Abstract
Background
There is limited research on HIV testing among older persons in Uganda. The aim of this study was to investigate the socio-demographic determinants of recent HIV testing among older persons in selected rural districts in Uganda.
Methods
A cross-sectional survey of 649 older men and women age 50 years and older, from central (Masaka district) and western (Hoima district) Uganda was conducted. Frequency distributions, chi-square tests and multivariable logistic regressions were used to examine the association between recent HIV testing and selected explanatory variables.
Results
Nearly six in ten (58%) of older persons had primary education. About 60% of the respondents were in union and 13% of them had two or more spouses. Half of the older people (51%) had sex in the last twelve months. A quarter (25%) of older persons gave or received gifts in exchange for sex in their lifetime. Nearly a third (29%) reported sexually transmitted infections in the last 12 months. Prevalence of lifetime HIV testing was 82% and recent (last 12 months) HIV testing was 53%. HIV testing in the last 12 months was associated with age (OR = 0.50; 95% CI: 0.31–0.79), self-reported sexually transmitted infections (OR = 1.59; 95% CI: 1.00–2.30), male circumcision (OR = 1.71; 95% CI: 1.0–2.93), and sexual activity in the last 12 months (OR = 2.89; 95% CI: 1.83–4.57).
Conclusion
Recent HIV testing among older persons was associated with younger age, self-reported STIs, male circumcision, and sexual activity among older persons in rural Uganda. HIV testing interventions need to target older persons who are 70 years and older, who were less likely to test.
Similar content being viewed by others
Background
The African Union framework on Ageing (AU-Plan) defines older persons as those age 60 years and older [1]. In Uganda, during the drafting of the policy for older persons in 2009, age 60 years and older was used [2, 3]. In this study, we used the World Health Organization (WHO) recommendation of using age 50 and older to define older persons [4]. Subsequently, several studies adopted age 50 and older, as an appropriate definition of old age in sub-Saharan Africa (SSA) countries including Kenya [5, 6]; Uganda [7] and South Africa [8] and those of the WHO Study on global AGEing and adult health (SAGE) and the INDEPTH network [9,10,11,12,13,14].
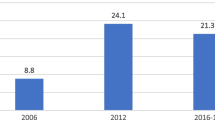
Globally, the proportion of older persons (age 60 years and older) in 2017 was 13% of the total population [15]. This proportion is projected to increase to 30% by 2050 [16]. Globally, the absolute number of older people increased from 205 million in 1950 to 810 million in 2012 and is anticipated to increase further to 1 billion by 2022 and to 2 billion by 2050 – outnumbering children aged 0–14 years [17,18,19]. The highest proportion of older persons is projected to live in developing countries by 2050 [20].
In Uganda, the proportion of older persons age 50 years and older was estimated at 7.6% in the 2014 Uganda Population and Housing Census (UBOS, 2014). There has been some growth in the absolute number of older people in Uganda from 1.1 million in 2002 (4.5% of the population) to 1.3 million in 2010 (out of 30 million) and is expected to increase to 5.5 million (constituting 5.7% of the population) by 2050 [3, 18].
HIV in old age is an emerging public health challenge [21] and considered as a “hidden epidemic” globally [22]. In SSA, only 45% of the general population who are HIV positive know their status [23, 24]. This is far from the UNAIDS ambitious target of ensuring that 90% of those who are HIV positive know their status [25]. With regard to older persons, it is not easy to estimate the prevalence of HIV and the proportion of those who know their HIV status in SSA in general and Uganda in particular [26]. HIV in old age has two major pathways namely; ageing with HIV and infections in old age (Scholten et al., 2011). Ageing with HIV is attributed to adherence to antiretroviral therapy (ART) [27,28,29].
Prevalence of HIV among older persons is estimated at 11–13% globally [22, 30]. In sub-Saharan Africa, ten countries (mostly in southern and eastern Africa) account for 80% of all people living with HIV. These include: South Africa (25%), Nigeria (13%), Mozambique (6%), Uganda (6%), Tanzania (6%), Zambia (4%), Zimbabwe (6%), Kenya (6%), Malawi (4%) and Ethiopia (3%) [31,32,33,34].
HIV testing varies across counties. Among older persons, HIV testing was nearly half (48%) in Uganda [26], 54% in South Africa [35], and 23% in Zimbabwe [36]. However, HIV testing programmes do not prioritize older persons. Yet many lack information on HIV prevention and rarely test for HIV/AIDS [31, 37, 38]. In addition, older persons experience stigma while accessing HIV testing services [37].
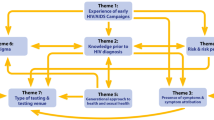
The determinants of HIV testing among older persons have been summarized in the conceptual model adapted from the healthcare utilization model. These include predisposing factors (age, gender, race / ethnicity, education, household income, employment status), enabling factors (health insurance, access to care, previous testing, seeing a doctor) and need factors especially HIV risk behaviours in the past 12 months [39,40,41,42].
Gender is a significant determinant of HIV testing among older persons, where older women are more likely to test for HIV compared to older men [43]. Among older persons, advanced age has been associated with reduced odds of HIV testing [44]. The perceived risk of contracting HIV is an important predictor of HIV testing, where a low perceived risk is associated with reduced odds of HIV testing [45]. Among older persons, prior history of testing reduces the odds of subsequent HIV testing [44].
A high level of education increases the odds of HIV testing among older people. With regard to marital status, HIV testing is higher among ever married persons outside union i.e. divorced or separated or widowed [26]. In addition, fear, emotional stress of positive HIV sero status results, HIV stigma [46] and knowledge of HIV transmission [37, 47] have been associated with HIV testing [37].
Despite the available evidence on HIV testing, there is dearth of information on HIV testing among older persons in developing countries in general and Uganda [48] in particular. In SSA, sources of data on HIV/AIDS such as Demographic and Health Surveys (DHS) and AIDS Indicator Surveys focus on age 15–54 years. The recent Uganda DHS, 2016 and Population and HIV Impact Surveys (PHIA) in 12 African countries also omit older persons [29, 33, 49]. In addition, several studies on the health of older people in Uganda have focused on later life problems associated with HIV/AIDS (Scholten et al., 2011; Seeley, Wolff, Kabunga, Tumwekwase, & Grosskurth, 2009) but not their uptake of HIV testing. There is need for language editing.
Therefore, the aim of this study was to investigate the determinants of access to HIV testing services among older persons in selected rural districts in Uganda. Findings are expected to contribute to understanding of factors associated with HIV testing among older persons [37, 38, 44, 50].
Methods
Study design and setting
The study used a cross-sectional and mixed methods study design. Both survey data and qualitative data were collected in February 2018. Qualitative data included focus group discussions and in-depth interviews. However, this paper is based on survey results. The study setting was in rural districts of Uganda: Masaka (central Uganda) and Hoima (western Uganda).
Study participants
Older persons were defined as those age 50 years and older as recommended by the World Health Organization [4]. We thus considered older persons 50 years and above who had the capacity to provide informed consent.
Sampling procedures
We used a multi-stage stratified cluster sampling design. We randomly selected two regions in Uganda namely: central and western regions out of the four administrative ones. Simple random sampling was used to select one district from each region: Masaka (central) and Hoima (western) from each region. We used the sampling frame of the 2014 Uganda Population and Housing Census [51] to select two sub-counties from Masaka [52] and three sub-counties from Hoima [53] using simple random sampling. From each sub-county, four enumeration areas or villages were selected using simple random sampling. The census sampling frame listed all enumeration areas in each sub-county. Using Microsoft office excel package, computer generated random numbers were assigned to all enumeration areas. Random numbers were used to randomly select enumeration areas. From each village, a sampling frame of older persons’ and their households was constructed in consultation with local leaders and systematic sampling was used to select participants for the survey. In households where older men and women live as couples, both were interviewed separately.
Kish’s formula [54] was applied to generate a sample size of 649 older persons for the survey. The prevalence of HIV testing for those age 50–59 years was 45% among men and 49% among women [55]. We used the lower bound of HIV testing (45%), the p = 0.45 and the q = 0.55. The level of confidence was set at 95% (z = 1.96) and the error at 8% (e = 0.008). The expected sample size was 148.5. The sample size was multiplied by the design effect of two (D = 2). Therefore, the expected sample size was 297. The final sample size after adjusting for a response rate of 90% became 330. To allow for small area (district) estimations, the sample size was multiplied by two since the study covered two districts. The overall sample size was 660 older persons. Due to non-response, the final sample size was 649 older persons. The number of older persons selected from each enumeration area was determined by probability proportionate sampling (PPS) from the 2014 Uganda census sampling frame [51].
Data collection procedures
Research assistants were trained for three days by the principal investigator. A pilot study / pre-testing of the tools was conducted in Wakiso town council. Feedback from pilot was integrated in revision of the tools – survey questionnaire and guides for qualitative data. The survey questionnaire was programmed in Android enabled tablets and the SurveyCTO online platform. The survey was conducted in Hoima and Masaka in February 2018. Two research teams (composed of five research assistants) were sent to each district at the same time to collect survey and qualitative data.
Data management using SurveyCTO
Survey data were collected using SurveyCTO [56] application installed on android enabled Tablets. Data were downloaded from the SurveyCTO Server as STATA files on daily basis.
Outcome variable
The outcome variable was recent HIV testing (last 12 months). Participants were asked if they had ever an HIV test in their life time (yes = 1, no =0) and if they tested for HIV in the last 12 months (yes =1 or no = 0). A follow up question was about reception of HIV results during the recent HIV test (yes or no responses). A binary variable called recent HIV testing was recoded to a binary variable (yes and no). Recent HIV testing means HIV testing and reception of results in the last 12 months.
Explanatory variables
Demographic variables included age, and sex. Age was recoded into three categories: 50–59, 60–69 and 70 and older. Sex was recoded into male and female.
Socio-economic variables included: education level (none, primary and secondary or higher), working in the last 12 months (yes and no), religion, marital status or currently in union, number of other wives, and children ever born and those currently alive. Religion was recoded as Catholics, Anglicans, Muslims and Others.
HIV related variables included knowledge about HIV transmission, HIV stigma, and need to test for HIV (yes or no). These questions were adopted from the Population HIV Impact Assessment (PHIA) survey [33] and the Demographic and Health survey [55]. To measure correct knowledge about HIV transmission, five questions were asked:
- 1.
Can the risk of HIV transmission be reduced by having sex with only one uninfected partner who has no other partners? (coded as yes =1, no = 0).
- 2.
A person can get HIV from mosquito bites? (coded as yes =0, no = 1).
- 3.
Can a person reduce their risk of getting HIV by using a condom every time they have sex? (coded as yes =1, no = 0).
- 4.
A person cannot get HIV by sharing food with someone who has HIV? (coded as yes =1, no = 0).
- 5.
Can a healthy-looking person have HIV? (coded as yes =1, no = 0).
These questions were recoded as binary variables. Then they were added together to generate an aggregate variable for correct HIV knowledge. The five statements of HIV knowledge had a low reliability test (Cronbach’s alpha of 0.43). Correct knowledge about HIV transmission was categorized as agreement to at least four to five statements. Those who had agreement to none to three statements were recoded as not having correct knowledge on HIV transmission.
HIV stigma was measured by eight binary (coded as yes = 1 and no = 0) statements (Cronbach’s alpha was 0.60):
- 1.
Would not buy fresh vegetables from an HIV positive vendor
- 2.
Children living with HIV should not be allowed to attend school with children who do not have HIV
- 3.
People hesitate to take an HIV test because they are afraid of how other people will react if the test result is positive
- 4.
People talk badly about people living with HIV, or who are thought to be living with HIV
- 5.
People living with HIV, or thought to be living with HIV, lose the respect of other people
- 6.
Fear that one could get HIV if in contact with the saliva of a person living with HIV
- 7.
Would be ashamed if someone in family had HIV
- 8.
Not willing to care for someone living with HIV
These HIV stigma statements were recoded into binary form and added together to form a score (range from 0 to 8). A binary variable called stigma on at least four statements was created (0 = agreement on 0–3 statements; 1 = agreement to 4–8 statements).
HIV related behaviour included sexual activity in the last 12 months (yes or no), number of life time sexual partners, transactional sex (life time and recent), alcohol consumption, male circumcision and self-reported STIs. Transactional sex involved giving and receiving of gifts for sex in the last 12 months. Substance use variables included alcohol consumption, smoking and use of tobacco. Males were asked to report about their circumcision status (yes, no and not applicable for females).
Self-reported STIs were measured by asking four questions:
- 1.
During the last 12 months, have you had an abnormal discharge from your vagina or experienced pelvic pain (if woman) or penis (if man)?
- 2.
During the last 12 months, have you had an ulcer or sore on or near your vagina (woman) or penis (man)?
- 3.
During the last 12 months, have you had pain on urination?
- 4.
In the last 12 months, did a doctor, clinical officer or nurse tell you that you had a sexually transmitted disease other than HIV?
These questions had three categories (yes, no and don’t know). The Cronbach’s alpha for the four statements was 0.71. The “don’t know” category was merged with the “No” category in order to create binary variables to allow creation of an aggregate variable. In addition, the responses to the former were few. After, an aggregate variable – self-reported STIs was created for those who reported an abnormal discharge, ulcer or sore in the genital area, pain during urination and were told to have an STI by a health provider.
Statistical analysis
Frequency distributions were used to describe the background characteristics of the older persons. Cross-tabulations were used to investigate associations between recent HIV testing (outcome variable) and selected explanatory variables. Pearson’s chi-squared (χ2) tests were used to examine the significant differences between recent HIV testing and the explanatory variables. The level of statistical significance using p-values was set at p < 0.05.
Multivariable logistic regression analyses were used to examine the association between recent HIV testing and explanatory variables whose p-values were less than 0.05 during the chi-square tests. We used a step-wise regression for multivariable analysis. The first model includes respondents’ background characteristics. In the second model, we added HIV knowledge and attitude factors, and in the third and final model we added behavior factors. Results are presented in the form of Odds Ratios (OR) reporting 95% confidence intervals. The level of statistical significance using p-values was set at p < 0.05. All analyses were performed in STATA version 15.
Results
Descriptive characteristics
Table 1 shows the descriptive characteristics of older persons in rural Uganda. About 52% of the respondents were female and 52% were 60 years and older. The majority (75%) had primary or no formal education, were working (53%), either Catholic or Anglican (75%), and were either married or cohabiting (60%).
With respect to HIV knowledge and attitude factors, the majority (65%) had correct knowledge on 4–5 HIV transmission statements, had less or no HIV associated stigma (67%), agreed to the need to test for HIV once a year (95%), and the need for male circumcision to prevent HIV (69%). About half (51%) had sex in the past 12 months. Majority (72%) had had one lifetime sexual partner. On the other hand, a small proportion of older people had received or given money or gifts for sex (24%) in their lifetime and in the last 12 months preceding the study (13%), drunk alcohol (34%) and used tobacco or drugs (13%). Some of the respondents reported suffering from STIs in the past 12 months (29%) and were circumcised (17%). Slightly over half (53%) and over three quarters (82%) tested for HIV in the last 12 months and in their lifetime, respectively.
Association between HIV testing in the past 12 months and independent factors
Table 2 shows the association between recent HIV testing and reception of results and background factors among older persons in Uganda.
HIV testing prevalence declined with increase in age (64% for 50–59 compared to 19% of 80+ year olds; p < 0.001). Higher proportion of HIV testing were observed among respondents that worked in the past year (59%; p < 0.001), currently in union (57%; p < 0.01), polygamous unions (66%; p < 0.01), had correct knowledge of HIV transmission on 4–5 aspects (56%; p = 0.01), felt the need to test for HIV annually (54%; p = 0.01), felt need for male circumcision (56%; p = 0.01), were actually circumcised (67%; p < 0.01), had sex in the last 12 months (67%; p < 0.001), had transactional sex (67%; p = 0.01) in the last 12 months, and self-reported STIs in the past year (62%; p < 0.01). Education, religion, stigma, number of lifetime sexual partners, alcohol and drug use were not significantly associated with HIV testing 12 months preceding the study.
Multivariable results
Table 3 shows the association between recent HIV testing and background factors among older persons in rural Uganda.
Age was consistently associated with HIV testing in the past 12 months. Older persons age 70 and older consistently had reduced odds of testing for HIV compared to 50–59 year olds after adjusting for background factors (aOR = 0.33; 95% CI: 0.22–0.50), adding knowledge factors and attitudes (aOR = 0.37; 95% CI: 0.24–0.56) and finally adding behavioural factors (aOR = 0.49; 95% CI: 0.31–0.79).
In addition, being circumcised, sexual activity, transactional sex, and self-reported STIs in the past year, being circumcised were significantly associated with recent HIV testing. The odds of HIV testing increased (aOR = 1.59; 95% CI: 1.0–2.3) among respondents who had a self-reported STI compared to those that did not. Older men who were circumcised compared to those (older men) who were not were more likely (aOR = 1.71; 95% CI: 1.0–2.9) to test for HIV in the last 12 months. Also, those who had sex in past year compared to those that did not, had increased odds (aOR = 2.89; 95% CI: 1.8–4.6) of HIV testing.
Working in the past year was significantly associated (aOR = 1.39; 95% CI: 1.0–1.9) with HIV testing after adjusting for background characteristics but subsequently lost its influence after adjusting for the rest of the explanatory factors (Models 2 and 3). Likewise, the odds of HIV testing among 60–69 year olds reduced in the first and second models compared to 50–59 year olds but were not significant in the third model. The association between sex, number of spouses, knowledge of HIV transmission modes, stigma, acknowledging the need for circumcision among older person and engaging in transactional sex 12 months prior to the study were not significantly associated with HIV testing 12 months prior to the study.
Discussion
We set out to establish the prevalence and examine the determinants of HIV testing in the last 12 months among older persons in rural Uganda. Over half of (53%) older persons had tested HIV during the 12 months preceding the study. This finding is in consistent with the proportion (48%) of older persons (age 45–59 years) that had tested for HIV [37] in the 2011 Uganda AIDS indicator survey [26].
The determinants of HIV testing among old persons in the year preceding the study in order of strength of influence were: sexual activity in the past year, male circumcision, having a self-reported STIs and advanced age. Sexual activity in the last 12 months increased the odds of recent HIV testing. Among older persons, recent sexual activity increases perceived risk of HIV infection which motivates older persons to have an HIV test [38, 45]. This is because sexual activity is one of the main avenues of HIV transmission [57]. Older men tend to remain sexually active and engage in extra-marital affairs more than older women [35].
Our study found that self-reported STIs were positively associated with HIV testing. Self-reported STIS are indicative of engagement in risky sexual behaviours that increase the odds of HIV infection. HIV testing in such cases is through risk perception or referral by health providers [45].
The study found that circumcised older persons had increased odds of HIV testing [58]. The possible explanation is that in case of medical circumcision, it is possible that older persons who interacted with the health sector also benefited from HIV relevant health education [59]. In addition, they might choose not to use condoms and instead prefer to test for HIV.
This study found that advanced age reduced odds of testing for HIV. This finding is in agreement with studies elsewhere [44]. This could be associated with low perceived HIV risk, and lack of associated information [38, 45].
This study merits the following strengths: first, it highlights important findings about HIV testing among older persons in Uganda using quantitative survey data with a good sample size. The findings provide a benchmark for conducting further studies in Uganda.
None the less, there are some limitations of the data. First, it is cross-sectional data and we cannot easily ascertain the direction of causality of associations between HIV testing and self-reported STIs and sexual activity in the last 12 months. Finally, HIV knowledge reliability score of 0.43 showed that the statements are not very reliable.
Conclusion
Recent HIV testing among older persons is associated with younger age (50–59 years), self-reported STIs, male circumcision, and sexual activity among older persons in rural Uganda. HIV testing interventions need to target older persons age 70 years and older, who were less likely to test. These interventions include behavioral risk assessment and routine screening for HIV infection.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available due for confidentiality reasons but are available from the corresponding author on reasonable request.
References
UNECA: The state of older persons in Africa - 2007. In: Regional review and appraisal of the Madrid International Plan of Action on Ageing. United Nations Economic Commision for Africa; 2007.
MoGLSD: National Policy for Older Persons: Ageing with Security and Dignity In. Kampala, Uganda: Ministry of Gender, Labour and Social Development; 2009.
UBOS: Uganda National Household Survey 2009–2010. Socio-economic module. Abridged report. In. Kampala, Uganda: Uganda Bureau of Statistics; 2010.
Definition of an older or elderly person: Proposed Working Definition of an Older Person in Africa for the MDS Project [http://www.who.int/healthinfo/survey/ageingdefnolder/en/].
Kyobutungi C, Ezeh A, Zulu E, Falkingham J. HIV/AIDS and the health of older people in the slums of Nairobi, Kenya: results from a cross sectional survey. BMC Public Health. 2009;9(1):153.
Ezeh A, Chepngeno-Langat G, Abdhalah Z, Woubalem Z: The situation of older people in poor urban settings: the case of Nairobi, Kenya In: Aging in Sub-Saharan Africa: Recommendations for Furthering Research edn. Edited by Cohen B, Menken J. Washington, US: The National Academies Press; 2006: 7–45.
MRC, UVRI: Direct and indirect effects of HIV/AIDS and anti-retroviral treatment on the health and wellbeing of older people. In: WHO’s Study on global AGEing and adult health (SAGE). Kampala: Uganda Virus Research Institute & Medical Research Council; 2011.
Gómez-Olivé FX, Thorogood M, Clark B, Kahn K, Tollman S. Self-reported health and health care use in an ageing population in the Agincourt sub-district of rural South Africa. Glob Health Action. 2013;6:19305.
HAI: Guidance on including older people in emergency shelter programmes: a summary. In.: HelpAge International, London, UK 2010.
Kyobutungi C, Egondi T, Ezeh A. The health and well-being of older people in Nairobi’s slums. Glob Health Action. 2010;3:45–53.
Kowal P, Kahn K, Ng N, Naidoo N, Adbullah S, Bawah A, Binka F, Chuc NTK, Debpuur C, Ezeh A et al: Ageing and adult health status in eight lower-income countries: the INDEPTH WHO-SAGE collaboration. Global Health Action 2010, Supplement 2.
Hirve S, Juvekar S, Lele P, Agarwal D. Social gradients in self-reported health and well-being among adults aged 50 and over in Pune District, India. Glob Health Action. 2010;2:88–95.
Gómez-Olivé FX, Thorogood M, Clark B, Kahn K, Tollman S. Assessing health and well-being among older people in rural South Africa. Glob Health Action. 2010;2:23–35.
Debpuur CY, Welaga P, Wak G, Hodgson A: Self-reported health and functional limitations among older people in the Kassena-Nankana District, Ghana; 2010.
UN: World Population Prospects: The 2017 Revision, Key Findings and Advance Tables In.: United Nations Department of Economic and Social Affairs/Population Division; 2017.
World Population Prospects: The 2017 Revision, Online Demographic Profiles [https://population.un.org/wpp/Graphs/DemographicProfiles/].
UNFPA HAI. Ageing in the twenty-first century: a celebration and a challenge. New York, and HelpAge International, London: United Nations Population Fund (UNFPA); 2012.
World Population Prospects: The 2010 Revision [http://esa.un.org/unpd/wpp/unpp/p2k0data.asp].
PRB: 2017 World Population Data Sheet In. Washington, D.C: Population Reference Bureau 2017.
UN: Population Ageing and Development: Department of Economic and Social Affairs, Population Division, United Nations. 2009.
AIDS by Numbers.
Linley L, Prejean J, An Q, Chen M, Hall HI. Racial/ethnic disparities in HIV diagnoses among persons aged 50 years and older in 37 US states, 2005-2008. Am J Public Health. 2012;102(8):1527–34.
Chamie G, Clark TD, Kabami J, Kadede K, Ssemmondo E, Steinfeld R, Lavoy G, Kwarisiima D, Sang N, Jain V, et al. A hybrid mobile approach for population-wide HIV testing in rural East Africa: an observational study. The lancet HIV. 2016;3(3):e111–9.
90–90–90 - An ambitious treatment target to help end the AIDS epidemic [https://www.unaids.org/en/resources/documents/2017/90-90-90].
90–90-90: An ambitious treatment target to help end the AIDS epidemic [http://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf].
Nabukenya AM, Matovu JKB. Correlates of HIV status awareness among older adults in Uganda: results from a nationally representative survey. BMC Public Health. 2018;18(1):1128.
Hontelez JAC, de Vlas SJ, Baltussen R, Newell M-L, Bakker R, Tanser F, Lurie M, Bärnighausen T: The impact of antiretroviral treatment on the age composition of the HIV epidemic in sub-Saharan Africa. AIDS (London, England) 2012, 26(0 1).
Mahy M, Autenrieth CS, Stanecki K, Wynd S: Increasing trends in HIV prevalence among people aged 50 years and older: evidence from estimates and survey data. AIDS (London, England) 2014, 28(4):S453.
Justice A, Falutz J. Aging and HIV: an evolving understanding. Curr Opin HIV AIDS. 2014;9(4):291–3.
Brooks JT, Buchacz K, Gebo KA, Mermin J. HIV infection and older Americans: the public health perspective. Am J Public Health. 2012;102(8):1516–26.
Freeman E, Anglewicz P. HIV prevalence and sexual behaviour at older ages in rural Malawi. Int J STD AIDS. 2012;23(7):490–6.
Kharsany ABM, Karim QA. HIV infection and AIDS in sub-Saharan Africa: current status, challenges and opportunities. Open AIDS J. 2016;10:34–48.
PHIA. Population-based HIV impact assessment (PHIA) survey. In. New York, USA: ICAP at Columbia University; 2018.
Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Zungu N, Labadarios D, Onoya D. South African national HIV prevalence, incidence and behaviour survey, 2012; 2014.
Schatz E, Knight L. "I was referred from the other side": gender and HIV testing among older south Africans living with HIV. PLoS One. 2018;13(4):e0196158.
Negin J, Gregson S, Eaton JW, Schur N, Takaruza A, Mason P, Nyamukapa C. Rising levels of HIV infection in older adults in eastern Zimbabwe. PLoS One. 2016;11(11):e0162967.
Mohlabane N, Tutshana B, Peltzer K, Mwisongo A. Barriers and facilitators associated with HIV testing uptake in south African health facilities offering HIV Counselling and testing. Health SA Gesondheid. 2016;21(1):86–95.
Negin J, Cumming RG. HIV infection in older adults in sub-Saharan Africa: extrapolating prevalence from existing data. Bull World Health Organ. 2010;88:847–53.
Ford CL, Godette DC, Mulatu MS, Gaines TL. Recent HIV testing prevalence, determinants, and disparities among U.S. older adult respondents to the behavioral risk factor surveillance system. Sex Transm Dis. 2015;42(8):405–10.
Aday LA, Andersen RM. A framework for the study of access to medical care. Health Serv Res. 1974:208–20.
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behaviour. 1995;36(March):1–10.
Andersen RM. National Health Surveys and the behavioral model of health services use. Med Care. 2008;46:647–53.
Negin J, Nemser B, Cumming R, Lelerai E, Amor YB, Pronyk P. HIV attitudes, awareness and testing among older adults in Africa. AIDS Behav. 2012;16(1):63–8.
Akers A, Bernstein L, Henderson S, Doyle J, Corbie-Smith G. Factors associated with lack of interest in HIV testing in older at-risk women. J Women's Health. 2007;16(6):842–58.
Oraka E, Mason S, Xia M. Too old to test? Prevalence and correlates of HIV testing among sexually active older adults. J Gerontol Soc Work. 2018;61(4):460–70.
Gwadz M, Leonard NR, Honig S, Freeman R, Kutnick A, Ritchie AS. Doing battle with "the monster:" how high-risk heterosexuals experience and successfully manage HIV stigma as a barrier to HIV testing. Int J Equity Health. 2018;17(1):46.
Madise NJ, Ziraba AK, Inungu J, Khamadi SA, Ezeh A, Zulu EM, Kebaso J, Okoth V, Mwau M. Are slum dwellers at heightened risk of HIV infection than other urban residents? Evidence from population-based HIV prevalence surveys in Kenya. Health & place. 2012;18(5):1144–52.
Gage AJ, Ali D. Factors associated with self-reported HIV testing among men in Uganda. AIDS Care. 2005;17(2):153–65.
UBOS, ICF: Uganda demographic and health survey 2016: key indicators report. In. Kampala, Uganda and Rockville, Maryland, USA; 2017.
Scholten F, Mugisha J, Seeley J, Kinyanda E, Nakubukwa S, Kowal P, Naidoo N, Boerma T, Chatterji S, Grosskurth H. Health and functional status among older people with HIV/AIDS in Uganda. BMC Public Health. 2011;11:886.
UBOS. Uganda population and housing census 2014. In. Uganda Bureau of Statistics: Kampala, Uganda; 2016.
Masaka district [http://www.lcmt.org/uganda/masaka].
Hoima district [http://www.lcmt.org/uganda/masaka].
Anderson TW, Kish L: Survey Sampling. In.; 1966.
UBOS, ICF international: Uganda demographic health survey 2016. In. Kampala, Uganda Uganda Bureau of Statistics (UBOS); 2017.
SurveyCto: SurveyCTO: How it works. In.; 2018.
Baeten JM, Donnell D, Kapiga SH, Ronald A, John-Stewart G, Inambao M, Manongi R, Vwalika B, Celum C: Male circumcision and risk of male-to-female HIV-1 transmission: a multinational prospective study in African HIV-1 serodiscordant couples. AIDS (London, England) 2010, 24(5):737.
Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, Nalugoda F, Kiwanuka N, Moulton LH, Chaudhary MA, Chen MZ. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369(9562):657–66.
Kironde B, Wamala R, Kwagala B. Determinants of male circumcision for HIV/AIDS prevention in east Central Uganda. Afr J Reprod Health. 2016;20(1):80–7.
Acknowledgements
We acknowledge the statistical support from Ronald Naitala (RN) of Baylor Uganda: Baylor College of Medicine Children’s Foundation.
Funding
This research was funded by the Consortium for Advanced Research Training in Africa (CARTA) as a Re-Entry grant (RCS/CARTAREENTRY/2016/002). CARTA is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Carnegie Corporation of New York (Grant No: B 8606.R02), Sida (Grant No: 54100029), the DELTAS Africa Initiative (Grant No: 107768/Z/15/Z). The DELTAS Africa Initiative is an Independent funding scheme of the African Academy of Sciences (AAS)‘s Alliance for Accelerating Excellence in Science in Africa (AESA) and supported by the New.
Partnership for Africa’s Development Planning and Coordinating Agency (NEPAD Agency) with funding from the Wellcome Trust (UK) (Grant No: 107768/Z/15/Z) and the UK government.
Some seed fund was granted by the Makerere University, College of Business and Management Sciences (CoBAMS) to support manuscript writing process. The funding body (CARTA or Makerere University) had no role in the design of the study; collection, analysis, and interpretation of data; and in the writing the manuscript.
Author information
Authors and Affiliations
Contributions
SOW conceptualized and developed the study. BK, and FM reviewed the study protocol. BK & FM wrote the background section. BK, PN and SOW reviewed the literature. SOW analysed the data. BK, SOW and SOW interpreted the results and participated in the drafting of the manuscript. All read and reviewed the manuscript. All authors read and approved the manuscript.
Authors’ information
SOW is a Lecturer at the Department of Population Studies (DPS), School of Statistics and Planning (SSP), Makerere University. He has a PhD in Population Studies (specialized on Population Ageing). His PhD thesis was titled: “Disparities in Health & of Access to Healthcare among Older persons in Uganda”. In addition, he has researched on Sexual and Gender-Based Violence. He holds a Master of Science in Population and Reproductive Health and a Bachelor of Science in Population Studies.
BK is a Senior Lecturer at the Department of Population Studies, School of Statistics and Planning, College of Business and Management (CoBAMS), Makerere University. BK holds a PhD in Sociology (University of Vienna), Masters in Development Studies (Women and Development), from the Institute of Social Studies (ISS) at The Hague. Her research interests focus on gender and reproductive health.
FM is an Assistant Lecturer at the DPS, Makerere University. He holds a Master of Science in Population Studies, Makerere University. He is a PhD student at the Makerere University. He has submitted his thesis for examination. His thesis focused on the “Determinants of Quality of life of older persons in rural Uganda”.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by The AIDS Support Organization (TASO REC), a local Research and Ethics Committee (REC) on July 4th 2017. The approval reference number is TASOREC/30/17-UG-REC-009. Finally, the protocol was registered with the Uganda National Council of Science and Technology (UNCST), with a registration number, SS 4424. Written voluntary informed consent was obtained from all study participants. Participants were assured of confidentiality. In order to ensure anonymity, participants’ names were not be recorded alongside their responses.
Consent for publication
Not applicable.
Competing interests
The author(s) declare that they have no competing interests. Stephen Ojiambo Wandera is part of the Editorial board of BMC Public Health, but otherwise, had no role in the editorial process of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wandera, S.O., Kwagala, B. & Maniragaba, F. Prevalence and determinants of recent HIV testing among older persons in rural Uganda: a cross-sectional study. BMC Public Health 20, 144 (2020). https://doi.org/10.1186/s12889-020-8193-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-020-8193-z