Abstract
Background
Early studies have suggested that biomass cooking fuels were associated with increased risk of low birth weight (LBW). However it is unclear if this reduced birth weight was due to prematurity or intrauterine growth restriction (IUGR).
Methods
In order to understand the relationship between various cooking fuels and risk of LBW and small for gestational age (SGA), we analyzed data from a birth cohort study conducted in Lanzhou, China which included 9,895 singleton live births.
Results
Compared to mothers using gas as cooking fuel, significant reductions in birth weight were observed for mothers using coal (weight difference = 73.31 g, 95 % CI: 26.86, 119.77) and biomass (weight difference = 87.84 g, 95 % CI: 10.76, 164.46). Using biomass as cooking fuel was associated with more than two-fold increased risk of LBW (OR = 2.51, 95 % CI: 1.26, 5.01), and the risk was mainly seen among preterm births (OR = 3.43, 95 % CI: 1.21, 9.74). No significant associations with LBW were observed among mothers using coal or electromagnetic stoves for cooking.
Conclusions
These findings suggest that exposure to biomass during pregnancy is associated with risk of LBW, and the effect of biomass on LBW may be primarily due to prematurity rather than IUGR.
Similar content being viewed by others
Background
Low birth weight (LBW, <2,500 grams) is an important indirect cause of infant death worldwide [21] and more than half of neonatal deaths occur among LBW infants [2]. LBW has also been associated with delayed childhood development [30] as well as metabolic, infectious, and chronic diseases later in life [4, 28, 41]. It has been estimated that globally approximately 21 million infants are born with LBW each year. Incidence of LBW varies significantly across countries, ranging from 6 to 18 % with the majority of LBW infants occurring in Asia. Although China has a relatively low prevalence of LBW, it contributes significantly to the overall number of LBW worldwide given its large population size [39.]. Underlying biological contributors to LBW include prematurity (gestational age <37 weeks) and intrauterine growth restriction (IUGR) as measured by small for gestational age (SGA) [8].
Studies have linked LBW with certain environmental factors, such as maternal smoking and ambient air pollution [11, 19, 35, 38]. Exposure to household air pollution resulting from cooking fuels has also been suggested as an important cause of LBW in developing countries [26]. Several studies reported that exposure to biomass smoke was associated with an increased risk of LBW [1, 5, 15, 23, 33, 34, 36]. However, none of these studies have controlled for gestational age. It is unclear whether biomass smoke was associated with prematurity or intrauterine growth restriction. To advance the understanding of the relationship between cooking fuels and risk of LBW, we analyzed data from a birth cohort study conducted in Lanzhou, China to examine the association between specific cooking fuel types and the risk of LBW as well as SGA.
Methods
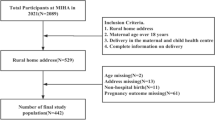
The present study was based on data from a birth cohort study conducted during 2010-2012 at the Gansu Provincial Maternity & Child Care Hospital (GPMCCH), the largest maternity and childcare hospital in Lanzhou, China [27]. A total of 14,359 women aged 18 years or older, with no history of mental illness and gestational ages ≥20 completed weeks were eligible for the study. Of the eligible women, 3,712 refused to participate and 105 did not complete in-person interviews, which yielded 10,542 (73.4 %) women who participated in the study and completed in-person interviews. The distributions for maternal age and birth outcomes (i.e., multiple births, birth defects, and low birth weight) were similar for participants and non-participants. After excluding multiple births (n = 323), stillbirths (n = 40), birth defects (n = 253), births with missing information on birth weight (n = 30), and gestational age <22 weeks (n = 1), the analytic sample size was 9,895.
All study procedures were ethically approved by the Yale University Human Investigation Committee and GPMCCH Institutional Review Board
Eligible women were informed of the study procedure upon their arrival at the hospital for delivery. After obtaining written consent, an in-person interview was conducted at the hospital either before or after delivery by trained study interviewers using a standardized and structured questionnaire. The questionnaire collected information regarding demographic factors, reproductive history, medical conditions and medication use, occupational exposures, and residential history.
Each participant was asked about current and past residences throughout her lifetime, including length of time residing at each residence (measured by dates of move-in and move-out). For each current and past residence, participants were asked about type of cooking fuel utilized (gas, coal, biomass, electromagnetic and others), ventilation practices while cooking, most frequently used types of cooking oil (e.g., canola oil, soybean oil, peanut oil, etc.), and the most commonly used cooking method (e.g., deep fried, pan fried, braised, etc.).
Information on birth outcomes and pregnancy complications were abstracted from medical records. Birth weight was measured in grams by trained professional nurses within the first hour of life. According to World Health Organization, LBW is defined as birth weight <2,500 grams, normal birth weight (NBW) is defined as birth weight between 2,500 grams and <4,000 grams, and macrosomia is defined as birth weight ≥4,000 grams [39].
Gestational age was calculated in completed pregnancy weeks based on the date of the last menstrual period. Information on last menstrual period was extracted from medical records. All self-reported last menstrual period dates were further verified by ultrasound examinations during antenatal care in the hospital. SGA, a measure of IUGR, is defined as a specified birth weight below the 10th percentile for gestational age of a reference standard; appropriate for gestational age (AGA) and large for gestational age (LGA) are specified as birth weights between the 10th and 90th and greater than 90th percentiles, respectively, for gestational age of the same reference standard [8]. We constructed SGA and AGA in our population based on the 2014 reference of Chinese infants from 28 to 44 gestation weeks [10]. Since there was no reference in the Chinese population for infants less than 28 weeks of gestation (n = 17), a United States national reference was applied for those with gestational ages between 22 and 27 weeks [12].
Chi-square or Fisher exact tests were employed to compare selected characteristics between LBW and NBW and between SGA and AGA. ANOVA tests were utilized to compare infants’ mean birth weights among women who utilized various types of cooking fuel during pregnancy. Unconditional logistic regression models were used to examine associations between cooking fuel and LBW and SGA. Potential confounding factors including maternal age, education, family income, parity, maternal weight gain during pregnancy, caesarean section, preeclampsia, vitamin supplements during pregnancy, smoking (active and passive), ventilation while cooking, and gestational age were included in the final models. Additional adjustment for maternal pre-pregnancy body mass index (BMI), alcohol consumption during pregnancy, gestational diabetes, infant gender, cooking temperature, and cooking oil type did not result in material changes in the observed associations and thus were not included in the final models. Odds ratios (OR) and 95 % confidence intervals (CI) were calculated using an unconditional logistic regression model. All analyses were performed using SAS 9.3 version (SAS Institute, Inc., Cary, NC).
Results
In our cohort, 650 births were LBW and 8,581 were NBW while 746 births were SGA and 7,775 were AGA (Table 1). Compared to mothers with NBW or AGA infants, mothers of LBW or SGA infants were more likely to have lower education, lower family income, less weight gain during pregnancy, higher incidence of caesarean section and preeclampsia, exposure to passive/active smoking, poor cooking ventilation, and no vitamin supplementation during pregnancy. No differences in gestational diabetes, alcohol consumption during pregnancy, and infants’ gender were observed between LBW and NBW groups or between SGA and AGA groups. Women with LBW infants were more likely to be either younger (<25 years) or older (≥30 years) than women with NBW infants, while women with SGA infants were younger compared to women with AGA infants. Women with LBW or SGA infants were less likely to be primiparous compared to women with NBW or AGA infants. There was no difference in pre-pregnancy BMI between LBW and NBW groups; however, women with SGA infants were more likely to be classified as underweight (BMI ≤18.5 kg/m2) compared to women with AGA infants.
In our study population, 7,907 participants exclusively used gas as their cooking fuel, 358 exclusively used coal, 120 exclusively used biomas, and 487 exclusively used electromagnetic stoves (Table 2). A total of 1,023 participants used other fuels or multiple stoves (n = 168, 1.7 %) for cooking. A total of 140 participants used electromagnetic stoves and other stoves simultaneously, which accounted for approximately 22.3 % of women who ever used electromagnetic stoves. Women who used coal, biomass, or electromagnetic stoves were younger and less educated, and had lower family income and vitamin supplementation intake compared to women who used gas stoves. They were also more likely to be multiparous, have higher BMI, be diagnosed with preeclampsia, and report exposure to tobacco smoke during pregnancy. Women who used coal or biomass were more likely to have a higher caesarean section rate as compared to those who used gas. Infants delivered by women who used coal, biomass, or electromagnetic stoves were more likely to be LBW or SGA. Women who used coal, biomass, or electromagnetic stoves were also more likely to report poor cooking ventilation compared to those who used gas stoves.
Table 3 displays mean birth weight for each type of cooking fuel, as well as estimates for the difference in mean birth weight for biomass, electromagnetic, and coal stove users compared to gas stove users after controlling for potential confounders. The mean birth weight of the entire study population was 3,270 g (standard deviation, SD: 536 g). The mean birth weight of infants from households using biomass stoves was the lowest, followed by those using coal, electromagnetic, and gas stoves, respectively. Compared to households using gas, there were significant reductions in birth weight among households using coal (weight difference = 73 g, 95 % CI: 27, 120) or biomass (weight difference = 88 g, 95 % CI: 11, 164).
The association between the various cooking fuels and LBW is presented in Table 4. Compared to using gas stoves for cooking, use of coal (OR = 1.92, 95 % CI: 1.37-2.69), biomass (OR = 3.74, 95 % CI: 2.35-5.94) or electromagnetic stoves (OR = 1.48, 95 % CI: 1.05-2.06) was associated with significantly increased risk of LBW. After additional adjustment for gestational age, only use of biomass for cooking remained statistically significant (OR = 2.51, 95 % CI: 1.26-5.01).
In our study population, 910 (9.2 %) infants were preterm, with a mean gestational age of 33.8 (SD = 2.3) weeks. Among the preterm births, 776 were moderate to late preterm births (gestational age 32–36 weeks) and 134 were very preterm births (gestational age <32 weeks). We stratified the analysis by preterm and term births (Table 5). A significant association was observed only for those using biomass as cooking fuel among preterm births, but not term births (OR = 5.24, 95 % CI: 2.03–13.53 without adjustment for gestational age; OR = 3.43, 95 % CI: 1.21–9.74 with adjustment for gestational age). We further stratified our analyses by moderate to late preterm versus very preterm births. The observed associations were similar among moderate to late preterm births compared to total preterm births. No significant association was observed among very preterm birth, however, we may be underpowered to detect this association if it exists (n = 11 exposed cases).
We further analyzed the association between cooking fuel types and the risk of SGA (Table 6). Compared to using a gas stove for cooking, use of biomass (OR = 1.22, 95 % CI: 0.70–2.08), coal (OR = 1.27, 95 % CI: 0.90–1.80), and electromagnetic stoves (OR = 1.27, 95 % CI: 0.93–1.74) were not significantly associated with the risk of SGA.
Discussion
This study is the first to investigate the associations between various types of cooking fuels and risk of LBW and SGA in the Chinese population. Our results support the hypothesis that use of biomass for cooking is associated with an increased risk of LBW compared to use of gas, and suggest that the association between biomass and LBW is likely due to prematurity but not IUGR.
Our study population primarily resided in an urban area. We noted a relatively high prevalence of gas stove use and low prevalence of biomass use compared to what we might expect in rural areas. The unbalanced prevalence of exposure may impact the accuracy of model estimation. However, the observed increased risk of LBW associated with biomass use was consistent with previous epidemiologic studies [1, 5, 15, 23, 33, 34, 36]. A cross-sectional study from India involving 14,850 infants found that using coal, kerosene, and biomass fuels for cooking was associated with a significant decrease in mean birth weight and increased risk of LBW [15]. Another Indian study including 47,139 infants reported that using biomass as cooking fuel was associated with a slightly increased risk of smaller size at birth; however, birth weight was measured indirectly, thus the results may be biased by the mother’s subjective recall [34]. A matched case-control study from the Gaza Strip including 446 births suggested that wood smoke was associated with an increased risk of LBW [1]. A retrospective population-based cohort study from Pakistan with a sample size of 634 suggested use of wood for cooking was associated with increased risk of LBW [33]. A Zimbabwean study based on 3,559 births reported that cooking with biomass was associated with reduced birth weight [23]. A study from Guatemala involving 1,717 women also showed a reduction in birth weight in association with using wood for cooking [5]. A birth cohort study of 9,604 participants reported that biomass was associated with increased risk of LBW and SGA [36]. A recent study from India that included 1,744 pregnant women found that wood fuel use was associated with non-significantly increased risk of LBW [40].
All of these published studies were conducted in areas where there was a very high prevalence of LBW, with rates as high as 33 %. In addition, the percentage of households that used biomass as a primary fuel source was also very high (up to 79 %), suggesting that the study populations had a very low socioeconomic status (SES). Malnutrition, which is common in these areas, plays an essential role in birth weight particularly in IUGR. However, neither these important confounders nor gestational age were controlled for in these prior studies.
Increased risk of LBW associated with biomass has been consistently reported in the literature, supporting our findings. Combustion of biomass fuel emits high concentrations of airborne particulate matter (PM) and toxic chemicals including carbon monoxide (CO), nitrogen dioxide (NO2), sulfur dioxide (SO2), and polycyclic aromatic hydrocarbons (PAHs) [17, 42]. When these pollutants are absorbed into the maternal bloodstream, the O2 content of maternal blood is reduced. Subsequently, O2 delivery to placenta is reduced, resulting in preterm delivery and subsequently LBW. Both epidemiological [9, 11, 13, 35, 38] and animal studies [25] have linked these pollutants to LBW. Therefore, it is biologically plausible that exposure to biomass smoke increases the risk of LBW.
Our study found that the effect of biomass on LBW was attenuated after adjusting for gestational age, which indicated a negative confounding effect. After stratification by preterm and term births, a significant association with biomass was only observed among preterm births but not term births. Our study also found no significant association between biomass and SGA, consistent with results from a recent study in India [40]. All these findings may suggest that prematurity rather than IUGR plays a major role in the association between biomass and LBW. An early study from southern India examined the effect of biomass use for cooking on LBW and SGA, and found that it was associated with both LBW and SGA, with a stronger association with LBW. In their study, the rates of LBW and SGA were approximately 33 % and 62 %, respectively [36], much higher than our study. These results suggested that if incidence of LBW was higher than 10 %, LBW was most likely caused by IUGR rather than prematurity, while if LBW incidence was less than 10 %, preterm infants constituted the majority of LBW [37]. The observed associations among preterm births need to be confirmed in future studies.
The literature has described a rapid rise in caesarean sections in China in the past decades. The current national rate is nearly 40 %, irrespective of geographic location or SES [16]. In our study population, the caesarean section rate was approximately 37.9 %, comparable to the national rate. Since the correlation between caesarean and preterm birth was relatively low (correlation coefficient = 0.08), caesarean section was unlikely a major contributor to preterm births.
A study from India reported a significant association between LBW and using coal for cooking, though they did not adjust for gestational age [15]. This was consistent with our study results prior to adjustment for gestational age; however, after controlling for gestational age the association diminished. A suggestive positive association between coal and SGA was also observed in our study. Because we cannot know if adjustment for gestational age would affect Epstein et al.’s results [15], it is unclear if the association with coal is unique to India or an artifact of uncontrolled confounding. It is possible that the level of pollutants released from combustion of coal in China is lower than those in India. A large number of studies have shown that concentrations of pollutants (i.e., CO and particular matters) released from coal are lower than those from biomass in China [14, 17, 22, 31, 32]. In addition, households in China usually use honeycomb briquettes with relatively high combustion efficiency, smoke is removed via chimney, and cooking generally occurs in a separate room or building [18]. As the majority of our study population came from an urban area, we would expect a higher percentage of households to be equipped with a chimney or hood in our study population. Our population is distinct from India, where most cooking stoves are simple (often made from mud as a U-shaped construction or three pieces of brick), have poor combustion efficiency, and are poorly ventilated [24].
We found that electromagnetic stoves were not associated with an increased risk of either LBW or SGA after controlling for gestational age. Electromagnetic stoves, more commonly known as induction cookers, use the electromagnetic induction principle to heat and cook food. Because the electromagnetic stove has many attractive features such as high energy efficiency, low noise, and no open flame, more families are beginning to replace coal, biomass, and gas stoves with induction stoves. To our knowledge, no previous study examined the association between electromagnetic stoves and LBW and SGA. Several studies have examined the association between electromagnetic fields (EMFs) and fetal growth. However, the results were inconsistent [29]. Occupational exposure to EMFs has been suggested to be associated with adverse birth outcomes (e.g., LBW, preterm, and birth defects) as reviewed by Robert [29]. Yet, studies have reported that among pregnant women, exposure to EMFs did not increase risk of LBW [3, 6, 20]. A non-significant but suggestive association between induction stove use during pregnancy and SGA in our study warrants further investigation.
The study population was recruited from the largest maternity and child care hospital in Lanzhou, the capital city of Gansu Province. The majority of study population came from Lanzhou City. Approximately 20 % of the remaining study population came from other cities and towns in Gansu Province. Although the study was hospital-based, which might impact generalizability, the LBW rate (6.2 %) in our study population was similar to the previously reported LBW rate (5.0 %) in all of Gansu Province [7].
Strengths and limitations should be considered when interpreting the study results. Information on birth weight was obtained from medical records and birth weight was measured in grams by trained professional nurses within the first hour of life, minimizing potential misclassification of the outcome. Information on gestational age was available, which allowed us to not only control for gestational age when studying the relationship with LBW, but also examine the association with SGA. One concern is that information on household heating source was not collected in the study. Since the majority of the study population came from urban areas where heating was centralized, the number of households using other fuels (such as coal or biomass) for heating was expected to be minimal. Generally households using coal or biomass for heating were likely to have lower SES; therefore we adjusted for SES (using education and family income as proxies) in our models. Lack of information regarding whether study participants were the primary person in charge of food preparation, number of meals cooked per day, and time spent in the kitchen might result in exposure misclassification. However exposure misclassification would likely be non-differential, if any, resulting in an underestimation of the observed associations. Given the various sources and factors that might influence indoor air pollution, it is important for future studies to employ more accurate methods, such as household or portable air quality monitors, to assess indoor air pollutants exposure.
Conclusions
Our findings provided further support for the hypothesis that exposure to biomass is associated with an increased risk of LBW. Our study suggests that the effect of biomass smoke on LBW could be primarily due to prematurity rather than IUGR. Future studies are needed to clarify the biological mechanisms underlying the association. Additionally, a suggestive association between induction stove use and SGA warrants further investigation.
Abbreviations
- AGA:
-
Appropriate for gestational age
- CI:
-
Confidence interval
- CO:
-
Carbon monoxide
- EMF:
-
Electromagnetic field
- GPMCCH:
-
Gansu Provincial Maternity & Child Care Hospital
- IUGR:
-
Intrauterine growth restriction
- LBW:
-
Low birth weight
- LGA:
-
Large for gestational age
- NBW:
-
Normal birth weight
- NO2:
-
Nitrogen dioxide
- OR:
-
Odds ratio
- PAH:
-
Polycyclic aromatic hydrocarbon
- PM:
-
Particulate matter
- SD:
-
Standard deviation
- SES:
-
Socioeconomic status
- SGA:
-
Small for gestational age
- SO2:
-
Sulfur dioxide
References
Abusalah A, Gavana M, Haidich AB, Smyrnakis E, Papadakis N, Papanikolaou A, et al. Low birth weight and prenatal exposure to indoor pollution from tobacco smoke and wood fuel smoke: a matched case-control study in Gaza Strip. Matern Child Health J. 2012;16(8):1718–27.
Adetola AO, Tongo OO, Orimadegun AE, Osinusi K. Neonatal mortality in an urban population in Ibadan, Nigeria. Pediatr Neonatol. 2011;52(5):243–50.
Auger N, Joseph D, Goneau M, Daniel M. The relationship between residential proximity to extremely low frequency power transmission lines and adverse birth outcomes. J Epidemiol Community Health. 2011;65(1):83–5.
Barker DJ, Eriksson JG, Forsen T, Osmond C. Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol. 2002;31(6):1235–9.
Boy E, Bruce N, Delgado H. Birth weight and exposure to kitchen wood smoke during pregnancy in rural Guatemala. Environ Health Perspect. 2002;110(1):109–14.
Bracken MB, Belanger K, Hellenbrand K, Dlugosz L, Holford TR, McSharry JE, et al. Exposure to electromagnetic fields during pregnancy with emphasis on electrically heated beds: association with birthweight and intrauterine growth retardation. Epidemiology. 1995;6(3):263–70.
Cheng N, Bai Y, Hu X, Pei H, Li Y, Zhang W, et al. Prevalence of birth defects and rubella infection in pregnant women in Gansu, west China. A survey. J Reprod Med. 2003;48(11):869–74.
Christian P, Lee SE, Donahue Angel M, Adair LS, Arifeen SE, Ashorn P, et al. Risk of childhood undernutrition related to small-for-gestational age and preterm birth in low- and middle-income countries. Int J Epidemiol. 2013;42(5):1340–55.
Dadvand P, Parker J, Bell ML, Bonzini M, Brauer M, Darrow LA, et al. Maternal exposure to particulate air pollution and term birth weight: a multi-country evaluation of effect and heterogeneity. Environ Health Perspect. 2013;121(3):267–373.
Dai L, Deng C, Li Y, Zhu J, Mu Y, Deng Y, et al. Birth weight reference percentiles for Chinese. Plos One. 2014;9(8), e104779.
Darrow LA, Klein M, Strickland MJ, Mulholland JA, Tolbert PE. Ambient air pollution and birth weight in full-term infants in Atlanta, 1994–2004. Environ Health Perspect. 2011;119(5):731–7.
Duryea EL, Hawkins JS, McIntire DD, Casey BM, Leveno KJ. A revised birth weight reference for the United States. Obstet Gynecol. 2014;124(1):16–22.
Ebisu K, Bell ML. Airborne PM2.5 chemical components and low birth weight in the northeastern and mid-Atlantic regions of the United States. Environ Health Perspect. 2012;120(12):1746–52.
Edwards RD, Liu Y, He G, Yin Z, Sinton J, Peabody J, et al. Household CO and PM measured as part of a review of China’s National Improved Stove Program. Indoor Air. 2007;17(3):189–203.
Epstein MB, Bates MN, Arora NK, Balakrishnan K, Jack DW, Smith KR. Household fuels, low birth weight, and neonatal death in India: the separate impacts of biomass, kerosene, and coal. Int J Hyg Environ Health. 2013;216(5):523–32.
Feng XL, Wang Y, An L, Ronsmans C. Cesarean section in the People’s Republic of China: current perspectives. Int J Womens Health. 2014;6:59–74.
Jin Y, Zhou Z, He G, Wei H, Liu J, Liu F, et al. Geographical, spatial, and temporal distributions of multiple indoor air pollutants in four Chinese provinces. Environ Sci Technol. 2005;39(24):9431–9.
Kan X, Chiang CY, Enarson DA, Chen W, Yang J, Chen G. Indoor solid fuel use and tuberculosis in China: a matched case-control study. BMC Public Health. 2011;11:498.
Lee NL, Samet JM, Yang G, Zhou M, Yang J, Correa A, et al. Prenatal secondhand smoke exposure and infant birth weight in China. Int J Environ Res Public Health. 2012;9(10):3398–420.
Mahram M, Ghazavi M. The effect of extremely low frequency electromagnetic fields on pregnancy and fetal growth, and development. Arch Iran Med. 2013;16(4):221–4.
Mathews TJ, MacDorman MF. Infant mortality statistics from the 2006 period linked birth/infant death data set. Natl Vital Stat Rep. 2010;58(17):1–31.
Mestl HE, Aunan K, Seip HM, Wang S, Zhao Y, Zhang D. Urban and rural exposure to indoor air pollution from domestic biomass and coal burning across China. Sci Total Environ. 2007;377(1):12–26.
Mishra V, Dai X, Smith KR, Mika L. Maternal exposure to biomass smoke and reduced birth weight in Zimbabwe. Ann Epidemiol. 2004;14(10):740–7.
Mishra VK, Retherford RD, Smith KR. Biomass cooking fuels and prevalence of tuberculosis in India. Int J Infect Dis. 1999;3(3):119–29.
Neale RJ. Effect of moderate carbon-monoxide exposure on fetal development. Lancet. 1972;2(7792):1419.
Pope DP, Mishra V, Thompson L, Siddiqui AR, Rehfuess EA, Weber M, et al. Risk of low birth weight and stillbirth associated with indoor air pollution from solid fuel use in developing countries. Epidemiol Rev. 2010;32(1):70–81.
Qiu J, He X, Cui H, Zhang C, Zhang H, Dang Y, et al. Passive smoking and preterm birth in urban China. Am J Epidemiol. 2014;180(1):94–102.
Qureshi A, Ijaz S, Syed A, Qureshi A, Khan AA. Periodontal infection: a potential risk factor for pre-term delivery of low birth weight (PLBW) babies. J Pakistan Med Assoc. 2005;55(10):448–52.
Robert E. Intrauterine effects of electromagnetic fields--(low frequency, mid-frequency RF, and microwave): review of epidemiologic studies. Teratology. 1999;59(4):292–8.
Salas J, Xaverius PK, Chang JJ. Does a medical home influence the effect of low birthweight on health outcomes? Matern Child Health J. 2012;16 Suppl 1:S143–150.
Shen G, Tao S, Wei S, Chen Y, Zhang Y, Shen H, et al. Field measurement of emission factors of PM, EC, OC, parent, nitro-, and oxy- polycyclic aromatic hydrocarbons for residential briquette, coal cake, and wood in rural Shanxi, China. Environ Sci Technol. 2013;47(6):2998–3005.
Shen G, Yang Y, Wang W, Tao S, Zhu C, Min Y, et al. Emission factors of particulate matter and elemental carbon for crop residues and coals burned in typical household stoves in China. Environ Sci Technol. 2010;44(18):7157–62.
Siddiqui AR, Gold EB, Yang X, Lee K, Brown KH, Bhutta ZA. Prenatal exposure to wood fuel smoke and low birth weight. Environ Health Perspect. 2008;116(4):543–9.
Sreeramareddy CT, Shidhaye RR, Sathiakumar N. Association between biomass fuel use and maternal report of child size at birth--an analysis of 2005-06 India Demographic Health Survey data. BMC Public Health. 2011;11:403.
Stieb DM, Chen L, Eshoul M, Judek S. Ambient air pollution, birth weight and preterm birth: a systematic review and meta-analysis. Environ Res. 2012;117:100–11.
Tielsch JM, Katz J, Thulasiraj RD, Coles CL, Sheeladevi S, Yanik EL, et al. Exposure to indoor biomass fuel and tobacco smoke and risk of adverse reproductive outcomes, mortality, respiratory morbidity and growth among newborn infants in south India. Int J Epidemiol. 2009;38(5):1351–63.
Villar J, Belizan JM. The relative contribution of prematurity and fetal growth retardation to low birth weight in developing and developed societies. Am J Obstet Gynecol. 1982;143(7):793–8.
Wang X, Ding H, Ryan L, Xu X. Association between air pollution and low birth weight: a community-based study. Environ Health Perspect. 1997;105(5):514–20.
WHO Ua. United Nations Children’s Fund and World Health Organizatio. Low Birthweight Country, regional and global estimates. New York: UNICEF; 2004.
Wylie BJ, Coull BA, Hamer DH, Singh MP, Jack D, Yeboah-Antwi K, et al. Impact of biomass fuels on pregnancy outcomes in central East India. Environ Health. 2014;13(1):1.
Xiao X, Zhang ZX, Li WH, Feng K, Sun Q, Cohen HJ, et al. Low birth weight is associated with components of the metabolic syndrome. Metabolism. 2010;59(9):1282–6.
Zhang JJ, Smith KR. Household air pollution from coal and biomass fuels in China: measurements, health impacts, and interventions. Environ Health Perspect. 2007;115(6):848–55.
Acknowledgements
We gratefully appreciate the time and effort of study participants. The study was supported by internal funding from the Gansu Provincial Maternity & Child Care Hospital, Gansu Provincial Science and Technology Department Grant (1204WCGA021), and the National Institutes of Health Grants (K02HD70324).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors declare they have no competing interests.
Authors’ contributions
MJ and CL developed the first manuscript draft. YZ, JQ, QL and SW contributed to the study design and oversaw the field implementation. YZ, MZ, XH, and HC developed the initial protocol. LL, XL, CZ, HZ, RX, DZ, YD, XH, HZ, HB, YC, ZT, RL, TY, JS, XX, XL, WW, YW, BM, and WQ contributed to the development of the study design and monitoring. CZ and XL developed the statistical analyses. MJ, HH and NZ conducted the data analyses. All authors reviewed and approved the manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Jiang, M., Qiu, J., Zhou, M. et al. Exposure to cooking fuels and birth weight in Lanzhou, China: a birth cohort study. BMC Public Health 15, 712 (2015). https://doi.org/10.1186/s12889-015-2038-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-015-2038-1