Abstract
Background
Depression and anxiety are common and disabling mental health problems in children and young adults. Group cognitive behavioral therapy (GCBT) is considered that an efficient and effective treatment for these significant public health concerns, but not all participants respond equally well. The aim of this study was to examine the predictive ability of heart rate variability (HRV), based on sensor data from consumer-grade wearable devices to detect GCBT effectiveness in early intervention.
Methods
In a study of 33 college students with depression and anxiety, participants were randomly assigned to either GCBT group or a wait-list control (WLC) group. They wore smart wearable devices to measure their physiological activities and signals in daily life. The HRV parameters were calculated and compared between the groups. The study also assessed correlations between participants’ symptoms, HRV, and GCBT outcomes.
Results
The study showed that participants in GCBT had significant improvement in depression and anxiety symptoms after four weeks. Higher HRV was associated with greater improvement in depressive and anxious symptoms following GCBT. Additionally, HRV played a noteworthy role in determining how effective GCBT was in improve anxiety(P = 0.002) and depression(P = 0.020), and its predictive power remained significant even when considering other factors.
Conclusion
HRV may be a useful predictor of GCBT treatment efficacy. Identifying predictors of treatment response can help personalize treatment and improve outcomes for individuals with depression and anxiety.
Trial registration
The trial has been retrospectively registered on [22/06/2023] with the registration number [NCT05913349] in the ClinicalTrials.gov.
Condensed abstract
Variations in heart rate variability (HRV) have been associated with depression and anxiety, but the relationship of baseline HRV to treatment outcome in depression and anxiety is unclear. This study predicted GCBT effectiveness using HRV measured by wearable devices. 33 students with depression and anxiety participated in a trial comparing GCBT and wait-list control. HRV parameters from wearables correlated with symptoms (PHQ, PSS) and GCBT effectiveness. Baseline HRV levels are strongly associated with GCBT treatment outcomes. HRV may serve as a useful predictor of efficacy of GCBT treatment,facilitating personalized treatment approaches for individuals with depression and anxiety.
Similar content being viewed by others
Introduction
Depression and anxiety are prevalent and debilitating conditions that significantly affect children and young adults [1,2,3,4]. Previous surveys have consistently highlighted the significant impact of depression and anxiety on adolescents and young adults, with prevalence rates ranging from 23 to 39% [5]. The college years represent a critical period characterized by increased vulnerability to a wide range of mental health challenges. Recent evidence indicates rising rates of depression, anxiety, and suicidality among college students [6, 7], highlighting mental health as an escalating and serious public health concern on college campuses [8, 9]. While common psychiatric conditions often emerge during late adolescence and early adulthood [10], a growing number of college students with subthreshold mental health issues face challenges in accessing effective help due to the insufficient number or duration of symptoms to meet DSM-IV or ICD-10 criteria [11]. Consequently, these unresolved issues can potentially develop into major depressive disorder (MDD) and generalized anxiety disorder (ANX) [12, 13], leading to an increased risk of suicide and functional impairment [14, 15]. The high rate of comorbidity between anxiety and depression among college students, ranging from 4.60 to 12.98% [16], can increase the risk of developing MDD and ANX, and is associated with more severe symptoms, impaired work performance, and poorer treatment outcomes [4, 17]. Therefore, early intervention is crucial to prevent the progression of these disorders and to mitigate their associated negative consequences, there is an urgent need to regulate key factors and develop more effective prevention and intervention strategies to address these growing mental health concerns among college students.
Common preventative intervention methods for depression and anxiety include medication, psychotherapy and physiotherapy. Cognitive behavioral therapy (CBT) has received widespread attention due to its highly structured nature and good therapeutic effect [18]. And CBT practiced in a group format offers a cost-effective option that can be delivered to many participants with a minimum of time and staff numbers. Group cognitive behavioral therapy (GCBT) can achieve its therapeutic effect by enhancing emotion regulation and cognitive control to promote self-regulation, which can help individuals better manage emotional fluctuations in daily life, resulting in further improvement of depressive and anxious symptoms [19]. However, despite various forms of CBT have shown effectiveness in adults, whether this kind of early intervention has positive effects on the adolescent and young adults remains unclear [20].
In previous studies on the efficacy of GCBT, the assessment of GCBT effectiveness primarily relied on therapists and psychiatrists, who employed patient questionnaire surveys and clinical observations for identification and monitoring. Additionally, the lengthy duration of CBT may exacerbate the lag effect in retrospective evaluations, further compromising their authenticity. Relying solely on subjective description, without objective biomarkers included in the assessment process, hinders an accurate reflection of the clinical severity of the evaluation and the participants’ response to efficacy. The applications of biological markers can provide more comprehensive and rigorous analysis, enabling the identification of participants who are more likely to benefit from treatment. One validated measure of autonomic function is heart rate variability (HRV), which refers to the variation in the intervals between heartbeats and is considered an objective biological marker with the potential to predict efficacy [21]. Previous studies have shown that HRV can be used as a biomarker to assess the response of antidepressants to anxiety and depression. Patients with higher high frequency of heart rate variability spectrum (HF-HRV) tend to have better prognoses than those with lower HF-HRV in anxious depression [22]. Changes in low frequency (LF) to high frequency ratio (LF/HF ratio) in response to emotional stimuli were positively correlated with a reduction in depression symptoms during fluoxetine treatment [23]. Additionally, Shapiro et al. showed that MDD responders had significantly increased HF-HRV and decreased LF-HRV during yoga therapy, compared to non-responders [24], which shows that HRV is closely related with clinical efficacy of different intervention. HRV is closely related to dysregulation in certain neural circuits of mental illness, especially amygdala and the medial prefrontal cortex (mPFC). Based on the neural circuit mechanisms and imaging of cognitive-behavioral therapy (CBT), it has been revealed that CBT effectively modulates abnormal neural circuits in patients by specifically targeting and modulating the amygdala and anterior cingulate cortical (ACC) circuits [25].Therefore, we put forward a hypothesis that HRV, a potential biological indicator, could predict the effectiveness of GCBT.
In the randomized control study, we investigated the predictive utility of pre-treatment HRV in effectiveness of GCBT in reducing depression and anxiety symptom among college students. The study seeks to examine the relationship between HRV and improvement clinical symptoms. By comparing traditional survey measures with HRV data, our study determine the additional value of HRV recorded in the real-world using wearable devices in GCBT. This approach helps identify individuals more likely to benefit from GCBT, facilitating a more efficient utilization of medical resources. The findings have implications for improving treatment approaches for subthreshold mental health and advancing personalized interventions.
Method
Participants
This randomized controlled study was conducted at Xinxiang Medical University in China, focusing on the recruitment of college students. Utilizing the WeChat subscription platform, participants were engaged in completing mental health screening questionnaires and providing demographic information, including age, gender, lifestyle, and health characteristics [26]. Validated self-report questionnaires, such as the PHQ-9, GAD-7, and PSS-14, were employed to assess depression, anxiety, and stress. Different cutoff points and approaches were utilized in pre- and post-treatment assessments to define participants with depression and anxiety, and the changes in these results will be considered as the primary outcomes for evaluating the efficacy of GCBT. The inclusion criteria required participants to have PHQ-9 or GAD-7 scores above 5, be aged between 16 and 25 years old, agree to undergo four-week treatment, and have no medication or psychotherapy in the three months prior to enrollment. Exclusion criteria encompassed no history of DSM-IV diagnosis of schizophrenia or other mental disorders, no evidence of head injury or organic brain disease, no diagnosis of substance dependence, and no high suicide risk or heart disease. Written informed consent was obtained from all participants. A total of 58 participants completed all online questionnaires and wore activity trackers from 7:00 to 21:00 for a minimum of 28 days during the treatment period. Eligible and consenting participants were randomly assigned to either the GCBT group or wait-list control (WLC) group using a web-based randomization procedure performed by a blinded research assistant. At the end of the four weeks, 30 participants remained in the GCBT group and 28 in the WLC group. Measurement of heart rate variability and clinical symptoms were obtained at baseline and four weeks for both groups. After the quality control of HRV and considering the actual wearing situation of wearable devices, a total of 16 participants from the GCBT group and 17 participants from the WLC group were ultimately included in the study analysis.
This study was conducted in compliance with ethical standards and was approved by the Ethics Committee of Xinxiang Medical University (XYLL-2,020,235). All participants participated in this study voluntarily and signed the online informed consent before participation. All participants who completed the assessments were provided with their individual psychometric results.
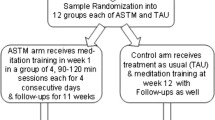
GCBT procedures
Treatment in the form of GCBT occurred over four sessions, each lasting 90 min, conducted across four consecutive weeks. The format included two face-to-face sessions and two online sessions. All GCBT modules were designed based on the cognitive behavioral model by Beck et al. [27], following the GCBT programmer (WY) registered psychologists with more than 3 years of experience, manualized intervention [28]. The intervention encompassed the following components: (a) Member introductions and understanding of depression, anxiety, and CBT. (b) Identification and exploration of distorted cognition and negative behaviors. (c) Acquisition of corrective skills to address distorted cognition. (d) Consolidation of cognitive changes and application of corrective skills. To support the research process, four local University College Student Volunteers (UCSVs) were recruited as research assistants and underwent a 1-day training session on data collection and participant management during the GCBT intervention period. After randomization, the GCBT group, were assigned to groups of six to ten participants, began the intervention immediately. The WLC group underwent a four-week waiting period and proceeded with treatment after the waiting period based on individual preference. Meanwhile, the WLC group had no scheduled contact with the project team, they can get help and support as needed. Throughout the entire intervention or waiting period, a psychological service hotline had been provided to prevent the occurrence of severe adverse events. Table 1 describes an overview of the treatment content.
Data collection
During the four-week study period from 07:00 am to 21:00 pm participants were informed about and instructed to wear wearable wristbands. The collected data was stored on the device and uploaded to research servers every night, with text reminders sent to those who failed to upload on time. We utilized Huawei Band 6 devices with photoplethysmography (PPG) sensors (100 Hz) to record the physiological signals and calculate the continuous inter-beat interval and heart rates. Huawei smart wearable devices had previously been employed in previous clinical studies for cardiovascular disease [29,30,31]. We then used inter-beat interval records to calculate Heart rate variability (HRV) parameters, such as Standard Deviation of Normal-to-Normal Intervals (SDNN), Root Mean Square of Successive Differences (RMSSD) and so on. The devices also featured a 3-axis accelerometer to measure acceleration, which was used to calculate activity level as an indicator of overall movement, with daily step count serving as a proxy for physical activity.
Data quality control
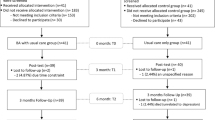
To standardize the study, it is recommended to perform short-term measurement analysis of heart rate variability (HRV) using a continuous 5-minute sequence of R-R intervals (RRI, represent R-wave peak to R-wave peak intervals in electrocardiogram (ECG) records) to assess the temporal changes between successive heartbeats [32]. Previous studies indicate that physiological information obtained from the R-R intervals in electrocardiogram can similarly be derived from the pulse period of photoplethysmography (PPG), with a confirmed strong correlation between PPG-derived peak-to-peak intervals and ECG-derived R-R intervals [33, 34]. In this study, PPG-derived peak-to-peak intervals were used to represent R-R intervals. All returned data were analyzed, and the number of valid 5-minute samples per hour for each record was calculated separately, as shown in Fig. 1. Taking into account HRV was influenced by circadian rhythms, we made the final decision to focus on HRV measurements for all participants taken between 01:00 pm and 02:00 pm [35]. This time slot was chosen due to its highest data integrity, ensuring minimal disturbance and thus providing the most accurate and reliable data. In accordance with the accepted guidelines, we only included series with a minimum of 85.0% sinus beats in order to ensure data quality and reliability for our study [36,37,38]. In the heart rate variability records collected by our participants, only 16 participants from the GCBT group and 17 participants from the WLC group met the criteria and were retained for subsequent analysis.
Data preprocessing
Prior to analysis, we utilized the HRV analysis toolkit (https://aurahealthcare.github.io/hrvanalysis/) to process R-R intervals, which underwent meticulous manual correction for ectopic beats and missing heartbeats [39]. In accordance with our criteria, whenever ectopic beat or missing heartbeats were detected, they were surgically removed and replaced with the mean of the two adjoining R-R intervals [21, 37]. HRV indices were computed in accordance with the recommendations outlined by the Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology in 1996 [40]. These calculations encompassed time domain features, frequency domain features, and non-linear domain features of HRV for individuals.Time domain features included Mean HR, Min HR, Max HR, Median NN, SDNN, SDSD, NN20, NN50, PNN50, PNN20, RMSSD. Frequency domain features encompassed LF, HF, and the LH/HF ratio. Additionally, the non-linear domain feature known as the Triangular index was calculated. We calculated valid samples within this time period for one week and took their average as the heart rate variability (HRV) for the recent week. The data from the first week is considered as the baseline HRV. Similarly, HRV for the fourth week is calculated in the same manner (See Abbreviation Supplemental Table 1).
Statistical analysis
In this study, we analyzed their data using IBM SPSS Statistics 25.0 software. To compare differences between groups at baseline, we employed various statistical tests, including Chi-square or Fisher’s tests for qualitative variables and Student’s t-test or Mann-Whitney test for quantitative variables. With “time” as the within-group factor and “group” as the between-group factor, we used repeated-measures analyses of variance (RMANOVA) to assess the effects of the intervention on outcome measures over time. The association between HRV, constructed a multiple linear Symptom and GCBT was analyzed in two stages. First, we employed Spearman rank correlations to explore the associations between clinical and functional indicators and HRV, with a significance threshold set at p < 0.05 to help explicate our results. Additionally, we performed regression model using relevant variables to investigate whether the baseline level of HRV can predict changes in depression and anxiety.
Results
Demographic characteristics of participants
After physiological signal data preprocessing and quality control, the analysis included 16 participants from the GCBT group and 17 participants from the WLC group. Please see Fig. 2 for details regarding participant flow and drop-out. There were no significant differences (P > 0.05) between groups in terms of sociodemographic in Table 2. In the other hand, there were no significant differences (P > 0.05) between groups in terms of heart rate variability in Table 3.
GCBT intervention effect of clinical symptoms
Kolmogorov-Smirnov tests showed that HRV and scale scores were normally distributed. For these variables, we used two-tailed T-tests for analysis and found no group differences in HRV and symptom severity (PHQ, GAD, PSS) before intervention between the GCBT and WLC groups (P > 0.05). RMANOVA with intervention (GCBT or WLC group) as a within-subject factor was used to compare the treatment and wait-list control groups. Depression scores: The main effect of GCBT intervention was not significant, F = 0.335, P = 0.57, partial η2 = 0.11; the main effect of time was not significant, F = 3.51, P = 0.07, partial η2 = 0.11; the interaction effect of GCBT intervention and time was significant, F = 5.87, P = 0.02, partial η2 = 0.16. Anxiety scores: The main effect of GCBT intervention was not significant, F = 0.78, P = 0.38, partial η2 = 0.06; the main effect of time was not significant, F = 4.119, P = 0.05, partial η2 = 0.12; the interaction effect of GCBT intervention and time was significant, F = 4.69, P = 0.04, partial η2 = 0.135. Stress scores: The main effect of GCBT intervention was not significant, F = 0.009, P = 0.924, partial η2 = 0.001; the main effect of time was not significant, F = 0.396, P = 0.534, partial η2 = 0.013; the interaction effect of GCBT intervention and time was significant, F = 6.034, P = 0.020, partial η2 = 0.163 (Table 4).
Associations between clinical symptoms and heart rate variability
The correlation analysis revealed significant negative associations between HRV, heart rate (HR), and the scale scores of the PSS and PHQ. Specifically, the mean HR exhibited a negative correlation with both PHQ scores (rho=−0.313, P = 0.01) and PSS scores (rho=−0.313, P = 0.01). Similarly, the minimum HR showed negative correlations with PHQ scores (rho=−0.228, P = 0.048) and PSS scores (rho=−0.253, P = 0.03). Additionally, HFnu (high frequency normalized units) exhibited negative correlations with both PHQ scores (rho=−0.49, P < 0.001) and PSS scores (rho=−0.283, P = 0.02), while the correlation between LFnu and PHQ and PSS scores was found to be exactly opposite to that of HFnu. Lastly, the LF/HF ratio (representing the low frequency and high frequency ratio) demonstrated positive correlations with PHQ scores (rho = 0.49, P < 0.001) and PSS scores (rho = 0.30, P = 0.01). No statistically significant correlation was found between HRV, HR, and GAD scores (Table 5).
Associations between treatment effect and baseline heart rate variability
From pre- to post-treatment, participants’ improvement in depressive symptoms was positively correlated with baseline HRV: NN20 (rho = 0.55, P = 0.03), Median NN (rho = 0.499, P = 0.049), PNN20 (rho = 0.547, P = 0.03), while Mean HR (rho=−0.507, P = 0.045), Min HR (rho=−0.551, P = 0.03) the negative correlation with declination of depression scores. The absolute difference in anxiety scores was also significant correlated with baseline HRV: SDNN (rho = 0.548, P = 0.03), SDSD (rho = 0.532, P = 0.03), NN50 (rho = 0.593, P = 0.02), PNN50 (rho = 0.612, P = 0.01), PNN20 (rho = 0.618, P = 0.01), RMMSD (rho = 0.532, P = 0.03), Min HR (rho=−0.734, P = 0.001), Triangular index (rho = 0.682, P = 0.004). A multiple linear regression model was used to explore the relationship between HRV and the anti-depressive and anti-anxiety efficacy of GCBT treatment. We screened for HRV features related to GCBT efficacy and constructed a multiple linear regression model using backward selection to ultimately establish a final model containing independent variables of HRV features, gender, age and BMI, and activity level (showed in Supplementary Table 2). The results showed that HRV was a significant predictor of GCBT anti-depressive and anti-anxiety efficacy after controlling for the effects of other independent variables. We found the multiple HRV features significantly predicted depressive symptoms changes (F = 7.308, P = 0.02, R2 = 0.936) (Fig. 3). We found that predicted changes in anxious symptoms were also significant (F = 13.849, P = 0.002, R2 = 0.954) (Fig. 4). Detailed information about HRV parameter in the models can be found in Supplementary Table 3.
Discussion
In this preliminary study, we assess the efficacy of GCBT as a treatment for depression and anxiety. Our analysis revealed significant and clinically meaningful reductions in depression symptoms (PHQ scores) and anxiety symptoms (GAD scores) relative to baseline, post-intervention at 4 weeks. Additionally, we assessed the association between autonomic abnormalities and symptoms of depression, anxiety, and pressure level. Our findings suggest that the reduction in depression and anxiety scores positively correlated with baseline HRV levels. To our knowledge, this is the first study to describe the efficacy of depression and anxiety treatment using passively collected data from wearable devices, providing a basis for future research on potential predictors of anti-depression and anti-anxiety treatment response.
Although a study by Balogh et al. (1993) had previously found no correlation between pre-treatment resting-state HRV and improvement in depressive symptoms [41], we speculate that this conclusion may have stemmed from inadequate sample size and dependence on laboratory data. To mitigate these limitations, participants in our study were required to wear wristbands for four weeks to collect personalized data. By collecting data passively from wearable devices over the course of a week, we avoided the systematic errors and laboratory effects present in previous studies that recruited patients and collected 5-minute HRV in the laboratory. This approach is more stable and reflects a resting HRV index that is closer to real-world conditions. In contrast, most previous studies used electrocardiograms to measure HRV. ECG electrodes are typically attached to the body with adhesive, which can cause skin damage related to medical adhesive, especially if worn for extended periods [42].
In our study, participants with lower HRV reported higher depression scores. Most diagnosed mental illnesses often exhibit lower HRV [43]. Although participants in our experiment were in state of subthreshold mental health with depression and anxiety, their HRV followed this pattern, indicating that even in the early stages of MDD or ANX, HRV has already begun to affect their onset and development. Abnormal functioning of the autonomic nervous system may develop into psychopathology. HRV can serve as a biological marker for predicting depression states.
Our study revealed a consistent positive correlation between HRV indices and self-reported depression and stress scores in patients. HRV serves as an indicator of an individual’s ability to adapt physiologically to changing internal and environmental demands, reflecting their overall quality factor [44]. Lower HRV is associated with increased vulnerability to stress and reduced coping abilities. It also indicates heightened control by the sympathetic nervous system, which can lead to difficulties in emotional regulation and increased impulsivity.
Additionally, higher resting HRV has been linked to various psychological processes, including more flexible and adaptive emotion regulation and recovery in response to threat [45,46,47]. Notably, pre-treatment HRV predicted outcomes of GCBT, with higher HRV predicting better treatment outcomes and lower HRV predicting poorer outcomes. Given the current results that individuals with higher HRV indexes a more flexible or responsive physiological system that may benefit more strongly from GCBT treatment. Interestingly, we found that HRV time-domain and non-linear indicators are more robust and closely related to treatment effects, while frequency-domain indicators and HR appear to reflect the participant’s state at the time of measurement, including their mood or stress levels.
After four weeks of cognitive-behavioral therapy, depressive and anxious score improved in GCBT group, as did the HF/LF ratio, we believe that cognitive-behavioral therapy may partially achieve its efficacy through improving HRV. This is based on the fact that the neural mechanism of CBT treatment mainly targets abnormal neural circuits in depression by regulating core targets such as the amygdala and anterior cingulate cortex [48]. The therapeutic effect of CBT is related to task-related activation, especially activation of the amygdala and subgenual ACC (sgACC), while sgACC is closely related to depression and autonomic nervous system activity. Increased connectivity patterns between affective (sgACC and amygdala) and cognitive control (dorsolateral prefrontal cortex and Temporal parietal junction) networks before and after CBT are associated with successful CBT treatment [49]. Connectivity in these regions can predict CBT treatment response in depressed adolescents. This indicates that successful treatment may be related to the reconfiguration of previously disordered connectivity patterns and provides neuroimaging evidence that HRV can be used as a biological marker to predict the efficacy of GCBT.
This study has several limitations that should be considered when interpreting the results. One limitation of this study is the small sample size. Although we have addressed this to some extent by collecting passive data over an extended period, there remains a possibility of chance occurrences. This could potentially impact the reliability and generalizability of the study findings. In future research, we aim to increase the sample size to further validate our findings. Additionally, a subset of participants was excluded from the data analysis, prompting us to delve into the intricacies of this phenomenon. Possible explanations include: WLC participants with higher depression and anxiety scores may have dropped out during the waiting period due to non-compliance with wristband requirements. Participants in the GCBT group, who had relatively milder clinical symptoms, may have exhibited poorer compliance with wearable devices and treatment. Finally, we controlled for activity level confounding factors in subsequent analyses even though we cannot guarantee that participants were in an absolute resting state. We believe that our definition of resting state may represent most states in daily life for college students. Meanwhile, the potential bias conducted by non-continuous data is mitigated due to our coverage requirement.
Conclusion
This exploratory pilot data tentatively supports the hypothesis that treatment outcomes of GCBT for depressive and anxious symptoms are associated with autonomic nervous system function. Smart wearable devices have emerged as low-cost, non-invasive, and convenient tools for monitoring and predicting mental health. Based on data collected from smart devices, HRV can be an easily measurable and objective predictor of treatment response to GCBT for individuals with anxiety and depression. It is therefore worth considering in the context of the high cost of treatment and the longer time it takes to transmit more sophisticated brain-based and other biological assessments. Future research could consider increasing sample size or exploring different treatment methods, such as Transcranial Direct Current Stimulation (tDCS) or repetitive Transcranial Magnetic Stimulation (rTMS), to assess whether low HRV can serve as an indicator of patient heterogeneity, thereby promoting personalized intervention treatments.
Data availability
The authors do not have the right to share any data information as per the ethics committee rules and regulations but are available upon a reasonable request from the corresponding author (FW).
References
Kessler RC, Merikangas KR, Wang PS. Prevalence, comorbidity, and service utilization for mood disorders in the United States at the beginning of the twenty-first century. Annu Rev Clin Psychol. 2007;3:137–58.
Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern med. 2007;146(5):317–25.
Judd LL, Paulus MP, Wells KB, Rapaport MH. Socioeconomic burden of subsyndromal depressive symptoms and major depression in a sample of the general population. Am J Psychiatry. 1996;153(11):1411–7.
Preisig M, Merikangas K, Angst J. Clinical significance and comorbidity of subthreshold depression and anxiety in the community. Acta Psychiatr Scand. 2001;104(2):96–103.
Jiang L, Wang Y, Zhang Y, Li R, Wu H, Li C, Wu Y, Tao Q. The reliability and validity of the center for epidemiologic studies depression scale (CES-D) for Chinese university students. Front Psychiatry. 2019;10:315.
Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu S-M, Olfson M. Mental health of college students and their non–college-attending peers: results from the national epidemiologic study on alcohol and related conditions. Arch Genl Psychiatry. 2008;65(12):1429–37.
Eisenberg D, Hunt J, Speer N. Mental health in American colleges and universities: variation across student subgroups and across campuses. J Nerv Ment. 2013;201(1):60–7.
Byrd DR, McKinney KJ. Individual, interpersonal, and institutional level factors associated with the mental health of college students. J Am Coll Health. 2012;60(3):185–93.
Ketchen Lipson S, Gaddis SM, Heinze J, Beck K, Eisenberg D. Variations in student mental health and treatment utilization across US colleges and universities. J Am Coll Health. 2015;63(6):388–96.
Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Üstün TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. 2007;20(4):359–64.
Johnson J, Weissman MM, Klerman GL. Service utilization and social morbidity associated with depressive symptoms in the community. JAMA. 1992;267(11):1478–83.
Cuijpers P, Smit F. Subthreshold depression as a risk indicator for major depressive disorder: a systematic review of prospective studies. Acta Psychiatr Scand. 2004;109(5):325–31.
Batelaan NM, de Graaf R, Spijker J, Smit JH, van Balkom AJ, Vollebergh WA, Beekman AT. The course of panic attacks in individuals with panic disorder and subthreshold panic disorder: a population-based study. J Affect Disord. 2010;121(1–2):30–8.
Balázs J, Miklósi M, Keresztény Á, Hoven CW, Carli V, Wasserman C, Apter A, Bobes J, Brunner R, Cosman D. Adolescent subthreshold-depression and anxiety: psychopathology, functional impairment and increased suicide risk. J Child Psychol Psychiatry. 2013;54(6):670–7.
Dvorak RD, Lamis DA, Malone PS. Alcohol use, depressive symptoms, and impulsivity as risk factors for suicide proneness among college students. J Affect Disord. 2013;149(1–3):326–34.
Mikolajczyk RT, Maxwell AE, El Ansari W, Naydenova V, Stock C, Ilieva S, Dudziak U, Nagyova I. Prevalence of depressive symptoms in university students from Germany, Denmark, Poland and Bulgaria. Soc Psychiatry Psychiatr Epidemiol. 2008;43:105–12.
Jain FA, Cook IA, Leuchter AF, Hunter AM, Davydov DM, Ottaviani C, Tartter M, Crump C, Shapiro D. Heart rate variability and treatment outcome in major depression: a pilot study. Int J Psychophysiol. 2014;93(2):204–10.
Nakao M, Shirotsuki K, Sugaya N. Cognitive–behavioral therapy for management of mental health and stress-related disorders: recent advances in techniques and technologies. BiopsychoSoc Med. 2021;15(1):1–4.
Bantjes J, Kazdin AE, Cuijpers P, Breet E, Dunn-Coetzee M, Davids C, Stein DJ, Kessler RC. A web-based group cognitive behavioral therapy intervention for symptoms of anxiety and depression among university students: open-label, pragmatic trial. JMIR Ment Health. 2021;8(5):e27400.
Ginsburg GS, Becker-Haimes EM, Keeton C, Kendall PC, Iyengar S, Sakolsky D, Albano AM, Peris T, Compton SN, Piacentini J. Results from the child/adolescent anxiety multimodal extended long-term study (CAMELS): primary anxiety outcomes. J Am Acad Child Adolesc Psychiatry. 2018;57(7):471–80.
Camm AJ, Malik M, Bigger JT, Breithardt G, Cerutti S, Cohen RJ, Coumel P, Fallen EL, Kennedy HL, Kleiger RE, Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation. 1996;93(5):1043–65.
Kircanski K, Williams LM, Gotlib IH. Heart rate variability as a biomarker of anxious depression response to antidepressant medication. Depress Anxiety. 2019;36(1):63–71.
Fraguas R Jr, Marci C, Fava M, Iosifescu DV, Bankier B, Loh R, Dougherty DD. Autonomic reactivity to induced emotion as potential predictor of response to antidepressant treatment. Psychiatry Res. 2007;151(1–2):169–72.
Shapiro D, Cook IA, Davydov DM, Ottaviani C, Leuchter AF, Abrams M. Yoga as a complementary treatment of depression: effects of traits and moods on treatment outcome. Evid-Based Complement Altern Med. 2007;4(4):493–502.
Chattopadhyay S, Tait R, Simas T, van Nieuwenhuizen A, Hagan CC, Holt RJ, Graham J, Sahakian BJ, Wilkinson PO, Goodyer IM. Cognitive behavioral therapy lowers elevated functional connectivity in depressed adolescents. EBioMedicine 2017, 17:216–22.
Karyotaki E, Riper H, Twisk J, Hoogendoorn A, Kleiboer A, Mira A, Mackinnon A, Meyer B, Botella C, Littlewood E. Efficacy of self-guided internet-based cognitive behavioral therapy in the treatment of depressive symptoms: a meta-analysis of individual participant data. JAMA Psychiatry. 2017;74(4):351–9.
Beck AT. Cognitive therapy of depression. Guilford Press; 1979.
Straub J, Koelch M, Fegert J, Plener P, Gonzalez-Aracil I, Voit A, Sproeber N. Innovations in practice: MICHI, a brief cognitive‐behavioural group therapy for adolescents with depression–a pilot study of feasibility in an inpatient setting. Child Adolesc Ment Health. 2013;18(4):247–50.
Harrison SL, Buckley BJ, Zheng Y, Hill A, Hlaing T, Davies R, Guo Y, Lane DA, Lip GY, Choi S. Evaluation of Huawei smart wearables for detection of atrial fibrillation in patients following ischemic stroke: the Liverpool-Huawei stroke study. Am Heart J. 2023;257:103–10.
Guo Y, Wang H, Zhang H, Liu T, Liang Z, Xia Y, Yan L, Xing Y, Shi H, Li S. Mobile photoplethysmographic technology to detect atrial fibrillation. J Am Coll Cardiol. 2019;74(19):2365–75.
Guo Y, Lane DA, Wang L, Zhang H, Wang H, Zhang W, Wen J, Xing Y, Wu F, Xia Y. Mobile health technology to improve care for patients with atrial fibrillation. J Am Coll Cardiol. 2020;75(13):1523–34.
Natarajan A, Pantelopoulos A, Emir-Farinas H, Natarajan P. Heart rate variability with photoplethysmography in 8 million individuals: a cross-sectional study. Lancet Digit Health. 2020;2(12):e650–7.
Selvaraj N, Jaryal A, Santhosh J, Deepak KK, Anand S. Assessment of heart rate variability derived from finger-tip photoplethysmography as compared to electrocardiography. J Med Eng Technol. 2008;32(6):479–84.
Vandenberk T, Stans J, Mortelmans C, Van Haelst R, Van Schelvergem G, Pelckmans C, Smeets CJ, Lanssens D, De Cannière H, Storms V. Clinical validation of heart rate apps: mixed-methods evaluation study. JMIR mHealth uHealth. 2017;5(8):e7254.
Vandewalle G, Middleton B, Rajaratnam SM, Stone BM, Thorleifsdottir B, Arendt J, DIJK DJ. Robust circadian rhythm in heart rate and its variability: influence of exogenous melatonin and photoperiod. J Sleep Res. 2007;16(2):148–55.
Huikuri HV, Seppänen T, Koistinen MJ, Airaksinen KJ, Ikaheimo M, Castellanos A, Myerburg RJ. Abnormalities in beat-to-beat dynamics of heart rate before the spontaneous onset of life-threatening ventricular tachyarrhythmias in patients with prior myocardial infarction. Circulation. 1996;93(10):1836–44.
Nunan D, Donovan G, Jakovljevic DG, Hodges LD, Sandercock GR, Brodie DA. Validity and reliability of short-term heart-rate variability from the Polar S810. Med Sci Sports Exerc. 2009;41(1):243–50.
Jurca R, Church TS, Morss GM, Jordan AN, Earnest CP. Eight weeks of moderate-intensity exercise training increases heart rate variability in sedentary postmenopausal women. Am Heart J 2004, 147(5):e8–e15.
Pichot V, Roche F, Celle S, Barthelemy J-C, Chouchou F. HRVanalysis: a free software for analyzing cardiac autonomic activity. Front Physiol. 2016;7:557.
Malik M. Heart rate variability: standards of measurement, physiological interpretation, and clinical use: Task force of the European Society of Cardiology and the North American Society for Pacing and Electrophysiology. Ann Noninvasive Electrocardiol. 1996;1(2):151–81.
Balogh S, Fitzpatrick DF, Hendricks SE, Paige SR. Increases in heart rate variability with successful treatment in patients with major depressive disorder. Psychopharmacol Bull; 1993.
Farris MK, Petty M, Hamilton J, Walters S-A, Flynn MA. Medical adhesive-related skin injury prevalence among adult acute care patients: a single-center observational study. J Wound Ostomy Cont Nurs. 2015;42(6):589–98.
Heiss S, Vaschillo B, Vaschillo EG, Timko CA, Hormes JM. Heart rate variability as a biobehavioral marker of diverse psychopathologies: a review and argument for an ideal range. Neurosci Biobehav Rev. 2021;121:144–55.
Appelhans BM, Luecken LJ. Heart rate variability as an index of regulated emotional responding. Rev Gen Psychol. 2006;10(3):229–40.
Friedman BH. An autonomic flexibility–neurovisceral integration model of anxiety and cardiac vagal tone. Biol Psychol. 2007;74(2):185–99.
Thayer JF, Åhs F, Fredrikson M, Sollers JJ III, Wager TD. A meta-analysis of heart rate variability and neuroimaging studies: implications for heart rate variability as a marker of stress and health. Neurosci Biobehav Rev. 2012;36(2):747–56.
Thayer JF, Lane RD. Claude Bernard and the heart–brain connection: further elaboration of a model of neurovisceral integration. Neurosci Biobehav Rev. 2009;33(2):81–8.
Fu CH, Williams SC, Cleare AJ, Scott J, Mitterschiffthaler MT, Walsh ND, Donaldson C, Suckling J, Andrew C, Steiner H. Neural responses to sad facial expressions in major depression following cognitive behavioral therapy. Biol Psychiatry. 2008;64(6):505–12.
Straub J, Metzger CD, Plener PL, Koelch MG, Groen G, Abler B. Successful group psychotherapy of depression in adolescents alters fronto-limbic resting-state connectivity. J Affect Disord. 2017;209:135–9.
Acknowledgements
The authors thank all the participants for their cooperation, and we are grateful for the support of Xinxiang Medical College of Henan Province.
Funding
This study was funded by National Science Fund for Distinguished Young Scholars (81725005 to Fei Wang), NSFC-Guangdong Joint Fund (U20A6005 to Fei Wang), Jiangsu Provincial Key Research and Development Program (BE2021617 to Fei Wang), National Natural Science Foundation of China (62176129 to Xizhe Zhang), Key Project supported by Medical Science and Technology Development Foundation, Jiangsu Commission of Health (ZD2021026 to Rongxin Zhu), National Natural Science Foundation of China (82151315 to Rongxin Zhu), Jiangsu Provincial Key Research and Development Program(BE2022160 to Rongxin Zhu), Henan Province Higher Education Teaching Reform Research and Practice Project (2021SJGLX189 to Rongxun Liu).
Author information
Authors and Affiliations
Contributions
ZL,JZ and YW designed the study. YW, ZL, JZ,RZ and ZS managed the literature searches and analyses. YW, RL, RZ and YW participated in the collection of data. ZL, YW, and JZ undertook the statistical analysis. ZL,YW and JZ wrote the first draft of the manuscript. YW, ZL, FW, XZ and JZ participated in the revision of the manuscript. All authors contributed to and have approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study has been approved by the Ethics Committee of Xinxiang Medical College of Henan Province (approval number: XYLL-2020235). An electronic informed consent form was provided before the start of the questionnaire, and after completing the informed consent form, participants completed the online questionnaire. We confirmed that informed consent was obtained from all participants. Moreover, all methods in this study were performed by the relevant guidelines and regulations.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lin, Z., Zheng, J., Wang, Y. et al. Prediction of the efficacy of group cognitive behavioral therapy using heart rate variability based smart wearable devices: a randomized controlled study. BMC Psychiatry 24, 187 (2024). https://doi.org/10.1186/s12888-024-05638-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-05638-x