Abstract
Background
To investigate the incidence of depression in middle-aged and elderly patients with diabetes in China and the influencing factors to provide a theoretical basis to improve the mental health of middle-aged and elderly patients with diabetes and formulate prevention, control, and intervention strategies.
Methods
The sample of this study was obtained from the China Health and Aging Tracking Survey (CHARLS) 2018 survey data, and middle-aged and older patients with diabetes(responding “Yes” to the questionnaire: “Have you ever been told by a doctor that you have diabetes or elevated blood glucose [including abnormal glucose tolerance and elevated fasting glucose]?”) aged ≥ 45 years were selected as study subjects (n = 2,613 ). Depressive symptoms of the study subjects were determined using the simplified version of the Depression Scale for Epidemiological Surveys scores(a score ≥ 10 was defined as depression), influence factors were analyzed using binary logistic regression, and proportion of depressive symptoms was standardized using the sex ratio of the seventh census.
Results
Among the 2,613 middle-aged and elderly patients with diabetes, 1782 (68.2%) had depressive symptoms and 831 (31.8%) had no depressive symptoms. There were 481 (27.0%) patients aged 45−59 years, 978 (54.9%) aged 60−74 years, and 323 (18.1%) aged ≥ 75 years. The depression rate among middle-aged and elderly Chinese patients with diabetes after standardization correction was 67.5%. Binary logistic regression results showed that age, education level, life satisfaction, marital satisfaction, self-rated health grade, somatic pain, visual impairment, physical disability, and the presence of comorbid chronic diseases were factors that influenced the onset of depression in middle-aged and elderly Chinese patients with diabetes (P < 0.05).
Conclusion
According to a survey analysis of the CHARLS 2018 data, depression is influenced by a combination of factors among middle-aged and elderly patients with diabetes in China. Therefore, for this population, targeted prevention and control should be carried out for key populations, such as middle-aged and elderly people, poor physical health, and low life satisfaction and marital satisfaction, from various dimensions (e.g., demographic and sociological factors, physical health status, and life satisfaction and marital satisfaction).
Similar content being viewed by others
Background
The prevalence of depression is increasing worldwide, and the increasing aging of the population in China has made depression a major health problem in the elderly. Depression, as one of the most common mental health problems in middle-aged and elderly people, not only has a serious impact on their mental health and quality of life, but is a great burden on families and society [1, 2]. Clinical studies have shown that depression and diabetes often coexist and that people with diabetes are twice as likely to experience depression, increasing the probability of developing diabetes [3].
The latest data released by the International Diabetes Federation in 2019 showed that there are 463 million diabetics worldwide, mainly middle-aged and elderly, and this figure will continue to grow in the future [4]. The psychological comorbidity rate of diabetics is very high due to a number of factors, such as the disease itself and the patients themselves [5]. Depression can significantly reduce the ability of patients with diabetes to self-manage, severely hinder compliance with treatment, making it difficult for caregivers to communicate effectively with patients, and even disrupt the therapeutic relationship; therefore, worsening the condition of diabetics. Some studies have shown that approximately 30% of patients with diabetes have depressive symptoms [6]. Depressed mood has a significant impact on blood glucose levels, the incidence of diabetic complications, cardiovascular events, and even morbidity and mortality in patients with diabetes [7].
Therefore, it is of great practical importance to understand the mental health status of middle-aged and elderly patients with diabetes and to explore as many influencing factors as possible. In this study, we used data from the China Health and Retirement Longitudinal Study (CHARLS) 2018 to analyze the incidence of depression and its influencing factors among middle-aged and elderly patients with diabetes in China, with the aim of providing a reference base to improve the mental health status of middle-aged and elderly patients with diabetes and formulate prevention, control, and intervention strategies. The questionnaire design of this survey refers to international experiences, including the Health and Retirement Survey in the United States and the English Longitudinal Study of Aging. These data are widely recognized and used in academia, allowing for an international comparison of the CHARLS findings with those of other studies. Compared to previous studies, this study has the advantages of broad coverage of the study, large sample size, and representativeness.
Methods
Objectives of the study
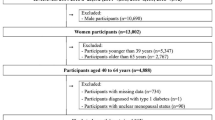
The sample for this study was obtained from the latest publicly released CHARLS 2018 survey data in September 2020, which covered 28 provinces, 150 districts and counties, and 19,816 respondents in China, with a more authoritative sample representation. The survey’s sampling method uses a multi-stage probability sampling method. The inclusion criteria were the following: (1) age ≥ 45 years; (2) responding “Yes” to the questionnaire “DA007: Have you ever been told by a doctor that you have diabetes or elevated blood glucose (including abnormal glucose tolerance and elevated fasting glucose)?”; (3) provide a clear answer to the Depression Scale (Center for Epidemiologic Studies Depression, CES-D). The exclusion criteria were as follows: (1) lack of information on diabetes; (2) lack of information on depression; and (3) lack of information on relevant covariates. A total sample of 2,613 middle-aged and elderly patients with diabetes were included in the study. This study was approved by the Biomedical Ethics Committee of Peking University (IRB00001052-11015), and informed consent was obtained from all respondents. Basic information on the study participants is presented in Table 1.
Investigation content relevant to this study
Information collected from all study participants includes general information (i.e., age, sex, residence, education, religion, marital status, and social interaction), physical health status (i.e., smoking, alcohol consumption, napping, self-rated health[Would you say your health is good,general or not good?], somatic pain, hearing impairment, speech impairment[Be mute or stutter], visual impairment, disability[physical disabilities or intellectual deficiency], instrumental activities of daily living [IADL], number of comorbid chronic diseases [hypertension, dyslipidemia, malignant tumor, chronic lung disease, heart disease, stroke, arthritis,rheumatism]), marital satisfaction, and life satisfaction.
Assessment of depressive symptoms
The CHARLS uses a simplified version of the CES-D [8], developed by RADLOFF, which has high reliability and validity in previous studies [9] and can be widely used in middle-aged and older populations. CES-D has 10 items with four scales: “3 = always,” “2 = often,” “1 = sometimes or rarely,” and “0 = never,” where the fifth and eighth items are reverse scored. The scale is rated on a scale of 0−30; the higher the score, the more severe the depression. Based on previous studies of middle-aged and elderly populations, the present study used a critical value of 10 as a classification for the presence or absence of depression, i.e., a score ≥ 10 was defined as depression [8].
Statistical methods
SPSS software (version 26.0) was used to perform the statistical analysis of the data. The count data were expressed as relative numbers and the χ2 test was used to compare between groups. Measurement data with normal distribution were expressed as ± standard deviation and those with non-normal distribution were expressed as M (P25, P75). The analysis of factors influencing depressive symptoms in middle-aged and elderly patients with diabetes was analyzed with binary logistic regression analysis, and the difference was considered statistically significant at P < 0.05. The proportion of depressive symptoms was standardized using census sex ratios.zi.The assignment of independent variables is detailed in Table 2.
Results
A univariate analysis of the occurrence of depressive symptoms in middle-aged and elderly patients with diabetes mellitus.
Among the 2,613 middle-aged and elderly patients, 1782 (68.2%) had depressive symptoms, 831 (31.8%) had no depressive symptoms.In people with depression, 640 (35.9%) were males and 1142 (64.1%) were females, 481 (27.0%) were aged 45−59 years old, 978 (54.9%) aged 60−74 years, and 323 (18.1%) aged ≥ 75 years.
There were statistically significant differences (P < 0.05) in age, sex, residence, education, smoking, alcohol consumption, napping, life satisfaction, marital satisfaction, self-rated general health, somatic pain, speech impairment, visual impairment, physical disability, and comorbid chronic diseases between middle-aged and elderly patients with diabetes with and without depressive symptoms (Table 3).
Binary logistic regression analysis of the occurrence of depressive symptoms in middle-aged and elderly patients with diabetes mellitus.
The results of the binary logistic regression analysis showed that age, education level, life satisfaction, marital satisfaction, self-rated health, somatic pain, visual impairment, physical disability, and comorbid chronic diseases were influencing factors (P < 0.05) among middle-aged and elderly patients with diabetes (Table 4).
Standardized correction of the depression rate in middle-aged and elderly diabetic patients
This study normalized the proportion of depressive symptoms using the census sex ratio (female: male = 1:0.95). The adjusted depression rate was 31.0% for males and 36.5% for females, for a total of 67.5% (Table 5).
Discussion
The results of this study showed that the detection rate of depressive symptoms among middle-aged and elderly patients with diabetes was 67.5%, indicating the severity of mental health problems in this population. In this study, age was an influential factor in the development of depression in middle-aged and elderly patients with diabetes. The results also showed that the prevalence of depression was lower in the age group 60−74 years and ≥ 75 years than in the age group 45−59 years; the younger the age, the higher the prevalence of depression. The results of this study are consistent with the findings of Majumdar et al. [10], which can be explained by the fact that the age group 45−59 years has higher expectations of life and faces great stress in both life and work. A study in South Asia has confirmed that family status, financial problems, physical illness, and sudden accidents contribute to the increased risk of depression in the age group 45−59 years [11]. Meanwhile, participants aged 45−59 years are in the middle stage of Chinese society and have to face the double responsibility of taking care of their children and parents, which is stressful; therefore, the prevalence of depression is higher in this age group. The present study showed that education level of middle school or lower was a risk factor for depression compared to illiterate middle-aged and elderly patients with diabetes. However, some studies [12, 13] found that low education level was a risk factor for the occurrence of depression in patients with diabetes, which is not consistent with the results of the present study, and specific reasons need to be studied further.
Self-rated health (SRH) is an individual’s perception of their health and has been widely recommended by the World Health Organization for personal investigation of their level of health [14]. SRH has also been suggested to be a predictor of the occurrence of diseases such as cardiovascular events [15, 16] and mental disorders [17]. In this study, SRH was an influential factor in the occurrence of depression in middle-aged and elderly diabetic patients. Ghislaine et al. [18] found that self-assessed health status was a significant predictor of the onset of major depression in patients with type II diabetes through a follow-up survey in 2013. Furthermore, Huang et al. [17] found that older adults with poorer SRH status had a higher risk of depression, both of which are consistent with the results of this study. Therefore, healthcare workers, as well as community workers, should pay attention to the assessment of health status in middle-aged and elderly patients with diabetes. In addition, this study showed that the combination of multiple chronic diseases was an influential factor in the development of depression in middle-aged and elderly diabetic patients. A meta-analysis study by Huang et al. [19] found that heart disease, stroke, obstructive pulmonary disease, and diabetes were risk factors for depression in the elderly. A survey by Patten et al. [20] showed that the incidence of depression in the elderly was significantly associated with chronic diseases characterized by inflammation and pain. Diabetes itself is a type of chronic disease that already interferes with the daily life of patients, and this effect is undoubtedly more severe when middle-aged and elderly people suffer from other chronic diseases, increasing the risk of depression in middle-aged and elderly patients with diabetes. In addition, using CHARLS2011 baseline data and 2013 follow-up data, some studies found that depression was more prevalent among elderly patients with chronic diseases and that the number of chronic disease comorbidities was positively associated with the risk of depression [21], which confirms the results of this study.
Diabetes is accompanied by various complications, such as neuropathy, diabetic foot, and retinopathy [22], which can cause physical disability, pain, and vision loss, and place a great burden on middle-aged and elderly patients and their families. The results of this study showed that middle-aged and elderly diabetic patients with physical pain had a higher detection rate of depressive symptoms than those without physical pain. Neuropathy becomes a common complication in patients with long-term diabetes, which can lead to pain, sensory loss, and even amputation [23], and this neuropathic pain affects one-third of diabetic patients [24]. A meta-analysis that included low- and middle-income countries and involved nearly 300,000 people showed that pain and depression were highly correlated [25]. Meanwhile, a study in the United States [26] showed that individuals with long-term physical disabilities suffer higher levels of pain and pain interference compared to normal individuals. Furthermore, Mathew et al. [27] identified physical disability as a risk factor for depression in patients with diabetes through a cross-sectional survey. This further confirms why middle-aged and older patients with diabetes with physical disabilities are at increased risk of depression. Middle-aged and elderly people with diabetes are a special group in their own right, and with pain and physical disability, their health status is worse and they are more likely to suffer from mental health problems. Diabetic retinopathy (DR), a major retinal vascular complication of diabetes, is a progressive disease and one of the leading causes of visual impairment and blindness in diabetic patients [28], and the results of this study showed that middle-aged and older diabetic patients with visual impairment had a higher incidence of depression. Dornan et al. [29] found that older patients with diabetes with visual impairment had a much poorer health status and were more frequently depressed than those without visual impairment. The results of a population-based systematic review by Gianni et al. [30] showed that visual impairment was significantly associated with the occurrence of depression. Older adults with visual impairment have a reduced ability to perform daily activities, and their probability of falling and social isolation is higher [31], therefore, in conjunction with the disease, middle-aged and older patients with diabetes with visual impairment are more likely to experience depression. Therefore, more care and assistance should be provided to middle-aged and elderly patients with diabetes with somatic pain, physical disability, and visual impairment.
This study also found that middle-aged and older patients with diabetes who were satisfied with their lives had a lower risk of depression compared to those who were dissatisfied with their lives and that middle-aged and older patients with diabetes who were satisfied with their marriage had a lower risk of developing depressive symptoms compared to those who were dissatisfied with their marriages. A previous study [32] showed that depressive symptoms were significantly associated with life satisfaction in middle-aged and elderly Chinese patients with diabetes, and when middle-aged and elderly people have diabetes, their dissatisfaction with life increases greatly due to decreased quality of life, indirectly increasing their risk of depression. Min et al. [33] found that spousal care and marital satisfaction were important moderators of the onset of depression in patients with chronic disease. Furthermore, a recent study [34] extended the study from the individual to the couple level using marriage as an important social context, and this binary approach study confirmed that one’s health has an impact on both the depressive symptoms of the individual and the partner, which implies that high marital satisfaction represents a high quality couple relationship and that a high quality couple relationship can help both partners mitigate the effects and negative experiences of negative events in their lives, and, conversely, it can exacerbate the negative experiences of both partners and therefore increase the risk of depression.
All the data in this study came from the CHARLS database. The standard of inclusion of diabetic patients was oral questioning without clinical diagnosis, which may lead to bias of case data, which is the limitation of this study.In addition,most of the sample in the study was rural, female and less educated. These factors may have contributed to the higher prevalence of depression in this study.
Conclusion
In this study, the incidence of depression in middle-aged and elderly diabetic patients in China is high and is affected by multiple factors. To improve the mental health of middle-aged and elderly diabetic patients in China and allow them to lead a more active and healthy life, it is recommended that communities and hospitals increase caregiving services for middle-aged and elderly diabetic patients, strengthen the training of relevant professional caregivers, and focus on middle-aged and elderly diabetic patients aged 45−59 years with poor self-assessed health status, multiple comorbid chronic diseases, somatic pain, physical disability, visual impairment, and low satisfaction with life and marriage. In addition, the factors included in this study were based on the CHARLS database and the variables included were limited. The specific conditions of patients with diabetes in the sample could not be classified, and the results obtained may have some limitations.
Data availability
The datasets used and analyzed in the current study are available upon reasonable request from the official CHARLS application.
References
König H, König HH, Konnopka A. The excess costs of depression: a systematic review and meta-analysis. Epidemiol Psychiatric Sci. 2019;29:e30.
Liu J, Peng HY, Yan ZF, Huang KL, Wang MY, Mao QY, Wu X, Zhao ZH. China Health and Elderly Care Tracking Survey: depressive symptoms and Associated factors in Middle-aged and Elderly people with Disabilities. Chin J Behav Med Brain Sci. 2021;30(03):273–8.
Detka J, Kurek A, Basta-Kaim A, Kubera M, Lasoń W, Budziszewska B. Neuroendocrine link between stress, depression and Diabetes. Pharmacol Rep. 2013;65(6):1591–600.
Graham EA, Deschênes SS, Khalil MN, Danna S, Filion KB, Schmitz N. Measures of depression and risk of type 2 Diabetes: a systematic review and meta-analysis. J Affect Disord. 2020;265:224–32.
Owens-Gary MD, Zhang X, Jawanda S, Bullard KM, Allweiss P, Smith BD. The importance of addressing Depression and Diabetes distress in adults with type 2 Diabetes. J Gen Intern Med. 2019;34(2):320–4.
Perrin NE, Davies MJ, Robertson N, Snoek FJ, Khunti K. The prevalence of diabetes-specific emotional distress in people with type 2 Diabetes: a systematic review and meta-analysis. Diabet Medicine: J Br Diabet Association. 2017;34(11):1508–20.
Black S, Kraemer K, Shah A, Simpson G, Scogin F, Smith A. Diabetes, Depression, and Cognition: a recursive cycle of Cognitive Dysfunction and Glycemic Dysregulation. Curr Diab Rep. 2018;18(11):118.
Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry. 1999;14(8):608–17.
Xin Tao S, Jiliang. Structural analysis of CES-D and its trial in adults [J]. Chin J Clin Psychol 1997,5(1):14–6.
Majumdar S, Sinha B, Dastidar BG, Gangopadhyay KK, Ghoshal S, Mukherjee JJ, Mazumdar A, Ray S, Dasgupta S, Bhattacharjee K. Assessing prevalence and predictors of depression in type 2 Diabetes Mellitus (DM) patients - the DEPDIAB study. Diabetes Res Clin Pract. 2021;178:108980.
Lloyd CE, Roy T, Nouwen A, Chauhan AM. Epidemiology of depression in Diabetes: international and cross-cultural issues. J Affect Disord. 2012;142(Suppl):22–9.
Lloyd CE, Nouwen A, Sartorius N, Ahmed HU, Alvarez A, Bahendeka S, Basangwa D, Bobrov AE, Boden S, Bulgari V, et al. Prevalence and correlates of depressive disorders in people with type 2 Diabetes: results from the International Prevalence and Treatment of Diabetes and Depression (INTERPRET-DD) study, a collaborative study carried out in 14 countries. Diabet Medicine: J Br Diabet Association. 2018;35(6):760–9.
Nefs G, Pouwer F, Denollet J, Pop V. The course of depressive symptoms in primary care patients with type 2 Diabetes: results from the Diabetes, Depression, type D personality zuidoost-brabant (DiaDDZoB) study. Diabetologia. 2012;55(3):608–16.
Fan Y, He D. Self-rated health, socioeconomic status and all-cause mortality in Chinese middle-aged and elderly adults. Sci Rep. 2022;12(1):9309.
Rumsfeld JS, Alexander KP, Goff DC Jr., Graham MM, Ho PM, Masoudi FA, Moser DK, Roger VL, Slaughter MS, Smolderen KG, et al. Cardiovascular health: the importance of measuring patient-reported health status: a scientific statement from the American Heart Association. Circulation. 2013;127(22):2233–49.
Dong W, Pan XF, Yu C, Lv J, Guo Y, Bian Z, Yang L, Chen Y, Wu T, Chen Z, et al. Self-rated Health Status and Risk of Incident Stroke in 0.5 million Chinese adults: the China Kadoorie Biobank Study. J Stroke. 2018;20(2):247–57.
Huang CQ, Zhang XM, Dong BR, Lu ZC, Yue JR, Liu QX. Health status and risk for depression among the elderly: a meta-analysis of published literature. Age Ageing. 2010;39(1):23–30.
Badawi G, Pagé V, Smith KJ, Gariépy G, Malla A, Wang J, Boyer R, Strychar I, Lesage A, Schmitz N. Self-rated health: a predictor for the three year incidence of major depression in individuals with type II Diabetes. J Affect Disord. 2013;145(1):100–5.
Huang CQ, Dong BR, Lu ZC, Yue JR, Liu QX. Chronic Diseases and risk for depression in old age: a meta-analysis of published literature. Ageing Res Rev. 2010;9(2):131–41.
Patten SB, Williams JVA, Lavorato DH, Wang JL, Jetté N, Sajobi TT, Fiest KM, Bulloch AGM. Patterns of association of chronic medical conditions and major depression. Epidemiol Psychiatric Sci. 2018;27(1):42–50.
He MF. Study on the prevalence of depression in middle-aged and elderly people with chronic Diseases in China and its impact on patients with chronic Diseases. Ph.D. Jilin University; 2019.
Diabetes Society of Chinese Medical Association. Guidelines for the Prevention and Treatment of type 2 Diabetes in China (2020 edition). Chin J Diabetes. 2021;13(04):315–409.
Calcutt NA. Diabetic neuropathy and neuropathic pain: a (con)fusion of pathogenic mechanisms? Pain 2020, 161(Suppl 1):S65–s86.
Ziegler D, Tesfaye S, Spallone V, Gurieva I, Al Kaabi J, Mankovsky B, Martinka E, Radulian G, Nguyen KT, Stirban AO, et al. Screening, diagnosis and management of diabetic sensorimotor polyneuropathy in clinical practice: International expert consensus recommendations. Diabetes Res Clin Pract. 2022;186:109063.
Stubbs B, Vancampfort D, Veronese N, Thompson T, Fornaro M, Schofield P, Solmi M, Mugisha J, Carvalho AF, Koyanagi A. Depression and pain: primary data and meta-analysis among 237 952 people across 47 low- and middle-income countries. Psychol Med. 2017;47(16):2906–17.
Molton I, Cook KF, Smith AE, Amtmann D, Chen WH, Jensen MP. Prevalence and impact of pain in adults aging with a physical disability: comparison to a US general population sample. Clin J Pain. 2014;30(4):307–15.
Madhu M, Abish A, Anu K, Jophin RI, Kiran AM, Vijayakumar K. Predictors of depression among patients with Diabetes Mellitus in Southern India. Asian J Psychiatry. 2013;6(4):313–7.
Coney JM. Addressing unmet needs in diabetic retinopathy. Am J Manag Care. 2019;25(16 Suppl):311–s316.
Dornan TL, Peck GM, Dow JD, Tattersall RB. A community survey of Diabetes in the elderly. Diabet Medicine: J Br Diabet Association. 1992;9(9):860–5.
Virgili G, Parravano M, Petri D, Maurutto E, Menchini F, Lanzetta P, Varano M, Mariotti SP, Cherubini A, Lucenteforte E. The Association between Vision Impairment and Depression: a systematic review of Population-Based studies. J Clin Med 2022, 11(9).
Ehrlich JR, Ramke J, Macleod D, Burn H, Lee CN, Zhang JH, Waldock W, Swenor BK, Gordon I, Congdon N, et al. Association between vision impairment and mortality: a systematic review and meta-analysis. The Lancet Global Health. 2021;9(4):e418–30.
Li C, Chi I, Zhang X, Cheng Z, Zhang L, Chen G. Urban and rural factors associated with life satisfaction among older Chinese adults. Aging Ment Health. 2015;19(10):947–54.
Min J, Yorgason JB, Fast J, Chudyk A. The impact of spouse’s Illness on depressive symptoms: the roles of spousal caregiving and marital satisfaction. The Journals of Gerontology Series B Psychological Sciences and Social Sciences. 2020;75(7):1548–57.
Monin JK, Levy B, Chen B, Fried T, Stahl ST, Schulz R, Doyle M, Kershaw T. Husbands’ and wives’ physical activity and depressive symptoms: longitudinal findings from the Cardiovascular Health Study. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine. 2015;49(5):704–14.
Acknowledgements
The authors thank the China Health and Retirement Longitudinal Study (CHARLS) team for providing data.
Funding
This study did not receive any specific funding from funding agencies in the public, commercial, or non-profit sectors.
Author information
Authors and Affiliations
Contributions
S.B., Y.M., J.L.: data collection S.B: Data processing and article writing A.Z, Z.Z: revise the article J.W: Review manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participation
This study was carried out based on data extracted from the CHARLS public database, and all methods were performed according to the relevant guidelines and regulations. Written informed consent was obtained from all participants or their legal agents before the commencement of any study process. The ethics approval for the collection of CHARLS data has been approved by the Peking University Biomedical Ethics Review Committee (IRB00001052-11015). The use of CHARLS data was approved by the Human Research Ethics Committee of the University of Newcastle (H-2015-0290).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bai, S., Wang, J., Liu, J. et al. Analysis of depression incidence and influence factors among middle-aged and elderly diabetic patients in China: based on CHARLS data. BMC Psychiatry 24, 146 (2024). https://doi.org/10.1186/s12888-023-05473-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-05473-6