Abstract
Objectives
Sexually transmitted infections (STIs) are a major cause of morbidity. Understanding drivers of transmission can inform effective prevention programs. We describe STI prevalence and identify factors associated with STIs in four African countries.
Methods
The African Cohort Study is an ongoing, prospective cohort in Kenya, Nigeria, Tanzania and Uganda. At enrollment, a physical exam was conducted and STI diagnosis made by a clinician using a syndromic management approach. Multivariable logistic regression was used to estimate adjusted odds ratios (aORs) and 95% confidence intervals (95% CIs) for factors associated with an STI diagnosis.
Results
As of June 2020, 3544 participants were enrolled. STI prevalence was 7.7% and did not differ by HIV status (p = 0.30). Prevalence differed by syndrome (3.5% vaginal discharge, 1.5% genital ulcer, 2.1% lower abdominal pain, 0.2% inguinal bubo). The odds of having an STI were higher at all sites compared to Kisumu West, Kenya, and among those with a primary level education or below compared to those with secondary or higher (aOR: 1.77; 95% CI: 1.32–2.38). The odds of an STI diagnosis was higher among participants 18–29 years (aOR: 2.29; 95% CI: 1.35–3.87), females (aOR: 2.64; 95% CI: 1.94–3.59), and those with depression (aOR: 1.78; 95% CI: 1.32–2.38). Among PLWH, similar factors were independently associated with an STI diagnosis. Viral suppression was protective against STIs (aOR: 2.05; 95% CI: 1.32–3.20).
Conclusions
Prevalence of STIs varied by site with young people and females most at risk for STIs. Mental health is a potential target area for intervention.
Similar content being viewed by others
Key messages
-
Syndromically managed STIs are uniquely relevant as clinical diagnosis is the standard of care in most resource-limited settings
-
Young people and women were most at risk for STIs in this setting
-
Robust mental health programming targeting depression and anxiety may decrease STI transmission in this population
Introduction
Globally, there is an estimated 376.4 million new cases of curable sexually transmitted infections (STIs), including Chlamydia trachomatis, Neisseria gonorrhoeae, syphilis and Trichomonas vaginalis among people aged 15–49 years, every year [1]. The WHO estimates that sub-Saharan Africa bears approximately 40% of the global burden of STIs [2]. Symptomatic and asymptomatic STIs are a major cause of morbidity in developing countries and can cause infertility, cervical cancer, pelvic inflammatory disease and pregnancy complications [3]. Furthermore, evidence suggests that STIs can increase the risk of acquisition and transmission of HIV [4,5,6,7].
Understanding the factors that drive STI transmission is important to implementing effective STI prevention programs, particularly in high HIV-burden settings. Several studies from Sub-Saharan Africa have identified women of reproductive age as at high risk for STIs [8]. Socio-behavioral risk factors for STIs in this group include low levels of education, not being married, multiple sex partners, alcohol and drug use, and early sexual debut [8,9,10,11]. Additionally, key populations such as men who have sex with men, transgender women, and commercial sex workers are at increased risk of STI acquisition [12, 13].
Few studies from high HIV-burden settings have addressed STI prevalence and management. The African Cohort Study (AFRICOS) addresses this paucity of data by examining STI diagnoses from four high HIV-burden African countries. In AFRICOS, STIs are diagnosed using a syndromic management clinical approach. In many low- and middle-income countries, including in Africa, a syndromic management approach is often used to diagnose and treat STIs without employing laboratory techniques [14].] Despite substantial drawbacks to this method, including lower sensitivity syndromic management of STIs are uniquely relevant as clinical diagnosis is the standard of care in most resource-limited settings [15, 16].
The aim of this study was to describe STI prevalence and identify factors associated with STI diagnosis in AFRICOS.
Materials and methods
Study design and participants
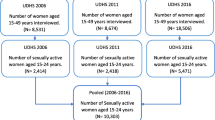
These analyses utilized data from AFRICOS, an ongoing, multi-site, prospective cohort study that has been described previously [17]. In brief, since 2013, AFRICOS has enrolled persons living with HIV (PLWH) and those at risk for HIV in 12 clinical sites across five programs in four countries: South Rift Valley, Kenya; Kisumu West, Kenya; Nigeria; Tanzania; and Uganda. The South Rift Valley site is comprised of six sites- Kericho District Hospital, Tenwek Mission Hospital, Kapkatet District Hospital, AC LITEIN Mission Hospital, Nandi Hills District Hospital, and Kapsabet District Hospital. The Kisumu West, Kenya site is based in the Kisumu West District Hospital, a Ministry of Health District Hospital in Kombewa, Kenya. The Nigerian sites are located in Abuja and Lagos, Nigeria. The Tanzania AFRICOS site is located at the National Institute for Medical Research-Mbeya Medical Research Center. The Uganda site is housed in the Kayunga District Hospital. Participants living with HIV were randomly selected from current client lists or were new enrollees to the clinic with a small subset (9%) recruited from previous HIV research studies. To recruit participants at risk for HIV, adult partners of AFRICOS enrollees living with HIV and seronegative adults from the community or program counseling and testing activities were offered enrollment. All non-pregnant, current clinic patients, 18 years and older, and consenting to data and specimen collection were eligible for inclusion in AFRICOS. This analysis included PLWH and HIV-uninfected participants enrolled in AFRICOS. Patients and the public were not involved in the design or conduct of the study, choice of outcome measures or recruitment to the study.
The study was approved by the institutional review boards of the Walter Reed Army Institute of Research (#1897), Makerere University School of Public Health (#173), Uganda National Committee of Science and Technology (HS-1175), Kenya Medical Research Institute Science and Ethics Review Unit (SSC# 2396, 2371), Tenwek Institutional Ethics Review Committee (SSC# 2371), Tanzania National Institute of Medical Research (NIMR/HQ/R.8a/Vol.1X/1060), Mbeya Medical and Research Ethics Committee (NIMR/HQ/R.8a/Vol.1X/1060), and Ministry of Defense Health Research and Ethics Committee (#3726112019). Research was performed in accordance with the Declaration of Helsinki. All participants gave written informed consent.
Data collection
At enrollment and biannual follow-up visits, participants received a clinical assessment, and an extensive demographic and socio-behavioral questionnaire was administered by trained study staff. Demographic and socio-behavioral variables included HIV status, age, sex, education, marital status, condom use at last sex, alcohol and drug use, age at first sexual intercourse, number of sexual partners and depression. Depression was assessed at enrollment and subsequent visits using the 20-item Center for Epidemiological Studies-Depression (CES-D) scale [18]. We employed a cutoff point of 16 or greater to identify individuals at risk for clinical depression [19].
Additional variables collected for PLWH included antiretroviral therapy (ART) status, ART adherence based on the self-reported number of days doses were missed in the past month, and HIV-related stigma, defined as experiencing any of the following: social isolation, physical violence, broken family relationships. ART status and regimen history was obtained at enrollment from medical record review and updated prospectively every 6 months. Syphilis testing was performed using country specific guidelines utilizing rapid plasma regain (RPR) as the initial (nontreponemal) screening test. Viral load testing was performed at enrollment and every 6 months for PLWH using nucleic acid amplification methods on one of several testing platforms with lower limit of quantification 20–48 copies/mL [20]. Viral suppression was defined as a viral load < 200 copies/mL.
During the clinical assessment, participants were asked about any symptoms potentially consistent with STIs in the last 2 weeks. An STI was diagnosed by any of the following: vaginal or penile discharge; genital ulcer; blood in urine; burning/painful urination; vaginal itching; painful intercourse; lower abdominal pain; swollen lymph nodes at groin; genital warts; and/or post coital bleeding. We additionally assessed prevalence of the following syndromes: vaginal discharge, genital ulcer, lower back pain, and inguinal bubo [14].
Data were entered and verified in the ClinPlus platform (Anju Software, Tempe, AZ).
Statistical analyses
Covariates were included based on clinical significance and factors previously identified in the literature to be associated with symptomatic STIs. These included age, sex, HIV status, education level, marital status, age at first sexual intercourse, number of partners, condom use at last sex, alcohol and drug use, and depression. Taking ART or not, ART adherence, stigma, and viral suppression were also considered for the subgroup of PLWH. These analyses were restricted to observations with non-missing data for the outcome variable and all variables included in the fully adjusted models.
Chi-squared tests for categorical variables and student’s t-tests for continuous variables were used to describe differences between those who were and were not diagnosed with an STI at enrollment. Logistic regression analysis was used to estimate unadjusted and adjusted odds ratios (ORs) and 95% confidence intervals (95% CIs) for factors associated with the presence of an STI at the enrollment visit. Backwards stepwise selection with a significance level of 0.10 was used to remove variables from the adjusted model. Modelling was repeated stratifying by study site. To evaluate HIV-specific factors, a subgroup analysis was performed among PLWH.
All analyses were performed in SAS version 9.4 (SAS Institute, Cary, North Carolina) and Stata version 16.0 (StataCorp, College Station, Texas) software.
Results
Study population characteristics
From 23 January 2013 to 1 June 2020, 3550 participants had been enrolled into the study, of whom 3544 (99.8%) were complete cases and included in these analyses. Of these 2931 (82.7%) were PLWH and 615 (17.3%) were at risk for HIV. Participants differed in key demographic characteristics by study site including greater proportion of females enrolled in Tanzania (64.0%), younger age in Nigeria, and a higher percentage of participants with at least a secondary education in Nigeria (88.4%) and South Rift Valley, Kenya (50.4%; Supplemental Table 1). STI prevalence did not vary significantly by HIV status but was numerically higher among PLWH as compared to HIV-uninfected participants, 7.9 and 6.7% respectively (p = 0.30). Prevalence differed by syndrome (3.5% vaginal discharge, 1.5% genital ulcer, 2.1% lower abdominal pain, 0.2% inguinal bubo).
At enrollment, STI prevalence varied significantly by site, age, education level, sex, marital status, condom use at last sex with regular and casual partners, age at first sexual intercourse, drug use and depression (Table 1). Kisumu, Kenya had the lowest prevalence of STIs with 11 cases (1.8%) while Kayunga, Uganda had the highest prevalence with 136 cases (21.3%; p < 0.001). STI prevalence was highest among the youngest participants aged 18–29 years (9.8%) and lowest among the oldest age group, those aged 50 years and older (3.8%; p < 0.001). STI prevalence was higher among those with a primary level education or less (8.9% vs 6.1% p = 0.002), females (10.4% vs 4.0%; p < 0.001), participants who were not married 9.2% vs 6.6%; p = 0.004), had no reported drug use (7.9% vs 1.9%; p = 0.024) and had depression (11.9% vs 6.7%; p < 0.001). STI prevalence was also higher among participants who reported not using condoms with their regular partner (10.9% vs 5.5%; p < 0.001), not using condoms with their casual partner (12.7% vs 7.8%; p = 0.020) and among those who were 16 years or younger at first sexual intercourse (8.9% vs 7.0%; p = 0.042).
Among the subgroup of PLWH, STI prevalence was higher among those with poor adherence or who were not on ART (6.8 and 14.7% vs 4.7%; p < 0.001) and among those who were virally unsuppressed at a level of 200 copies/mL or less (7.7% vs 4.1%; p < 0.001).
Factors associated with STI diagnosis
Factors independently associated with an STI diagnosis at enrollment among all participants included site, age, sex, education level and depression (Table 2). As compared to Kisumu West, Kenya, the odds of being diagnosed with an STI at enrollment were higher for participants at the South Rift Valley Kenyan, Uganda, Tanzanian and Nigerian sites (South Rift Valley, Kenya aOR:3.03; 95% CI 1.56–5.88, Uganda aOR: 16.26; 95% CI 8.65–30.55, Tanzania aOR 3.70; 95% CI: 1.88–7.29, Nigeria aOR: 5.84; 95% CI 2.78–12.28). Participants in the youngest age group, 18–29 years, had higher odds of being diagnosed with an STI at enrollment compared to the oldest age group, those 50 years and older (aOR: 2.29; 95% CI: 1.35–3.87). Females had higher odds of being diagnosed with an STI compared to males (aOR: 2.64; 95% CI: 1.94–3.59). Those with a primary level education or lower had a higher odds of being diagnosed with an STI as compared to those with a secondary level education or higher (aOR: 1.41; 95% CI: 1.05–1.90). Those with depression were had higher odds of being diagnosed with an STI at enrollment (aOR: 1.78; 95% CI: 1.32–2.38).
Stratifying by site, we found that sex was the only factor included in all models across all sites (Table 3). There were no significant factors associated with STI prevalence in Kisumu West, Kenya due to the limited power with the small number of participants with an STI diagnosis from this site. Participants from the Tanzania and Nigeria sites who had an early sexual debut ≤16 years of age had increased odds of STI at enrollment (aOR Tanzania: 2.91, 95% CI: 1.48–5.70; aOR Nigeria: 3.29, 95% CI: 1.33–8.16) compared to those with a later sexual debut.
Similar factors were found to be independently associated with prevalent STIs among PLWH, including site, age, and sex (Table 4). Viral suppression at ≥200 copies/mL was found to be protective against STIs as compared to those with a viral load < 200 copies/mL (aOR: 2.06; 95% CI: 1.32–3.21). Additionally, PLWH with depression had a 63% higher odds of being diagnosed with an STI at enrollment than those without depression (aOR: 1.63; 95% CI: 1.18–2.26).
Discussion
The overall prevalence of syndromic STIs in this multi-country cohort in four sub-Saharan African countries was 7.7% and did not differ significantly by HIV status. Global estimates based on a systematic review of 130 studies, estimate that in 2016, the prevalence of diagnosed STIs was lower than our findings for symptomatic STIs. However, when restricting to the African region only, prevalence was similar although varied by pathogen [1]. A cross-sectional study in another high-HIV prevalence setting found a higher prevalence of STIs and similar findings of no association with HIV status [8]. Another meta-analysis of 18 HIV prevention studies of women found that the prevalence of these four STIs varied by age and clinic or community setting [21]. Few recent studies have assessed the overall burden of syndromically managed STIs in Africa.
This study found a higher prevalence of symptomatic STIs among female participants compared to males. Other studies conducted in sub-Saharan Africa have similarly found that females have a higher prevalence of STIs compared to males in both surveillance and cross-sectional studies [22, 23]. Females may be at increased risk for STIs for several reasons. Gender inequities may reduce educational and economic opportunities for women and encourage risky sexual behavior such as engagement in transactional sex and decreased bargaining power for condom use during sex [24]. Biological factors such as vaginal microbiota and thinner vaginal lining may also put women at increased risk of STI acquisition compared to men [25]. Women are particularly vulnerable to STI acquisition and should be a priority target population, especially those of childbearing age for whom STIs can cause severe morbidity and pregnancy complications.
The prevalence of STIs was highest among those aged 18–29 years old. Other studies have found elevated STI prevalence among young women across various regions and populations [21]. A study among men who have sex with men and transgender women in Nigeria found that Chlamydia and gonorrhea were about twice as common in participants younger than 30 years old compared to those 30 years and older [26]. It is evident that young people are at high risk for STIs and should be a primary target population for intervention. Other studies have shown that cash transfer programs, whereby individuals are given a sum of money either unconditionally or conditionally on an action like attending school, can be effective in reducing STI infections among young women and should be explored in this population [27, 28].
The interaction of mental health and high-risk sexual behavior is well established in resource rich countries. However, this interaction has been poorly studied in Africa. A prior study of key populations affected by HIV in Nigeria suggested that stigmatizing experiences and mental health issues increase STI risk through pathways that include decreased condom use [29]. We have previously reported that depression was associated with decreased ART adherence and elevated viral loads among AFRICOS participants living with HIV [30]. Our data suggest an association between depression, viral non-suppression and an increased risk of STIs. This potentially represents a robust target for intervention as only 10% of persons living in Sub-Saharan Africa have adequate access to mental health care [31]. Integrating care, such as mental health services and behavioral counseling for STI prevention, may be an effective and cost-effective intervention to reduce STIs [32].
Differences in the burden of STIs observed across clinical care site may reflect other social, structural, or cultural nuances that may affect STI transmission and acquisition but that we were unable to capture adequately. Future studies should interrogate site-specific factors to identify those that could potentially reduce the risk of STIs.
Limitations
This study helps fill a gap in the literature by examining syndromic management of STIs from four high HIV-burden African countries; however, several limitations of these analyses are acknowledged. The syndromic management approach to STI diagnosis used in this study is uniquely relevant as it is the standard of care in most resource-limited settings. However, it likely underestimates the true STI burden [3, 26]. In addition, participants enrolled in a clinic-based cohort study are more likely to be connected to a healthcare system and may have better access to condoms and counseling on condom use than the general population [33]. We also addressed missing data by using complete cases only which potentially can introduce bias. However, as the data were missing at random we believe that the bias is minimal. Our list of genitourinary symptoms was broader than that utilized in STI syndromic management and thus may be at greater risk of false positives. Lastly, these cross-sectional analyses only captured STI diagnoses at a single point in time. Further analyses should utilize longitudinal data to understand factors associated with incident STIs and persistent infection.
Conclusion
This study identified individuals at high risk for STIs as well as target areas for potential future intervention. Young people and women were most at risk for STIs and should be a focus of future interventions due to the implications of untreated STIs in pregnant women. Additionally, programs focused on women’s health may improve outcomes in all groups. Persons with depression were also identified to be at higher risk for STIs, thus robust mental health programming targeting depression/anxiety may decrease STI transmission.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to privacy protections but are available from the corresponding author on reasonable request. The Henry M. Jackson Foundation for the Advancement of Military Medicine (HJF) and the Water Reed Army Institute of Research (WRAIR) are committed to safeguarding the privacy of research participants. Distribution of data will require compliance with all applicable regulatory and ethical processes, including establishment and approval of an appropriate data-sharing agreement. To request a minimal data set, please contact the data coordinating and analysis center (DCAC) at PubRequest@hivresearch.org and indicate the RV329 study along with the name of the manuscript.
Abbreviations
- AFRICOS:
-
African Cohort Study
- ART:
-
Antiretroviral therapy
- CESD:
-
Center for Epidemiological Studies-Depression
- CIs:
-
Confidence intervals
- OR:
-
Odds ratio
- PLWH:
-
People living with HIV
- STI:
-
Sexually transmitted infection
References
Rowley J, Vander Hoorn S, Korenromp EL, Low N, Unemo M. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ. 2019;97(8):548–62. https://doi.org/10.2471/BLT.18.228486.
World Health Organization. Global Health Sector Strategy on Sexually Transmitted Infections, 2016–2021. 2016. Available from: https://www.who.int/publications/i/item/WHO-RHR-16.09.
Francis SC, Mthiyane TN, Baisley K, Mchunu SL, Ferguson JB, Smit T, et al. Prevalence of sexually transmitted infections among young people in South Africa: a nested survey in a health and demographic surveillance site. PLoS Med. 2018;15(2):1–25.
Wilkinson D, Abdool Karim SS, Harrison A, Lurie M, Colvin M, Connolly C, et al. Unrecognized sexually transmitted infections in rural south African women: a hidden epidemic. Bull World Health Organ. 1999;77(1):22–8.
Ward-Peterson M, Fennie K, Mauck D, Shakir M, Cosner C, Bhoite P, et al. Using multilevel models to evaluate the influence of contextual factors on HIV/AIDS, sexually transmitted infections, and risky sexual behavior in sub-Saharan Africa: a systematic review. Ann Epidemiol. 2018;28(2):119–34 Available from: https://www.ncbi.nlm.nih.gov/pubmed/29439782.
Galvin S, Cohen M. The role of sexually transmitted diseases in HIV transmissione. Nat Rev Microbiol. 2004;2(1):33–42. https://doi.org/10.1038/nrmicro794.
Crowell TA, Lawlor J, Lombardi K, Nowak RG, Hardick J, Odeyemi S, et al. Anorectal and Urogenital Mycoplasma genitalium in Nigerian Men Who Have Sex With Men and Transgender Women: Prevalence, Incidence, and Association With HIV. Sex Transm Dis. 2020;47(3):202–6. https://doi.org/10.1097/OLQ.0000000000001105.
Ginindza TG, Stefan CD, Tsoka-Gwegweni JM, Dlamini X, Jolly PE, Weiderpass E, et al. Prevalence and risk factors associated with sexually transmitted infections (STIs) among women of reproductive age in Swaziland. Infect Agent Cancer. 2017;12(1):1–12.
Kakaire O, Byamugisha JK, Tumwesigye NM, Gamzell-Danielsson K. Prevalence and factors associated with sexually transmitted infections among HIV positive women opting for intrauterine contraception. PLoS One. 2015;10(4):1–12.
Oyeyemi O, Fadipe O, Oyeyemi I. Trichomonas vaginalis infection in Nigerian pregnant women and risk factors associated with sexually transmitted infections. Int J STD AIDS. 2015;27(13):1187–93. https://doi.org/10.1177/0956462415611292.
Fatusi A, Wang W. Multiple sexual partnership mediates the association between early sexual debut and sexually transmitted infection among adolescent and young adult males in Nigeria. Eur J Contracept Reprod Heal Care. 2009;14(2):134–43. https://doi.org/10.1080/13625180802601110.
Mayer KH, Allan-Blitz L. Similar, but different: drivers of the disproportionate HIV and sexually transmitted infection burden of key populations. J Int AIDS Soc. 2019;22(S6):e25344.
Rieg G, Lewis R, Miller L, Witt MD, Guerrero M, Daar ES. Asymptomatic sexually transmitted infections in HIV-infected men who have sex with men : and screening strategies. AIDS Patient Care STDs. 2008;22(12):947–54. https://doi.org/10.1089/apc.2007.0240.
World Health Organization. Guidelines for the management of sexually transmitted infections. 2004. Available from: https://www.who.int/hiv/pub/sti/pub6/en/.
Garrett NJ, Osman F, Maharaj B, Naicker N, Gibbs A, Norman E, et al. Beyond syndromic management : opportunities for diagnosis-based treatment of sexually transmitted infections in low- and middle-income countries. PLoS One. 2018:13(4);1–13.
Wi TEC, Ndowa FJ, Ferreyra C, Kelly-cirino C, Toskin I, Kiarie J, et al. Diagnosing sexually transmitted infections in resource- constrained settings: challenges and ways forward. J Int AIDS Soc. 2019;22(56):8–18.
Ake JA, Polyak CS, Crowell TA, Kiweewa F, Semwogerere M, Maganga L, et al. Noninfectious comorbidity in the African cohort study. Clin Infect Dis. 2019;69(4):639–47. https://doi.org/10.1093/cid/ciy981.
Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. https://doi.org/10.1177/014662167700100306.
Lewinsohn P, Seeley J, Roberts R, Allen N. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997;12(2):277–87. https://doi.org/10.1037/0882-7974.12.2.277.
Esber A, Polyak C, Kiweewa F, Maswai J, Owuoth J, Maganga L, et al. Persistent Low-level Viremia predicts subsequent Virologic failure: is it time to change the third 90? Clin Infect Dis. 2019;69(5):805–12. https://doi.org/10.1093/cid/ciy989.
Torrone EA, Morrison CS, Chen PL, Kwok C, Francis SC, Hayes RJ, et al. Prevalence of sexually transmitted infections and bacterial vaginosis among women in sub-Saharan Africa: An individual participant data meta-analysis of 18 HIV prevention studies. PLoS Medicine. 2018;15:1–38.
Sabri B, Wirtz AL, Ssekasanvu J, Nonyane BAS, Nalugoda F, Kagaayi J, et al. Intimate partner violence, HIV and sexually transmitted infections in fishing, trading and agrarian communities in Rakai, Uganda. BMC Public Health. 2019;19(1):1–16.
Korenromp EL, Mahiané G, Rowley J, Nagelkerke N, Abu-Raddad L, Ndowa F, et al. Estimating prevalence trends in adult gonorrhoea and syphilis in low- and middle-income countries with the Spectrum-STI model: results for Zimbabwe and Morocco from 1995 to 2016. Sex Transm Infect. 2017;93(8):599–606. https://doi.org/10.1136/sextrans-2016-052953.
Mbonye M, Nalukenge W, Nakamanya S, Nalusiba B, King R, Vandepitte J, et al. Gender inequity in the lives of women involved in sex work in Kampala , Uganda. J Int AIDS Soc. 2012;15(Suppl 1):1–9.
Brotman RM. Vaginal microbiome and sexually transmitted infections: an epidemiologic perspective. J Clin Invest. 2011;121(12):4610–7. https://doi.org/10.1172/JCI57172.
Keshinro B, Crowell TA, Nowak RG, Adebajo S, Peel S, Gaydos CA, et al. High prevalence of HIV, chlamydia and gonorrhoea among men who have sex with men and transgender women attending trusted community centres in Abuja and Lagos, Nigeria. J Int AIDS Soc. 2016;19(1):1–9.
De Walque D, Dow WH, Nathan R, Abdul R, Abilahi F, Gong E, et al. Incentivising safe sex: A randomised trial of conditional cash transfers for HIV and sexually transmitted infection prevention in rural Tanzania. BMJ Open. 2012;2(1):e000747.
Baird SJ, Garfein RS, McIntosh CT, Özler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet. 2012;379(9823):1320–9. Available from:. https://doi.org/10.1016/S0140-6736(11)61709-1.
Rodriguez-Hart C, Nowak RG, Musci R, German D, Orazulike I, Kayode B, et al. Pathways from sexual stigma to incident HIV and and sexually transmitted infections among Nigerian men who have sex with men. AIDS. 2017;31(17):2415–20. https://doi.org/10.1097/QAD.0000000000001637.
Meffert SM, Neylan TC, McCulloch CE, Maganga L, Adamu Y, Kiweewa F, et al. East African HIV care: depression and HIV outcomes. Glob Ment Heal. 2019;6:e9.
Ulanja MB, Lyons C, Ketende S, Stahlman S, Diouf D, Kouamé A, et al. The relationship between depression and sexual health service utilization among men who have sex with men ( MSM ) in Côte d ’ Ivoire , West Africa. BMC Int Health Hum Rights. 2019;19(11):1–11.
Brookmeyer K, Hogben M, Kinsey J. The rold of behavioral counseling in STD prevention program settings. Sex Transm Dis. 2016;43(1):S102–12. https://doi.org/10.1097/OLQ.0000000000000327.
Analogbei T, Dear N, Reed D, Esber A, Akintunde A, Bahemana E, et al. Predictors and Barriers to Condom Use in the African Cohort Study. AIDS Patient Care STDS. 2020;34(5):228–36.
Acknowledgements
We thank the study participants, local implementing partners, and hospital leadership at Kayunga District Hospital, Kericho District Hospital, AC Litein Mission Hospital, Kapkatet District Hospital, Tenwek Mission Hospital, Kapsabet District Hospital, Nandi Hills District Hospital, Kisumu West District Hospital, Mbeya Zonal Referral Hospital, Mbeya Regional Referral Hospital, Defence Headquarters Medical Center, and the 68th Nigerian Army Reference Hospital.
We would also like to thank the AFRICOS Study Team – from the US Military HIV Research Program Headquarters team: Danielle Bartolanzo, Alexus Reynolds, Katherine Song, Mark Milazzo, Leilani Francisco, Shauna Mankiewicz, Steven Schech, Alexandra Golway, Badryah Omar, Tsedal Mebrahtu, Elizabeth Lee, Kimberly Bohince, Ajay Parikh, Jaclyn Hern, Emma Duff, Kara Lombardi, Michelle Imbach, and Leigh Anne Eller; from the AFRICOS Uganda team: Hannah Kibuuka, Michael Semwogerere, Prossy Naluyima, Godfrey Zziwa, Allan Tindikahwa, Hilda Mutebe, Cate Kafeero, Enos Baghendaghe, William Lwebuge, Freddie Ssentogo, Hellen Birungi, Josephine Tegamanyi, Paul Wangiri, Christine Nabanoba, Phiona Namulondo, Richard Tumusiime, Ezra Musingye, Christina Nanteza, Joseph Wandege, Michael Waiswa, Evelyn Najjuma, Olive Maggaga, Isaac Kato Kenoly, and Barbara Mukanza; from the AFRICOS South Rift Valley, Kenya team: Jonah Maswai, Rither Langat, Aaron Ngeno, Lucy Korir, Raphael Langat, Francis Opiyo, Alex Kasembeli, Christopher Ochieng, Japhet Towett, Jane Kimetto, Brighton Omondi, Mary Leelgo, Michael Obonyo, Linner Rotich, Enock Tonui, Ella Chelangat, Joan Kapkiai, Salome Wangare, Zeddy Bett Kesi, Janet Ngeno, Edwin Langat, Kennedy Labosso, Joshua Rotich, Leonard Cheruiyot, Enock Changwony, Mike Bii, Ezekiel Chumba, Susan Ontango, Danson Gitonga, Samuel Kiprotich, Bornes Ngtech, Grace Engoke, Irene Metet, Alice Airo, and Ignatius Kiptoo; from the AFRICOS Kisumu, Kenya team: John Owuoth, Valentine Sing’oei, Winne Rehema, Solomon Otieno, Celine Ogari, Elkanah Modi, Oscar Adimo, Charles Okwaro, Christine Lando, Margaret Onyango, Iddah Aoko, Kennedy Obambo, Joseph Meyo, and George Suja; from the AFRICOS Abuja, Nigeria team: Michael Iroezindu, Yakubu Adamu, Nnamdi Azuakola, Mfreke Asuquo, Abdulwasiu Bolaji Tiamiyu, Afoke Kokogho, Samirah Sani Mohammed, Ifeanyi Okoye, Sunday Odeyemi, Aminu Suleiman, Lawrence Umejo, Onome Enas, Miriam Mbachu, Ijeoma Chigbu-Ukaegbu, Wilson Adai, Felicia Anayochukwu Odo, Rabi Abdu, Rosemary Akiga, Helen Nwandu, CHisara Okolo, Ndubuisis Okeke; from the AFRICOS Lagos, Nigeria team: Zahra Parker, Asogwa Ugochukwu Linus, Concilia Amaka Agbaim, Tunde Adegbite, Nkenchiere Harrison, Adewale Adelakun, Ekeocha Chioma, Victoria Idi, Rachel Eluwa, Jumoke Nwalozie, Igiri Faith, Blessing Okanigbuan, Achugwo Emmanuel, Nkiru Nnadi, Ndubuisi Rosemary, Uzoegwu Amaka Natalie, Obende Theresa Owanza, Falaju Idowu Francis, Jacintal Elemere, Obilor Ifeoma Lauretta, Edward Akinwale, and Inalegwu Ochai; from the AFRICOS Mbeya, Tanzania team: Lucas Maganga, Emmanuel Bahemana, Samoel Khamadi, John Njegite, Connie Lueer, Abisai Kisinda, Jaquiline Mwamwaja, Faraja Mbwayu, Gloria David, Mtasi Mwaipopo, Reginald Gervas, Doroth Mkondoo, Nancy Somi, Paschal Kiliba, Gwamaka Mwaisanga, Johnisius Msigwa, Hawa Mfumbulwa, Peter Edwin, Willyhelmina Olomi.
Disclaimer
The views expressed are those of the authors and should not be construed to represent the positions of the US Army or the Department of Defense. The investigators have adhered to the policies for protection of human subjects as prescribed in Army Regulation 70–25.
Funding
This work was supported by the President’s Emergency Plan for AIDS Relief via a cooperative agreement between the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc., and the U.S. Department of Defense [W81XWH-11-2-0174, W81XWH-18-2-0040].
Author information
Authors and Affiliations
Consortia
Contributions
MS, AE, and DR conceived of the presented research idea. EB, MS, HK, FK, JO, JM, and MI carried out the data collection, laboratory activities and reviewed the collected data for quality and reliability. AE, ND, and DR designed the model and the computational framework and analysed the data. MS, AE, TC, ND, JT and CP contributed to the interpretation of the results. MS took the lead in writing the manuscript. CP and JA were in charge of overall direction and planning. All authors provided critical feedback and helped shape the research, analysis and manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional review boards of the Walter Reed Army Institute of Research (#1897), Makerere University School of Public Health (#173), Uganda National Committee of Science and Technology (HS-1175), Kenya Medical Research Institute Science and Ethics Review Unit (SSC# 2396, 2371), Tenwek Institutional Ethics Review Committee (SSC# 2371), Tanzania National Institute of Medical Research (NIMR/HQ/R.8a/Vol.1X/1060), Mbeya Medical and Research Ethics Committee (NIMR/HQ/R.8a/Vol.1X/1060), and Ministry of Defense Health Research and Ethics Committee (#3726112019). Research was performed in accordance with the Declaration of Helsinki. All participants gave written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Table 1.
Study Population Characteristics at Enrollment Visit by Study Site.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Semwogerere, M., Dear, N., Tunnage, J. et al. Factors associated with sexually transmitted infections among care-seeking adults in the African Cohort Study. BMC Public Health 21, 738 (2021). https://doi.org/10.1186/s12889-021-10762-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-021-10762-4