Abstract
Background
Little is known about the state of psychological distress of the elderly in China, and research on specific subgroups such as Hakka older adults is almost lacking. This study investigates psychache and associated factors among Hakka elderly in Fujian, China.
Methods
The data analysed in this study were derived from China’s Health-Related Quality of Life Survey for Older Adults 2018. The Chinese version of the Psychache Scale (PAS) was used to assess the frequency and intensity of psychache in Hakka older adults. Generalized linear regression analysis was conducted to identify the main socio-demographic factors associated with psychache overall and its frequency and intensity.
Results
A total of 1,262 older adults participated, with mean scores of 18.27 ± 6.88 for total PAS, 12.50 ± 4.79 for PAS-Frequency and 5.77 ± 2.34 for PAS-Intensity. On average, females scored higher than males on PAS-Frequency (β = 0.84, 95% CI = 0.34, 1.35) and PAS-Intensity (β = 0.48, 95% CI = 0.22, 0.73). Older adults currently living in towns (β = -2.18, 95% CI = -2.81, -1.54), with their spouse only (β = -3.71, 95% CI = -4.77, -2.65), or with children (β = -3.24, 95% CI = -4.26, -2.22) were more likely to score lower on PAS-Frequency. Conversely, older adults who were regular sleepers (β = -1.19, 95% CI =-1.49, -0.88) or lived with their spouse only (β = -1.25, 95% CI = -1.78, -0.72) were more likely to score lower on PAS-Intensity.
Conclusion
Among Hakka elderly, we found a higher frequency and greater intensity of psychache in females, those with poor health status, irregular sleepers, rural residents, solo dwellers, those with below CNY 10,000 in personal savings, and the medically uninsured. The study’s findings indicate that policymakers should give more attention to the susceptible population and implement practical interventions to reduce their psychological burden.
Similar content being viewed by others
Background
Population aging has become a significant challenge facing most countries and a global research focus for scholars [1]. Worldwide, the proportion of people aged 60 and over is growing faster than any other age group [2]. Several projections also indicate that global population aging will accelerate in the next few decades [3]. By 2050, the number of people aged 60 and over is expected to reach 22% of the world’s population [4]. The health of older people substantially influences their quality of life which can profoundly impact social development, including education, work and retirement, housing, transportation, and even built environment design. The one-child policy and increasing life expectancy in China have combined to produce the largest elderly population in any country [5]. Moreover, China’s population is one of the fastest aging in the world [6], and the health of its elderly population is becoming an urgent concern. Despite the predictability of population aging, China and the rest of the world are far from prepared to address this demographic transition [7]. For example, China’s elderly population still faces the problems of low health literacy, a high prevalence of chronic diseases, insufficient social participation, and neglect of mental health issues. Moreover, the country’s combined medical and health care service system is inadequate, medical security coordination capacity is low, and preventive medical services are limited.
The Decade of Healthy Aging (2021–2030) was approved by the World Health Assembly (WHA) in August 2020 and proclaimed by the United Nations General Assembly (UNGA) in December 2020 [8]. Healthy aging is a inclusive concept, defined by the World Health Organization (WHO) as the process of developing and maintaining the functional ability that enables well-being in older age [9]. Amid such advocacy of healthy aging, many studies have focused on older adults’ physical health [10, 11], recognizing that with rising age, the body ceases to be the trusted friend of youth and adulthood. Nevertheless, the health status of older adults undergoes gradual and complex change processes. Mental and physical illnesses coexist in many older adults [12]. With the development of modern medical technology, physical diseases are now fairly well controlled in elderly populations, but mental health is relatively more neglected. In China, psychiatric disorders such as anxiety and depression are becoming increasingly prevalent and need to be taken more seriously [13]. Conversely, some programs understand healthy aging only as emotional well-being, promoting life satisfaction [14]. Therefore, the mental health of older adults, as one key indicator of healthy aging [15], urgently requires more attention from all sectors of society.
Psychache is an unpleasant feeling (a suffering) of a psychological, non-physical origin. Psychache is the individual’s introspective experience of negative emotions such as guilt, despair, fear, and feelings of loss [16]. Anxiety, depression, physical pain, and chronic illness are common risk factors for psychache that may indicate suicide attempts [17]. Older adults die by suicide at a higher rate than any other age group in nearly every country globally [18]. Noteworthy is the fact that psychache has been particularly associated with suicide ideation and attempts [19]. The rates of suicidal thoughts and attempts are higher in patients with high psychological pain. As a socially vulnerable group, the elderly are more psychologically fragile and prone to psychological emotions such as sadness and fear or psychological disorders such as anxiety, depression, and tolerance of psychache [20, 21]. According to the WHO, over 20% of adults aged 60 and over suffer from a mental or neurological disorder [22], and a study in China indicated that about 28% of older adults reported feeling lonely [23]. The prevalence of depressive disorder and anxiety disorder in Chinese elderly over 65 years old was reported as 3.8% and 4.7%, respectively [24], entailing high economic costs and personal psychological distress. Many Chinese older adults have historically sought social support from family members. However, dramatic economic and sociocultural changes in China have left many older adults struggling to get the social support they need from their families [25], increasing their vulnerability to mental illnesses such as autism. Previous studies have shown that Chinese people are more likely to avoid or delay seeking help for mental illness than people of other countries because of their cultural environment [26]. This is why older adults should be considered a priority population.
There have been many reports on mental problems for different groups [27,28,29]. However, psychache falls under the category of pain science and thus differs from general psychological problems. Shneidman pointed out that psychache is the direct cause of and necessary antecedent for suicide, and that other factors such as depression and despair are only associated with suicide when linked to psychache [16]. Much of the extensive study on psychache has focused on measuring psychache [30, 31] and analyzing its relationship connects to other relevant concepts [32, 33]. In the last two decades, psychache has been widely investigated in psychiatry, especially with respect to suicide [34, 35]. Some studies have indicated that older people have the highest suicide risk of any age group [36]: among elderly individuals worldwide, the suicide rate is 31.3 per 100,000 per year, while the rate among elderly Chinese men is highest at 40.3 per 100,000 per year [37]. It is evidently necessary to study psychache in older adults. Regarding the level of psychache and related factors, Chinese and foreign scholars have mainly focused on patients suffering from certain diseases, especially cancer [38, 39], while only one study investigated older adults [40]. The “Hakka” means “guest” in Chinese, which indicates that the Hakka were historically migrant people from multiple regions. During the migration, the Hakka gradually established a village-wide living arrangement and coexisted in a large “castled house”, where they collaborated and interacted closely. However, the traditional extended family has been increasingly supplanted by private nuclear families in recent years due to lifestyle changes, and an increasing number of Hakka senior people are now living alone, which may lead to some differences existing between Hakka and other populations.Therefore, this study explores psychache in an elderly population and aims to identify its potential socio-demographic correlates using the Chinese version of the Psychache Scale (PAS). The findings will raise societal awareness about psychache in older adults and provide a reference for promoting healthy aging.
Materials and methods
Study design and participants
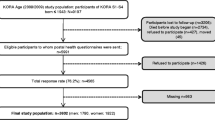
The present study is a cross-sectional, community-based survey conducted in Ninghua, Fujian. Data collection for the present study was nested in a larger cross-sectional population-based survey named the China’s Health-Related Quality of Life Survey for Older Adults 2018 (CHRQLS-OA 2018) [41]. We collected data on the socio-ecological factors and mental psychache status of the Hakka elderly. The study’s design was described in our published works [42]. A total of 1,500 questionnaires were distributed, after excluding the poorly completed questionnaires (mainly those who dropped out during of the survey), a total of 1,262 valid questionnaires were obtained, with an effective rate of 84.13%.
Measures
Participants in this study had four dimensions of demographic characteristics: individual characteristics, behavioral lifestyle, interpersonal relationships and living/ working environment. Gender, age, self-rated health status, smoking, alcohol consumption, sleep, exercise, current residence, education level, marital status, living arrangement, personal savings (CNY), medical insurance, and work status were collected as socio-demographic data of the participants. Smoking was categorized into smoking (individuals who smoke at least one cigarette per week currently) or not smoking (individuals who have never smoked or have quit smoking), and drinking was similarly classified into the binary options of drinking (individuals who drink more than one time per week) or not drinking (individuals who never drank in the past or have quit drinking). Sleep was classified as regular if answered frequently or always have sleep regularly. Conversely, they were classified as irregular sleep. Exercise was classified as frequent if answered exercise ≥ 3 times per week and for an average of ≥ 30 min each time. Conversely, they were classified as infrequent. The measures were also reported in our published work [43].
Psychache was assessed using the Chinese version of Psychache Scale (PAS) [30, 44]. The PAS was originally developed by Holden et al. [30] in 2001, and was translated into Chinese version by Yang and Chen [44] in 2017. The total PAS is a unidimensional structure with 13 items scored on a 5-point scale, score ranged from 13 to 65, with higher scores representing heavier psychache. The PAS contains two subscales: PAS-Frequency and PAS-Intensity. PAS-Frequency included nine entries describing the frequency of pain, rated from 1 (never) to 5 (always). PAS-Intensity composed of four entries reflecting the intensity of pain, rated from 1 (strongly disagree) to 5 (strongly agree). The Chinese version PAS questionnaire was identified as having good internal consistency and reliability and can be used as a measure of psychache [30, 44, 45]. The cronbach’s α coefficient for the psychache scale in the questionnaire design was 0.97.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS) version 25.0 (SPSS/ IBM Corp, Armonk, NY, USA) was employed to perform all statistical analysis work. The test level was set at α = 0.05. A summary of the demographic characteristics of the study sample was presented in the form of frequencies and proportions. Means and standard deviations (S. D) of frequency, intensity, and total PAS were calculated by demographic characteristics to assess the distribution of psychache status among major demographic characteristics of the Hakka elderly in Fujian. To analyze the factors associated with psychache affecting older adults, the variables in each of the four levels of the social-ecological model were considered independent variables in this study. During the study, psychache scale score status was used as the dependent variable, and generalized linear regression analysis models were constructed for each level of each dependent variable separately. Upon this basis, a generalized linear regression analysis model was constructed to identify the main socio-demographic factors that best predicted the psychache of the Hakka elderly by correlating the factors at multiple levels. The coefficients (β) with a 95% confidence interval (95% CI) obtained from the models were reported.
Results
Demographic characteristic of the survey participants
The study was conducted on 1,500 subjects, but 1,262 questionnaires were completed and valid (response rate 84.13%). Among these participants, 51.43% were female, and 28.21% were between 60 and 64 years old. As shown in Table 1, more than half (66.80%) of the participants were married, 53.41% had never been educated, and 15.21% had only attended literacy classes or home school. Of the 1,262 participants, 400 respondents (31.70%) lived with their spouse only, and 435 (34.47%) lived with children. About half of the participants reported general health status (56.34%). Nearly 40% of the respondents with below CNY 10,000 in personal savings and 40.41% lived in the county. Only 8.08% were medically uninsured, the other 13.07% of respondents had urban employee medical insurance (UEBMI), and 78.85% of respondents had urban and rural resident medical insurance (URRBMI). PAS scores among different subgroups are summarized in Table 1. PAS scores were further divided into three categories: PAS-Frequency, PAS-Intensity, and total PAS. To be specific, mean scores of 18.27 ± 6.88 for total PAS, 12.50 ± 4.79 for PAS-Frequency and 5.77 ± 2.34 for PAS-Intensity.
Factors affecting psychache of the Hakka elderly at each independent level
We separately included the variables in each of the four levels into the model for analysis, and the results are shown in Table 2. Among the individual trait level, differences between gender, age, self-rated health status and PAS-Frequency, PAS-Intensity, and total PAS groups were statistically significant (P < 0.05). Regarding the lifestyle and behavior level, the differences between smoking, sleep, and exercise and PAS-Frequency, PAS-Intensity, and total PAS groups were statistically significant (P < 0.05). For the interpersonal level, the differences between the subgroups of current residence, living arrangement, and PAS-Frequency were statistically significant (P < 0.05). The differences between the subgroups of current residence, education level, widowed, living arrangement, and PAS-Intensity were statistically significant (P < 0.05). The differences between the subgroups of current residence, primary education, widowed, and living arrangement and total PAS were statistically significant (P < 0.05). There was a statistically significant difference between personal savings, work status, PAS-Frequency, PAS-Intensity, and total PAS group at the level of life and work environment (P < 0.05).
Factors affecting PAS-Frequency of the Hakka elderly
As shown in Table 3, females (β = 0.84, 95% CI = 0.34, 1.35) scored higher than males in PAS-Frequency. Those aged 65 and over scored lower in PAS-Frequency as compared to those aged 60–64. Older adults with very poor/ poor self-rated health (β = 2.50, 95% CI = 1.64, 3.37) scored higher in PAS-Frequency than those with very good/good self-rated health, indicating that they were more likely to suffer from psychache frequently. Those who smoked had higher PAS-Frequency scores than those who did not smoke (β = 1.31, 95% CI = 0.67, 1.96). A lower PAS-Frequency score was found in those Hakka elderly with regular sleep than those with irregular sleep (β = -1.62, 95% CI = -2.22, -1.02). Individuals who exercised regularly (β = -1.33, 95% CI = -2.00, -0.66) had a lower PAS-Frequency. In terms of interpersonal factors, those who were currently living in town (β = -2.18, 95% CI = -2.81, -1.54), county (β = -1.79, 95% CI = -2.55, -1.03) had lower PAS-Frequency scores than those who were living in the village. With “living alone” as the reference group, people in “living with spouse only” (β = -3.71, 95% CI = -4.77, -2.65), “living with children” (β = -3.24, 95% CI = -4.26, -2.22), and “mixed habitation” groups (β = -2.96, 95% CI = -3.92, -2.00) displayed a lower score of PAS-Frequency. Compared those with personal savings below CNY 10,000, those who were classified with CNY 30 001\(\sim\)50 000 (β = -1.03, 95% CI = -2.01, -0.05), 70 001\(\sim\)100 000 (β = -1.33, 95% CI = -2.55, -0.10) had a lower score of PAS-Frequency. PAS-Frequency scores were higher among the uninsured/ unknown (β = 1.94, 95% CI = 0.94, 2.94) compared to those covered by URRBMI.
Factors affecting PAS-Intensity of the Hakka elderly
As demonstrated in Table 4, females (β = 0.48, 95% CI = 0.22, 0.73) scored higher than males in PAS-Intensity. Those with fair self-rated health (β = 0.36, 95% CI = 0.07, 0.65) and poor self-related health status (β = 0.86, 95% CI = 0.43, 1.30) scored higher in PAS-Intensity. Regular sleepers (β = -1.19, 95% CI=-1.49, -0.88) scored lower in PAS-Intensity than irregular sleepers. Those living in rural areas scored higher in PAS-Intensity than those living in towns or cities. PAS-Intensity score was higher among the older with “literacy class/ home school” education level (β = 0.82, 95% CI = 0.41, 1.24), and “primary school school” education level (β = 1.26, 95% CI = 0.81, 1.72) than the illiterate elderly. The scores of PAS-Intensity for the elderly with living arrangements of “living with spouse only” (β = -1.25, 95% CI = -1.78, -0.72), “living with children” (β = -1.12, 95% CI = -1.63, -0.61), “mixed habitation” (β = -1.06, 95% CI = -1.54, -0.58), and “others” (β = -1.85, 95% CI = -2.45, -1.26) were lower than those living alone.
Factors affecting total PAS of the Hakka elderly
Table 5 shows that females (β = 1.32, 95% CI = 0.59, 2.05) scored higher than males in total PAS. Those aged 65–69 (β = -2.64, 95% CI = -3.67, -1.62), 70–74 (β = -2.09, 95% CI = -3.17, -1.00), 75–79 (β = -2.95, 95% CI = -4.16, -1.74) and ≥ 80 years (β = -1.90, 95% CI = -3.14, -0.65) scored lower than those aged 60–64 years in total PAS. Older adults with good self-rated health scored lower than those with general (β = 0.94, 95% CI = 0.11, 1.77) and poor (β = 3.37, 95% CI = 2.12, 4.61) self-rated health in total PAS. Cigarette smokers (β = 2.20, 95% CI = 1.27, 3.13) and alcohol drinkers (β = 0.83, 95% CI = 0.09, 1.57) scored higher than non-smokers and non-drinkers in total PAS. A comparison with irregular sleepers reveals that regular sleepers (β = -2.81, 95% CI = -3.65, -1.94) scored lower on total PAS. In comparison with infrequent exercisers, it was found that frequent exercisers (β = -1.67, 95% CI = -2.63, -0.70) scored lower in total PAS. Older people living in towns (β = -3.42, 95% CI = -4.51, -2.33) or counties (β = -3.65, 95% CI = -4.57, 2.74) scored lower than those living in villages in total PAS. Higher total PAS scores were found among people with literacy class/ home school education (β = 2.96, 95% CI = 1.77, 4.16), primary school education (β = 3.81, 95% CI = 2.49, 5.12), and junior high school education and above (β = 1.95, 95% CI = 0.55, 3.36) compared to illiterate people. Those categorized as “other marital status” (β = -1.47, 95% CI = -2.71, -0.23) scored lower than in marriage/ cohabitation in total PAS. Compared to those who lived alone, those who lived with spouse only (β = -4.97, 95% CI = -6.49, -3.44), lived with children (β = -4.36, 95% CI = -5.82, -2.90), mixed living (β = -4.02, 95% CI = -5.40, -2.64), and other living arrangements (β = -6.60, 95% CI = -8.31, -4.89) were negatively associated with a higher total PAS.
Discussion
The majority of psychache research has been conducted on its correlation with mental disorders, including schizophrenia [46], bipolar disorder [47], generalized anxiety disorder [48], and obsessive-compulsive disorder [49]. There is a dearth of studies on psychache among specific subgroups such as Hakka older adults in China. Old age is a period associated with many forms of loss. A culmination of chronic physical illnesses and worsening sensory impairment can considerably affect an individual’s quality of life and psychological well-being. Previous studies have shown that the mental health of older adults is affected by gender, marital status, and social support [50]. We found that age, gender, smoking condition, sleep, exercise, current residence, living arrangement, marital status, education level and personal savings were the associated factors of psychache among Hakka elderly.
In this study of Hakka elderly, we found that females were more likely than males to feel psychache, which is consistent with prior findings [51]. The demands of traditional Chinese culture have contributed to an introversion in Chinese women’s personalities, resulting in a tendency to allow the pressure they suffer to accumulate and cause psychological pain. Chinese women are generally required to take responsibility for domestic and social work and, therefore, face home and workplace pressures. Women also experience more psychological stress than men from changes to social roles, which can easily disrupt their psychological balance. Thus, it is meaningful to support females to promptly release pent-up tension and reach out to psychological counselors for assistance if necessary.
Among the study’s participants, psychache frequency was highest among those aged 60–64 years, which seems inconsistent with previous findings [52]. Evidence suggests that the prevalence of depression tends to increase with age [53]. However some studies point to a decline in depression rates between the ages of 60 and 70, indicating that retirement is good for mental health [54]. The average age of the Fujian Hakka elderly selected for this study was higher than of the elderly in general studies, and the 60–64 age group was the youngest; members of this group may not have been fully retired yet already facing demands to care for grandchildren, resulting in more frequent psychological stress. Self-rated health status can also play a role in the psychological distress of older adults [55]. Perceiving impaired health status and cognitive decline often triggers their anxiety and, in severe cases, psychological suffering. The youth population in families are reminded to be mindful of the mental health of elderly individuals who look after their grandchildren and of parents who are in poor health conditions.
Previous studies have found that people with mental illness are more susceptible to smoking [56]. There is also some empirical evidence, mainly from the United States, that smokers with psychiatric issues make exactly as many attempts to stop as the normal smoker, but their success rate is lower [57]. Our study revealed a higher frequency of psychache among Hakka older adults who smoked, possibly because those with an indication of a mental health problem were more highly dependent on smoking and accustomed to soothing their emotions in this way [58]. Besides vulnerability to smoking, recent studies suggest that people who rely on alcohol to cope with stressful events may quickly become psychologically dependent on alcohol, and need it to withstand the resulting negative emotions from stressful events [59]. Research also suggests that heavy drinking is associated with higher levels of negative affect [60], and that older adults who experience psychological distress tend to use alcohol to enhance their positive emotions [61]. However, this study found no correlation between alcohol consumption and psychache, which may be explained by the local Chinese culture, especially the belief that “drink wine to drown your sorrow, it will heavier grow.” Social media needs to clarify awareness about the risks associated with drinking and smoking and encourage healthier ways to relieve psychological pain.
Irregular sleep and poor sleep quality are common in the elderly population. Poor sleep significantly reduces quality of life and promotes other adverse pathological outcomes, such as increased fall risk, memory problems, chronic fatigue, and weakness [62, 63]. Psychological distress has consistently been found to correlate with sleep troubles [64, 65], and this study demonstrated that psychache was more intense and/or frequent among Hakka elderly with irregular sleep. The positive association between physical exercise and mental health has also been widely discussed and extensively documented [66,67,68]. Older adults who engage in high levels of physical exercise tend to be more resistant to functional decline and psychological distress [68]. Therefore, we unsurprisingly found more frequent psychache in older adults who do not engage regularly in physical exercise. To avoid being psychache, elderly people should maintain regular physical activity and sleep routines.
A previous study showed that have shown that urban residents are less likely to experience depressive symptoms than rural residents [69], whereas Sengupta P et al. suggested that rural residents have a stronger sense of community belonging and are at lower risk of mental illness [70]. A study of older people in China suggested that the level of psychological pain among rural older people was more serious than among urban older [40]. Our study found that older people living in rural (vs. urban) areas were more likely to feel psychache. This could be explained by the migration of young people from rural to urban areas, resulting in a lack of social support for rural older people. Seniors living alone commonly face problems, such as loneliness, neglect, and boredom, which can affect their mental health. Previous studies show that older adults without emotional support from family members have a higher risk of psychological illness [40, 71]. Likewise, loneliness and unspoken physical and mental problems increase the frequency of psychache in our study. The government should improve welfare policies for the elderly in rural areas.
Among older adults, marital partners become increasingly important in maintaining a sense of social connectedness when family, friends, and neighbors are lost through death and relocation [72]. Marriage protects against loneliness, but not all marriages are equally protective. A study used dyadic data from the second wave (2010–11) of the National Social Life, Health, and Aging Project (NSHAP) shows that more than half of married older adults live in marital conflict, indifference, or avoidance; about one in six older married couples report moderate or high levels of loneliness [73]. Our study found a higher frequency of psychache among married/ cohabiting Hakka elders than unmarried/ divorced/ separated people. This could be explained by the older age of participants compared to other studies, since social and health transitions can increase stress and reduce marriage quality, opening the door to feelings of disconnection, isolation, and loneliness. Our findings highlight the need for further research to identify strategies to help older adults optimize their marital relationships.
Interestingly, this study found that older adults with private/ elementary school education or junior high school education had higher levels of psychache than those who were illiterate. This finding seems at odds with current understanding that low educational attainment is a risk factor for depression. Illiteracy in elderly individuals was found to be associated with a higher rate and increased severity of depression [74], while another study reported that higher educational attainment was associated with healthier psychological well-being [75]. The discrepancy in our findings may be linked to the uneven distribution of educational attainment among survey respondents, more than half of whom were illiterate. Income partly reflects an individual’s social status [76], and lower income can lead to greater financial dependence on family members, leaving older adults insecure and more prone to psychological pain, consistent with our survey. In addition, this study found that medically uninsured older adults had more intense and/or frequent psychache than those enrolled in urban employee health insurance, possibly because being uninsured means less security and more health risks [77], which can easily lead to poor mental health. Thus, the government should increase the amount of security subsidies for the elderly. It is also essential to appeal to children to visit older people frequently, providing a sense of security.
Limitation
As the first study targeting the Hakka elderly to reveal their psychache status and associated factors, this study has several limitations. First of all, the cross-sectional design of our study limited our ability to examine causal relationships and instead only examined correlations; hence, more prospective researches are required. Secondly, psychache may indicate suicide attempts. Yet, we did not track suicide because participant information related to suicide was not the main focus of this study. Thirdly, the Hakka elderly in the present study were from Fujian, China. Nonetheless, the Hakka population is also dispersed throughout Southeast Asia, including Thailand, Malaysia, and Singapore, as well as Guangdong and Jiangxi in China. Our samples are not representative of the entire Hakka population. Therefore, the conclusions of this study need to be cautious when extrapolating. Additional research on comparing the Hakka elderly with the general Chinese elderly population is imperative. In addition, some variables were limited by the questionnaire and relied on the self-reporting for categorization are vulnerable to recall bias.
Conclusion
In short, this study provides comprehensive understanding of psychache in the Hakka elderly of Fujian. The results revealed more intense and/or frequent psychache in females, 60–64-year-olds, those with poor self-rated health, smokers, irregular sleepers, infrequent exercisers, rural residents, solo dwellers, those with personal savings below CNY 10,000, and the medically uninsured. Hence, Hakka older adults with any of these characteristics should be given more attention. China’s policymakers and health professionals should initiate practicable interventions to reduce the psychological burden on older adults, which could be conducive to preventing and controlling their mental health problems. Future studies should conduct longitudinal investigations of the influencing factors of psychache. Studying Hakka people in different regions would produce more generalizable findings.
Data availability
The datasets used and/or analysed during the current study are available from the first and/ or corresponding author(s) on reasonable request because the datasets contain sensitive material that can identify participant information.
Abbreviations
- CI:
-
Confidence interval
- OR:
-
Odds ratios
- SPSS:
-
Statistical Package for the Social Sciences
- CNY:
-
China Yuan
- URRBMI:
-
Urban and rural residents’ basic medical insurance
- UEBMI:
-
Urban employees basic medical insurance
- CHRQLS-OA 2018:
-
China’s Health-Related Quality of Life Survey for Older Adults 2018
- χ 2 :
-
Chi-square value
- β :
-
Coefficient
- n:
-
Subsample
References
Lee R. The outlook for population growth. Science. 2011;333(6042):569–73.
World Health Organization: active aging: a policy framework. Geneva 2002.
Wu L, Huang Z, Pan Z. The spatiality and driving forces of population ageing in China. PLoS ONE. 2021;16(1):e0243559.
Kanasi E, Ayilavarapu S, Jones J. The aging population: demographics and the biology of aging. Periodontol 2000. 2016;72(1):13–8.
Sun J, Xiao T, Lyu S, Zhao R. The relationship between Social Capital and depressive symptoms among the Elderly in China: the mediating role of life satisfaction. Risk Manag Healthc Policy. 2020;13:205–13.
Zhao Y, Smith JP, Strauss J. Can China age healthily? Lancet. 2014;384(9945):723–4.
da Silva JB Jr., Rowe JW, Jauregui JR. Healthy aging in the Americas. Rev Panam Salud Publica. 2021;45:e116.
Guillén MF. 2030: How Today’s Biggest Trends Will Collide and Reshape the Future of Everything. New York: St. Martin’s Press; 2020.
Rudnicka E, Napierała P, Podfigurna A, Męczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. 2020;139:6–11.
Jeong GW, Kim YJ, Park S, Kim H, Kwon O. Associations of recommended food score and physical performance in Korean elderly. BMC Public Health. 2019;19(1):128.
Li J, Lin S, Yan X, Wei Y, Yang F, Pei L. Cross-country comparison of income-related inequality in physical functional disability among middle-aged and older adults: evidence from 33 countries. J Glob Health. 2023;13:04053.
Raju M. Population Ageing and the Elderly. Indian J Psychiatry. 2018;60(Suppl 3):S295.
Ding KR, Wang SB, Xu WQ, Lin LH, Liao DD, Chen HB, Tan WY, Huang JH, Hou CL, Jia FJ. Low mental health literacy and its association with depression, anxiety and poor sleep quality in Chinese elderly. Asia Pac Psychiatry. 2022;14(4):e12520.
Estebsari F, Taghdisi MH, Rahimi Foroushani A, Eftekhar Ardebili H, Shojaeizadeh D. An educational program based on the successful aging approach on health-promoting behaviors in the elderly: a clinical trial study. Iran Red Crescent Med J. 2014;16(4):e16314.
Abdul Manaf MR, Mustafa M, Abdul Rahman MR, Yusof KH, Abd Aziz NA. Factors influencing the prevalence of Mental Health problems among malay Elderly Residing in a Rural Community: a cross-sectional study. PLoS ONE. 2016;11(6):e0156937.
Shneidman ES. Suicide as psychache. J Nerv Ment Dis. 1993;181(3):145–7.
Cavusoglu C, Ileri I, Tuna Dogrul R, Ozsurekci C, Caliskan H, Cemal Kizilarslanoglu M, Goker B. Relationship between psychological pain and death anxiety with comprehensive geriatric assessment in older adults. Geriatr Gerontol Int. 2020;20(11):1056–60.
Stanley IH, Hom MA, Rogers ML, Hagan CR, Joiner TE Jr. Understanding suicide among older adults: a review of psychological and sociological theories of suicide. Aging Ment Health. 2016;20(2):113–22.
Campos RC, Holden RR. Psychological pain and previous suicide attempts in young adults: results with the Portuguese version of the Psychache Scale. J Clin Psychol. 2020;76(10):1965–71.
Sharma M, Bhattarai T, Sharma P. Anxiety and depression among senior citizens. J Nepal Health Res Counc. 2021;19(2):305–10.
Demirkol ME, Tamam L, Namli Z, Davul Ö. Validity and reliability study of the Turkish version of the tolerance for mental pain scale-10. Psychiatry Clin Psychopharmacol. 2019;29(4):899–906.
World Health Organization. Mental health of older adults [https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults].
Luo Y, Waite LJ. Loneliness and mortality among older adults in China. J Gerontol B Psychol Sci Soc Sci. 2014;69(4):633–45.
Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, Yu Y, Kou C, Xu X, Lu J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6(3):211–24.
Chen S, Conwell Y, Chiu HF. Loneliness and aging in China–a public health problem in need of solutions. Int Psychogeriatr. 2014;26(11):1771–2.
Chiu M. Ethnic Differences in Mental Health and Race-Based Data Collection. Healthc Q. 2017;20(3):6–9.
Santini ZI, Jose PE, York Cornwell E, Koyanagi A, Nielsen L, Hinrichsen C, Meilstrup C, Madsen KR, Koushede V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. 2020;5(1):e62–70.
Woolston C. Depression and anxiety ‘the norm’ for UK PhD students. Nature 2021.
Pile V, Williamson G, Saunders A, Holmes EA, Lau JYF. Harnessing emotional mental imagery to reduce anxiety and depression in young people: an integrative review of progress and promise. Lancet Psychiatry. 2021;8(9):836–52.
Holden, Ronald R, Mehta, Karishma, Cunningham E. Jane, McLeod, Lindsay: Development and preliminary validation of a scale of psychache. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement 2001.
Shneidman ES. The psychological pain assessment scale. Suicide Life Threat Behav. 1999;29(4):287–94.
Li H, Fu R, Zou Y, Cui Y. Predictive roles of three-Dimensional Psychological Pain, Psychache, and depression in suicidal ideation among Chinese College students. Front Psychol. 2017;8:1550.
Bäck K, Hakeberg M, Wide U, Hange D, Dahlström L. Orofacial pain and its relationship with oral health-related quality of life and psychological distress in middle-aged women. Acta Odontol Scand. 2020;78(1):74–80.
Chodkiewicz J, Miniszewska J, Strzelczyk D, Gąsior K. Polish adaptation of the Psychache Scale by Ronald Holden and co-workers. Psychiatr Pol. 2017;51(2):369–81.
Verrocchio MC, Carrozzino D, Marchetti D, Andreasson K, Fulcheri M, Bech P. Mental Pain and suicide: a systematic review of the literature. Front Psychiatry. 2016;7:108.
Lindner R, Drinkmann A, Schneider B, Sperling U, Supprian T. [Suicidality in older adults]. Z Gerontol Geriatr. 2022;55(2):157–64.
Klein B, Shandley K, McLaren S, Clinnick L, Nguyen HV. Suicidality among older Australian adults. Front Public Health. 2022;10:992884.
Thapa S, Sun H, Pokhrel G, Wang B, Dahal S, Yu S. Performance of Distress Thermometer and Associated factors of psychological distress among Chinese Cancer patients. J Oncol. 2020;2020:3293589.
Ncitakalo N, Mabaso M, Joska J, Simbayi L. Factors associated with external HIV-related stigma and psychological distress among people living with HIV in South Africa. SSM Popul Health. 2021;14:100809.
Zhou H, Han D, Zhou H, Ke X, Jiang D. Influencing factors of psychological pain among older people in China: a cross-sectional study. Heliyon. 2023;9(10):e21141.
Yang Y, Wang S, Chen L, Luo M, Xue L, Cui D, Mao Z. Socioeconomic status, social capital, health risk behaviors, and health-related quality of life among Chinese older adults. Health Qual Life Outcomes. 2020;18(1):291.
Liu X, Liu F, Ruan W, Chen Y, Qu S, Wang W. Mental health status and associated contributing factors among the Hakka elderly in Fujian, China. Front Public Health. 2022;10:928880.
Yang Y, Wang S, Hu B, Hao J, Hu R, Zhou Y, Mao Z. Do older adults with parent(s) alive experience higher Psychological Pain and suicidal ideation? A cross-sectional study in China. Int J Environ Res Public Health 2020, 17(17).
Yang L, Chen W. Reliability and validity of the Psychache Scale in Chinese undergraduates. Chin J Clin Psychol 2017.
Gomes GAO, Luchesi BM, Gratão ACM, Orlandi FS, Say KG, Inouye K, Alexandre TDS, Brigola AG, Pavarini SCI. Prevalence of physical inactivity and Associated factors among older caregivers of older adults. J Aging Health. 2019;31(5):793–813.
Demirkol ME, Tamam L, Namli Z, Karaytuğ MO, Uğur K. Association of Psychache and Alexithymia with suicide in patients with Schizophrenia. J Nerv Ment Dis. 2019;207(8):668–74.
Demirkol ME, Güleç H, Tamam L, Güleç MY, Öztürk SA, Uğur K, Karaytuğ MO, Eroğlu MZ. Reliability and validity of Mee-Bunney Psychological Pain Assessment Scale Turkish version. Curr Psychol. 2020;39(4):1181–8.
Demirkol ME, Tamam L, Namli Z, Karaytuğ MO, Yeşiloğlu C. The relationship among anxiety sensitivity, psychache, and suicidality in patients with generalized anxiety disorder. J Nerv Ment Dis. 2022;210(10):760–6.
Demirkol ME, Namlı Z, Eriş Davul Ö, Karaytuğ MO, Tamam L, Yılmaz H. Psychache and suicidal history in patients with obsessive-compulsive disorder. Neuropsychiatr Dis Treat. 2019;15:3531–9.
Taylor HO, Taylor RJ, Nguyen AW, Chatters L. Social isolation, Depression, and psychological distress among older adults. J Aging Health. 2018;30(2):229–46.
Matud MP, Bethencourth JM, Ibáñez I, Fortes D. Gender and psychological well-being in older adults. Int Psychogeriatr. 2020;32(11):1293–302.
Bramajo ON. An Age-Period-Cohort Approach to Analyse Late-Life Depression Prevalence in six European countries, 2004–2016. Eur J Popul. 2022;38(2):223–45.
Bell A. Life-course and cohort trajectories of mental health in the UK, 1991–2008–a multilevel age-period-cohort analysis. Soc Sci Med. 2014;120:21–30.
Fernández-Niño JA, Bonilla-Tinoco LJ, Manrique-Espinoza BS, Romero-Martínez M, Sosa-Ortiz AL. Work status, retirement, and depression in older adults: an analysis of six countries based on the study on Global Ageing and Adult Health (SAGE). SSM Popul Health. 2018;6:1–8.
Matud MP. Masculine/Instrumental and Feminine/Expressive Traits and Health, Well-Being, and psychological distress in Spanish men. Am J Mens Health. 2019;13(1):1557988319832749.
Szatkowski L, McNeill A. Diverging trends in smoking behaviors according to mental health status. Nicotine Tob Res. 2015;17(3):356–60.
Kulik MC, Glantz SA. Softening among U.S. smokers with psychological distress: more quit attempts and lower consumption as smoking drops. Am J Prev Med. 2017;53(6):810–7.
Brose LS, Brown J, Robson D, McNeill A. Mental health, smoking, harm reduction and quit attempts - a population survey in England. BMC Public Health. 2020;20(1):1237.
Windle M, Windle RC. A prospective study of stressful events, coping motives for drinking, and alcohol use among middle-aged adults. J Stud Alcohol Drugs. 2015;76(3):465–73.
Carvalho AF, Stubbs B, Maes M, Solmi M, Vancampfort D, Kurdyak PA, Brunoni AR, Husain MI, Koyanagi A. Different patterns of alcohol consumption and the incidence and persistence of depressive and anxiety symptoms among older adults in Ireland: a prospective community-based study. J Affect Disord. 2018;238:651–8.
van Gils Y, Franck E, Dierckx E, van Alphen SPJ, Dom G. The role of psychological distress in the relationship between drinking motives and Hazardous drinking in older adults. Eur Addict Res. 2021;27(1):33–41.
Sariarslan HA, Gulhan YB, Unalan D, Basturk M, Delibas S. The relationship of sleep problems to life quality and depression. Neurosciences (Riyadh). 2015;20(3):236–42.
Martin JL, Fiorentino L, Jouldjian S, Josephson KR, Alessi CA. Sleep quality in residents of assisted living facilities: effect on quality of life, functional status, and depression. J Am Geriatr Soc. 2010;58(5):829–36.
Jiang J, Li Y, Mao Z, Wang F, Huo W, Liu R, Zhang H, Tian Z, Liu X, Zhang X, et al. Abnormal night sleep duration and poor sleep quality are independently and combinedly associated with elevated depressive symptoms in Chinese rural adults: Henan Rural Cohort. Sleep Med. 2020;70:71–8.
Zhou L, Zhang H, Luo Z, Liu X, Yang L, Hu H, Wang Y, Wang C, Wang F. Abnormal night sleep duration and inappropriate sleep initiation time are associated with elevated anxiety symptoms in Chinese rural adults: the Henan Rural Cohort. Psychiatry Res. 2020;291:113232.
Mochcovitch MD, Deslandes AC, Freire RC, Garcia RF, Nardi AE. The effects of regular physical activity on anxiety symptoms in healthy older adults: a systematic review. Braz J Psychiatry. 2016;38(3):255–61.
Tada A. Psychological effects of exercise on community-dwelling older adults. Clin Interv Aging. 2018;13:271–6.
Zhang C, Xiao S, Lin H, Shi L, Zheng X, Xue Y, Dong F, Zhang J, Xue B. The association between sleep quality and psychological distress among older Chinese adults: a moderated mediation model. BMC Geriatr. 2022;22(1):35.
Li W, Gao G, Sun F, Jiang L. The role of community factors in predicting depressive symptoms among Chinese workforce: a longitudinal study in rural and urban settings. BMC Public Health. 2022;22(1):1429.
Sengupta P, Benjamin AI. Prevalence of depression and associated risk factors among the elderly in urban and rural field practice areas of a tertiary care institution in Ludhiana. Indian J Public Health. 2015;59(1):3–8.
Tengku Mohd TAM, Yunus RM, Hairi F, Hairi NN, Choo WY. Social support and depression among community dwelling older adults in Asia: a systematic review. BMJ Open. 2019;9(7):e026667.
Ben-Zur H. Loneliness, optimism, and well-being among married, divorced, and widowed individuals. J Psychol. 2012;146(1–2):23–36.
Hsieh N, Hawkley L. Loneliness in the older adult marriage: associations with dyadic aversion, indifference, and ambivalence. J Soc Pers Relat. 2018;35(10):1319–39.
Bennett S, Thomas AJ. Depression and dementia: cause, consequence or coincidence? Maturitas. 2014;79(2):184–90.
Wang W, Dong Y, Liu X, Zhang L, Bai Y, Hagist S. The more educated, the healthier: evidence from Rural China. Int J Environ Res Public Health 2018, 15(12).
Buvneshkumar M, John KR, Logaraj M. A study on prevalence of depression and associated risk factors among elderly in a rural block of Tamil Nadu. Indian J Public Health. 2018;62(2):89–94.
Malta DC, Bernal RTI, Vieira Neto E, Curci KA, Pasinato MTM, Lisbôa RM, Cachapuz RF, Coelho KSC, Santos FPD, Freitas MIF. Noncommunicable diseases, risk factors, and protective factors in adults with and without health insurance. Cien Saude Colet. 2020;25(8):2973–83.
Acknowledgements
Not applicable.
Funding
This work is supported by the General Project of Humanities and Social Science Research of the Ministry of Education of the People’s Republic of China [Grant No. 22YJCZH112] and Fujian Basic Theory Research Foundation of Philosophy & Social Science Guided by Marxism [Grant No. JSZM2021027].
Author information
Authors and Affiliations
Contributions
XL and YC designed the study. YC and LC wrote the manuscript. WR, LZ and YC collected, analyzed and interpreted the data. XL, YC and LC critically reviewed, edited and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Data collection for this study was nested within a larger population-based cross-sectional survey–the China’s Health-Related Quality of Life Survey for Older Adults 2018 (CHRQLS-OA 2018). The survey followed the guidelines outlined in the Declaration of Helsinki, and was approved by the Institutional Review Board of School of Health Science and Faculty of Medical Sciences, Wuhan University (IRB number: 2019YF2050). Informed consent information was attached to each questionnaire and introduced before the surveys.
Consent for publication
Not applicable.
Conflicts of interest
The authors declare they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, Y., Cai, L., Ruan, W. et al. Psychache status and associated contributing factors among the Hakka elderly in Fujian, China. BMC Psychiatry 24, 354 (2024). https://doi.org/10.1186/s12888-024-05797-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-05797-x