical Med Int Health. 2006;11(10):1576–84.
Helton AS, Snodgrass FG. Battering during pregnancy: intervention strategies. Birth. 1987;14(3):142–7.
Fagan JA, Stewart DK, Hansen KV. Violent men or violent husbands? Background factors and situational correlates. The dark side of families. Curr Fam Viol Res. 1983;49:68.
Taillieu TL, Brownridge DA. Violence against pregnant women: prevalence, patterns, risk factors, theories, and directions for future research. Aggress Violent Behav. 2010;15(1):14–35.
Gebrezgi BH, Badi MB, Cherkose EA, Weldehaweria NB. Factors associated with intimate partner physical violence among women attending antenatal care in Shire Endaselassie town, Tigray, northern Ethiopia: a cross-sectional study, July 2015. Reprod Health. 2017;14(1):1–10.
Nasir K, Hyder AA. Violence against pregnant women in developing countries: review of evidence. Eur J Public Health. 2003;13(2):105–7.
Ntaganira J, Muula AS, Masaisa F, Dusabeyezu F, Siziya S, Rudatsikira E. Intimate partner violence among pregnant women in Rwanda. BMC Womens Health. 2008;8(1):1–7.
Mahenge B, Likindikoki S, Stöckl H, Mbwambo J. Intimate partner violence during pregnancy and associated mental health symptoms among pregnant women in T anzania: a cross-sectional study. BJOG Int J Obstet Gynaecol. 2013;120(8):940–7.
Orpin J, Papadopoulos C, Puthussery S. The prevalence of domestic violence among pregnant women in Nigeria: a systematic review. Trauma Violence Abuse. 2020;21(1):3–15.
Groves AK, Moodley D, McNaughton-Reyes L, Martin SL, Foshee V, Maman S. Prevalence, rates and correlates of intimate partner violence among south African women during pregnancy and the postpartum period. Matern Child Health J. 2015;19(3):487–95.
Ahinkorah BO, Dickson KS, Seidu A-A. Women decision-making capacity and intimate partner violence among women in sub-Saharan Africa. Arch Publ Health. 2018;76(1):1–10.
Cools S, Kotsadam A. Resources and intimate partner violence in sub-Saharan Africa. World Dev. 2017;95:211–30.
Tiruye TY, Harris ML, Chojenta C, Holliday E, Loxton D. Determinants of intimate partner violence against women in Ethiopia: a multi-level analysis. PLoS One. 2020;15(4):e0232217.
Chernet AG, Cherie KT. Prevalence of intimate partner violence against women and associated factors in Ethiopia. BMC Womens Health. 2020;20(1):1–7.
Corsi DJ, Neuman M, Finlay JE, Subramanian S. Demographic and health surveys: a profile. Int J Epidemiol. 2012;41(6):1602–13.
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia demographic and health survey. Addis Ababa and Rockville: CSA and ICF; 2016.
Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2) development and preliminary psychometric data. J Fam Issues. 1996;17(3):283–316.
Snijders TA, Bosker RJ. Multilevel analysis: an introduction to basic and advanced multilevel modeling: sage; 2011.
Merlo J, Yang M, Chaix B, Lynch J, Råstam L. A brief conceptual tutorial on multilevel analysis in social epidemiology: investigating contextual phenomena in different groups of people. J Epidemiol Community Health. 2005;59(9):729–36.
Oweis A, Gharaibeh M, Al-Natour A, Froelicher E. Violence against women: unveiling the suffering of women with a low income in Jordan. J Transcult Nurs. 2009;20(1):69–76.
Ibrahim Z, Sayed Ahmed W, El-Hamid S, Hagras A. Intimate partner violence among Egyptian pregnant women: incidence, risk factors, and adverse maternal and fetal outcomes. Clin Exp Obstet Gynecol. 2015;42(2):212–9.
Almeida FSJ, Coutinho EC, Duarte JC, Chaves CMB, Nelas PAB, Amaral OP, et al. Domestic violence in pregnancy: prevalence and characteristics of the pregnant woman. J Clin Nurs. 2017;26(15–16):2417–25.
Abate BA, Wossen BA, Degfie TT. Determinants of intimate partner violence during pregnancy among married women in Abay Chomen district, Western Ethiopia: a community based cross sectional study. BMC Womens Health. 2016;16(1):1–8.
Berhanie E, Gebregziabher D, Berihu H, Gerezgiher A, Kidane G. Intimate partner violence during pregnancy and adverse birth outcomes: a case-control study. Reprod Health. 2019;16(1):1–9.
Belay S, Astatkie A, Emmelin M, Hinderaker SG. Intimate partner violence and maternal depression during pregnancy: a community-based cross-sectional study in Ethiopia. PLoS One. 2019;14(7):e0220003.
Organization WH. Violence prevention: the evidence; 2010.
Jacques-Tiura AJ, Tkatch R, Abbey A, Wegner R. Disclosure of sexual assault: characteristics and implications for posttraumatic stress symptoms among African American and Caucasian survivors. J Trauma Dissoc. 2010;11(2):174–92.
Kennedy AC, Prock KA. “I still feel like I am not normal”: a review of the role of stigma and stigmatization among female survivors of child sexual abuse, sexual assault, and intimate partner violence. Trauma Violence Abuse. 2018;19(5):512–27.
Tang N, Bensman L, Hatfield E. Culture and sexual self-disclosure in intimate relationships; 2013.
Kershner M, Anderson JE. Barriers to disclosure of abuse among rural women. Minn Med. 2002;85(3):32–7.
Archer J. Cross-cultural differences in physical aggression between partners: a social-role analysis. Personal Soc Psychol Rev. 2006;10(2):133–53.
Sambisa W, Angeles G, Lance PM, Naved RT, Curtis SL. Physical and sexual abuse of wives in urban Bangladesh: husbands' reports. Studies in family planning. 2010;41(3):165-78.
Nigatu D, Gebremariam A, Abera M, Setegn T, Deribe K. Factors associated with women’s autonomy regarding maternal and child health care utilization in bale zone: a community based cross-sectional study. BMC Womens Health. 2014;14(1):1–9.
Fawole OI, Aderonmu AL, Fawole AO. Intimate partner abuse: wife beating among civil servants in Ibadan, Nigeria. Afr J Reprod Health. 2005:54–64.
Abeya SG, Afework MF, Yalew AW. Intimate partner violence against women in western Ethiopia: prevalence, patterns, and associated factors. BMC Public Health. 2011;11(1):1–18.
Bushman BJ, Cooper HM. Effects of alcohol on human aggression: an intergrative research review. Psychol Bull. 1990;107(3):341.
Weiser SD, Leiter K, Heisler M, McFarland W, Percy-de Korte F, DeMonner SM, et al. A population-based study on alcohol and high-risk sexual behaviors in Botswana. PLoS Med. 2006;3(10):e392.
Bradshaw S. Women’s decision-making in rural and urban households in Nicaragua: the influence of income and ideology. Environ Urban. 2013;25(1):81–94.
Hepp P, Somerville C, Borisch B. Accelerating the united Nation's 2030 global agenda: why prioritization of the gender goal is essential. Global Policy. 2019;10(4):677–85.
Bekana DM. Policies of gender equality in Ethiopia: the transformative perspective. Int J Public Adm. 2020;43(4):312–25.
Acknowledgments
The authors would like to thank measure DHS for their permission to access the EDHS datasets.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
AML: Conceptualization, data curation, formal analysis, investigation, methodology, resources, software, validation, visualization, writing – original draft, Writing – review & editing. AZA and HGA: Data curation, formal analysis, investigation, methodology, resources, software, validation, visualization, writing – original draft, Writing – review & editing. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
A public domain survey data sets, which are freely available online at www.measuredhs.com website was used for this study. But to access and use the data we obtained permission and approval from Measure DHS through the online request. We also confirm that all methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
Both authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liyew, A.M., Alem, A.Z. & Ayalew, H.G. Magnitude and factors associated with intimate partner violence against pregnant women in Ethiopia: a multilevel analysis of 2016 Ethiopian demographic and health survey. BMC Public Health 22, 284 (2022). https://doi.org/10.1186/s12889-022-12720-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-12720-0