Abstract
Background
Strategies to control coronavirus 2019 disease (COVID-19) have often been based on preliminary and limited data and have tended to be slow to evolve as new evidence emerges. Yet knowledge about COVID-19 has grown exponentially, and the expanding rollout of vaccines presents further opportunity to reassess the response to the pandemic more broadly.
Main text
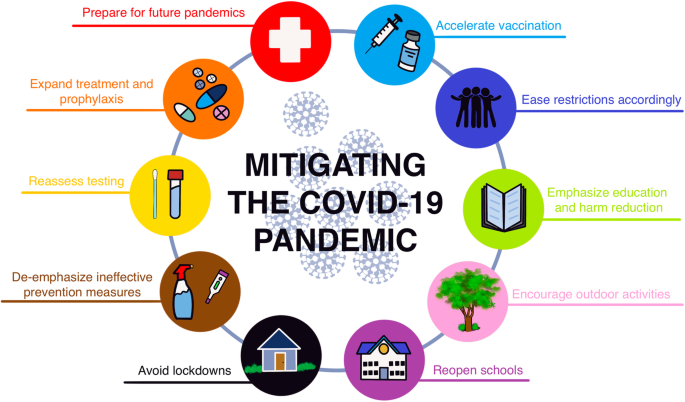
We review the latest evidence concerning 10 key COVID-19 policy and strategic areas, specifically addressing: 1) the expansion of equitable vaccine distribution, 2) the need to ease restrictions as hospitalization and mortality rates eventually fall, 3) the advantages of emphasizing educational and harm reduction approaches over coercive and punitive measures, 4) the need to encourage outdoor activities, 5) the imperative to reopen schools, 6) the far-reaching and long-term economic and psychosocial consequences of sustained lockdowns, 7) the excessive focus on surface disinfection and other ineffective measures, 8) the importance of reassessing testing policies and practices, 9) the need for increasing access to outpatient therapies and prophylactics, and 10) the necessity to better prepare for future pandemics.
Conclusions
While remarkably effective vaccines have engendered great hope, some widely held assumptions underlying current policy approaches call for an evidence-based reassessment. COVID-19 will require ongoing mitigation for the foreseeable future as it transforms from a pandemic into an endemic infection, but maintaining a constant state of emergency is not viable. A more realistic public health approach is to adjust current mitigation goals to be more data-driven and to minimize unintended harms associated with unfocused or ineffective control efforts. Based on the latest evidence, we therefore present recommendations for refining 10 key policy areas, and for applying lessons learned from COVID-19 to prevent and prepare for future pandemics.
Similar content being viewed by others
Background
The coronavirus disease 2019 (COVID-19) pandemic has caused devastating loss of life and disrupted healthcare systems and daily life globally. By late October 2021, over 245 million confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection cases and over 4.9 million related deaths had been reported globally [1]. As the international vaccination rollout continues to expand [2], we call for a reexamination of existing mitigation approaches to adapt to emerging evidence on effectiveness and to minimize unintended consequences. COVID-19 vaccines have proven to be highly effective at preventing severe disease and mortality and, to a lesser extent, milder symptomatic and asymptomatic cases. While vaccination has ushered in great hope, the time is ripe to revisit the assumptions underlying some current interventions and to implement more context-sensitive, evidence-based policies. Accordingly, we review the available evidence regarding 10 key policy areas for which we recommend modification or refinement (Fig. 1).
One limitation of this review is the paucity of data from randomized controlled trials (RCTs) to measure the efficacy and effectiveness of COVID-19 prevention interventions. Aside from vaccines and therapeutics [3, 4], the only exceptions to date are two RCTs of masks [5, 6]. A trial conducted in Denmark found no statistically significant difference in infection rates between the group provided with and urged to wear surgical masks and a control group [5]. Meanwhile, a cluster RCT in Bangladesh found a statistically significant 9% reduction in symptomatic seroprevalence in villages where surgical masks were provided and their use promoted [6]. In this study, no significant decrease in symptomatic seroprevalence was observed in villages where cloth masks were promoted. Moreover, some public health interventions can be difficult or even impossible to definitely study with RCTs [7–10]. We therefore rely mainly on the best available observational data, despite limitations and potential biases, to suggest refinements to current approaches and policies.
1: Accelerate vaccination rollout
Even with the continuing emergence of viral variants, widespread vaccination remains the quickest and most powerful way to reduce the toll from COVID-19 and continue returning toward a greater sense of normality. Maximizing global vaccine production and equitable distribution must be the highest priority, with innovative mechanisms of financing and licensing production as required. The wealthier countries should largely pay for this ongoing effort as a humanitarian imperative as well as from enlightened self-interest. This could be modeled on the experience with AIDS, in which antiretroviral drugs are provided to poorer countries by bilateral and multilateral donors at discounted prices and/or through low-cost international generic production via waived patents [11, 12], while pharmaceutical companies continue to benefit financially in higher-income countries. Many countries have recently made encouraging promises in this regard, including at the June 2021 G7 Summit [13], but such promises will need to be kept if not exceeded.
Since vaccine supplies are still not adequate to meet the global population’s needs, they must be used as strategically and efficiently as possible. Such strategies include prioritizing vulnerable populations and healthcare workers (HCWs), and delaying doses for those with previous COVID-19 until those without prior immunity are vaccinated. Delaying the second dose of 2-dose vaccines for longer than the interval used in clinical trials may increase overall public health benefit by maximizing coverage with first doses more quickly and may also lead to greater immunogenicity [14–19]. The US Centers for Disease Control and Prevention (CDC) recommended that the second dose can be given up to 6 weeks following the first one [20], but implementing an even longer duration between doses, when necessary, is consistent with a population-health perspective. Several countries, such as Canada, have taken this approach of extending the duration between doses. Moreover, persons known to have been previously infected may defer vaccination for 6 months or perhaps even longer post-infection [21, 22], and when they get vaccinated, appear to require only 1 dose of a 2-dose vaccine regimen [23–26].
Such approaches will require careful implementation and messaging to minimize the potential risk of persons not getting vaccinated in the unconfirmed belief that they have already been infected, or not returning for a second dose in the mistaken belief that they are fully protected by a single dose. Other challenges facing some countries involve choosing between rapid application of less effective vaccines or waiting for the availability of better ones. Generally, those approaches that offer the most people some protection as quickly as possible should be followed. Furthermore, higher-income countries should refrain from distributing booster shots more broadly or frequently than necessary (e.g., for the immunocompetent general population), as this appears currently unjustified both scientifically and ethically [27, 28]. In late October 2021, it was estimated that globally about three times as many booster shots were being given per day compared to the total number of vaccine shots administered daily in lower-income countries [29].
Vaccination and other mitigation efforts must focus on protecting the most vulnerable through prioritizing the elderly, HCWs, and other essential workers. Additional criteria for determining which persons should be prioritized due to existing medical conditions must be evidence-based. Cardiometabolic comorbidities such as diabetes, chronic obstructive pulmonary disease, hypertension, and obesity are known risk factors strongly associated with increased COVID-19 severity and mortality [30–35]. But asthma, for example, turns out not to be a risk factor (and is probably even partially protective against death and other serious COVID-19 outcomes) [36–41]. In certain situations and particularly among groups at the highest risk of disease or exposure, vaccination mandates can be considered, e.g., for working in hospitals, nursing homes, prisons, or other high-risk settings [42, 43]. While we applaud the US and other countries for having joined the World Health Organization (WHO) COVAX Initiative, we urge high-income countries to also unilaterally deploy their soon-to-expire as well as other doses overseas and to join the WHO COVID-19 Technology Access Pool, which would allow other countries to produce patented vaccines, thereby expanding their availability in low and middle-income countries [11]. International governance of vaccine distribution is essential to address vaccine inequity and to maximize outcomes globally.
2: Gradually ease restrictions as vaccination expands
Accumulating real-world evidence is documenting the large extent to which COVID-19 vaccines reduce severe disease, hospitalizations, and mortality. Although asymptomatic infection and symptomatic disease were both greatly reduced by the vaccines in the context of the Alpha variant and earlier D614G mutants [18, 19, 44–53], more recent data during the ascendency of the Delta variant indicate reduced effectiveness against asymptomatic or mild infections [54–60]. However, the vaccine-induced protection against severe disease from the Delta variant appears to be remarkably intact across multiple settings, at over 90% [55, 59]. Declines in antibodies are expected over time following vaccination, but cellular memory (which enhances antibody production and protects against severe disease) appears to be much more durable [61, 62].
Once vaccination has been made widely and equitably available and rates of hospitalization and mortality eventually fall, it becomes untenable to expect the vaccinated to follow all current restrictions imposed mainly to protect those who decline vaccination. The same can be said regarding immunity following infection. Given the rarity of reinfection [7, 22, 63] and the duration of immunity post-infection (at least 6–12 months ) [21, 63–68], those with evidence of prior infection appear to be as immune as those who have been vaccinated [69–72].
Mass vaccination will accelerate achieving much greater pandemic control, allowing measures such as masking and physical distancing to be gradually relaxed [7]. It is critical to acknowledge the physical, psychological, sociopolitical, and other costs of enforcing restrictions and to begin easing them as hospitalization and death rates fall substantially, while remaining vigilant and ready to revisit such decisions if circumstances change significantly.
3: Emphasize education and harm reduction approaches over coercive and punitive measures
“Abstinence-only” approaches have not worked for AIDS or teen pregnancy prevention [73], nor have absolutist approaches worked well for preventing SARS-CoV-2 [74, 75]. Instead, prevention measures should be founded on the provision of accurate information, sensitively communicated, and informed by harm reduction approaches that are more effective and sustainable in the longer term [7, 74–76]. Harm reduction involves informing people how to assess and mitigate risk, while acknowledging the real-world conditions that may lead some persons to take calculated risks. One example of a successful mitigation campaign (prior to vaccines) is that of Japan’s 3 Cs, which generally did not shut down society, but instead advised the public to avoid close, sustained interactions in crowded enclosed spaces [77]. Importantly, educating and motivating the public to adopt effective precautions, including vaccination, as opposed to coercive or punitive measures (e.g., shaming, fines or imprisonment, and even police violence) will be more effective and will help alleviate pandemic response fatigue [7, 78–80]. Accordingly, any restrictions and mandates, including vaccinations passports [81–83], should focus on high-risk situations and consider a number of scientific and ethical questions. Most importantly, COVID-19 measures should be formulated and reassessed based on the latest information, levels of ongoing threat, and resource availability. As mentioned above, vaccine mandates should be carefully focused and should take into account prior SARS-CoV-2 infection [22].
4: Encourage outdoor activities
Current evidence on SARS-CoV-2 transmission dynamics must inform policy recommendations for mitigation strategies and restrictions [84]. Unfortunately, lower-risk activities, especially those conducted in outdoor environments (e.g., parks, beaches, hiking trails, playgrounds), have often been discouraged or even prohibited [85–90]. The risk of SARS-CoV-2 transmission outdoors is vastly lower than indoors, with most studies finding the proportion of new cases attributable to outdoor exposure to be < 1% [7, 42, 91–94]. Policies should reflect this enormous difference in risk, including allowing access to outdoor spaces even during periods of severe restrictions and reserving mask mandates for indoor (and very crowded outdoor) situations [7], as recommended by the WHO and CDC [95–97]. Strongly encouraging outdoor activities and including nuance in public health recommendations (such as discouraging outdoor gatherings from leading to crowded indoor situations) is more consistent with the previously discussed harm reduction-based approaches [7, 98]. When weather or other factors preclude holding activities outdoors, windows should be kept open whenever possible, including in shared vehicles [99], and air ventilation (at least 4 air exchanges per hour) should be ensured to reduce the risk of transmission [100–102].
5: Reopen schools now
COVID-19 has caused by far the largest disruption to learning in recent history [103]. As the pandemic has unfolded, there is mounting evidence that the harm of keeping schools closed dwarfs any public health benefits [41, 104, 105]. By early 2020, most kindergarten-to-grade 12 (K-12) schools worldwide had closed for in-person instruction, and many remain shuttered over a year later [104, 106–109]. As of September 2021, based on United Nations Educational, Scientific and Cultural Organization (UNESCO) data [109], over 100 million students remained affected and 18 countries still had nationwide closures. There is no good substitute for in-person schooling [108]. Remote learning further exacerbates inequities, especially among communities with low resources, not only related to education but also to safety, wellbeing, social support, and nutrition [105, 108, 110–112].
Schools have not been shown to be major drivers of SARS-CoV-2 transmission, when studied in a variety of settings employing a range of mitigation strategies and intensity [106, 107, 113, 114]. However, their prolonged closure have had disastrous academic, psychosocial, and other harmful consequences on children, including access to essential services, especially in lower-income populations [41, 111, 115, 116]. Furthermore, contact tracing studies worldwide have found children are less likely to infect adults or other children, and that most SARS-CoV-2 infections among children are mild and are contracted at home or in the community, not at school [106, 107, 117–119].
In the US state of North Carolina prior to vaccine availability, 11 school districts (many in regions with high SARS-CoV-2 incidence) implemented in-person instruction accompanied by mitigation plans, for > 90,000 children over 9 weeks [117]. Across the 11 school districts, there were 773 community-acquired SARS-CoV-2 infections documented by reverse transcriptase-polymerase chain reaction (RT-PCR) testing, of which only 32 were identified as secondary cases, with no cases of within-school transmission from children to teachers or other adults. Among 17 US schools in rural Wisconsin also conducting in-person learning, with a range of precautions, SARS-CoV-2 incidence among students, teachers, and other staff members was lower than in the surrounding communities overall [118]. During 13 weeks in late 2020, 191 cases were identified among students and staff, of which only 7 (3.7%) cases (all among students) were traced to in-school transmission. In Sweden, where schools generally remained open (and masks have not been required) [120, 121], deaths of children aged 1–16 years were statistically similar in the 4 months before versus after COVID-19 arrived, and intensive care unit admission rates for teachers were comparable to those for other occupations [122]. Many other investigations, such as one among children aged 0 to 19 years in childcare facilities and schools in Baden-Württemberg, Germany, after the reopening of schools in May 2020, have also suggested that child-to-child transmission in school settings is uncommon [123]. To the extent that in-school transmission is an issue, especially given the continuing emergence of highly transmissible variants (e.g., Delta), vaccinating school staff is likely the most effective way to protect those at risk [124–126].
Also, after reviewing data indicating that 3 ft of physical distancing is sufficient [127], in March 2021 the CDC modified their guidelines accordingly, at least for elementary school settings [128]. A large-scale CDC study, comparing schools that mandated various interventions in late 2020 with ones that did not, found that while improving ventilation and requiring teachers and staff members to wear masks was associated with reduced SARS-CoV-2 incidence in schools, mandating students to wear masks was not [129]. Masking guidelines for children from major public health organizations differ, which has generated confusion. For instance, the CDC currently recommends that all children over age 2 wear masks indoors, while the WHO mask guidance applies to children over age 5, with a caveat that benefits from mask mandates at school may not outweigh the potential academic and psychosocial harms [130]. Despite the inconsistent data and guidelines, student masking in communities where rates of hospitalization and death remain high may be useful [113], if for no other reason than to help maintain the necessary consensus to keep schools open.
The emergence of variants does not warrant closing or delaying the reopening of schools unless compelling evidence unexpectedly indicates that a new mutation affects children in some substantially new way [131]. Reassuring data from high schools [106, 107, 117, 118, 122, 123] suggest that in-person classes also can be safely conducted in colleges, especially if combined with interventions to prevent outside-the-classroom transmission. As endorsed by the United Nations Children’s Fund (UNICEF) [132], no effort should be spared to keep students in classes, and closing schools should be a measure of last resort.
6: Avoid lockdowns
The cumulative evidence suggests that “sledge-hammer” lockdown approaches, such as the closing of all non-essential workplaces and schools, should be avoided in favor of more effective, carefully targeted “scalpel” public health strategies [7, 78, 133, 134]. Indiscriminate lockdowns have had far-reaching unintended consequences, disproportionately affecting socioeconomically disadvantaged and vulnerable populations. Other consequences include alarming increases in mental health problems (e.g., depression, anxiety, and social isolation), drug overdose, domestic violence, child abuse, weight gain, abuse by law enforcement in some places, and discontinuation of non-COVID-19 clinical services and prevention programs [41, 78, 110, 115, 134–139]. While substantial evidence highlights the deleterious impact of sustained lockdowns, the direct impact of SARS-CoV-2 transmission on disease outcomes, healthcare systems, and employment, particularly in the context of huge inequity, can also produce many of the same negative effects, even in the absence of official lockdowns [140, 141].
Tailored, context-sensitive interventions involving fewer economic, societal, and quality-of-life costs than lockdowns are likely more effective and minimize harm [7]. Non-pharmaceutical interventions such as physical distancing, improved ventilation, and effective indoor mask wearing are also more sustainable than broad stay-at-home orders [142–146]. Although emerging genetic SARS-CoV-2 variants may pose additional challenges [147], the biological and epidemiological evidence suggests that the same interventions will work to reduce their transmission. When lockdowns, isolation, or quarantine measures are mandated, economic hardship should be considered and paid sick/quarantine leaves and other types of support must be provided to affected workers, especially those who are most economically vulnerable [7].
7: De-emphasize excessive surface disinfection and other ineffective measures
The evidence is consistent that indirect contact (fomite) transmission is not a significant driver of SARS-CoV-2 spread [148–151], as acknowledged by the CDC [152]. Many routine disinfection rituals, including the ubiquitous usage of alcohol-based hand sanitizers and the excessive use of strong cleaning products, are unnecessary [41, 153]. Misuse of sanitizers, cleansers, and disinfectants has resulted in toxic reactions occasionally leading to hospitalization and even death [154–156]. Such hazardous disinfection practices include washing food products with bleach, applying household cleaning or disinfectant products to bare skin, mixing bleach solutions with vinegar or ammonia, and intentionally or accidentally inhaling or ingesting such products [155, 156]. Beyond being ineffective and occasionally dangerous, excessive cleaning rituals divert important resources, time, and energy from much more useful forms of prevention [151, 153]. There are also growing concerns about the potential longer-term impact on what many scientists have warned is the looming “next pandemic,” that of antimicrobial resistance [157, 158]. Similarly to the misplaced focus on disinfection rituals, public health authorities and the media must do a much better job of educating the public how the coronavirus is—and is not—typically transmitted [159, 160]. For example, fleeting encounters pose minimal risk, even from more transmissible variants41, 78.
Another pervasive practice, temperature screening—especially when using non-contact handheld cutaneous infrared thermometers—is often inaccurate due to environmental factors (e.g., subject-to-sensor distance, ambient temperature, humidity), operator-dependent performance, device variability, and feature changes in target subjects [161–165]. Furthermore, fever is a poor differentiator of the presence or absence of SARS-CoV-2 infection (and the use of antipyretic drugs may mask fever). The ubiquitous use of thermometers for permitting entry to public establishments is thus ineffective. A systematic review of studies regarding exit and entry screening practices (e.g., symptom questionnaires, body temperature measurement) during previous epidemics of influenza A(H1N1), Ebola, and severe acute respiratory syndrome (SARS) found extremely low or no utility in differentiating infected from uninfected [166]. For COVID-19, similar findings have been reported, with only a very small proportion of SARS-CoV-2 infection cases detected during such screening practices [167]. Again, such measures divert resources and attention away from much more effective strategies to control infection.
Furthermore, travel-related restrictions have clearly had a considerable impact on global trade and economies as well as on other systems, including those for international humanitarian responses [145]. Other negative consequences include generating a false sense of security, discouraging travelers from engaging transparently with authorities, and potentially disincentivizing open disclosure by countries during future outbreaks [131, 168]. Although a few countries (e.g., New Zealand, Australia, Taiwan, China), mainly island nations, have attempted SARS-CoV-2 elimination through use of robust quarantine and contact tracing measures [7, 131, 169], it makes little sense, from either an epidemiological or human rights perspective, to shut international land borders or require a negative RT-PCR test result for entry into countries where SARS-CoV-2 is already circulating widely. Similarly, the routine use of quarantine upon arrival and various other entrance screening procedures [164] are also largely ineffective. Such border controls are akin to confiscating matches after the forest is already ablaze. Experience, including lessons learned during this pandemic, suggests that imposition of travel restrictions also generally fails to prevent the spread of new genetic variants, as their discovery typically lags well behind their emergence, and local detection often depends more on which locations are conducting routine genomic surveillance than on where the new variants actually originate [131].
8: Reassess testing practices and policies
Experience suggests that choice of diagnostic technologies should be determined by the intended use, whether to detect infection in individuals with suspected clinical symptoms or to identify potentially infectious individuals to inform isolation recommendations and conduct contact tracing. RT-PCR-based assays have so far been the preferred method for most such purposes [170]. Rapid antigen tests, which are both cheaper and faster, can lead to false negatives, especially in pre-symptomatic carriers, and when conducted without adequate quality control procedures. However, if performed correctly in appropriate populations, they may be sufficiently sensitive and specific for detecting potential infectivity [171], thus suggesting that antigen tests should increasingly be utilized for public health screening. Moreover, further investigation is needed regarding the extent to which positive SARS-CoV-2 RT-PCR results do not always reflect actual infectiousness [172–174], particularly among vaccinated or asymptomatic persons. Finally, given that vaccination reduces symptomatic and asymptomatic SARS-CoV-2 infections and that vaccinated individuals are likely to be less infectious if infected [175–177], testing and quarantine of vaccinated (or previously infected) persons following exposure to someone with suspected or confirmed COVID-19 should in general only be needed if COVID-19 symptoms develop [178]. As we increasingly recognize that SARS-CoV-2 is gradually becoming an endemic virus, it is vital to deemphasize identification of new cases as the key outcome metric of mitigation measures and rather to assess mortality and hospitalization rates [179]. This is also relevant considering that the vaccines were developed to reduce severe and fatal outcomes from COVID-19 and not to fully prevent onward transmission and infection.
9: Expand access to outpatient therapies and prophylactics
As with vaccines, the pandemic has presented challenges in identifying effective therapeutics on a greatly accelerated timeline. Although vaccination remains the priority, some vaccinated individuals will still contract SARS-CoV-2, and some persons will remain unvaccinated. While some medications have been tentatively permitted (not without controversy) on a compassionate use basis in a few countries, approved outpatient therapies for COVID-19 have been limited in most places to intravenous monoclonal antibodies, which are cost-prohibitive in most settings globally and often pose other considerable challenges for widespread use. As evidence on treatment options evolves, policymakers should prioritize quick access to effective outpatient therapies in patients with risk factors for severe disease and to prophylactics for unvaccinated persons at high risk. Assessment of previously identified safe medications might be an efficient way to quickly identify new therapies [180]. In addition, more research is urgently needed regarding the prevalence, diagnosis, prognosis, and treatment options for longer-term (“long haul”) COVID-19 complications.
10: Prevent and prepare for future pandemics
COVID-19 is the second major respiratory viral pandemic in just over a decade and the third coronavirus pandemic within 2 decades. More pandemics are likely in the coming years, whether from new coronaviruses and/or from other pathogens. We clearly must do everything possible to prevent and be better prepared for future pandemics and other public health emergencies [181, 182], and must learn and apply lessons from the recent experience with mitigating COVID-19.
Regarding prevention, policymakers need to take prudent actions immediately to reduce the likelihood of future pandemics, including addressing environmental destruction that brings different species into closer contact with humans, restricting the trafficking of animals, and strengthening biosecurity in laboratories that work with potential human pathogens.
Preparation for the next pandemics should include detailed plans by international organizations that are widely vetted and agreed upon. Lockdowns and quarantines, when (and only if) necessary, need to be designed equitably and to include protection, prioritization, and compensation for those most vulnerable [7], including the elderly, the poor, and workers in frontline and informal jobs. Effective mechanisms must also be established to address equity in access to treatments and vaccines, prioritizing those at highest risk. We certainly must avoid another situation where public health authorities and politicians are left to fly blind and then try to clean up the damage later. It would be a grave error to respond to a new pandemic without applying lessons from the current one.
Conclusions
Given the high transmissibility of SARS-CoV-2, its continuing widespread circulation in some regions, and the emergence of new viral variants [147], it is unlikely that SARS-CoV-2 will be eradicated. Therefore, we will need to continue focusing on mitigation strategies, particularly vaccination [131]. Although SARS-CoV-2 genetic variants will keep emerging, vaccines have so far largely retained their ability to prevent fatal and other severe COVID-19 outcomes [183, 184]. Concerns that such variants will soon evade current vaccines may be overstated, as both the mRNA and adenovirus-DNA vaccines encode for the entire spike protein, providing robust and complex antibody-mediated as well as T-cell immune responses [17, 21, 185, 186]. Furthermore, vaccines can be rapidly modified, if necessary, to adapt to future variants [183, 184]. As previously noted, it is crucial to focus on the key public health objectives of preventing death and other severe disease outcomes, rather than continuing to use numbers of reported cases as the main metric. In any event, maintaining a constant state of emergency until the pandemic is over is not viable. Public health decision-making requires transparency and debate, which are often precluded by emergency orders. A more realistic public health goal is to adjust mitigation and treatment goals as the pandemic evolves, minimizing negative outcomes including the unintended harms associated with unfocused or irrelevant control efforts. The foregoing suggestions for refining our current approaches are presented as best practices that will nevertheless require continuous adjustment through reassessment of the latest evidence. We offer these in the reasonable hope of widespread vaccination helping to achieve far greater control of COVID-19, and also that the world will be better prepared for the next pandemic.
Availability of data and materials
Not applicable.
Abbreviations
- CDC:
-
US Centers for Disease Control and Prevention
- COVID-19:
-
Coronavirus disease 2019
- HCW:
-
Healthcare worker
- RCT:
-
Randomized controlled trial
- RT-PCR:
-
Reverse transcriptase-polymerase chain reaction
- SARS:
-
Severe acute respiratory syndrome
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- UNESCO:
-
United Nations Educational, Scientific and Cultural Organization
- UNICEF:
-
United Nations Children’s Fund
- WHO:
-
World Health Organization
References
Johns Hopkins University. Coronavirus Resource Center. https://coronavirus.jhu.edu/. Accessed 30 Oct 2021.
Mathieu E, Ritchie H, Ortiz-Ospina E, Roser M, Hasell J, Appel C, et al. A global database of COVID-19 vaccinations. Nat Hum Behav. 2021;5(7):947–53. https://doi.org/10.1038/s41562-021-01122-8.
He Q, Mao Q, Zhang J, Bian L, Gao F, Wang J, et al. COVID-19 vaccines: current understanding on immunogenicity, safety, and further considerations. Front Immunol. 2021;12:669339. https://doi.org/10.3389/fimmu.2021.669339.
Lai C-C, Chen I-T, Chao C-M, Lee P-I, Ko W-C, Hsueh P-R. COVID-19 vaccines: concerns beyond protective efficacy and safety. Expert Rev Vaccines. 2021;20(8):1013–25. https://doi.org/10.1080/14760584.2021.1949293.
Bundgaard H, Bundgaard JS, Raaschou-Pedersen DET, von Buchwald C, Todsen T, Norsk JB, et al. Effectiveness of adding a mask recommendation to other public health measures to prevent SARS-CoV-2 infection in Danish mask wearers. Ann Intern Med. 2021;174(3):335–43. https://doi.org/10.7326/M20-6817.
Abaluck J, Kwong LH, Styczynski A, Haque A, Kabir A, Bates-Jefferys E, et al. The impact of community masking on COVID-19: A cluster-randomized trial in Bangladesh. Preprint at poverty-action.org. 2021. https://www.poverty-action.org/publication/impact-community-masking-covid-19-cluster-randomized-trial-bangladesh, DOI: https://doi.org/10.1093/qje/qjab017.
Escandón K, Rasmussen AL, Bogoch II, Murray EJ, Escandón K, Popescu SV, et al. COVID-19 false dichotomies and a comprehensive review of the evidence regarding public health, COVID-19 symptomatology, SARS-CoV-2 transmission, mask wearing, and reinfection. BMC Infect Dis. 2021;21(1):710. https://doi.org/10.1186/s12879-021-06357-4.
Victora CG, Habicht J-P, Bryce J. Evidence-based public health: moving beyond randomized trials. Am J Public Health. 2004;94(3):400–5. https://doi.org/10.2105/AJPH.94.3.400.
Rutter H, Savona N, Glonti K, Bibby J, Cummins S, Finegood DT, et al. The need for a complex systems model of evidence for public health. Lancet. 2017;390(10112):2602–4. https://doi.org/10.1016/S0140-6736(17)31267-9.
Greenhalgh T. Will COVID-19 be evidence-based medicine’s nemesis? PLoS Med. 2020;17(6):e1003266. https://doi.org/10.1371/journal.pmed.1003266.
Iacobucci G. Covid-19: how will a waiver on vaccine patents affect global supply? BMJ. 2021;373:n1182. https://doi.org/10.1136/bmj.n1182.
Gandhi M. The most important thing rich countries can do to help; 2021. https://time.com/6046096/india-covid-19-vaccine-patents/. Accessed 22 Jun 2021.
Martuscelli C. G7 leaders pledge 870 million vaccines to developing world; 2021. Politico. https://www.politico.eu/article/g7-leaders-coronavirus-vaccines-developing-countries/. Accessed 30 Jun 2021.
Parry H, Bruton R, Stephens C, Brown K, Amirthalingam G, Hallis B, et al. Extended interval BNT162b2 vaccination enhances peak antibody generation. Preprint at medRxiv. 2021. https://doi.org/10.1101/2021.05.15.21257017.
Parry H, Bruton R, Stephens C, Brown K, Amirthalingam G, Otter A, et al. Differential immunogenicity of BNT162b2 or ChAdOx1 vaccines after extended-interval homologous dual vaccination in older people. Immun Ageing. 2021;18(1):34. https://doi.org/10.1186/s12979-021-00246-9.
Payne RP, Longet S, Austin JA, Skelly DT, Dejnirattisai W, Adele S, et al. Immunogenicity of standard and extended dosing intervals of BNT162b2 mRNA vaccine. Cell. 2021 (in press). https://doi.org/10.1016/j.cell.2021.10.011.
Plotkin SA, Halsey N. Accelerate coronavirus disease 2019 (COVID-19) vaccine rollout by delaying the second dose of mRNA vaccines. Clin Infect Dis. 2021;73(7):1320–1. https://doi.org/10.1093/cid/ciab068.
Amit S, Regev-Yochay G, Afek A, Kreiss Y, Leshem E. Early rate reductions of SARS-CoV-2 infection and COVID-19 in BNT162b2 vaccine recipients. Lancet. 2021;397(10277):875–7. https://doi.org/10.1016/S0140-6736(21)00448-7.
Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397(10269):99–111. https://doi.org/10.1016/S0140-6736(20)32661-1.
US Centers for Disease Control and Prevention. Interim clinical considerations for use of COVID-19 vaccines currently authorized in the United States; 2021. https://www.cdc.gov/vaccines/covid-19/info-by-product/clinical-considerations.html. Accessed 28 Aug 2021.
Dan JM, Mateus J, Kato Y, Hastie KM, Yu ED, Faliti CE, et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science. 2021;371(6529):eabf4063. https://doi.org/10.1126/science.abf4063.
Klausner J, Kojima N. Op-Ed: Quit ignoring natural COVID immunity; 2021. Medpage Today. https://www.medpagetoday.com/infectiousdisease/covid19/92836. Accessed 20 Jun 2021.
Saadat S, Tehrani ZR, Logue J, Newman M, Frieman MB, Harris AD, et al. Binding and neutralization antibody titers after a single vaccine dose in health care workers previously infected with SARS-CoV-2. JAMA. 2021;383(24):2320–32. https://doi.org/10.1001/jama.2021.3341.
Ebinger JE, Fert-Bober J, Printsev I, Wu M, Sun N, Prostko JC, et al. Antibody responses to the BNT162b2 mRNA vaccine in individuals previously infected with SARS-CoV-2. Nat Med. 2021:27(6):981–4. https://doi.org/10.1038/s41591-021-01325-6.
Manisty C, Otter AD, Treibel TA, McKnight Á, Altmann DM, Brooks T, et al. Antibody response to first BNT162b2 dose in previously SARS-CoV-2-infected individuals. Lancet. 2021;397(10279):1057–8. https://doi.org/10.1016/S0140-6736(21)00501-8.
Prendecki M, Clarke C, Brown J, Cox A, Gleeson S, Guckian M, et al. Effect of previous SARS-CoV-2 infection on humoral and T-cell responses to single-dose BNT162b2 vaccine. Lancet. 2021;397(10280):1178–81. https://doi.org/10.1016/S0140-6736(21)00502-X.
Maxmen A. COVID boosters for wealthy nations spark outrage. Nature News. 2021. https://doi.org/10.1038/d41586-021-02109-1.
Pai M. 10 images that illustrate the shameful global vaccine inequity, Nature Portfolio Microbiology Community. 2021. https://naturemicrobiologycommunity.nature.com/posts/10-images-illustrate-the-global-vaccine-inequity
Mancini DP, Burn-Murdoch D. Global Covid-19 death toll tops 5m but underestimates true figure, say experts. 2021. Financial times. https://www.ft.com/content/35a3d40a-f71f-4fca-893d-884fec5633d8. Accessed 2 Nov 2021.
Brosseau LM, Escandón K, Ulrich AK, Rasmussen AL, Roy CJ, Bix GJ, et al. SARS-CoV-2 dose, infection, and disease outcomes for COVID-19 – a review. Clin Infect Dis. 2021 (Epub ahead of print). https://doi.org/10.1093/cid/ciab903.
Ssentongo P, Ssentongo AE, Heilbrunn ES, Ba DM, Chinchilli VM. Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: a systematic review and meta-analysis. PLoS One. 2020;15(8):e0238215. https://doi.org/10.1371/journal.pone.0238215.
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5. https://doi.org/10.1016/j.ijid.2020.03.017.
Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Inf Secur. 2020;81(2):e16–25. https://doi.org/10.1016/j.jinf.2020.04.021.
Fang X, Li S, Yu H, Wang P, Zhang Y, Chen Z, et al. Epidemiological, comorbidity factors with severity and prognosis of COVID-19: a systematic review and meta-analysis. Aging. 2020;12(13):12493–503. https://doi.org/10.18632/aging.103579.
Földi M, Farkas N, Kiss S, Zádori N, Váncsa S, Szakó L, et al. Obesity is a risk factor for developing critical condition in COVID-19 patients: a systematic review and meta-analysis. Obes Rev. 2020;21(10):e13095. https://doi.org/10.1111/obr.13095.
Mendes NF, Jara CP, Mansour E, Araújo EP, Velloso LA. Asthma and COVID-19: a systematic review. Allergy, Asthma Clin Immunol. 2021;17(1):5. https://doi.org/10.1186/s13223-020-00509-y.
Halpin DMG, Faner R, Sibila O, Badia JR, Agusti A. Do chronic respiratory diseases or their treatment affect the risk of SARS-CoV-2 infection? Lancet Respir Med. 2020;8(5):436–8. https://doi.org/10.1016/S2213-2600(20)30167-3.
Sunjaya AP, Allida SM, Di Tanna GL, Jenkins C. Asthma and risk of infection, hospitalization, ICU admission and mortality from COVID-19: systematic review and meta-analysis. J Asthma. 2021 (Epub ahead of print). https://doi.org/10.1080/02770903.2021.1888116.
Wang Y, Chen J, Chen W, Liu L, Dong M, Ji J, et al. Does asthma increase the mortality of patients with COVID-19?: a systematic review and meta-analysis. Int Arch Allergy Immunol. 2021;182(1):76–82. https://doi.org/10.1159/000510953.
Morais-Almeida M, Pité H, Aguiar R, Ansotegui I, Bousquet J. Asthma and the coronavirus disease 2019 pandemic: a literature review. Int Arch Allergy Immunol. 2020;181(9):680–8. https://doi.org/10.1159/000509057.
Halperin DT. Facing COVID without panic: 12 common myths and 12 lesser known facts about the pandemic, clearly explained by an epidemiologist. Independently published; July 2020.
Leclerc QJ, Fuller NM, Knight LE, Funk S, Knight GM. What settings have been linked to SARS-CoV-2 transmission clusters? Wellcome Open Res. 2020;5:83. https://doi.org/10.12688/wellcomeopenres.15889.2.
Althouse BM, Wenger EA, Miller JC, Scarpino SV, Allard A, Hébert-Dufresne L, et al. Superspreading events in the transmission dynamics of SARS-CoV-2: opportunities for interventions and control. PLoS Biol. 2020;18(11):e3000897. https://doi.org/10.1371/journal.pbio.3000897.
Pawlowski C, Lenehan P, Puranik A, Agarwal V, Venkatakrishnan AJ, Niesen MJM, et al. FDA-authorized mRNA COVID-19 vaccines are effective per real-world evidence synthesized across a multi-state health system. Med. 2021;2(8):979–992.e8. https://doi.org/10.1016/j.medj.2021.06.007.
Thompson MG, Burgess JL, Naleway AL, Tyner HL, Yoon SK, Meece J, et al. Interim estimates of vaccine effectiveness of BNT162b2 and mRNA-1273 COVID-19 vaccines in preventing SARS-CoV-2 infection among health care personnel, first responders, and other essential and frontline workers — eight U.S. locations, December 2020–March 2021. MMWR Morb Mortal Wkly Rep. 2021;70(13):495–500. https://doi.org/10.15585/mmwr.mm7013e3.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–15. https://doi.org/10.1056/NEJMoa2034577.
Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403–16. https://doi.org/10.1056/NEJMoa2035389.
Hall VJ, Foulkes S, Saei A, Andrews N, Oguti B, Charlett A, et al. COVID-19 vaccine coverage in health-care workers in England and effectiveness of BNT162b2 mRNA vaccine against infection (SIREN): a prospective, multicentre, cohort study. Lancet. 2021;397(10286):1725–35. https://doi.org/10.1016/S0140-6736(21)00790-X.
Emary KRW, Golubchik T, Aley PK, Ariani CV, Angus B, Bibi S, et al. Efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 variant of concern 202012/01 (B.1.1.7): an exploratory analysis of a randomised controlled trial. Lancet. 2021;397(10282):1351–62. https://doi.org/10.1016/S0140-6736(21)00628-0.
Haas EJ, Angulo FJ, McLaughlin JM, Anis E, Singer SR, Khan F, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet. 2021;397(10287):1819–29. https://doi.org/10.1016/S0140-6736(21)00947-8.
Chemaitelly H, Yassine HM, Benslimane FM, Al Khatib HA, Tang P, Hasan MR, et al. mRNA-1273 COVID-19 vaccine effectiveness against the B.1.1.7 and B.1.351 variants and severe COVID-19 disease in Qatar. Nat Med. 2021;27(9):1614–21. https://doi.org/10.1038/s41591-021-01446-y.
Lopez Bernal J, Andrews N, Gower C, Robertson C, Stowe J, Tessier E, et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ. 2021;373:n1088. https://doi.org/10.1136/bmj.n1088.
Pritchard E, Matthews PC, Stoesser N, Eyre DW, Gethings O, Vihta K-D, et al. Impact of vaccination on new SARS-CoV-2 infections in the United Kingdom. Nat Med. 2021;27(8):1370–8. https://doi.org/10.1038/s41591-021-01410-w.
Rosenberg ES, Holtgrave DR, Dorabawila V, Conroy M, Greene D, Lutterloh E, et al. New COVID-19 cases and hospitalizations among adults, by vaccination status — New York, May 3–July 25, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(34):1150–5. https://doi.org/10.15585/mmwr.mm7034e1.
Lopez Bernal J, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (Delta) variant. N Engl J Med. 2021;385(7):585–94. https://doi.org/10.1056/NEJMoa2108891.
Fowlkes A, Gaglani M, Groover K, Thiese MS, Tyner H, Ellingson K. Effectiveness of COVID-19 vaccines in preventing SARS-CoV-2 infection among frontline workers before and during B.1.617.2 (Delta) variant predominance — eight U.S. locations, December 2020–August 2021. MMWR Morb Mortal Wkly Rep. 2021;70(34):1167–9. https://doi.org/10.15585/mmwr.mm7034e4.
Nanduri S, Pilishvili T, Derado G, Soe MM, Dollard P, Wu H, et al. Effectiveness of Pfizer-BioNTech and Moderna vaccines in preventing SARS-CoV-2 infection among nursing home residents before and during widespread circulation of the SARS-CoV-2 B.1.617.2 (Delta) variant — National Healthcare Safety Network, March 1–August 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(34):1163–6. https://doi.org/10.15585/mmwr.mm7034e3.
Tande AJ, Pollock BD, Shah ND, Binnicker M, Berbari EF. mRNA vaccine effectiveness against asymptomatic SARS-CoV-2 infection over a seven-month period. Infect Control Hosp Epidemiol. 2021 (Epub ahead of print). https://doi.org/10.1017/ice.2021.399.
Seppälä E, Veneti L, Starrfelt J, Danielsen AS, Bragstad K, Hungnes O, et al. Vaccine effectiveness against infection with the Delta (B.1.617.2) variant, Norway, April to August 2021. Eurosurveillance. 2021;26(35):2100793. https://doi.org/10.2807/1560-7917.ES.2021.26.35.2100793.
Bian L, Gao Q, Gao F, Wang Q, He Q, Wu X, et al. Impact of the Delta variant on vaccine efficacy and response strategies. Expert Rev Vaccines. 2021;20(10):1201–9. https://doi.org/10.1080/14760584.2021.1976153.
Noh JY, Jeong HW, Kim JH, Shin E. T cell-oriented strategies for controlling the COVID-19 pandemic. Nat Rev Immunol. 2021;21(11):687–8. https://doi.org/10.1038/s41577-021-00625-9.
Sette A, Crotty S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell. 2021;184(4):861–80. https://doi.org/10.1016/j.cell.2021.01.007.
Lumley SF, O’Donnell D, Stoesser NE, Matthews PC, Howarth A, Hatch SB, et al. Antibody status and incidence of SARS-CoV-2 infection in health care workers. N Engl J Med. 2021;384(6):533–40. https://doi.org/10.1056/NEJMoa2034545.
Vitale J, Mumoli N, Clerici P, De Paschale M, Evangelista I, Cei M, et al. Assessment of SARS-CoV-2 reinfection 1 year after primary infection in a population in Lombardy, Italy. JAMA Intern Med. 2021;384(6):533–40. https://doi.org/10.1001/jamainternmed.2021.2959.
Hall VJ, Foulkes S, Charlett A, Atti A, Monk EJM, Simmons R, et al. SARS-CoV-2 infection rates of antibody-positive compared with antibody-negative health-care workers in England: a large, multicentre, prospective cohort study (SIREN). Lancet. 2021;397(10283):1459–69. https://doi.org/10.1016/S0140-6736(21)00675-9.
Leidi A, Koegler F, Dumont R, Dubos R, Zaballa M-E, Piumatti G, et al. Risk of reinfection after seroconversion to SARS-CoV-2: a population-based propensity-score matched cohort study. Clin Infect Dis. 2021 (Epub ahead of print). https://doi.org/10.1093/cid/ciab495.
Ripperger TJ, Uhrlaub JL, Watanabe M, Wong R, Castaneda Y, Pizzato HA, et al. Orthogonal SARS-CoV-2 serological assays enable surveillance of low-prevalence communities and reveal durable humoral immunity. Immunity. 2020;53(5):925–933.e4. https://doi.org/10.1016/j.immuni.2020.10.004.
Hansen CH, Michlmayr D, Gubbels SM, Mølbak K, Ethelberg S. Assessment of protection against reinfection with SARS-CoV-2 among 4 million PCR-tested individuals in Denmark in 2020: a population-level observational study. Lancet. 2021;397(10280):1204–12. https://doi.org/10.1016/S0140-6736(21)00575-4.
Gazit S, Shlezinger R, Perez G, Lotan R, Peretz A, Ben-Tov A, et al. Comparing SARS-CoV-2 natural immunity to vaccine-induced immunity: reinfections versus breakthrough infections. Preprint at medRxiv. 2021. https://doi.org/10.1101/2021.08.24.21262415.
Skelly DT, Harding AC, Gilbert-Jaramillo J, Knight ML, Longet S, Brown A, et al. Two doses of SARS-CoV-2 vaccination induce robust immune responses to emerging SARS-CoV-2 variants of concern. Nat Commun. 2021;12(1):5061. https://doi.org/10.1038/s41467-021-25167-5.
Greaney AJ, Loes AN, Gentles LE, Crawford KHD, Starr TN, Malone KD, et al. Antibodies elicited by mRNA-1273 vaccination bind more broadly to the receptor binding domain than do those from SARS-CoV-2 infection. Sci Transl Med. 2021;13(600):eabi9915. https://doi.org/10.1126/scitranslmed.abi9915.
Block J. Vaccinating people who have had covid-19: why doesn’t natural immunity count in the US? BMJ. 2021;374:n2101. https://doi.org/10.1136/bmj.n2101.
Potts M, Halperin DT, Kirby D, Swidler A, Marseille E, Klausner JD, et al. Public health. Reassessing HIV prevention. Science. 2008;320(5877):749–50. https://doi.org/10.1126/science.1153843.
Kutscher E, Greene RE. A harm-reduction approach to coronavirus disease 2019 (COVID-19)—safer socializing. JAMA Health Forum. 2020;1(6):e200656. https://doi.org/10.1001/jamahealthforum.2020.0656.
Marcus J. Quarantine fatigue is real; 2020. The Atlantic. https://www.theatlantic.com/ideas/archive/2020/05/quarantine-fatigue-real-and-shaming-people-wont-help/611482/. Accessed 20 May 2020.
Barocas J, Gandhi M. Harm reduction principles can help us restore trust in public health messaging on covid-19. 2020. The BMJ Opinion. https://blogs.bmj.com/bmj/2020/12/15/harm-reduction-principles-can-help-us-restore-trust-in-public-health-messaging-on-covid-19/. Accessed 8 Mar 2021.
Normile D. Japan ends its COVID-19 state of emergency. 2020. Science. https://doi.org/10.1126/science.abd0092.
Halperin DT. Coping with COVID-19: learning from past pandemics to avoid pitfalls and panic. Glob Heal Sci Pract. 2020;8(2):155–65. https://doi.org/10.9745/GHSP-D-20-00189.
Barocas J, Gonsalves G. Make it easier to stay safe from COVID- 19, instead of shaming and punishing people. 2020. USA Today. https://www.usatoday.com/story/opinion/2020/12/07/stop-covid-shaming-punishing-give-incentives-to-stay-safe-column/3812823001/. Accessed 31 Jan 2021.
Marcus J, Martin M. Epidemiologist on why “pandemic shaming” isn’t working; 2020. National Public Radio. https://www.npr.org/2020/12/19/948403401/epidemiologist-on-why-pandemic-shaming-isn-t-working. Accessed 1 Jan 2021.
Pavli A, Maltezou HC. COVID-19 vaccine passport for safe resumption of travel. J Travel Med. 2021;28(4):taab079. https://doi.org/10.1093/jtm/taab079.
Sharun K, Tiwari R, Dhama K, Rabaan AA, Alhumaid S. COVID-19 vaccination passport: prospects, scientific feasibility, and ethical concerns. Hum Vaccin Immunother. 2021 (Epub ahead of print). https://doi.org/10.1080/21645515.2021.1953350.
Dye C, Mills MC. COVID-19 vaccination passports. Science. 2021;371(6535):1184. https://doi.org/10.1126/science.abi5245.
Cevik M, Marcus JL, Buckee C, Smith TC. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission dynamics should inform policy. Clin Infect Dis. 2021;73(S2):S170–6. https://doi.org/10.1093/cid/ciaa1442.
Miller AM. Stop shaming people for going outside. The risks are generally low, and the benefits are endless. 2020. Business Insider. https://www.businessinsider.com/you-can-still-go-outside-while-quarantining-sheltering-in-place-2020-4. Accessed 27 Jun 2020.
Popkin G. Don’t cancel the outdoors. We need it to stay sane. 2020. The Washington Post. https://www.washingtonpost.com/outlook/2020/03/24/dont-cancel-outdoors-we-need-them-stay-sane/. Accessed 1 Jun 2020.
DeCosta-Klipa N. UMass Amherst is prohibiting outdoor exercise during its lockdown. But why? 2021. Boston.com. https://www.boston.com/news/coronavirus/2021/02/11/umass-amherst-lockdown-outdoor-exercise. Accessed 8 Mar 2021.
Bote J. Officers at dorms, outdoor exercise ban: UC Berkeley extends dorm lockdown with stricter mandates. 2021. SFGate. https://www.sfgate.com/education/article/Police-dorms-outdoor-exercise-UC-Berkeley-lockdown-15937294.php. Accessed 8 Mar 2021.
Tufekci Z. Keep the parks open; 2020. The Atlantic. https://www.theatlantic.com/health/archive/2020/04/closing-parks-ineffective-pandemic-theater/609580/. Accessed 15 Jun 2020.
Tufekci Z. Scolding beachgoers isn’t helping; 2020. The Atlantic. https://www.theatlantic.com/health/archive/2020/07/it-okay-go-beach/613849/. Accessed 6 Jul 2020.
Qian H, Miao T, Liu L, Zheng X, Luo D, Li Y. Indoor transmission of SARS-CoV-2. Indoor Air. 2021;31(3):639–45. https://doi.org/10.1111/ina.12766.
McGreevy R. Outdoor transmission accounts for 0.1% of State’s Covid-19 cases; 2021. The Irish Times. https://www.irishtimes.com/news/ireland/irish-news/outdoor-transmission-accounts-for-0-1-of-state-s-covid-19-cases-1.4529036. Accessed 30 Apr 2021.
Lakha F, Rudge JW, Holt H. Rapid synthesis of evidence on settings which have been associated with SARS-CoV-2 transmission clusters. 2020. https://superspreadingdatabase.github.io/Evidence_on_clusters_final.pdf. Accessed 10 Sept 2020.
Fouda B, Tram HPB, Makram OM, Abdalla AS, Singh T, Hung I-C, et al. Identifying SARS-CoV2 transmission cluster category: an analysis of country government database. J Infect Public Health. 2021;14(4):461–7. https://doi.org/10.1016/j.jiph.2021.01.006.
US Centers for Disease Control and Prevention. Choosing safer activities; 2021. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/participate-in-activities.html. Accessed 1 Jun 2021.
World Health Organization. Mask use in the context of COVID-19: Interim guidance. 2020. https://apps.who.int/iris/handle/10665/337199. Accessed 30 Jan 2021.
US Centers for Disease Control and Prevention. Guidance for wearings masks; 2021. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html. Accessed 30 Apr 2021.
Slater SJ, Christiana RW, Gustat J. Recommendations for keeping parks and green space accessible for mental and physical health during COVID-19 and other pandemics. Prev Chronic Dis. 2020;17(E59):200204. https://doi.org/10.5888/pcd17.200204.
Mathai V, Das A, Bailey JA, Breuer K. Airflows inside passenger cars and implications for airborne disease transmission. Sci Adv. 2021;7(1):eabe0166. https://doi.org/10.1126/sciadv.abe0166.
Allen JG, Ibrahim AM. Indoor air changes and potential implications for SARS-CoV-2 transmission. JAMA. 2021;325(20):2112. https://doi.org/10.1001/jama.2021.5053.
Halperin D. A marshall plan for Covid-19. 2020. Real Clear Policy. https://www.realclearpolicy.com/articles/2020/11/05/a_marshall_plan_for_covid-19_583019.html. Accessed 5 Mar 2021.
World Health Organization. Roadmap to improve and ensure good indoor ventilation in the context of COVID-19; 2021. https://www.who.int/publications/i/item/9789240021280. Accessed 30 Mar 2021.
United Nations Educational Scientific and Cultural Organization. One year into COVID: Prioritizing education recovery to avoid a generational catastrophe; 2021. https://unesdoc.unesco.org/ark:/48223/pf0000376984.
Evans D, Hares S, Mendez Acosta A, Saintis C. It’s been a year since schools started to close due to COVID-19; 2021. https://www.cgdev.org/blog/its-been-year-schools-started-close-due-covid-19. Accessed 9 Apr 2021.
Hawrilenko M, Kroshus E, Tandon P, Christakis D. The association between school cosures and child mental health during COVID-19. JAMA Netw Open. 2021;4(9):e2124092. https://doi.org/10.1001/jamanetworkopen.2021.24092.
Honein MA, Barrios LC, Brooks JT. Data and policy to guide opening schools safely to limit the spread of SARS-CoV-2 infection. JAMA. 2021;325(9):823. https://doi.org/10.1001/jama.2021.0374.
European Centre for Disease Prevention and Control. COVID-19 in children and the role of school settings in transmission–second update. 2020. https://www.ecdc.europa.eu/en/publications-data/children-and-school-settings-covid-19-transmission. Accessed 7 Aug 2021.
Reid M. Latin America’s silent tragedy of empty classrooms. De Economist. 2021; https://www.economist.com/the-americas/2021/06/19/latin-americas-silent-tragedy-of-empty-classrooms. Accessed 23 Jun 2021.
United Nations Educational Scientific and Cultural Organization. Education: From disruption to recovery. COVID-19 impact on education. https://en.unesco.org/covid19/educationresponse#schoolclosures. Accessed 16 Sep 2021.
Douglas M, Katikireddi SV, Taulbut M, McKee M, McCartney G. Mitigating the wider health effects of covid-19 pandemic response. BMJ. 2020;369:m1557. https://doi.org/10.1136/bmj.m1557.
Mayurasakorn K, Pinsawas B, Mongkolsucharitkul P, Sranacharoenpong K, Damapong S. School closure, COVID-19 and lunch programme: unprecedented undernutrition crisis in low-middle income countries. J Paediatr Child Health. 2020;56(7):1013–7. https://doi.org/10.1111/jpc.15018.
Cattan S, Farquharson C, Krutikova S, Phimister A, Salisbury A, Sevilla A. Inequalities in responses to school closures over the course of the first COVID-19 lockdown: Institute for Fiscal Studies; 2021. https://doi.org/10.1920/wp.ifs.2021.421.
Christie A, Brooks JT, Hicks LA, Sauber-Schatz EK, Yoder JS, Honein MA. Guidance for implementing COVID-19 prevention strategies in the context of varying community transmission levels and vaccination coverage. MMWR Morb Mortal Wkly Rep. 2021;70(30):1044–7. https://doi.org/10.15585/mmwr.mm7030e2.
Lessler J, Grabowski MK, Grantz KH, Badillo-Goicoechea E, Metcalf CJE, Lupton-Smith C, et al. Household COVID-19 risk and in-person schooling. Science. 2021;372(6546):1092–7. https://doi.org/10.1126/science.abh2939.
Ghosh R, Dubey MJ, Chatterjee S, Dubey S. Impact of COVID −19 on children: special focus on the psychosocial aspect. Minerva Pediatr. 2020;72(3):226–35. https://doi.org/10.23736/S0026-4946.20.05887-9.
Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19-related school closings and risk of weight gain among children. Obesity. 2020;28(6):1008–9. https://doi.org/10.1002/oby.22813.
Zimmerman KO, Akinboyo IC, Brookhart MA, Boutzoukas AE, McGann KA, Smith MJ, et al. Incidence and secondary transmission of SARS-CoV-2 infections in schools. Pediatrics. 2021;147(4):e2020048090. https://doi.org/10.1542/peds.2020-048090.
Falk A, Benda A, Falk P, Steffen S, Wallace Z, Høeg TB. COVID-19 cases and transmission in 17 K–12 schools — Wood County, Wisconsin, August 31–November 29, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(4):136–40. https://doi.org/10.15585/mmwr.mm7004e3.
Soriano-Arandes A, Gatell A, Serrano P, Biosca M, Campillo F, Capdevila R, et al. Household severe acute respiratory syndrome coronavirus 2 transmission and children: a network prospective study. Clin Infect Dis. 2021;73(6):e1261–9. https://doi.org/10.1093/cid/ciab228.
Baral S, Chandler R, Prieto RG, Gupta S, Mishra S, Kulldorff M. Leveraging epidemiological principles to evaluate Sweden’s COVID-19 response. Ann Epidemiol. 2021;54:21–6. https://doi.org/10.1016/j.annepidem.2020.11.005.
Vlachos J, Hertegård EB, Svaleryd H. The effects of school closures on SARS-CoV-2 among parents and teachers. Proc Natl Acad Sci. 2021;118(9):e2020834118. https://doi.org/10.1073/pnas.2020834118.
Ludvigsson JF, Engerström L, Nordenhäll C, Larsson E. Open schools, Covid-19, and child and teacher morbidity in Sweden. N Engl J Med. 2021;384(7):669–71. https://doi.org/10.1056/NEJMc2026670.
Ehrhardt J, Ekinci A, Krehl H, Meincke M, Finci I, Klein J, et al. Transmission of SARS-CoV-2 in children aged 0 to 19 years in childcare facilities and schools after their reopening in may 2020, Baden-Württemberg, Germany. Eurosurveillance. 2020;25(36):4–7. https://doi.org/10.2807/1560-7917.ES.2020.25.36.2001587.
US Centers for Disease Control and Prevention. Guidance for COVID-19 prevention in K-12 schools; 2021. https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/k-12-guidance.html. Accessed 1 Sept 2021.
Torjesen I. Covid-19: Delta variant is now UK’s most dominant strain and spreading through schools. BMJ. 2021;373:n1445. https://doi.org/10.1136/bmj.n1445.
Lam-Hine T, McCurdy SA, Santora L, Duncan L, Corbett-Detig R, Kapusinszky B, et al. Outbreak associated with SARS-CoV-2 B.1.617.2 (Delta) variant in an elementary school — Marin County, California, May–June 2021. MMWR Morb Mortal Wkly Rep. 2021;70(35):1214–9. https://doi.org/10.15585/mmwr.mm7035e2.
van den Berg P, Schechter-Perkins EM, Jack RS, Epshtein I, Nelson R, Oster E, et al. Effectiveness of three versus six feet of physical distancing for controlling spread of COVID-19 among primary and secondary students and staff: a retrospective, state-wide cohort study. Clin Infect Dis. 2021 (Epub ahead of print). https://doi.org/10.1093/cid/ciab230.
US Centers for Disease Control and Prevention. Operational strategy for K-12 schools through phased prevention; 2021. https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/operation-strategy.html. Accessed 30 May 2021.
Gettings J, Czarnik M, Morris E, Haller E, Thompson-Paul AM, Rasberry C, et al. Mask use and ventilation improvements to reduce COVID-19 incidence in elementary schools — Georgia, November 16–December 11, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(21):779–84. https://doi.org/10.15585/mmwr.mm7021e1.
Gandhi M, Baral S. What does public health really mean? Lessons from covid-19. BMJ Opinion. 2021; https://blogs.bmj.com/bmj/2021/07/26/what-does-public-health-really-mean-lessons-from-covid-19/.
Grubaugh ND, Hodcroft EB, Fauver JR, Phelan AL, Cevik M. Public health actions to control new SARS-CoV-2 variants. Cell. 2021;184(5):1127–32. https://doi.org/10.1016/j.cell.2021.01.044.
United Nations Children’s Fund. UNICEF chief: Closing schools should be “measure of last resort”. 2021. United Nations News. https://news.un.org/en/story/2021/01/1081912. Accessed 30 Jan 2021.
Hodgins S, Saad A. Will the higher-income country blueprint for COVID-19 work in low- and lower middle-income countries? Glob Heal Sci Pract. 2020;8(2):136–43. https://doi.org/10.9745/GHSP-D-20-00217.
Bavli I, Sutton B, Galea S. Harms of public health interventions against covid-19 must not be ignored. BMJ. 2020;371:m4074. https://doi.org/10.1136/bmj.m4074.
Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7(6):468–71. https://doi.org/10.1016/S2215-0366(20)30171-1.
Marques ES, de Moraes CL, Hasselmann MH, Deslandes SF, Reichenheim ME. Violence against women, children, and adolescents during the COVID-19 pandemic: overview, contributing factors, and mitigating measures. Cad Saude Publica. 2020;36(4):e00074420. https://doi.org/10.1590/0102-311X00074420.
Baral S, Rao A, Twahirwa Rwema JO, Lyons C, Cevik M, Kågesten AE, et al. Competing health risks associated with the COVID-19 pandemic and response: a scoping review. Preprint at medRxiv. 2021. https://doi.org/10.1101/2021.01.07.21249419.
Chang AY, Cullen MR, Harrington RA, Barry M. The impact of novel coronavirus COVID-19 on noncommunicable disease patients and health systems: a review. J Intern Med. 2021;289(4):450–62. https://doi.org/10.1111/joim.13184.
Lin AL, Vittinghoff E, Olgin JE, Pletcher MJ, Marcus GM. Body weight changes during pandemic-related shelter-in-place in a longitudinal cohort study. JAMA Netw Open. 2021;4(3):e212536. https://doi.org/10.1001/jamanetworkopen.2021.2536.
Aum S, Lee SY, Shin Y. COVID-19 doesn’t need lockdowns to destroy jobs: The effect of local outbreaks in Korea. Labour Econ. 2021;70:101993. https://doi.org/10.1016/j.labeco.2021.101993.
Chetty R, Friedman JN, Hendren N, Stepner M. The economic impacts of COVID-19: Evidence from a new public database built using private sector data. National Bureau Econ Res. 2020. https://www.nber.org/papers/w27431
Honein MA, Christie A, Rose DA, Brooks JT, Meaney-Delman D, Cohn A, et al. Summary of guidance for public health strategies to address high levels of community transmission of SARS-CoV-2 and related deaths, December 2020. MMWR Morb Mortal Wkly Rep. 2020;69(49):1860–7. https://doi.org/10.15585/mmwr.mm6949e2.
Escandón K, Martin GP, Kuppalli K, Escandón K. Appropriate usage of face masks to prevent SARS-CoV-2: sharpening the messaging amid the COVID-19 pandemic. Disaster Med Public Health Prep. 2021;15(4):e5–7. https://doi.org/10.1017/dmp.2020.336.
Bo Y, Guo C, Lin C, Zeng Y, Li HB, Zhang Y, et al. Effectiveness of non-pharmaceutical interventions on COVID-19 transmission in 190 countries from 23 January to 13 April 2020. Int J Infect Dis. 2021;102:247–53. https://doi.org/10.1016/j.ijid.2020.10.066.
Haug N, Geyrhofer L, Londei A, Dervic E, Desvars-Larrive A, Loreto V, et al. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat Hum Behav. 2020;4(12):1303–12. https://doi.org/10.1038/s41562-020-01009-0.
Rasmussen AL, Escandón K, Popescu SV. Facial masking for Covid-19. N Engl J Med. 2020;383(21):2092. https://doi.org/10.1056/NEJMc2030886.
World Health Organization. COVID-19 weekly epidemiological update. Edition 56. 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19-7-september-2021. Accessed 11 Sept 2021.
Mondelli MU, Colaneri M, Seminari EM, Baldanti F, Bruno R. Low risk of SARS-CoV-2 transmission by fomites in real-life conditions. Lancet Infect Dis. 2021;21(5):e112. https://doi.org/10.1016/S1473-3099(20)30678-2.
Goldman E. Exaggerated risk of transmission of COVID-19 by fomites. Lancet Infect Dis. 2020;20(8):892–3. https://doi.org/10.1016/S1473-3099(20)30561-2.
Meyerowitz EA, Richterman A, Gandhi RT, Sax PE. Transmission of SARS-CoV-2: a review of viral, host, and environmental factors. Ann Intern Med. 2021;174(1):69–79. https://doi.org/10.7326/M20-5008.
Lewis D. COVID-19 rarely spreads through surfaces. So why are we still deep cleaning? Nature. 2021;590(7844):26–8. https://doi.org/10.1038/d41586-021-00251-4.
US Centers for Disease Control and Prevention. Scientific brief: SARS-CoV-2 transmission. 2021. https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html. Accessed 8 May 2021.
Thompson D. Hygiene theater is still a huge waste of time; 2021. https://www.theatlantic.com/ideas/archive/2021/02/hygiene-theater-still-waste/617939/. Accessed 8 Mar 2021.
Yip L, Bixler D, Brooks DE, Clarke KR, Datta SD, Dudley S, et al. Serious adverse health events, including death, associated with ingesting alcohol-based hand sanitizers containing methanol — Arizona and New Mexico, May–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1070–3. https://doi.org/10.15585/mmwr.mm6932e1.
Gharpure R, Hunter CM, Schnall AH, Barrett CE, Kirby AE, Kunz J, et al. Knowledge and practices regarding safe household cleaning and disinfection for COVID-19 prevention — United States, May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):705–9. https://doi.org/10.15585/mmwr.mm6923e2.
Chang A, Schnall AH, Law R, Bronstein AC, Marraffa JM, Spiller HA, et al. Cleaning and disinfectant chemical exposures and temporal associations with COVID-19 — National Poison Data System, United States, January 1, 2020–March 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(16):496–8. https://doi.org/10.15585/mmwr.mm6916e1.
Rezasoltani S, Yadegar A, Hatami B, Asadzadeh Aghdaei H, Zali MR. Antimicrobial resistance as a hidden menace lurking behind the COVID-19 outbreak: the global impacts of too much hygiene on AMR. Front Microbiol. 2020;11:590683. https://doi.org/10.3389/fmicb.2020.590683.
Makary M, Das I, Hashim F, Walsh C. The next pandemic is here. 2021. MedPage Today. https://www.medpagetoday.com/opinion/marty-makary/90795. Accessed 8 Mar 2021.
Zhang XS, Duchaine C. SARS-CoV-2 and health care worker protection in low-risk settings: a review of modes of transmission and a novel airborne model involving inhalable particles. Clin Microbiol Rev. 2020;34(1):e00184–20. https://doi.org/10.1128/CMR.00184-20.
Leung NHL. Transmissibility and transmission of respiratory viruses. Nat Rev Microbiol. 2021;19(8):528–45. https://doi.org/10.1038/s41579-021-00535-6.
Wright WF, Mackowiak PA. Why temperature screening for coronavirus disease 2019 with noncontact infrared thermometers does not work. Open Forum Infect Dis. 2021;8(1):4–6. https://doi.org/10.1093/ofid/ofaa603.
Aw J. The non-contact handheld cutaneous infra-red thermometer for fever screening during the COVID-19 global emergency. J Hosp Infect. 2020;104(4):451. https://doi.org/10.1016/j.jhin.2020.02.010.
Dzien C, Halder W, Winner H, Lechleitner M. Covid-19 screening: are forehead temperature measurements during cold outdoor temperatures really helpful? Wien Klin Wochenschr. 2021;133(7–8):331–5. https://doi.org/10.1007/s00508-020-01754-2.
Normile D. Airport screening is largely futile, research shows. Science. 2020;367(6483):1177–8. https://doi.org/10.1126/science.367.6483.1177.
Kojima N, Klausner J. It’s time to ditch COVID-19 temperature checks. 2021. https://www.thedailybeast.com/its-time-to-ditch-covid-19-temperature-checks?source=email&via=desktop. Accessed 3 Jun 2021.
Mouchtouri, Christoforidou, an der Heiden, Lemos, Fanos, Rexroth, et al. Exit and entry screening practices for infectious diseases among travelers at points of entry: Looking for evidence on public health impact. Int J Environ Res Public Health. 2019;16(23):4638. https://doi.org/10.3390/ijerph16234638.
Mouchtouri VA, Bogogiannidou Z, Dirksen-Fischer M, Tsiodras S, Hadjichristodoulou C. Detection of imported COVID-19 cases worldwide: early assessment of airport entry screening, 24 January until 17 February 2020. Trop Med Health. 2020;48(1):79. https://doi.org/10.1186/s41182-020-00260-5.
Devi S. Travel restrictions hampering COVID-19 response. Lancet. 2020;395(10233):1331–2. https://doi.org/10.1016/S0140-6736(20)30967-3.
Baker MG, Wilson N, Blakely T. Elimination could be the optimal response strategy for covid-19 and other emerging pandemic diseases. BMJ. 2020;371:m4907. https://doi.org/10.1136/bmj.m4907.
Binnicker MJ. Challenges and controversies to testing for COVID-19. J Clin Microbiol. 2020;58(11):e01695–20. https://doi.org/10.1128/JCM.01695-20.
Mina MJ, Andersen KG. COVID-19 testing: one size does not fit all. Science. 2021;371(6525):126–7. https://doi.org/10.1126/science.abe9187.
Cevik M, Tate M, Lloyd O, Maraolo AE, Schafers J, Ho A. SARS-CoV-2, SARS-CoV, and MERS-CoV viral load dynamics, duration of viral shedding, and infectiousness: a systematic review and meta-analysis. Lancet Microbe. 2021;2(1):e13–22. https://doi.org/10.1016/S2666-5247(20)30172-5.
Walsh KA, Jordan K, Clyne B, Rohde D, Drummond L, Byrne P, et al. SARS-CoV-2 detection, viral load and infectivity over the course of an infection. J Inf Secur. 2020;81(3):357–71. https://doi.org/10.1016/j.jinf.2020.06.067.
Jefferson T, Spencer EA, Brassey J, Heneghan C. Viral cultures for COVID-19 infectious potential assessment – a systematic review. Clin Infect Dis. 2020 (Epub ahead of print). https://doi.org/10.1093/cid/ciaa1764.
Levine-Tiefenbrun M, Yelin I, Katz R, Herzel E, Golan Z, Schreiber L, et al. Initial report of decreased SARS-CoV-2 viral load after inoculation with the BNT162b2 vaccine. Nat Med. 2021;27(5):790–2. https://doi.org/10.1038/s41591-021-01316-7.
Petter E, Mor O, Zuckerman N, Oz-Levi D, Younger A, Aran D, et al. Initial real world evidence for lower viral load of individuals who have been vaccinated by BNT162b2. Preprint at medRxiv. https://doi.org/10.1101/2021.02.08.21251329.
McEllistrem MC, Clancy CJ, Buehrle DJ, Lucas A, Decker BK. Single dose of an mRNA SARS-CoV-2 vaccine is associated with lower nasopharyngeal viral load among nursing home residents with asymptomatic COVID-19. Clin Infect Dis. 2021;73(6):e1365–7. https://doi.org/10.1093/cid/ciab263.
US Centers for Disease Control and Prevention. COVID-19 interim public health recommendations for fully vaccinated people. 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated-guidance.html. Accessed 28 May 2021.
Denzer O, Nienaber M. Germany drops incidence levels as key COVID yardstick. 2021. Reuters. https://www.reuters.com/world/europe/german-drop-incidence-levels-key-covid-yardstick-sources-2021-08-23/. Accessed 1 Sept 2021.
Bugin K, Woodcock J. Trends in COVID-19 therapeutic clinical trials. Nat Rev Drug Discov. 2021;20(4):254–5. https://doi.org/10.1038/d41573-021-00037-3.
Bedford J, Farrar J, Ihekweazu C, Kang G, Koopmans M, Nkengasong J. A new twenty-first century science for effective epidemic response. Nature. 2019;575(7781):130–6. https://doi.org/10.1038/s41586-019-1717-y.
Alam U, Nabyonga-Orem J, Mohammed A, Malac DR, Nkengasong JN, Moeti MR. Redesigning health systems for global heath security. Lancet Glob Heal. 2021;9(4):e393–4. https://doi.org/10.1016/S2214-109X(20)30545-3.
Darby AC, Hiscox JA. Covid-19: variants and vaccination. BMJ. 2021:372n771. https://doi.org/10.1136/bmj.n771.
Fontanet A, Autran B, Lina B, Kieny MP, Karim SSA, Sridhar D. SARS-CoV-2 variants and ending the COVID-19 pandemic. Lancet. 2021;397(10278):952–4. https://doi.org/10.1016/S0140-6736(21)00370-6.
Tarke A, Sidney J, Methot N, Yu ED, Zhang Y, Dan JM, et al. Impact of SARS-CoV-2 variants on the total CD4+ and CD8+ T cell reactivity in infected or vaccinated individuals. Cell Reports Med. 2021;2(7):100355. https://doi.org/10.1016/j.xcrm.2021.100355.
Ledford H. How ‘killer’ T cells could boost COVID immunity in face of new variants. Nature. 2021;590(7846):374–5. https://doi.org/10.1038/d41586-021-00367-7.
Acknowledgments
We thank Karina Escandón for designing the figure for this manuscript. We acknowledge Arthur Allen, Arlyne Beeche, Richard Cash, Julia Marcus, Malcolm Potts, Josh Sharfstein, Ann Swidler, Muhammad Usman, Zeynep Tufekci, and David Wolfson for their useful comments. This article was first preprinted in April 2021 at https://osf.io/nrvtf/ and was continuously updated until publication date.
Funding
This article did not receive any funding or sponsorship for publication.
Author information
Authors and Affiliations
Contributions
DTH initially conceptualized the article and led the manuscript development. All authors (DTH, NH, SH, RCB, JDK, HJ, RW, JAL, MO, SB, KE, and MG) contributed to the writing of the manuscript, critically revised subsequent versions, and agreed upon the final version of this manuscript prior to submission. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Dr. Kevin Escandón and Dr. Stefan Baral are Senior Editorial Board Members for BMC Infectious Diseases. These authors were not involved in any of the decisions regarding review of the manuscript or its acceptance. Two in-house Editors for the BMC Series and two anonymous expert reviewers assessed this manuscript. Dr. Jeffrey D. Klausner serves as an independent medical director of Curative, Inc., a SARS-CoV-2 testing and vaccination company. The other authors declare no conflicts of interest. The authors confirm that they have read BMC’s guidance on competing interests. Views expressed here are solely those of the authors and do not represent the position or policy of any institution or organization.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Halperin, D.T., Hearst, N., Hodgins, S. et al. Revisiting COVID-19 policies: 10 evidence-based recommendations for where to go from here. BMC Public Health 21, 2084 (2021). https://doi.org/10.1186/s12889-021-12082-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-021-12082-z