Abstract
Background
Hypertension is a leading cause of cardiovascular diseases and a growing public health problem in many developed and developing countries. However, population-based data to inform policy development are scarce in Rwanda. This nationally representative study aimed to determine population-based estimates of the prevalence and risk factors associated with hypertension in Rwanda.
Methods
We conducted secondary epidemiological analysis of data collected from a cross-sectional population-based study to assess the risk factors for NCDs using the WHO STEPwise approach to Surveillance of non-communicable diseases (STEPS). Adjusted odds ratios at 95% confidence interval were used to establish association between hypertension, socio-demographic characteristics and health risk behaviors.
Results
Of the 7116 study participants, 62.8% were females and 38.2% were males. The mean age of study participants was 35.3 years (SD 12.5). The overall prevalence of hypertension was 15.3% (16.4% for males and 14.4% for females). Twenty two percent of hypertensive participants were previously diagnosed. A logistic regression model revealed that age (AOR: 8.02, 95% CI: 5.63–11.42, p < 0.001), living in semi-urban area (AOR: 1.30, 95% CI: 1.01–1.67, p = 0.040) alcohol consumption (AOR: 1.24, 95% CI: 1.05–1.44, p = 0.009) and, raised BMI (AOR: 3.93, 95% CI: 2.54–6.08, p < 0.001) were significantly associated with hypertension. The risk of having hypertension was 2 times higher among obese respondents (AOR: 3.93, 95% CI: 2.54–6.08, p-value < 0.001) compared to those with normal BMI (AOR: 1.74, 95% CI: 1.30–2.32, p-value < 0.001). Females (AOR: 0.75, 95% CI: 0.63–0.88, p < 0.001) and students (AOR: 0.45, 95% CI: 0.25–0.80, p = 0.007) were less likely to be hypertensive.
Conclusion
The findings of this study indicate that the prevalence of hypertension is high in Rwanda, suggesting the need for prevention and control interventions aimed at decreasing the incidence taking into consideration the risk factors documented in this and other similar studies.
Similar content being viewed by others
Background
Hypertension is one of the five leading causes of mortality in the world and a major risk factor associated with more than 40% of deaths related to cardiovascular and renal diseases [1,2,3,4,5,6]. Because of its asymptomatic nature, many people with the disease remain undiagnosed and untreated thus resulting in increased premature and sudden deaths due to direct or indirect complications [7]. According to 2010 WHO estimates, 22% of adults aged 18 years and above were hypertensive, and 9.4 million deaths were estimated to have been caused by hypertension, which is about 7% of the global burden of disease [8]. Across the WHO regions, Africa has the highest prevalence of high blood pressure with 30% of the people affected, while the lowest was recorded in the American Region [8, 9]. According to a systematic analysis conducted in 2014, prevalence of hypertension increased from 19.7% in 1990 to 30.8% in 2010 in Africa [10]. The changing epidemiology of hypertension is associated with the global economic development resulting in aging population in some societies, and changing lifestyle resulting in increased prevalence of obesity, alcohol and tobacco consumption and physical inactivity [11,12,13]. Worse still, the level of awareness, treatment and control of hypertension remain low in Africa, thus most of the affected persons are unaware of their status [10].
Like many other developing countries, Rwanda is in a phase of epidemiological transition. While communicable diseases remain the major causes of morbidity and mortality in the country, the increasing incidence of non-communicable diseases such as hypertension results in a double burden of diseases [14]. This pattern is associated with improvements in the socioeconomic status of the country in the last 20 years resulting in changes in lifestyle [15]. A study conducted in Bugesera district in 2007 estimated the prevalence of high blood pressure at 16.8% [16]; this study identified age, overweight, dietary intake and physical inactivity as risk factors associated with development of hypertension. [16]. A cross-sectional survey conducted at an urban tertiary education institution in Rwanda found that 36% of employees were hypertensive and demonstrated a low level of awareness among hypertensive participants [17]. Low awareness was also documented in a study conducted among hypertensive patients enrolled in the outpatient department of Kigali University Teaching Hospital [18]. The review of medical records showed that hypertension accounted for 2.5% of total admissions in Ruhengeri district hospital out of which 47.4% presented with severe hypertension. The review highlighted that alcohol consumption, diabetes mellitus, congestive heart failure were significantly associated with hypertension [19]. WHO estimated the number of deaths attributable to hypertension in Rwanda at 18/100,000 [20]. Available health facility-based data showed that the proportion of people consulting for high blood pressure increased from 1.9% in 2009 to 6.4% in 2014 in Rwanda [14].
The discrepancy in the prevalence of hypertension between the community and hospital-based data is wide [14, 16]. This can be attributed to the asymptomatic nature of the disease with many people not being aware of their status, not self-reporting and hence not captured in the health facility-based data. Given that the community data is a more reliable reflection of the true burden of any disease, we identified the need to analyze the nation-wide survey data collected from a representative sample to better estimate the prevalence of hypertension in Rwanda.
This study is a nationally representative study and provides population-based estimates of the prevalence and risk factors associated with hypertension in Rwanda. The findings will serve as baseline for monitoring the changing pattern of hypertension and its risk factors, and inform development of appropriate policies, strategies, planning and targeting of preventive public health interventions.
Methods
Study design and survey participants
We conducted a secondary analysis of primary data collected from a national population-based cross-sectional study to assess the risk factors for NCDs; the primary study was conducted using the WHO STEPwise approach to Surveillance of non-communicable diseases (STEPS) and took place in Rwanda from November 2012 to April 2013. The survey assessed the prevalence of risk factors for Non-Communicable Diseases (NCDs) in the country [21]. Study participants included people aged between 15 and 64 years residing in Rwanda, who participated in the STEPwise national survey.
Description of STEPS survey
STEPS sample size and method
The sample size was calculated using the formula N = Z2 P (1-P)/e2 and assumptions described by WHO STEPwise approach to non-communicable disease risk factor surveillance [22], where N = sample size, Z = level of confidence, P = baseline level of the selected indicator and e = margin of error. P was estimated at 0.50 (recommended by the STEPS survey guidelines when the estimated baseline is unknown), Z = 1.96 (at 95% Confidence Interval), e = 0.05, thus the estimated sample size was N = 1.962 × 0.5(1–0.5)/0.052 = 384. This basic sample size was adjusted for design effect for complex sample design (1.50), age-sex estimates, 15–64 age range (10 year intervals) and the required sample size was therefore N = 384* 1.5* 10 = 5760. Assuming a non-response rate of 20%, the final sample size was therefore adjusted upward to: 5760/0.8 = 7200.
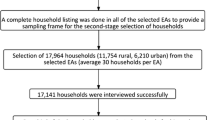
A multi-stage cluster sampling method was used to select participants from the population based on information from the 2012 census. The three clusters were enumeration areas (EAs) (defined as villages in the Rwandan context), households and eligible participant within the household (Additional file 1). In the first stage, the list of all the villages in Rwanda was obtained from the National Institute of Statistics of Rwanda (NISR) and used as a sampling frame for random selection of EAs. Probability Proportional to Size (PPS) sampling method was applied to randomly select 279 EAs, thus the selection was done based on the size of EAs. [23]. In the second stage, the number of households to be sampled in each EA was determined by dividing the total sample size by the total number of EAs selected, thus the number of households in each EA came to 26. These households were then selected from each of the identified EAs, using the systematic random sampling method. The sampling interval for household selection in each village was determined by dividing the total households in a village by 26. In the third stage, one eligible participant (aged 15–64 years) was randomly selected from each household and enrolled into the survey. Eligible participants’ and household identification, name, sex and age were recorded on the electronic Kish sampling system built in personal digital assistant (PDA) and a random selection of the survey respondents in the household was made through the PDA and Kish selection methodFootnote 1 was used in case more than one household members were eligible for the interview [24,25,26].
Data collection tools and approach
The WHO STEPS for NCD risk factors surveillance consist of three sequential steps namely 1) gathering information on sociodemographic characteristics and key risk factors using a uniform set of questionnaires; 2) physical measurements of blood pressure, height, weight and waist circumference; and 3) biochemical measurements of parameters such as fasting blood glucose, blood lipids etc. The WHO generic STEPS instrument was adapted to the Rwanda context and used to collect data for the STEPS survey. The questionnaire had 133 questions grouped into six sections, and included ten questions on hypertension. Survey teams, each comprising of one supervisor whose role was planning and checking the completeness of the questionnaire, three experienced nurses who conducted the interviews and, one laboratory technician who collected capillary and venous blood samples for quality control at the National Reference Laboratory collected the data for the study. One community health worker (CHW) was assigned to each survey team to assist with notification of the heads of the selected villages about the day and time when the survey team will visit their villages and guide the survey team to the selected villages and households. Prior to data collection, the teams were trained on the objectives, methods of the survey, and the tools for data collection were pre-tested. Data were collected using PDAs. Before leaving the participant’s residence, the data collection team reviewed responses for completeness and any missing information was appropriately updated. The information from the PDAs was backed up and uploaded onto a computer using e-STEPS which is a suite of software that support implementation of data collection using PDA, and epi-data software on weekly basis. Data quality was assessed on a weekly basis and feedback was sent to the survey supervisors in the field to correct any discrepancies. The data were edited and coded as per the WHO STEPS manual and entered into the WHO recommended EpiData software version 3.1,
Socio-demographic information collected included age, sex, residence (rural, semi-urban and urban as defined by NISR), level of completed education, marital status, and occupation. Variables assessed included height, weight, tobacco use, alcohol intake, physical activity, high blood pressure, and biochemical measurements such as blood glucose, total cholesterol and HDL cholesterol.
Definition and measurement of variables
High blood pressure
High blood pressure was defined as a systolic blood pressure of more than or equal to 140 mmHg and/or diastolic blood pressure more than or equal to 90 mmHg [27] or currently taking antihypertensive medications An automated blood pressure machine (OMRON® digital device) was used to obtain the blood pressure readings [22, 28]. Three readings were taken 3–5 min apart after 15 min rest of the survey participant. As recommended by WHO, the average of the last two readings were calculated and used as the final blood pressure measurement.
Body mass index (BMI)
BMI was expressed as weight in kilogram/height in square meters (kg/m2). Weight and height were measured using Genesis weighing scales with a laser for measuring height. The survey participants were measured without shoes and wearing only light cloths. Respectively, height and weight were measured to the nearest whole centimeter and 0.1 kg. BMI was classified as <18.5 kg/m2 (lean), 18.5–24.9 kg/m2 (normal), 25.0–29.9 kg/m2 (overweight), and 30+ kg/m2 (obese) [29].
Biochemical measurements
The finger prick method was used to collect capillary blood sample after 8 h of fasting. For every tenth finger-prick test performed, a venous sample was taken for quality control at the National Reference Laboratory. Total cholesterol, high-density lipoprotein (HDL) and fasting blood glucose were measured using CardioChek PA (Glucose, Cholesterol, and HDL) [30].
Blood glucose was categorized as normal (<5.6 mmol/l), impaired fasting glycaemia (≥ 5.6 mmol/L and <6.1 mmol/l), and raised fasting blood glucose (≥ 6.1 mmol/l, or currently on medication) [31]. For total cholesterol, normal range was defined as <5.0 mmol/l. The level of HDL cholesterol was classified as normal (≥1.03 mmol/l for males, ≥ 1.29 mmol/l for females) and low (< 1 mmol/l or 40 mg/dl in males, and <1.3 mmol/l or 50 mg/dl in females) [22].
Data analysis
We extracted and performed secondary data analysis on all participants in the STEPS aged 15–64 years. The level of education, marital status, occupation, alcohol consumption and physical activity and BMI were re-categorized from the original dataset to facilitate the analysis and results interpretation (Additional file 2).
The data were weighted by sample weights and analyzed using Stata version 13. Descriptive analyses comprising frequencies of high blood pressure according to sociodemographic characteristics and behavioral health risks among study population by sex and age; and analytical analyses were performed. The Pearson Chi-square test was used to test the independence between variables. The association between sociodemographic characteristics, behavioral health risks and hypertension were determined using bivariate and multivariable analyses methods. Furthermore, multivariate logistic regression was conducted for all variables of interest with p-value <0.05 in the univariate model. These variables are socio-demographic including age, sex, residence, marital status, education, occupation; behavioral variables such as tobacco use, alcohol consumption, physical activities, and metabolic risk factors such as BMI, blood glucose, total cholesterol and HDL cholesterol which are risk factors recommended for assessment in the STEPS survey manual [22]. Adjusted odds ratios (AOR), 95% confidence intervals (CI), and p-values were generated to determine independent predictors for hypertension.
Results
Over seven thousand (7116) participants aged 15–64 years were extracted from the STEPS database and enrolled into the study. Four thousand (4466) study participants (62.8%) were females. The mean age of respondents was 35.3 years (SD 12.5), and a third of the respondents were between 25 to 34 years old. Respondent residing in rural area, less educated, self-employed, and married were more represented in the study. The overall prevalence of hypertension in Rwanda was 15.4% (95% CI: 14.6%–16.3%); this was 16.5% (95% CI: 15.1%–18.0%) among males and 14.4% (95% CI: 13.4%–15.5%) among females. The prevalence of hypertension was more than double in those aged 55–64 years as compared to those 44 years and below (38.6%). The Western and Northern Provinces were more affected while prevalence of hypertension was higher in the semi-urban areas (18.6%). Prevalence of hypertension was higher among the separated, divorced and widowed, the less educated, and employed. The lowest rate of hypertension was observed among students (Table 1).
Among respondents who were hypertensive, 23.0% self-reported that they had been previously diagnosed by a registered physician and 70.7% reported to have never been told by a physician or a health professional that they had high blood pressure. Seventy nine percent of people who had hypertension in the rural areas were undiagnosed as compared to 71.2% in semi-urban/urban areas (Table 1).
Hypertension and associated risk factors
The prevalence of hypertension was 2 times higher among respondents with BMI more than or equal to 30 kg/m2 as compared to those with normal BMI. The descriptive analysis showed that hypertension prevalence was higher among respondents who had a history of smoking, alcohol consumption, and those with low physical activity. The prevalence was also higher among respondents who had high fasting blood glucose or were on medication for diabetes, and those with raised total cholesterol (Table 2).
The multivariate logistic regression showed that increase in age was associated with a linear increase in the risk of having hypertension, being four times more prevalent among respondents aged 55–64 (AOR: 8.02, 95% CI: 5.63–11.42, p-value < 0.001) compared to those aged 25–34 years old (AOR: 1.69, 95%CI: 1.25–2.80, p-value < 0.001). The risk of having hypertension was respectively 1.30 (95% CI: 1.01–1.67, p-value = 0.028,) and 1.24 (95% CI: 1.05–1.44, p-value = 0.009) times higher among respondents who reside in semi-urban area and those who consumed alcohol. Females (AOR: 0.75, 95% CI: 0.63–0.88, p-value < 0.001,) and students (AOR: 0.45, 95% CI: 0.25–0.80, p-value = 0.007,) were less likely to be hypertensive. The risk of having hypertension was 2 times higher among obese respondents (AOR: 3.93, 95% CI: 2.54–6.08, p-value < 0.001,) compared to those with normal BMI (AOR: 1.74, 95% CI: 1.30–2.32, p-value < 0.001) (Table 3).
Discussion
This study provided national population-based and age-adjusted estimates of hypertension in Rwanda, which showed an overall prevalence of 15.3%, among the population aged 15 to 64 years with males being more affected than females. This prevalence was about 6 times higher than what was reported through hospital-based data [14], but similar to the findings of a previous study in Bugesera district [16]. High prevalence was observed among the less educated and respondents who were not in union with their spouses (separated, divorced and widowed). More than three quarter of the hypertensive persons had never been informed about their high blood pressure, hence a lower level of awareness. Increasing age, living in semi-urban area, alcohol consumption and raised BMI were significantly associated with hypertension which compared favorably to the findings of other studies in and outside the region [32,33,34,35,36,37,38,39,40,41].
The prevalence of hypertension observed in this study is lower than what has been documented by similar studies conducted in Sub-Saharan African countries nevertheless we consider this prevalence as high. The low level of awareness of study participants observed in these findings might perhaps be due to inadequate public health interventions for prevention and control of hypertension. Health programs have for long time focused on communicable diseases rather than non-communicable conditions. Moreover, the enhanced surveillance of NCDs including hypertension was not yet fully integrated in the existing health system in Rwanda. Similar findings have also been reported across and outside the continent [10, 42,43,44,45]. However, contrasting findings of high level of awareness and control of hypertension was also observed in developed countries [46, 47].
The high prevalence of hypertension among less educated was documented by other studies [48,49,50,51] and could be attributed to the lack of appropriate health information and poor health education programs which normally improve the knowledge of the population and enhance the level of awareness of chronic conditions [52, 53]. Furthermore, uneducated people are less likely to understand risk factors related to diseases induced by lifestyle and thus unable to change their behavior and adopt positive practices [54, 55]. Although the high prevalence of hypertension was evident among less educated in our study, contrasting findings have been reported [56,57,58].
The increased prevalence of hypertension among separated, divorced and widowed could be due to stress induced by the absence of psychosocial and economic support from a spouse. On the other hand, separated, divorced and widowed are more likely to lose interest in life, therefore engage more in high-risk health behaviors such as smoking, alcohol consumption, lack of exercises and change in diet [59,60,61,62,63].
The socio-economic transition and urbanization observed in Rwanda which results in lifestyle, dietary changes and unhealthy behaviors may explain the high risk of hypertension in semi-urban area observed in this study. The impact of urbanization on lifestyle and health has been reported by other authors [64,65,66,67,68]; however our findings on association between hypertension and semi-urban residence were inconsistent with what was reported in a few low and middle income countries [69,70,71,72].
Study limitations
This study has three main limitations. First, the original study was a cross-sectional survey, thus the simultaneous collection of information on high blood pressure and its risk factors could have clouded the association between a risk factor and an outcome. Therefore, only an association and not causation can be inferred.
Second, the prevalence of hypertension may have been over or under-estimated because the three blood pressure measurements were performed on one occasion only. However, the large sample size, the use of standardized and tested methodologies, tools and high response rate observed in the study increased its representativeness and minimized this limitation.
Third, we were unable to explore the contribution of other risk factors such as unhealthy diet, salt intake, and psychosocial stress on the prevalence of hypertension because the related information were not collected during primary data collection.
Conclusions
The findings of this study show that the prevalence of hypertension is high in Rwanda. However, the level of awareness about the disease is low. The study identified age, overweight and obesity, alcohol consumption, residence in semi-urban area as the risk factors associated with hypertension. These findings and those of other similar studies should be used to synthesize appropriate evidence-based policies for the prevention and control of hypertension in the country. Prevention strategies including the integration of hypertension surveillance system into national disease surveillance system, conducting targeted screening of high-risk groups, and treatment (where indicated) of all persons attending health facilities are recommended. Measures aimed at reducing harmful use of alcohol especially among the high-risk group are also proposed. Furthermore, stakeholders should put in place strong health promotion and awareness creation aimed at addressing identified risk factors. Further studies on the association of hypertension and other factors such as psychosocial stress, salt and oil intake which were not examined in this study are essential to inform NCD program managers on the exhaustive risk factors of hypertension in the country and inform development of prevention and control strategies.
Change history
22 September 2017
An erratum to this article has been published.
Notes
The Kish sampling method was developed by Leslie Kish (1910–2000); itis built into the PDAs which were used to select eligible respondents in the households when more than one household members are eligible for the interview. Once a household is selected, the interviewer creates a list (sampling frame) of all the persons in the household that are eligible for the interview process. This list includes the name of the person, their gender, their relationship to the head of the household and their age. Once the listing is done, each eligible member is assigned a unique number. Then using a randomized response table a particular member is chosen for the interview.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- BMI:
-
Body Mass Index
- CDC:
-
Center for Disease Control
- CHWs:
-
Community Health Workers
- CI:
-
Confidence Interval
- HDL:
-
High Density Lipoproteins
- HIV/AIDS:
-
Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome
- HTN:
-
Hypertension
- LMIC:
-
Low Middle Income Countries
- MOH:
-
Ministry of Health
- NCDs:
-
Non Communicable Diseases
- NISR:
-
National Institute of Statistics of Rwanda
- PDA:
-
Personal Digital Assistant
- PPS:
-
Probability Proportional to Size
- RBC:
-
Rwanda Biomedical Center
- SD:
-
Standard Deviation
- WHO:
-
World Health Organization
References
Danaei G. Lu Y. Singh GM. Carnahan E. Stevens GA. Cowan MJ et al. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010. Lancet Diabetes and Endocrinol. 2014; 2(8):634–47. oi: 10.1016/S2213-8587(14)70102-0.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2013;380(9859):2224–60.
World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. 2009. http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf. Accessed 19 Dec 2016.
Fahimfar N, Khalili D, Mohebi R, Azizi F, Hadaegh F. Risk factors for ischemic stroke; results from 9 years of follow-up in a population based cohort of Iran. BMC Neurol. 2012;12(1):1. doi:10.1186/1471-2377-12-117.
Mukhopadhyay J, Biswas M, Bhowmik J. Hypertension and Atherosclerosis-The Cardiovascular Risk Continuum. Medicine Update. 2011:41–5. Available from http://www.apiindia.org/ Accessed 19 Dec 2016.
McAloon CJ, Boylan LM, Hamborg T, Stallard N, Osman F, Lim PB, et al. The changing face of cardiovascular disease 2000–2012: an analysis of the world health organisation global health estimates data. Int J Cardiol. 2016 Dec 1;224:256–64.
Ataklte F, Erqou S, Kaptoge S, Taye B, Echouffo-Tcheugui JB, Kengne AP. Burden of undiagnosed hypertension in sub-Saharan Africa: a systematic review and meta-analysis. Hypertens. 2015;65(2):291–8. doi:10.1161/HYPERTENSIONAHA.114.04394.
World Health Organization. Global status report on non-communicable diseases.2010. www.who.int/nmh/publications/ncd_report_full_en.pdf . Accessed 19 Dec 2016.
World Health Organization. STEPS country reports. 2015. http://www.who.int/chp/steps/reports/en/. Accessed 19 Dec 2016.
Adeloye D, Basquill C. Estimating the prevalence and awareness rates of hypertension in Africa: a systematic analysis. PLoS One. 2014;9(8):e104300. doi:10.1371/journal.pone.0104300.
Aballay LR, Eynard AR, del Pilar Díaz M, Navarro A, Muñoz SE. Overweight and obesity: a review of their relationship to metabolic syndrome, cardiovascular disease, and cancer in South America. Nutri Rev. 2013;71(3):168–79. doi:10.1111/j.1753-4887.2012.00533.x.
Bromfield S, Muntner P. High blood pressure: the leading global burden of disease risk factor and the need for worldwide prevention programs. Curr Hyperten Reps. 2013;15(3):134–6. doi:10.1007/s11906-013-0340-9.
Yusuf S, Reddy S, Ôunpuu S, Anand S. Global burden of cardiovascular diseases part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circ. 2001;104(22):2746–53.
Ministry of Health. Rwanda Health Statistics booklet 2009–2014. http/www.moh.gov.rw. Accessed 19 Dec 2016.
National Institute of Statistics of Rwanda Fourth Population and Housing Census, Rwanda, 2012. Available from http://www.statistics.gov.rw/. Accessed 19 Dec 2016.
de Ramirez SS, Enquobahrie DA, Nyadzi G, Mjungu D, Magombo F, Ramirez M, et al. Prevalence and correlates of hypertension: a cross-sectional study among rural populations in sub-Saharan Africa. J Hum Hypertens. 2010 Dec 1;24(12):786–95. doi:10.1038/jhh.2010.14.
Banyangiriki J, Phillips J. Prevalence of hypertension among working adults in Rwanda. Iranian J Publ Health, Vol. 42, No.8, Aug 2013, pp.925–926. Available at: http://ijph.tums.ac.ir
Kamali P, Page C, Kagame A. Quality of blood pressure control in hypertensive patients attending the Kigali University teaching hospital (CHUK). Annals of Global Health. 2016 May 1;82(3):427.
Pande R, NIYONZIMA JP. Prevalence and clinical features of arterial hypertension in Ruhengeri District hospital, Musanze. Rwanda Rwanda Medical Journal. 2013 May 30;69(2):9–13.
World Health Organization. World Health rankings Live Longer Live Better 2016. www.worldlifeexpectancy.com/world-health-rankings. Accessed 19 Dec 2016.
Rwanda Non-communicable Diseases Risk Factors Report, MOH 2015. http://www.who.int/chp/steps/Rwanda_2012_STEPS_Report.pdf. Accessed 19 Dec 2016.
World Health Organization. The WHO STEPwise approach to non-communicable disease risk factor surveillance. http://www.who.int/chp/steps/manual/en/. Accessed 19 Dec 2016.
Alam M, Sumy SA, Parh YA. Selection of the Samples with Probability Proportional to Size. Science Journal of Applied Mathematics and Statistics. Vol. 3, No. 5, 2015, pp. 230–233.doi: 10.11648/j.sjams.20150305.13
Nemeth R. Respondent selection within the household-A modification of the Kish grid. In Meeting of Young Statisticians 2002 (p. 51).
Rizzo L, Brick JM, Park I. Minimally intrusive methods for sampling persons in random digit dial surveys. Public Opin Q. 2004; Jun 1;68(2):267–74.
Kumar RV. Respondent selection methods in household surveys. Jharkhand Journal of development and management studies. Available at SSRN. https://ssrn.com/abstract=2392928
World Health Organization. Clinical guidelines for the management of hypertension. 2005.
Kenya stepwise survey for non-communicable diseases risk factors 2015 report [INTERNET]: Ministry of Health. Available from www.health.go.ke/wp-content/uploads/2016/04/Executive-summary-6-2.pdf
World Health Organization. Global database on body mass index. 2006 [internet]. Available from apps.who.int/bmi/index.jsp?introPage=intro_3.html.
Plüddemann A, Thompson M, Price CP, Wolstenholme J, Heneghan C. Point-of-care testing for the analysis of lipid panels: primary care diagnostic technology update. Br J Gen Pract. 2012 Mar 1;62(596):e224–6.
World Health Organization. Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia. Available from http://www.who.int/diabetes/publications
Khanam MA, Lindeboom W, Razzaque A, Niessen L, Milton AH. Prevalence and determinants of pre-hypertension and hypertension among the adults in rural Bangladesh: findings from a community-based study. BMC Public Health. 2015;15(1):1. doi:10.1186/s12889-015-1520-0.
Iwelunmor J, Airhihenbuwa CO, Cooper R, Tayo B, Plange-Rhule J, Adanu R, et al. Prevalence, determinants and systems-thinking approaches to optimal hypertension control in West Africa. Global Health. 2014;10(1):1. doi:10.1186/1744-8603-10-42.
Basu S, Millett C. Social epidemiology of hypertension in middle-income countries determinants of prevalence, diagnosis, treatment, and control in the WHO SAGE study. Hypertension. 2013;62(1):18–26. doi:10.1161/HYPERTENSIONAHA.113.01374.
Bjertness MB, Htet AS, Meyer HE, Htike MM, Zaw KK, Oo WM, et al. Prevalence and determinants of hypertension in Myanmar-a nationwide cross-sectional study. BMC Public Health. 2016;16(1):590. doi:10.1186/s12889-016-3275-7.
Rani R, Mengi V, Gupta RK, Sharma HK. Hypertension and its risk factors–a cross sectional study in an urban population of a north Indian District. Public Health Research. 2015;5(3):67–72.
Goma M, Nzala H, Babaniyi O, Songolo P, Cosmos Z, Rudatsikira E, et al. Prevalence of hypertension and its correlates in Lusaka urban district of Zambia : a population based survey. Int Arch Med. 2011;4(1):34. doi:10.1186/1755-7682-4-34.
Adediran O, Akintunde AA, Edo AE, Opadijo OG, Araoye AM. Impact of urbanization and gender on frequency of metabolic syndrome among native Abuja settlers in Nigeria. J Cardiovasc Dis Res. 2012 Sep 30;3(3):191–6. doi:10.4103/0975-3583.98890.
Sliwa K, Acquah L, Gersh BJ, Mocumbi AO. Impact of socioeconomic status, ethnicity, and urbanization on risk factor profiles of cardiovascular disease in Africa. Circulation. 2016;133(12):1199–208. doi:10.1161/circulationaha.114.008730.
Mohan I, Gupta R, Misra A, Sharma KK, Agrawal A, Vikram NK, et al. Disparities in prevalence of Cardiometablic risk factors in rural, urban-poor, and urban-middle class women in India. PLoS One. 2016 Feb 16;11(2):e0149437. doi:10.1371/journal.pone.0149437.
Peter LS, John B, Nadia M, Shah E, Somnath C. Hypertension among older adults in low and middle-income countries: prevalence, awareness and control. Int J Epidemiol. 2014:1–13. doi:10.1093/ije/dyt215.
Omboni S, Carabelli G, Ghirardi E, Carugo S. Awareness, treatment, and control of major cardiovascular risk factors in a small-scale Italian community: results of a screening campaign. Vas Health and Risk Manag. 2013;9:177. doi:10.2147/VHRM.S40925.
Ordunez P, Martinez R, Niebylski ML, Campbell NR. Hypertension prevention and control in Latin America and the Caribbean. J Clin Hyper. 2015 Jul 1;17(7):499–502.
Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013; Sep 4;310(9):959–68.
Irazola VE, Gutierrez L, Bloomfield G, Carrillo-Larco RM, Dorairaj P, Gaziano T, et al. Hypertension prevalence, awareness, treatment, and control in selected LMIC communities: results from the NHLBI/UHG network of Centers of excellence for chronic diseases. Glob Heart. 2016;11(1):47–59. doi:10.1016/j.gheart.2015.12.008.
Joffres M, Falaschetti E, Gillespie C, Robitaille C, Loustalot F, Poulter N, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open. 2013 Aug 1;3(8):e003423.
Neuhauser HK, Adler C, Rosario AS, Diederichs C, Ellert U. Hypertension prevalence, awareness, treatment and control in Germany 1998 and 2008–11. J Hum Hypertens. 2015 Apr 1;29(4):247–53.
Jaramillo PL, Lopez PC, Alvarado L, Molina DI, Sanchez G, Arcos E, et al. Educational level influence in the prevalence, awareness, treatment and control of hypertension in Colombia. J Hypertens. 2015;33:e392–3.
Wang Y, Chen T, Wang K, Edwards CL. Education as an important risk factor for the prevalence of hypertension and elevated blood pressure in Chinese men and women. J Hum Hypertens. 2006;20(11):898–900. doi:10.1038/sj.jhh.1002086.
Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness, treatment, and control: the role of neighborhood context. Social Sci Med. 2007;65(9):1853–66.
Psaltopoulou T, Orfanos P, Naska A, Lenas D, Trichopoulos D, Trichopoulou A. Prevalence, awareness, treatment and control of hypertension in a general population sample of 26 913 adults in the Greek EPIC study. Int J Epidemiol. 2004 Dec 1;33(6):1345–52.
Khatib R, Schwalm JD, Yusuf S, Haynes RB, McKee M, Khan M, et al. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta-analysis of qualitative and quantitative studies. PLoS One. 2014;9(1):e84238. doi:10.1371/journal.pone.0084238.
Prezio EA, Cheng D, Balasubramanian BA, Shuval K, Kendzor DE, Culica D. Community diabetes education (CoDE) for uninsured Mexican Americans: a randomized controlled trial of a culturally tailored diabetes education and management program led by a community health worker. Diab Res Clin Pract. 2013;100(1):19–28. doi:10.1016/j.diabres.2013.01.027.
Samal D, Greisenegger S, Auff E, Lang W, Lalouschek W. The relation between knowledge about hypertension and education in hospitalized patients with stroke in Vienna. Stroke. 2007;38(4):1304–8. doi:10.1161/01.STR.0000259733.43470.27.
Mohan V, Seedat YK, Pradeepa R. The rising burden of diabetes and hypertension in southeast Asian and African regions: need for effective strategies for prevention and control in primary health care settings. Int J Hypertens. 2013; doi:10.1155/2013/409083.
Nyarko SH. Prevalence and sociodemographic determinants of hypertension history among women in reproductive age in Ghana. Int J Hypertens. 2016 Apr;20:2016.
Vargas CM, Ingram DD, Gillum RF. Incidence of hypertension and Educational attainment the NHANES I epidemiologic Followup study. Am J Epidemiol. 2000 Aug 1;152(3):272–8.
Tedesco MA, Di Salvo G, Caputo S, Natale F, Ratti G, Iarussi D, et al. Educational level and hypertension: how socioeconomic differences condition health care. J Hum Hypertens. 2001 Oct 1;15(10):727.
Kavishe B, Biraro S, Baisley K, Vanobberghen F, Kapiga S, Munderi P, et al. High prevalence of hypertension and of risk factors for non-communicable diseases (NCDs): a population based cross-sectional survey of NCDS and HIV infection in northwestern Tanzania and southern Uganda. BMC Med. 2015;13(1):1. doi:10.1186/s12916-015-0357-9.
Schneider RH, Grim CE, Rainforth MV, Kotchen T, Nidich SI, Gaylord-King C, et al. Stress reduction in the secondary prevention of cardiovascular disease randomized, controlled trial of transcendental meditation and health education in blacks. Circ Cardiovas Qual Outcomes. 2012;5(6):750–8. doi:10.1161/CIRCOUTCOMES.112.967406.
Schwandt HM, Coresh J, Hindin MJ. Marital status, hypertension, coronary heart disease, diabetes, and death among African American women and men: incidence and prevalence in the atherosclerosis risk in communities (ARIC) study participants. J Fam Issues. 2010;31(9):1211–29. doi:10.1177/0192513X10365487.
Wang H. Effects of marital status and transition on hypertension in Chinese women: a longitudinal study. [Unpublished] 2005. Presented at the 2005 Annual Meeting of the Population Association of America Philadelphia Pennsylvania March 31–April 2 2005.
Shabir D, Sajad H, Rafiq M, Ashfaq. The role of gender and their marital status in the Prevalance of hypertension in Kashmiri population. Scholars J Appl Med Sci. 2013;1(6):975–80.
Mohan I, Gupta R, Misra A, Sharma KK, Agrawal A, Vikram NK, et al. Disparities in prevalence of Cardiometablic risk factors in rural, urban-poor, and urban-middle class women in India. PLoS One. 2016; Feb 16;11(2):e0149437. doi:10.1371/journal.pone.0149437.
Ekezie J, Anyanwu EG, Danborno B, Anthony U. Impact of urbanization on obesity, anthropometric profile and blood pressure in the Igbos of Nigeria. N Am J Med Sci. 2011;3(5):242. doi:10.4297/najms.2011.3242.
Attard SM, Herring AH, Zhang B, Du S, Popkin BM, Gordon-Larsen P. Associations between age, cohort, and urbanization with systolic and diastolic blood pressure in China: a population-based study across 18 years. J Hypertens. 2015;33(5):948–56. doi:10.1097/HJH.0000000000000522.
Bhansali A, Dhandania VK, Deepa M, Anjana RM, Joshi SR, Joshi PP, et al. Prevalence of and risk factors for hypertension in urban and rural India: the ICMR–INDIAB study. J Hum Hypertens. 2015;29(3):204–9. doi:10.1038/jhh.2014.57.
Mathenge W, Foster A, Kuper H. Urbanization, ethnicity and cardiovascular risk in a population in transition in Nakuru, Kenya: a population-based survey. BMC Public Health. 2010;10(1):1. doi:10.1186/1471-2458-10-569.
Do HT, Geleijnse JM, Le MB, Kok FJ, Feskens EJ. National prevalence and associated risk factors of hypertension and prehypertension among Vietnamese adults. Am J Hypertens. 2015 Jan 1;28(1):89–97.
Gao Y, Chen G, Tian H, Lin L, Lu J, Weng J, et al. Prevalence of hypertension in China: a cross-sectional study. PLoS One. 2013 Jun 11;8(6):e65938.
Lloyd-Sherlock P, Beard J, Minicuci N, Ebrahim S, Chatterji S. Hypertension among older adults in low-and middle-income countries: prevalence, awareness and control. Int J Epidemiol. 2014 Feb 1;43(1):116–28.
Modesti PA, Bamoshmoosh M, Rapi S, Massetti L, Al-Hidabi D, Al GH. Epidemiology of hypertension in Yemen: effects of urbanization and geographical area. Hypertens Res. 2013;36(8):711–7. doi:10.1038/hr.2013.
Acknowledgements
The authors would like to thank the WHO Country Office Rwanda and Regional Office for Africa for providing the technical support to conduct this secondary analysis. We also thank MOH and RBC for providing the administrative approval to publish the results from the study. The authors alone are responsible for the views expressed in this article, which do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated.
Funding
The survey was conducted using funds from Government of Rwanda, the US Centers for Disease Control and Prevention, WHO and other health partners in the country.
Availability of data and materials
Data associated with this study are available on request from the corresponding author.
Author information
Authors and Affiliations
Contributions
MN participated in the development of the research protocol, study design, data collection and analysis and drafting of the manuscript. AN participated in the development of the research protocol, study design, data collection and analysis, and drafting of the manuscript. MAM participated in the data collection and analysis and drafting of the manuscript. OO participated in the conception of this study, data analysis and drafting of the manuscript. JUC participated in the data analysis and drafting of the manuscript. AR participated in the development of the research protocol, study design, data collection and analysis and drafting of the manuscript. JBK participated in the development of the research protocol, study design, data collection and analysis and drafting of the manuscript. CTN was involved in data analysis and drafting of the manuscript. JBG participated in data analysis and drafting of the manuscript. MOO and JCO participated in data analysis and drafting of the manuscript. All authors revised, made significant inputs into all the drafts of the manuscript, read and approved the final draft and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Authors’ information
MN, CTN, OO and AR are epidemiologists and members of staff of WHO Rwanda and were directly responsible for the planning, implementation, monitoring and supervision of the organization’s NCD activities in Rwanda. AN is a Medical Education and Research Officer in Ministry of Health, MAM is Head of Non-Communicable Diseases program in Rwanda, JBK was HMIS Advisor in CDC Rwanda, JBG is health promotion program officer in WHO Rwanda, JUC is the Director General of Rwanda Biomedical Center. MOO and JCO are staff members of the WHO Regional Office for Africa.
Ethics approval and consent to participate
The Rwanda National Ethic Committee and the US Centers for Disease Control and Prevention provided ethical clearance to conduct the survey; informed written consent was obtained from each study participant prior to interview for steps 1 and 2. To participate in step 3 (biochemical measurement), a separate consent form was obtained from respondents. Participants who were identified as being at high risk of developing, or with, advanced chronic conditions were referred for a follow-up clinical examination. We sought and obtained the administrative clearance from the Ministry of health and WHO (WHO e-Pub no: ePub-IP-00075109-EC) to publish the results.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional information
An erratum to this article is available at https://doi.org/10.1186/s12889-017-4709-6.
Additional files
Additional file 1:
STEPS Survey Sampling Flowchart. (DOCX 172 kb)
Additional file 2:
Variables Re-categorized from the Original Dataset. (DOCX 13 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Nahimana, MR., Nyandwi, A., Muhimpundu, M.A. et al. A population-based national estimate of the prevalence and risk factors associated with hypertension in Rwanda: implications for prevention and control. BMC Public Health 18, 2 (2018). https://doi.org/10.1186/s12889-017-4536-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-017-4536-9